Lissencephaly: Difference between revisions
No edit summary |
m (A summary of a video has been added.) |
||
| (20 intermediate revisions by 3 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox">'''Original Editor '''- [[User: Sehriban Ozmen]] <br> | <div class="editorbox">'''Original Editor '''- [[User: Sehriban Ozmen|Sehriban Ozmen]] <br> | ||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}}</div> | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}}</div> | ||
== Introduction == | |||
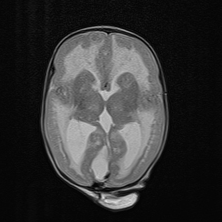
[[File:Lissencephaly.jpg|alt=|"Smooth brain" appearance of lissencephaly.|frame]] | |||
Lissencephaly (LIS) is a spectrum that includes various [[Brain Anatomy|brain]] malformations. <ref name=":0">Koenig M, Dobyns WB, Di Donato N. [https://www.sciencedirect.com/science/article/abs/pii/S109037982100180X Lissencephaly: Update on diagnostics and clinical management.] European Journal of Paediatric Neurology. 2021 Nov 1;35:147-52.</ref> Its prevalence is estimated at 11.7 to 40 per million births. <ref name=":1">Fry AE, Cushion TD, Pilz DT. [https://onlinelibrary.wiley.com/doi/abs/10.1002/ajmg.c.31402 The genetics of lissencephaly.] InAmerican Journal of Medical Genetics Part C: Seminars in Medical Genetics 2014 Jun (Vol. 166, No. 2, pp. 198-210).</ref> | |||
The prognosis depends on the severity of the syndrome. Most children remain in an early developmental level and have a short life expectancy, many dying before 10 years old. Aspiration and [[Respiratory Disorders|respiratory disease]] and the most common reasons for death.<ref>Kattuoa M, Das J. [https://www.ncbi.nlm.nih.gov/books/NBK560766/ Lissencephaly]. Stat Pearls: Treasure Island, FL, USA. 2021.Available:https://www.ncbi.nlm.nih.gov/books/NBK560766/ (accessed 7.10.2023)</ref> | |||
[[ | |||
It is derived from the combination of two Greek words meaning soft ("lissos") and brain ("enkephalos"). <ref name=":1" /> This smooth appearance of the brain, which can be observed in MRI imaging, is associated with malformations of cortical development such as agyria (absence of gyrus), pachygyria (extremely wide gyrus), and subcortical band heterotopia (SBH, double cortex). <ref name=":0" /><ref>Malinger G, Kidron D, Schreiber L, Ben‐Sira L, Hoffmann C, Lev D, Lerman‐Sagie T. [https://pubmed.ncbi.nlm.nih.gov/17219377/ Prenatal diagnosis of malformations of cortical development by dedicated neurosonography.] Ultrasound in Obstetrics and Gynecology: The Official Journal of the International Society of Ultrasound in Obstetrics and Gynecology. 2007 Feb;29(2):178-91.</ref> | It is derived from the combination of two Greek words meaning soft ("lissos") and brain ("enkephalos"). <ref name=":1" /> This smooth appearance of the brain, which can be observed in [[MRI Scans|MRI]] imaging, is associated with malformations of cortical development such as agyria (absence of gyrus), pachygyria (extremely wide gyrus), and subcortical band heterotopia (SBH, double cortex). <ref name=":0" /><ref>Malinger G, Kidron D, Schreiber L, Ben‐Sira L, Hoffmann C, Lev D, Lerman‐Sagie T. [https://pubmed.ncbi.nlm.nih.gov/17219377/ Prenatal diagnosis of malformations of cortical development by dedicated neurosonography.] Ultrasound in Obstetrics and Gynecology: The Official Journal of the International Society of Ultrasound in Obstetrics and Gynecology. 2007 Feb;29(2):178-91.</ref> | ||
Lissencephaly is generally divided into two subtypes: type 1 (classical LIS / isolated lissencephaly sequence) and type 2 (cobblestone LIS). <ref name=":3">Fernández V, Llinares‐Benadero C, Borrell V. [https://www.embopress.org/doi/full/10.15252/embj.201593701 Cerebral cortex expansion and folding: what have we learned?.] The EMBO journal. 2016 May 17;35(10):1021-44.</ref> | Lissencephaly is generally divided into two subtypes: type 1 (classical LIS / isolated lissencephaly sequence) and type 2 (cobblestone LIS). <ref name=":3">Fernández V, Llinares‐Benadero C, Borrell V. [https://www.embopress.org/doi/full/10.15252/embj.201593701 Cerebral cortex expansion and folding: what have we learned?.] The EMBO journal. 2016 May 17;35(10):1021-44.</ref> | ||
| Line 19: | Line 16: | ||
Type 1 can present in different forms such as isolated LIS, Miller-Dieker Syndrome (MDS), Norman-Roberts syndrome, and X-linked LIS with ambiguous genitalia (XLAG). <ref>Herrera JF, Ramírez RG, Zárate MD. [https://www.medigraphic.com/cgi-bin/new/resumenI.cgi?IDARTICULO=16883 Lisencefalia tipo I: síndrome de Miller-Dieker. Informe de un caso.] Revista Mexicana de Pediatría. 1999;66(4):157-60.</ref><ref name=":2">Juric-Sekhar G, Hevner RF. [https://www.annualreviews.org/doi/abs/10.1146/annurev-pathmechdis-012418-012927 Malformations of cerebral cortex development: molecules and mechanisms.] Annual Review of Pathology: Mechanisms of Disease. 2019 Jan 24;14:293-318.</ref> | Type 1 can present in different forms such as isolated LIS, Miller-Dieker Syndrome (MDS), Norman-Roberts syndrome, and X-linked LIS with ambiguous genitalia (XLAG). <ref>Herrera JF, Ramírez RG, Zárate MD. [https://www.medigraphic.com/cgi-bin/new/resumenI.cgi?IDARTICULO=16883 Lisencefalia tipo I: síndrome de Miller-Dieker. Informe de un caso.] Revista Mexicana de Pediatría. 1999;66(4):157-60.</ref><ref name=":2">Juric-Sekhar G, Hevner RF. [https://www.annualreviews.org/doi/abs/10.1146/annurev-pathmechdis-012418-012927 Malformations of cerebral cortex development: molecules and mechanisms.] Annual Review of Pathology: Mechanisms of Disease. 2019 Jan 24;14:293-318.</ref> | ||
Type 2 represents the severe end of a spectrum and can present in three syndromes: Walker-Warburg syndrome (WWS), muscle eye-brain (MEB) disease, and Fukuyama | Type 2 represents the severe end of a spectrum and can present in three syndromes: Walker-Warburg syndrome (WWS), muscle eye-brain (MEB) disease, and Fukuyama Congenital Muscular Dystrophy (FCMD). <ref>Shenoy AM, Markowitz JA, Bonnemann CG, Krishnamoorthy K, Bossler AD, Tseng BS. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2925645/ Muscle-eye-brain disease. Journal of clinical neuromuscular disease.] 2010 Mar;11(3):124.</ref><ref>Angelini C, Angelini C. [https://link.springer.com/chapter/10.1007/978-3-319-56454-8_27 Fukuyama congenital muscular dystrophy: walker-warburg syndrome.] Springer International Publishing; 2018.</ref><ref name=":2" /> | ||
== Clinically Relevant Anatomy == | == Clinically Relevant Anatomy == | ||
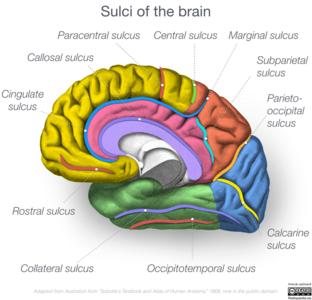
[[File:Whole Brain Sulci.png|right|frameless|312x312px]]The [[Cerebral Cortex|cerebral cortex]] is the outermost part of the brain surrounded by [[meninges]]. <ref name=":4">Javed K, Reddy V, Lui F. [https://www.ncbi.nlm.nih.gov/books/NBK537247/ Neuroanatomy, cerebral cortex] [Internet]. Treasure Island.</ref> It contains about 16 billion neurons, making up more than eighty per cent of the total weight of the [[Brain Anatomy|brain]]. <ref>Azevedo FA, Carvalho LR, Grinberg LT, Farfel JM, Ferretti RE, Leite RE, Filho WJ, Lent R, Herculano‐Houzel S. [https://onlinelibrary.wiley.com/doi/abs/10.1002/cne.21974 Equal numbers of neuronal and nonneuronal cells make the human brain an isometrically scaled‐up primate brain.] Journal of Comparative Neurology. 2009 Apr 10;513(5):532-41.</ref> | |||
The development of the [[Cerebral Cortex|cerebral cortex]], which is anatomically composed of the neocortex (or isocortex) and allocortex, <ref name=":5">Cadwell CR, Bhaduri A, Mostajo-Radji MA, Keefe MG, Nowakowski TJ. [https://www.sciencedirect.com/science/article/pii/S089662731930635X Development and arealization of the cerebral cortex.] Neuron. 2019 Sep 25;103(6):980-1004.</ref> begins in the uterus at the rostral (anterior) portion of the neural tube. <ref name=":6">Quezada S, Castillo‐Melendez M, Walker DW, Tolcos M. [https://physoc.onlinelibrary.wiley.com/doi/10.1113/JP277151 Development of the cerebral cortex and the effect of the intrauterine environment.] The Journal of physiology. 2018 Dec;596(23):5665-74.</ref> With the proliferation of neurons in the forebrain, the 6-layer structure, which is the initial state of the neocortex, is formed. <ref>Agirman G, Broix L, Nguyen L. [https://febs.onlinelibrary.wiley.com/doi/epdf/10.1002/1873-3468.12924 Cerebral cortex development: an outside‐in perspective.] FEBS letters. 2017 Dec;591(24):3978-92.</ref><ref name=":5" /> | The development of the [[Cerebral Cortex|cerebral cortex]], which is anatomically composed of the neocortex (or isocortex) and allocortex, <ref name=":5">Cadwell CR, Bhaduri A, Mostajo-Radji MA, Keefe MG, Nowakowski TJ. [https://www.sciencedirect.com/science/article/pii/S089662731930635X Development and arealization of the cerebral cortex.] Neuron. 2019 Sep 25;103(6):980-1004.</ref> begins in the uterus at the rostral (anterior) portion of the neural tube. <ref name=":6">Quezada S, Castillo‐Melendez M, Walker DW, Tolcos M. [https://physoc.onlinelibrary.wiley.com/doi/10.1113/JP277151 Development of the cerebral cortex and the effect of the intrauterine environment.] The Journal of physiology. 2018 Dec;596(23):5665-74.</ref> With the proliferation of neurons in the forebrain, the 6-layer structure, which is the initial state of the neocortex, is formed. <ref>Agirman G, Broix L, Nguyen L. [https://febs.onlinelibrary.wiley.com/doi/epdf/10.1002/1873-3468.12924 Cerebral cortex development: an outside‐in perspective.] FEBS letters. 2017 Dec;591(24):3978-92.</ref><ref name=":5" /> | ||
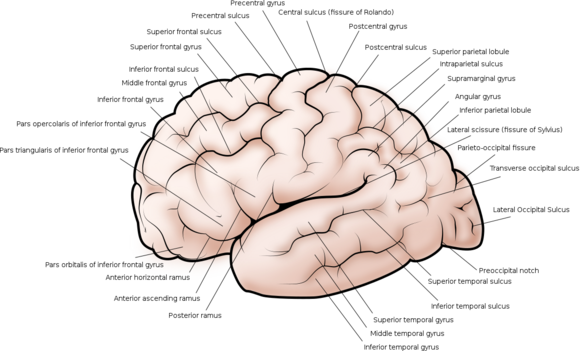
Later, as the volume of the brain grows, folding occurs, forming the gyrus and sulcus of the brain. <ref>Welker W. [https://link.springer.com/chapter/10.1007/978-1-4615-3824-0_1 Why does cerebral cortex fissure and fold? A review of determinants of gyri and sulci.] Cerebral Cortex: comparative structure and evolution of Cerebral Cortex, Part II. 1990:3-136.</ref> This process, called gyrification, is an adaptation of the brain to fit into the cranium, <ref name=":3" /> starts in the 2nd trimester of gestation, <ref name=":6" /> peaks in early adolescence, stabilise in adulthood and regresses with ageing. <ref>Raznahan A, Shaw P, Lalonde F, Stockman M, Wallace GL, Greenstein D, Clasen L, Gogtay N, Giedd JN. [https://pubmed.ncbi.nlm.nih.gov/21562281/ How does your cortex grow?]. Journal of Neuroscience. 2011 May 11;31(19):7174-7.</ref>[[File:Cerebral_cortex_side_view.png|alt=|right|frameless|580x580px]]Gyrification is also important for the functional organization of the brain. <ref name=":3" /> Prominent sulci such as Sylvian, central, parieto-occipital and calcarine divide the brain roughly into 4 lobes ([[Frontal Lobe|frontal]], [[Parietal Lobe|parietal]], [[Temporal Lobe|temporal]], [[Occipital Lobe|occipital]]) each of which is specialized functions. <ref name=":4" /><ref>Stiles J, Jernigan TL. [https://link.springer.com/article/10.1007/s11065-010-9148-4 The basics of brain development.] Neuropsychology review. 2010 Dec;20(4):327-48.</ref> | |||
As in lissencephaly, disruptions that occur in the gyrification process cause changes in the structure and thus function of the brain, leading to intellectual and motor disability, also intractable [[epilepsy]]. <ref name=":6" /><ref name=":3" /> | |||
As in lissencephaly, disruptions that occur in the gyrification process cause changes in the structure and thus function of the brain, leading to intellectual | |||
== Pathological Process == | == Pathological Process == | ||
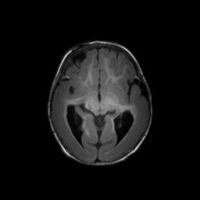
[[File:Lissencephaly-pachygyria-complex-1.jpg|thumb|200x200px|MRI of a lissencephaly case with pachygria.]] | |||
Lissencephaly is caused by genetic (mutations especially in LIS1 (PAFAH1B1) gene for classical LIS, <ref>Reiner O, Carrozzo R, Shen Y, Wehnert M, Faustinella F, Dobyns WB, Caskey CT, Ledbetter DH. [https://www.nature.com/articles/364717a0 Isolation of a Miller–Dicker lissencephaly gene containing G protein β-subunit-like repeats.] Nature. 1993 Aug 19;364(6439):717-21.</ref> doublecortin (DCX) gene for SBH <ref name=":2" /> and TUBA1A gene for [[microcephaly]] <ref>Chang BS. [https://journals.sagepub.com/doi/pdf/10.5698/1535-7597-15.2.65 Tubulinopathies and their brain malformation syndromes: every TUB on its own bottom: the phenotypic Spectrum of Tubulinopathies.] Epilepsy Currents. 2015 Mar;15(2):65-7.</ref>) or non-genetic factors (viral infections, <ref name=":2" /> <ref name=":7">Lapo-Córdova NS, Ruiz-García M, Hernández-Antúnez BG. [https://www.scielo.org.mx/scielo.php?pid=S1665-50442021000400134&script=sci_arttext&tlng=en Lissencephaly: Clinical and neuroimaging features in children.] Revista mexicana de neurociencia. 2021 Aug;22(4):134-40.</ref> hypoxia, <ref name=":2" /> preterm birth <ref>Brown WR. [https://www.nature.com/articles/pr2009139 Association of preterm birth with brain malformations.] Pediatric research. 2009 Jun;65(6):642-6.</ref>). | Lissencephaly is caused by genetic (mutations especially in LIS1 (PAFAH1B1) gene for classical LIS, <ref>Reiner O, Carrozzo R, Shen Y, Wehnert M, Faustinella F, Dobyns WB, Caskey CT, Ledbetter DH. [https://www.nature.com/articles/364717a0 Isolation of a Miller–Dicker lissencephaly gene containing G protein β-subunit-like repeats.] Nature. 1993 Aug 19;364(6439):717-21.</ref> doublecortin (DCX) gene for SBH <ref name=":2" /> and TUBA1A gene for [[microcephaly]] <ref>Chang BS. [https://journals.sagepub.com/doi/pdf/10.5698/1535-7597-15.2.65 Tubulinopathies and their brain malformation syndromes: every TUB on its own bottom: the phenotypic Spectrum of Tubulinopathies.] Epilepsy Currents. 2015 Mar;15(2):65-7.</ref>) or non-genetic factors (viral infections, <ref name=":2" /> <ref name=":7">Lapo-Córdova NS, Ruiz-García M, Hernández-Antúnez BG. [https://www.scielo.org.mx/scielo.php?pid=S1665-50442021000400134&script=sci_arttext&tlng=en Lissencephaly: Clinical and neuroimaging features in children.] Revista mexicana de neurociencia. 2021 Aug;22(4):134-40.</ref> hypoxia, <ref name=":2" /> preterm birth <ref>Brown WR. [https://www.nature.com/articles/pr2009139 Association of preterm birth with brain malformations.] Pediatric research. 2009 Jun;65(6):642-6.</ref>). | ||
Pathological processes caused by genetic mutations can be summarized as follows; | Pathological processes caused by genetic mutations can be summarized as follows; | ||
Primitive neurons (neuroblasts) generated from the stem cells in the neural tube should migrate through the entire cortical thickness and stop precisely near the cortical surface, but instead, they fail to migrate and position properly. <ref>Wynshaw-Boris A, Pramparo T, Youn YH, Hirotsune S. [https://www.sciencedirect.com/science/article/abs/pii/S1084952110001242 Lissencephaly: mechanistic insights from animal models and potential therapeutic strategies.] InSeminars in cell & developmental biology 2010 Oct 1 (Vol. 21, No. 8, pp. 823-830). Academic Press.</ref><ref name=":3" /> | Primitive neurons (neuroblasts) generated from the stem cells in the neural tube should migrate through the entire cortical thickness and stop precisely near the cortical surface, but instead, they fail to migrate and position properly. <ref>Wynshaw-Boris A, Pramparo T, Youn YH, Hirotsune S. [https://www.sciencedirect.com/science/article/abs/pii/S1084952110001242 Lissencephaly: mechanistic insights from animal models and potential therapeutic strategies.] InSeminars in cell & developmental biology 2010 Oct 1 (Vol. 21, No. 8, pp. 823-830). Academic Press.</ref><ref name=":3" />[[File:Lissencephaly-Subcortical Band Heterotopia.jpg|MRI of a lissencephaly case with SBH.|alt=|thumb|185x185px]]In type 1 LIS they accumulate below the preplate in only four layers, thus causing thickened cortex with reduced folding (pachygyria or agyria). <ref>Golden JA, Harding BN. [https://cir.nii.ac.jp/crid/1130282271826869632 Developmental neuropathology. (No Title).] 2004.</ref><ref name=":1" /> | ||
In type 1 LIS they accumulate below the preplate in only four layers, thus causing thickened cortex with reduced folding (pachygyria or agyria). <ref>Golden JA, Harding BN. [https://cir.nii.ac.jp/crid/1130282271826869632 Developmental neuropathology. (No Title).] 2004.</ref><ref name=":1" /> | |||
Their accumulation in the cortical white matter just below the cortical grey matter and forming a thick grey layer called SBH. Reduction in the size of the cerebral cortex and some cases also microgyria accompany this. <ref name=":8">Barkovich AJ, Guerrini R, Kuzniecky RI, Jackson GD, Dobyns WB. [https://academic.oup.com/brain/article/135/5/1348/304670 A developmental and genetic classification for malformations of cortical development: update 2012.] Brain. 2012 May 1;135(5):1348-69.</ref><ref>Barkovich AJ, Kuzniecky RI, Dobyns WB. [https://journals.lww.com/co-neurology/Abstract/2001/04000/Radiologic_classification_of_malformations_of.2.aspx Radiologic classification of malformations of cortical development.] Current opinion in neurology. 2001 Apr 1;14(2):145-9.</ref><ref>Ross ME, Walsh CA. [https://www.annualreviews.org/doi/abs/10.1146/annurev.neuro.24.1.1041 Human brain malformations and their lessons for neuronal migration.] Annual review of neuroscience. 2001 Mar;24(1):1041-70.</ref> | Their accumulation in the cortical white matter just below the cortical grey matter and forming a thick grey layer called SBH. Reduction in the size of the cerebral cortex and some cases also microgyria accompany this. <ref name=":8">Barkovich AJ, Guerrini R, Kuzniecky RI, Jackson GD, Dobyns WB. [https://academic.oup.com/brain/article/135/5/1348/304670 A developmental and genetic classification for malformations of cortical development: update 2012.] Brain. 2012 May 1;135(5):1348-69.</ref><ref>Barkovich AJ, Kuzniecky RI, Dobyns WB. [https://journals.lww.com/co-neurology/Abstract/2001/04000/Radiologic_classification_of_malformations_of.2.aspx Radiologic classification of malformations of cortical development.] Current opinion in neurology. 2001 Apr 1;14(2):145-9.</ref><ref>Ross ME, Walsh CA. [https://www.annualreviews.org/doi/abs/10.1146/annurev.neuro.24.1.1041 Human brain malformations and their lessons for neuronal migration.] Annual review of neuroscience. 2001 Mar;24(1):1041-70.</ref> | ||
| Line 46: | Line 38: | ||
== Clinical Presentation == | == Clinical Presentation == | ||
[[File:Microlissencephaly.gif| | [[File:Microlissencephaly.gif|MRI of a micro-lissencephaly case.|alt=|frame]] | ||
Clinical symptoms/findings of lissencephaly can be various including: | Clinical symptoms/findings of lissencephaly can be various including: | ||
| Line 53: | Line 45: | ||
* Drug-resistant [[epilepsy]] <ref>Dobyns WB. [https://onlinelibrary.wiley.com/doi/full/10.1111/j.1528-1167.2009.02433.x The clinical patterns and molecular genetics of lissencephaly and subcortical band heterotopia.] Epilepsia. 2010 Feb;51:5-9.</ref> | * Drug-resistant [[epilepsy]] <ref>Dobyns WB. [https://onlinelibrary.wiley.com/doi/full/10.1111/j.1528-1167.2009.02433.x The clinical patterns and molecular genetics of lissencephaly and subcortical band heterotopia.] Epilepsia. 2010 Feb;51:5-9.</ref> | ||
* Neonatal hypotonia later evolves into spastic quadriparesis with truncal hypotonia (in isolated lissencephaly sequence) <ref name=":1" /> | * Neonatal hypotonia later evolves into spastic quadriparesis with truncal hypotonia (in isolated lissencephaly sequence) <ref name=":1" /> | ||
* Hypertonia <ref name=":7" /> | * [[Hypertonia Assessment Tool|Hypertonia]] <ref name=":7" /> | ||
* Muscle spasms <ref>Saillour Y, Carion N, Quelin C, Leger PL, Boddaert N, Elie C, Toutain A, Mercier S, Barthez MA, Milh M, Joriot S. [https://jamanetwork.com/journals/jamaneurology/article-abstract/797746 LIS1-related isolated lissencephaly: spectrum of mutations and relationships with malformation severity.] Archives of neurology. 2009 Aug 1;66(8):1007-15.</ref><ref name=":4" /> | * Muscle spasms <ref>Saillour Y, Carion N, Quelin C, Leger PL, Boddaert N, Elie C, Toutain A, Mercier S, Barthez MA, Milh M, Joriot S. [https://jamanetwork.com/journals/jamaneurology/article-abstract/797746 LIS1-related isolated lissencephaly: spectrum of mutations and relationships with malformation severity.] Archives of neurology. 2009 Aug 1;66(8):1007-15.</ref><ref name=":4" /> | ||
* Facial dysmorphism: Usually MDS-related high forehead, small jaw, short upturned nose, protuberant upper lip and bitemporal hollowing. <ref>Dobyns WB, Curry CJ, Hoyme HE, Turlington L, Ledbetter DH. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1682996/ Clinical and molecular diagnosis of Miller-Dieker syndrome.] American journal of human genetics. 1991 Mar;48(3):584.</ref><ref>Cardoso C, Leventer RJ, Ward HL, Toyo-Oka K, Chung J, Gross A, Martin CL, Allanson J, Pilz DT, Olney AH, Mutchinick OM. [https://www.sciencedirect.com/science/article/pii/S0002929707606132 Refinement of a 400-kb critical region allows genotypic differentiation between isolated lissencephaly, Miller-Dieker syndrome, and other phenotypes secondary to deletions of 17p13. 3.] The American Journal of Human Genetics. 2003 Apr 1;72(4):918-30.</ref> | * Facial dysmorphism: Usually MDS-related high forehead, small jaw, short upturned nose, protuberant upper lip and bitemporal hollowing. <ref>Dobyns WB, Curry CJ, Hoyme HE, Turlington L, Ledbetter DH. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1682996/ Clinical and molecular diagnosis of Miller-Dieker syndrome.] American journal of human genetics. 1991 Mar;48(3):584.</ref><ref>Cardoso C, Leventer RJ, Ward HL, Toyo-Oka K, Chung J, Gross A, Martin CL, Allanson J, Pilz DT, Olney AH, Mutchinick OM. [https://www.sciencedirect.com/science/article/pii/S0002929707606132 Refinement of a 400-kb critical region allows genotypic differentiation between isolated lissencephaly, Miller-Dieker syndrome, and other phenotypes secondary to deletions of 17p13. 3.] The American Journal of Human Genetics. 2003 Apr 1;72(4):918-30.</ref> | ||
| Line 62: | Line 54: | ||
== Diagnostic Procedures == | == Diagnostic Procedures == | ||
Prenatal diagnosis is usually possible after 27 weeks of gestation with fetal | Prenatal diagnosis is usually possible after 27 weeks of gestation with fetal Magnetic Resonance Imaging (MRI) or [[Ultrasound Scans|Ultrasound]]. <ref>Malinger G, Kidron D, Schreiber L, Ben‐Sira L, Hoffmann C, Lev D, Lerman‐Sagie T. [https://obgyn.onlinelibrary.wiley.com/doi/full/10.1002/uog.3906 Prenatal diagnosis of malformations of cortical development by dedicated neurosonography.] Ultrasound in Obstetrics and Gynecology: The Official Journal of the International Society of Ultrasound in Obstetrics and Gynecology. 2007 Feb;29(2):178-91.</ref> In the postnatal period, MRI is a reliable diagnostic method. <ref name=":0" /> | ||
Alongside neuroimaging methods, genetic testing is highly recommended as a modern diagnostic tool. <ref name=":0" /> Considering that 31 genes providing almost 90% diagnostic yield associated with lissencephaly have been identified so far, <ref name=":0" /> it is important in terms of prenatal diagnosis, prognostic information, risk of recurrence in the family, avoidance of unnecessary research, and personalized medicine. <ref name=":1" /><ref name=":2" /> | Alongside neuroimaging methods, genetic testing is highly recommended as a modern diagnostic tool. <ref name=":0" /> Considering that 31 genes providing almost 90% diagnostic yield associated with lissencephaly have been identified so far, <ref name=":0" /> it is important in terms of prenatal diagnosis, prognostic information, risk of recurrence in the family, avoidance of unnecessary research, and personalized medicine. <ref name=":1" /><ref name=":2" /> | ||
| Line 78: | Line 70: | ||
== Differential Diagnosis == | == Differential Diagnosis == | ||
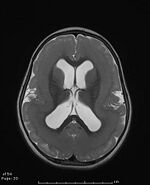
[[File:Lissencephaly type 2.png| | [[File:Lissencephaly type 2.png|MRI of a lissencephaly case with cobblestone malformation.|alt=|frame]] | ||
During MRI analysis, lissencephaly needs to be well differentiated from other malformations of cortical developments (especially cobblestone and polymicrogyria). <ref name=":0" /> Even a recent study <ref>Mohamed K, Bakry M, Elmalik EE, Bayoumi MA. [https://www.proquest.com/openview/74f95929206764c97a3d97b9c20b6b82/1?pq-origsite=gscholar&cbl=2040977 Lissencephaly causing refractory neonatal seizures in a term neonate.] BMJ Case Reports. 2022 May 1;15(5):e249245.</ref> advocates that although Cobblestone malformation is often referred to as type 2 lissencephaly, this term should not be used due to its different pathological mechanisms. On the other hand, polymicrogyria is a characteristic malformation of [[schizencephaly]] and they were put together in a category of the classification for malformations of cortical development <ref name=":8" />. | During MRI analysis, lissencephaly needs to be well differentiated from other malformations of cortical developments (especially cobblestone and polymicrogyria). <ref name=":0" /> Even a recent study <ref>Mohamed K, Bakry M, Elmalik EE, Bayoumi MA. [https://www.proquest.com/openview/74f95929206764c97a3d97b9c20b6b82/1?pq-origsite=gscholar&cbl=2040977 Lissencephaly causing refractory neonatal seizures in a term neonate.] BMJ Case Reports. 2022 May 1;15(5):e249245.</ref> advocates that although Cobblestone malformation is often referred to as type 2 lissencephaly, this term should not be used due to its different pathological mechanisms. On the other hand, polymicrogyria is a characteristic malformation of [[schizencephaly]] and they were put together in a category of the classification system for malformations of cortical development <ref name=":8" />. | ||
In addition, major brain abnormalities (e.g., severe congenital microcephaly, agenesis of the corpus callosum, or cerebellar hypoplasia) are not found in classical LIS. <ref name=":8" /> And compared to MDS, the face is less dysmorphic, and extracerebral malformations such as heart defects, omphalocele, cleft palate and genital anomalies, which are occasionally reported in MDS, are not generally encountered. <ref name=":1" /> | In addition, major brain abnormalities (e.g., severe congenital microcephaly, agenesis of the corpus callosum, or cerebellar hypoplasia) are not found in classical LIS. <ref name=":8" /> And compared to MDS, the face is less dysmorphic, and extracerebral malformations such as heart defects, omphalocele, cleft palate and genital anomalies, which are occasionally reported in MDS, are not generally encountered. <ref name=":1" /> | ||
== Resources == | == Resources == | ||
* [https://www.lissfoundation.org/resources Lissencephaly Foundation Inc | USA] | |||
* An interview video of a child with lissencephaly by 'Special Books by Special Kids'. | |||
{{#ev:youtube|j0H5qoC9GYw}}<ref>Special Books by Special Kids. Living with a Smooth Brain (Lissencephaly). Available from: https://www.youtube.com/watch?v=j0H5qoC9GYw</ref><br /> | |||
== References == | == References == | ||
| Line 94: | Line 85: | ||
[[Category:Paediatrics]] | [[Category:Paediatrics]] | ||
[[Category:Conditions]] | [[Category:Conditions]] | ||
[[Category:Head]] | |||
[[Category:Head - Conditions]] | |||
[[Category:Neurological - Conditions]] | |||
Latest revision as of 23:41, 2 April 2024
Top Contributors - Sehriban Ozmen, Kirenga Bamurange Liliane and Lucinda hampton
Introduction[edit | edit source]
Lissencephaly (LIS) is a spectrum that includes various brain malformations. [1] Its prevalence is estimated at 11.7 to 40 per million births. [2]
The prognosis depends on the severity of the syndrome. Most children remain in an early developmental level and have a short life expectancy, many dying before 10 years old. Aspiration and respiratory disease and the most common reasons for death.[3]
It is derived from the combination of two Greek words meaning soft ("lissos") and brain ("enkephalos"). [2] This smooth appearance of the brain, which can be observed in MRI imaging, is associated with malformations of cortical development such as agyria (absence of gyrus), pachygyria (extremely wide gyrus), and subcortical band heterotopia (SBH, double cortex). [1][4]
Lissencephaly is generally divided into two subtypes: type 1 (classical LIS / isolated lissencephaly sequence) and type 2 (cobblestone LIS). [5]
Type 1 can present in different forms such as isolated LIS, Miller-Dieker Syndrome (MDS), Norman-Roberts syndrome, and X-linked LIS with ambiguous genitalia (XLAG). [6][7]
Type 2 represents the severe end of a spectrum and can present in three syndromes: Walker-Warburg syndrome (WWS), muscle eye-brain (MEB) disease, and Fukuyama Congenital Muscular Dystrophy (FCMD). [8][9][7]
Clinically Relevant Anatomy[edit | edit source]
The cerebral cortex is the outermost part of the brain surrounded by meninges. [10] It contains about 16 billion neurons, making up more than eighty per cent of the total weight of the brain. [11]
The development of the cerebral cortex, which is anatomically composed of the neocortex (or isocortex) and allocortex, [12] begins in the uterus at the rostral (anterior) portion of the neural tube. [13] With the proliferation of neurons in the forebrain, the 6-layer structure, which is the initial state of the neocortex, is formed. [14][12]
Later, as the volume of the brain grows, folding occurs, forming the gyrus and sulcus of the brain. [15] This process, called gyrification, is an adaptation of the brain to fit into the cranium, [5] starts in the 2nd trimester of gestation, [13] peaks in early adolescence, stabilise in adulthood and regresses with ageing. [16]
Gyrification is also important for the functional organization of the brain. [5] Prominent sulci such as Sylvian, central, parieto-occipital and calcarine divide the brain roughly into 4 lobes (frontal, parietal, temporal, occipital) each of which is specialized functions. [10][17]
As in lissencephaly, disruptions that occur in the gyrification process cause changes in the structure and thus function of the brain, leading to intellectual and motor disability, also intractable epilepsy. [13][5]
Pathological Process[edit | edit source]
Lissencephaly is caused by genetic (mutations especially in LIS1 (PAFAH1B1) gene for classical LIS, [18] doublecortin (DCX) gene for SBH [7] and TUBA1A gene for microcephaly [19]) or non-genetic factors (viral infections, [7] [20] hypoxia, [7] preterm birth [21]). Pathological processes caused by genetic mutations can be summarized as follows;
Primitive neurons (neuroblasts) generated from the stem cells in the neural tube should migrate through the entire cortical thickness and stop precisely near the cortical surface, but instead, they fail to migrate and position properly. [22][5]
In type 1 LIS they accumulate below the preplate in only four layers, thus causing thickened cortex with reduced folding (pachygyria or agyria). [23][2]
Their accumulation in the cortical white matter just below the cortical grey matter and forming a thick grey layer called SBH. Reduction in the size of the cerebral cortex and some cases also microgyria accompany this. [24][25][26]
In type 2 LIS because of the impaired cortical basement membrane, they over-migrate into the subarachnoid space, causing a bumpy appearance as cobblestones on the cortical surface. [27][28]
Clinical Presentation[edit | edit source]
Clinical symptoms/findings of lissencephaly can be various including:
- Neurodevelopmental delay [20]
- Intellectual disability [10]
- Drug-resistant epilepsy [29]
- Neonatal hypotonia later evolves into spastic quadriparesis with truncal hypotonia (in isolated lissencephaly sequence) [2]
- Hypertonia [20]
- Muscle spasms [30][10]
- Facial dysmorphism: Usually MDS-related high forehead, small jaw, short upturned nose, protuberant upper lip and bitemporal hollowing. [31][32]
- Microcephaly: If the brain size is ≥2.5 standard deviations below average for age and gender in LIS cases, it is called micro-lissencephaly. [7]
- Macrocephaly [20]
- Feeding difficulties such as dysphagia [33][10]
- Low weight for age [20]
Diagnostic Procedures[edit | edit source]
Prenatal diagnosis is usually possible after 27 weeks of gestation with fetal Magnetic Resonance Imaging (MRI) or Ultrasound. [34] In the postnatal period, MRI is a reliable diagnostic method. [1]
Alongside neuroimaging methods, genetic testing is highly recommended as a modern diagnostic tool. [1] Considering that 31 genes providing almost 90% diagnostic yield associated with lissencephaly have been identified so far, [1] it is important in terms of prenatal diagnosis, prognostic information, risk of recurrence in the family, avoidance of unnecessary research, and personalized medicine. [2][7]
Outcome Measures[edit | edit source]
To measure the severity of impairment in classical lissencephaly and SBH, the 6-point grading system ranging from severe grade 1 (complete agyria) to mild grade 6 (SBH only) modified from Dobyns and Truwit [35] is developed.
Management[edit | edit source]
Clinical management is carried out by a multidisciplinary team. There is no specific treatment for LIS, treatment is individual and based on symptoms. [1] In this sense, some of the elements that can be included in the treatment are as follows:
- Medication
- Physiotheraphy
- Occupational therapy
- Speech and swallowing therapy
Differential Diagnosis[edit | edit source]
During MRI analysis, lissencephaly needs to be well differentiated from other malformations of cortical developments (especially cobblestone and polymicrogyria). [1] Even a recent study [36] advocates that although Cobblestone malformation is often referred to as type 2 lissencephaly, this term should not be used due to its different pathological mechanisms. On the other hand, polymicrogyria is a characteristic malformation of schizencephaly and they were put together in a category of the classification system for malformations of cortical development [24].
In addition, major brain abnormalities (e.g., severe congenital microcephaly, agenesis of the corpus callosum, or cerebellar hypoplasia) are not found in classical LIS. [24] And compared to MDS, the face is less dysmorphic, and extracerebral malformations such as heart defects, omphalocele, cleft palate and genital anomalies, which are occasionally reported in MDS, are not generally encountered. [2]
Resources[edit | edit source]
- Lissencephaly Foundation Inc | USA
- An interview video of a child with lissencephaly by 'Special Books by Special Kids'.
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 Koenig M, Dobyns WB, Di Donato N. Lissencephaly: Update on diagnostics and clinical management. European Journal of Paediatric Neurology. 2021 Nov 1;35:147-52.
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 Fry AE, Cushion TD, Pilz DT. The genetics of lissencephaly. InAmerican Journal of Medical Genetics Part C: Seminars in Medical Genetics 2014 Jun (Vol. 166, No. 2, pp. 198-210).
- ↑ Kattuoa M, Das J. Lissencephaly. Stat Pearls: Treasure Island, FL, USA. 2021.Available:https://www.ncbi.nlm.nih.gov/books/NBK560766/ (accessed 7.10.2023)
- ↑ Malinger G, Kidron D, Schreiber L, Ben‐Sira L, Hoffmann C, Lev D, Lerman‐Sagie T. Prenatal diagnosis of malformations of cortical development by dedicated neurosonography. Ultrasound in Obstetrics and Gynecology: The Official Journal of the International Society of Ultrasound in Obstetrics and Gynecology. 2007 Feb;29(2):178-91.
- ↑ 5.0 5.1 5.2 5.3 5.4 Fernández V, Llinares‐Benadero C, Borrell V. Cerebral cortex expansion and folding: what have we learned?. The EMBO journal. 2016 May 17;35(10):1021-44.
- ↑ Herrera JF, Ramírez RG, Zárate MD. Lisencefalia tipo I: síndrome de Miller-Dieker. Informe de un caso. Revista Mexicana de Pediatría. 1999;66(4):157-60.
- ↑ 7.0 7.1 7.2 7.3 7.4 7.5 7.6 Juric-Sekhar G, Hevner RF. Malformations of cerebral cortex development: molecules and mechanisms. Annual Review of Pathology: Mechanisms of Disease. 2019 Jan 24;14:293-318.
- ↑ Shenoy AM, Markowitz JA, Bonnemann CG, Krishnamoorthy K, Bossler AD, Tseng BS. Muscle-eye-brain disease. Journal of clinical neuromuscular disease. 2010 Mar;11(3):124.
- ↑ Angelini C, Angelini C. Fukuyama congenital muscular dystrophy: walker-warburg syndrome. Springer International Publishing; 2018.
- ↑ 10.0 10.1 10.2 10.3 10.4 Javed K, Reddy V, Lui F. Neuroanatomy, cerebral cortex [Internet]. Treasure Island.
- ↑ Azevedo FA, Carvalho LR, Grinberg LT, Farfel JM, Ferretti RE, Leite RE, Filho WJ, Lent R, Herculano‐Houzel S. Equal numbers of neuronal and nonneuronal cells make the human brain an isometrically scaled‐up primate brain. Journal of Comparative Neurology. 2009 Apr 10;513(5):532-41.
- ↑ 12.0 12.1 Cadwell CR, Bhaduri A, Mostajo-Radji MA, Keefe MG, Nowakowski TJ. Development and arealization of the cerebral cortex. Neuron. 2019 Sep 25;103(6):980-1004.
- ↑ 13.0 13.1 13.2 Quezada S, Castillo‐Melendez M, Walker DW, Tolcos M. Development of the cerebral cortex and the effect of the intrauterine environment. The Journal of physiology. 2018 Dec;596(23):5665-74.
- ↑ Agirman G, Broix L, Nguyen L. Cerebral cortex development: an outside‐in perspective. FEBS letters. 2017 Dec;591(24):3978-92.
- ↑ Welker W. Why does cerebral cortex fissure and fold? A review of determinants of gyri and sulci. Cerebral Cortex: comparative structure and evolution of Cerebral Cortex, Part II. 1990:3-136.
- ↑ Raznahan A, Shaw P, Lalonde F, Stockman M, Wallace GL, Greenstein D, Clasen L, Gogtay N, Giedd JN. How does your cortex grow?. Journal of Neuroscience. 2011 May 11;31(19):7174-7.
- ↑ Stiles J, Jernigan TL. The basics of brain development. Neuropsychology review. 2010 Dec;20(4):327-48.
- ↑ Reiner O, Carrozzo R, Shen Y, Wehnert M, Faustinella F, Dobyns WB, Caskey CT, Ledbetter DH. Isolation of a Miller–Dicker lissencephaly gene containing G protein β-subunit-like repeats. Nature. 1993 Aug 19;364(6439):717-21.
- ↑ Chang BS. Tubulinopathies and their brain malformation syndromes: every TUB on its own bottom: the phenotypic Spectrum of Tubulinopathies. Epilepsy Currents. 2015 Mar;15(2):65-7.
- ↑ 20.0 20.1 20.2 20.3 20.4 Lapo-Córdova NS, Ruiz-García M, Hernández-Antúnez BG. Lissencephaly: Clinical and neuroimaging features in children. Revista mexicana de neurociencia. 2021 Aug;22(4):134-40.
- ↑ Brown WR. Association of preterm birth with brain malformations. Pediatric research. 2009 Jun;65(6):642-6.
- ↑ Wynshaw-Boris A, Pramparo T, Youn YH, Hirotsune S. Lissencephaly: mechanistic insights from animal models and potential therapeutic strategies. InSeminars in cell & developmental biology 2010 Oct 1 (Vol. 21, No. 8, pp. 823-830). Academic Press.
- ↑ Golden JA, Harding BN. Developmental neuropathology. (No Title). 2004.
- ↑ 24.0 24.1 24.2 Barkovich AJ, Guerrini R, Kuzniecky RI, Jackson GD, Dobyns WB. A developmental and genetic classification for malformations of cortical development: update 2012. Brain. 2012 May 1;135(5):1348-69.
- ↑ Barkovich AJ, Kuzniecky RI, Dobyns WB. Radiologic classification of malformations of cortical development. Current opinion in neurology. 2001 Apr 1;14(2):145-9.
- ↑ Ross ME, Walsh CA. Human brain malformations and their lessons for neuronal migration. Annual review of neuroscience. 2001 Mar;24(1):1041-70.
- ↑ Barkovich AJ, Dobyns WB, Guerrini R. Malformations of cortical development and epilepsy. Cold Spring Harbor perspectives in medicine. 2015 May 1;5(5):a022392.
- ↑ Van Reeuwijk J, Brunner HG, Van Bokhoven H. Glyc‐O‐genetics of Walker–Warburg syndrome. Clinical genetics. 2005 Apr;67(4):281-9.
- ↑ Dobyns WB. The clinical patterns and molecular genetics of lissencephaly and subcortical band heterotopia. Epilepsia. 2010 Feb;51:5-9.
- ↑ Saillour Y, Carion N, Quelin C, Leger PL, Boddaert N, Elie C, Toutain A, Mercier S, Barthez MA, Milh M, Joriot S. LIS1-related isolated lissencephaly: spectrum of mutations and relationships with malformation severity. Archives of neurology. 2009 Aug 1;66(8):1007-15.
- ↑ Dobyns WB, Curry CJ, Hoyme HE, Turlington L, Ledbetter DH. Clinical and molecular diagnosis of Miller-Dieker syndrome. American journal of human genetics. 1991 Mar;48(3):584.
- ↑ Cardoso C, Leventer RJ, Ward HL, Toyo-Oka K, Chung J, Gross A, Martin CL, Allanson J, Pilz DT, Olney AH, Mutchinick OM. Refinement of a 400-kb critical region allows genotypic differentiation between isolated lissencephaly, Miller-Dieker syndrome, and other phenotypes secondary to deletions of 17p13. 3. The American Journal of Human Genetics. 2003 Apr 1;72(4):918-30.
- ↑ Kolbjer S, Martin DA, Pettersson M, Dahlin M, Anderlid BM. Lissencephaly in an epilepsy cohort: Molecular, radiological and clinical aspects. European Journal of paediatric neurology. 2021 Jan 1;30:71-81.
- ↑ Malinger G, Kidron D, Schreiber L, Ben‐Sira L, Hoffmann C, Lev D, Lerman‐Sagie T. Prenatal diagnosis of malformations of cortical development by dedicated neurosonography. Ultrasound in Obstetrics and Gynecology: The Official Journal of the International Society of Ultrasound in Obstetrics and Gynecology. 2007 Feb;29(2):178-91.
- ↑ Dobyns WB, Truwit CL. Lissencephaly and other malformations of cortical development: 1995 update. Neuropediatrics. 1995 Jun;26(03):132-47.
- ↑ Mohamed K, Bakry M, Elmalik EE, Bayoumi MA. Lissencephaly causing refractory neonatal seizures in a term neonate. BMJ Case Reports. 2022 May 1;15(5):e249245.
- ↑ Special Books by Special Kids. Living with a Smooth Brain (Lissencephaly). Available from: https://www.youtube.com/watch?v=j0H5qoC9GYw