Hypomagnesemia: Difference between revisions
No edit summary |
Kim Jackson (talk | contribs) (Removed case studies as all links were directed to a University site and were unaccessible) |
||
| (18 intermediate revisions by 2 users not shown) | |||
| Line 1: | Line 1: | ||
| | ||
<div class="editorbox"> | <div class="editorbox"> | ||
'''Original Editors '''-Shawn Abraham & Sean Joyce- [[Pathophysiology of Complex Patient Problems|Students from Bellarmine University's Pathophysiology of Complex Patient Problems project.]] | '''Original Editors '''- [[User:Shawn Abraham|Shawn Abraham]] & [[User:Sean Joyce|Sean Joyce]]- [[Pathophysiology of Complex Patient Problems|Students from Bellarmine University's Pathophysiology of Complex Patient Problems project.]] | ||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | ||
</div> | </div> | ||
== Definition/Description == | == Definition/Description == | ||
[[File:Mg-TableImage.png|right|frameless|334x334px]] | |||
Hypomagnesemia is an electrolyte imbalance with inadequate levels of magnesium in the bloodstream<ref name="Office">Office of Dietary Supplements - Magnesium [Internet]. Ods.od.nih.gov. 2016 [cited 5 April 2016]. Available from: https://ods.od.nih.gov/factsheets/Magnesium-HealthProfessional/</ref>. Magnesium (Mg) is a principal cation (ie an [[Electrolytes|electrolyte]]) in the intracellular fluid that is an essential part of many enzyme systems associated with energy metabolism.<ref name="West">West MPaz J. Acute Care Handbook for Physical Therapists (Fourth Edition). Elsevier Health Sciences; 2013.</ref> | |||
Magnesium | Magnesium | ||
* Acts as a natural calcium blocker, helping your muscle cells relax after contracting. When magnesium levels are low, your muscles may contract too much and cause symptoms such as cramps or muscle spasms. | |||
* Helps your heart muscle cells relax by countering calcium, which stimulates contractions. These minerals compete with each other to ensure heart cells contract and relax properly. | |||
* Acts as the gatekeeper for NMDA receptors, which are involved in healthy brain development, memory and learning. It prevents nerve cells from being overstimulated, which can kill them and may cause brain damage. | |||
Higher magnesium intakes have been linked to health benefits such as a lower risk of heart disease, fewer migraines, reduced symptoms of depression and improved blood pressure, blood sugar levels and sleep.<ref name=":1" /> | |||
Certain medical conditions and medications can cause excessive loss of magnesium resulting in deficiency.<ref name="Goodman">Goodman C, Snyder T. Differential diagnosis for physical therapists. St. Louis, Mo.: Saunders/Elsevier; 2007.</ref><ref name="File">File:Mg-TableImage.png - Wikimedia Commons [Internet]. Commons.wikimedia.org. 2016 [cited 7 April 2016]. Available from: https://commons.wikimedia.org/wiki/File:Mg-TableImage.png#filelinks</ref> | |||
[[ | Subclinical magnesium deficiency is a common and under-recognised problem throughout the world. | ||
* Does not manifest as clinically apparent symptoms and thus is not easily recognised by the clinician | |||
* Likely leads to hypertension, arrhythmias, arterial calcifications, atherosclerosis, heart failure and an increased risk for thrombosis. | |||
* Is a principal, yet under-recognised, driver of cardiovascular disease<ref name=":2">DiNicolantonio JJ, O’Keefe JH, Wilson W. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5786912/ Subclinical magnesium deficiency: a principal driver of cardiovascular disease and a public health crisis]. Open heart. 2018 Jan 1;5(1):e000668.Available from:https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5786912/ (accessed 17.11.2020)</ref>. | |||
* Higher magnesium intakes have been linked to health benefits such as a lower risk of heart disease, fewer migraines, reduced symptoms of depression and improved blood pressure, blood sugar levels and sleep.<ref name=":1">Healthline [https://www.healthline.com/nutrition/what-does-magnesium-do#dietary-sources Magnesium and your body] Available from:https://www.healthline.com/nutrition/what-does-magnesium-do#dietary-sources (last accessed 17.11.2020)</ref> | |||
== Etiology == | |||
Hypomagnesemia can be: | |||
* Secondary to decreased intake, as seen in: Starvation; Alcohol use disorder (alcohol acts acutely as a Mg diuretic, causing a prompt, vigorous increase in the urinary excretion of Mg, Second, and the body stores of Mg become depleted)<ref>Rivlin RS. [https://pubmed.ncbi.nlm.nih.gov/7836619/ Magnesium deficiency and alcohol intake: mechanisms, clinical significance and possible relation to cancer development (a review)]. Journal of the American College of Nutrition. 1994 Oct 1;13(5):416-23.Available from;https://pubmed.ncbi.nlm.nih.gov/7836619/ (last accessed 17.11.2020)</ref>; Critically ill patients who are receiving total parenteral nutrition (ie intravenous feeding, is a method of getting nutrition into the body through the veins). | |||
* Secondary to the following medications: Loop and thiazide [[Diuretics in the Treatment of Hypertension|diuretics]]; Proton pump inhibitors (a group of drugs that reduce the secretion of gastric acid); Aminoglycoside antibiotics (any of a group of antibacterial antibiotics derived from species of Streptomyces); Amphotericin B (an antifungal medication used for serious fungal infections and leishmaniasis); [[Glycosides and Congestive Heart Failure|Digitalis]]; [[Chemotherapy Side Effects and Syndromes|Chemotherapeutic drugs]]. | |||
* Induced by gastrointestinal and/or renal losses, including but not limited to the following conditions: Acute diarrhea; Chronic diarrhea ([[Crohn's Disease|Crohn]] disease, ulcerative colitis); Hungry bone syndrome; Acute [[pancreatitis]]; [[Management of Obesity|Gastric bypass surgery]]<ref name=":0">Gragossian A, Friede R. [https://www.ncbi.nlm.nih.gov/books/NBK500003/ Hypomagnesemia].6.9.2020 Available from:https://www.ncbi.nlm.nih.gov/books/NBK500003/ (last accessed 16.11.2020)</ref>. | |||
== | == Epidemiology == | ||
[[File:FoodSourcesOfMagnesium.jpg|right|frameless]] | |||
The risk of hypomagnesemia depends on multiple characteristics in various healthcare settings, with the following being the latest incidences: | |||
* 2% in the general population | |||
*2% in the general population | * 10% to 20% in hospitalized patients | ||
*10 | * 50% to 60% in intensive care unit patients | ||
*50 | * 30% to 80% in persons with [[Alcoholism|alcohol]] use disorder | ||
*30 | * 25% in outpatients with [[diabetes]] | ||
*25% in outpatients with diabetes | Hypomagnesemia is a relatively common occurrence in clinical medicine. That it often goes unrecognized is due to the fact that magnesium levels are rarely evaluated since few clinicians are aware of the many clinical states in which deficiency or excess, of this ion may occur’<ref name=":2" />.<ref name=":0" /> | ||
* Since 1940 there has been a tremendous decline in the micronutrient density of foods. eg loss of magnesium during food refining/processing is significant: white flour (−82%), polished rice (−83%), starch (−97%) and white sugar (−99%); Magnesium deficiency in plants is becoming an increasingly severe problem with the development of industry and agriculture and the increase in human population.Processed foods, fat, refined flour and sugars are all devoid of magnesium, and thus our Western diet predisposes us to magnesium deficiency.<ref name=":2" /> | |||
<ref name=" | * Image: Food rich in Mg | ||
< | |||
== Characteristics/Clinical Presentation == | == Characteristics/Clinical Presentation == | ||
Patients with symptomatic magnesium depletion can present in many ways. The major clinical manifestations include neuromuscular and cardiovascular manifestations and other electrolyte abnormalities.<ref name=":0" /> | |||
Early signs of low magnesium include: | |||
* nausea | |||
* vomiting | |||
* weakness | |||
* decreased appetite | |||
As magnesium deficiency worsens, symptoms may include: | |||
* numbness | |||
* tingling | |||
* muscle cramps | |||
* seizures | |||
* muscle spasticity | |||
* personality changes | |||
* abnormal heart rhythms<ref>Healthline Hypomagnesemia (Low Magnesium) Available from:https://www.healthline.com/health/hypomagnesemia#symptoms (last accessed 17.11.2020)</ref><ref name="Goodman" /><ref name="Updated">Updated by: Laura J. Martin a. Low magnesium level: MedlinePlus Medical Encyclopedia [Internet]. Nlm.nih.gov. 2016 [cited 5 April 2016]. Available from: https://www.nlm.nih.gov/medlineplus/ency/article/000315.htm</ref><ref name="Martin">Martin K, Gonzalez E, Slatopolsky E. Clinical Consequences and Management of Hypomagnesemia. Journal of the American Society of Nephrology. 2008;20(11):2291-2295.</ref> | |||
< | |||
== | == Treatment == | ||
[[File:Magnesium Sulfate IV 1.jpg|right|frameless]] | |||
Magnesium deficiency is commonly encountered in clinical practice. The key is to find the primary cause. | |||
* Asymptomatic patients can be managed with supplements prescribed as outpatients. | |||
* Symptomatic patients need admission and parenteral magnesium. The prognosis for most patients with a reversible cause is excellent. | |||
It is important to treat hypomagnesemia. Dangerously low levels of magnesium have the potential to cause fatal cardiac arrhythmias. Moreover, hypomagnesemia in patients with acute myocardial infarction puts them at higher risk of ventricular arrhythmias within the first 24 hours. | |||
Clinicians, nurses, and pharmacists must coordinate care to find a rapid resolution to magnesium deficiency. This often involves education of the patient, family, and a team approach from the health practitioners. | |||
== | Patients with hypomagnesemia should be encouraged to eat the following foods: | ||
* Green vegetables, such as spinach | |||
* Beans | |||
* Peas | |||
* Nuts | |||
* Seeds | |||
* Unrefined grains<ref name=":0" /> | |||
* Dark chocolate<ref name=":2" />. | |||
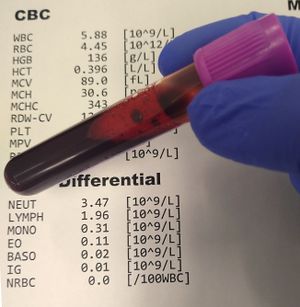
== Diagnosis == | |||
[[File:Blood test.jpg|right|frameless]] | |||
Diagnosis is based on a physical exam, symptoms, medical history, and a [[Blood Tests|blood test]]. | |||
A blood magnesium level doesn’t tell you the amount of magnesium your body has stored in your bones and muscle tissue, however it’s still helpful for indicating whether you have hypomagnesemia. Blood test include blood calcium and potassium levels. | |||
* A normal serum (blood) magnesium level is 1.8 to 2.2 milligrams per deciliter (mg/dL). Serum magnesium lower than 1.8 mg/dL is considered low. A magnesium level below 1.25 mg/dL is considered very severe hypomagnesemia. | |||
* The average adult holds approximately 25 g magnesium. 50% to 60% is found in the [[Bone|bones]] and most of the rest is found in soft tissue, the remaining less than 1% of magnesium is found in [[Blood Physiology|blood serum]]. Normal serum magnesium levels fall between 0.75 and 0.95 mmol/L. Hypomagnesemia is characterized as serum levels falling below 0.75 mmol/L.<ref name="Office" /> | |||
== Systemic Involvement == | == Systemic Involvement == | ||
Hypomagnesemia has a systemic link to other electrolyte deficiencies, especially hypokalemia and hypocalcemia. | Hypomagnesemia has a systemic link to other electrolyte deficiencies, especially hypokalemia and [[Hypocalcemia|hypocalcemia.]] | ||
# [[Hypokalemia]] has been found to occur in 40-60% of cases of hypomagnesemia cases (related to underlying disorders that cause magnesium and potassium losses eg diuretic therapy and diarrhea). | |||
Hypokalemia has been found to occur in 40-60% of cases of hypomagnesemia cases | 2. [[Hypocalcemia]].<ref name="Hypomagnesemia">Hypomagnesemia Differential Diagnoses [Internet]. Emedicine.medscape.com. 2016 [cited 7 April 2016]. Available from: http://emedicine.medscape.com/article/2038394-differential</ref> | ||
== Physical Therapy Management == | |||
<ref name="Hypomagnesemia" / | |||
<ref | |||
== Physical Therapy Management | |||
There are no direct physical therapy interventions for hypomagnesemia. Patient will be referred to physical therapy for treatment of impairments that may be a cause of hypomagnesemia such as decline in muscle strength, fatigue, or abnormal eye movements. (See Clinical Presentation) | There are no direct physical therapy interventions for hypomagnesemia. Patient will be referred to physical therapy for treatment of impairments that may be a cause of hypomagnesemia such as decline in muscle strength, fatigue, or abnormal eye movements. (See Clinical Presentation) | ||
| Line 127: | Line 95: | ||
*Foods high in magnesium | *Foods high in magnesium | ||
*Importance of following medical recommendations for magnesium intake< | *Importance of following medical recommendations for magnesium intake | ||
A frequently asked question relates to magnesium and leg cramps. Inform the client that despite the availability of a vast number of medications, their efficacy is low and unpredictable. Educate patients on proper [[Dehydration|hydration]] and [[stretching]] prior to any [[Physical Activity|physical activity]]. In addition, the patient's electrolyte status should be normal.<ref>Miller TM, Layzer RB. [https://www.statpearls.com/articlelibrary/viewarticle/25384/ Muscle cramps]. Muscle & Nerve: Official Journal of the American Association of Electrodiagnostic Medicine. 2005 Oct;32(4):431-42.Available from:https://www.statpearls.com/articlelibrary/viewarticle/25384/ (last accessed 17.11.2020)</ref> | |||
== | == Facts about Magnesium Deficiency == | ||
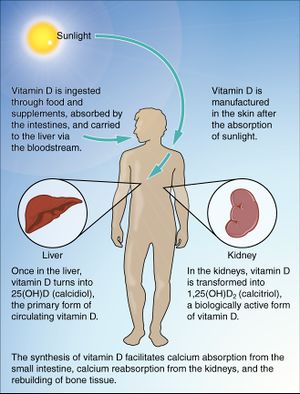
*[[File:Vitamin D.jpg|right|frameless]]Your body absorbs up to 30 percent less magnesium from foods as you age. | |||
* [[Smoking Cessation and Brief Intervention|Smoking]] and alcohol use reduce magnesium levels. | |||
* Processed foods have lower levels of magnesium. | |||
* Many common drugs, such as statins and antacids, reduce magnesium absorption. | |||
* Low [[Vitamin D Deficiency|vitamin D]] levels reduce absorption of magnesium.<ref name=":1" /> | |||
* Magnesium is widely used to treat leg cramps, particularly in Latin America and Europe. But almost all of the many clinical studies of magnesium treatment for cramps found it to be ineffective.<ref name=":1" /> | |||
<br> | |||
== Resources == | == Resources == | ||
[https://ods.od.nih.gov/factsheets/Magnesium-HealthProfessional | [https://ods.od.nih.gov/factsheets/Magnesium-HealthProfessional/ Magnesium Fact Sheet for Health Professionals (NIH)]<br> | ||
{{#ev:youtube|45DeOCSyGYU}} | {{#ev:youtube|45DeOCSyGYU}} | ||
Latest revision as of 17:32, 30 November 2020
Original Editors - Shawn Abraham & Sean Joyce- Students from Bellarmine University's Pathophysiology of Complex Patient Problems project.
Top Contributors - Shawn Abraham, Sean Joyce, Lucinda hampton, Kim Jackson, Elaine Lonnemann, Selena Horner, 127.0.0.1 and WikiSysop
Definition/Description[edit | edit source]
Hypomagnesemia is an electrolyte imbalance with inadequate levels of magnesium in the bloodstream[1]. Magnesium (Mg) is a principal cation (ie an electrolyte) in the intracellular fluid that is an essential part of many enzyme systems associated with energy metabolism.[2]
Magnesium
- Acts as a natural calcium blocker, helping your muscle cells relax after contracting. When magnesium levels are low, your muscles may contract too much and cause symptoms such as cramps or muscle spasms.
- Helps your heart muscle cells relax by countering calcium, which stimulates contractions. These minerals compete with each other to ensure heart cells contract and relax properly.
- Acts as the gatekeeper for NMDA receptors, which are involved in healthy brain development, memory and learning. It prevents nerve cells from being overstimulated, which can kill them and may cause brain damage.
Higher magnesium intakes have been linked to health benefits such as a lower risk of heart disease, fewer migraines, reduced symptoms of depression and improved blood pressure, blood sugar levels and sleep.[3]
Certain medical conditions and medications can cause excessive loss of magnesium resulting in deficiency.[4][5]
Subclinical magnesium deficiency is a common and under-recognised problem throughout the world.
- Does not manifest as clinically apparent symptoms and thus is not easily recognised by the clinician
- Likely leads to hypertension, arrhythmias, arterial calcifications, atherosclerosis, heart failure and an increased risk for thrombosis.
- Is a principal, yet under-recognised, driver of cardiovascular disease[6].
- Higher magnesium intakes have been linked to health benefits such as a lower risk of heart disease, fewer migraines, reduced symptoms of depression and improved blood pressure, blood sugar levels and sleep.[3]
Etiology[edit | edit source]
Hypomagnesemia can be:
- Secondary to decreased intake, as seen in: Starvation; Alcohol use disorder (alcohol acts acutely as a Mg diuretic, causing a prompt, vigorous increase in the urinary excretion of Mg, Second, and the body stores of Mg become depleted)[7]; Critically ill patients who are receiving total parenteral nutrition (ie intravenous feeding, is a method of getting nutrition into the body through the veins).
- Secondary to the following medications: Loop and thiazide diuretics; Proton pump inhibitors (a group of drugs that reduce the secretion of gastric acid); Aminoglycoside antibiotics (any of a group of antibacterial antibiotics derived from species of Streptomyces); Amphotericin B (an antifungal medication used for serious fungal infections and leishmaniasis); Digitalis; Chemotherapeutic drugs.
- Induced by gastrointestinal and/or renal losses, including but not limited to the following conditions: Acute diarrhea; Chronic diarrhea (Crohn disease, ulcerative colitis); Hungry bone syndrome; Acute pancreatitis; Gastric bypass surgery[8].
Epidemiology[edit | edit source]
The risk of hypomagnesemia depends on multiple characteristics in various healthcare settings, with the following being the latest incidences:
- 2% in the general population
- 10% to 20% in hospitalized patients
- 50% to 60% in intensive care unit patients
- 30% to 80% in persons with alcohol use disorder
- 25% in outpatients with diabetes
Hypomagnesemia is a relatively common occurrence in clinical medicine. That it often goes unrecognized is due to the fact that magnesium levels are rarely evaluated since few clinicians are aware of the many clinical states in which deficiency or excess, of this ion may occur’[6].[8]
- Since 1940 there has been a tremendous decline in the micronutrient density of foods. eg loss of magnesium during food refining/processing is significant: white flour (−82%), polished rice (−83%), starch (−97%) and white sugar (−99%); Magnesium deficiency in plants is becoming an increasingly severe problem with the development of industry and agriculture and the increase in human population.Processed foods, fat, refined flour and sugars are all devoid of magnesium, and thus our Western diet predisposes us to magnesium deficiency.[6]
- Image: Food rich in Mg
Characteristics/Clinical Presentation[edit | edit source]
Patients with symptomatic magnesium depletion can present in many ways. The major clinical manifestations include neuromuscular and cardiovascular manifestations and other electrolyte abnormalities.[8]
Early signs of low magnesium include:
- nausea
- vomiting
- weakness
- decreased appetite
As magnesium deficiency worsens, symptoms may include:
- numbness
- tingling
- muscle cramps
- seizures
- muscle spasticity
- personality changes
- abnormal heart rhythms[9][4][10][11]
Treatment[edit | edit source]
Magnesium deficiency is commonly encountered in clinical practice. The key is to find the primary cause.
- Asymptomatic patients can be managed with supplements prescribed as outpatients.
- Symptomatic patients need admission and parenteral magnesium. The prognosis for most patients with a reversible cause is excellent.
It is important to treat hypomagnesemia. Dangerously low levels of magnesium have the potential to cause fatal cardiac arrhythmias. Moreover, hypomagnesemia in patients with acute myocardial infarction puts them at higher risk of ventricular arrhythmias within the first 24 hours.
Clinicians, nurses, and pharmacists must coordinate care to find a rapid resolution to magnesium deficiency. This often involves education of the patient, family, and a team approach from the health practitioners.
Patients with hypomagnesemia should be encouraged to eat the following foods:
Diagnosis[edit | edit source]
Diagnosis is based on a physical exam, symptoms, medical history, and a blood test.
A blood magnesium level doesn’t tell you the amount of magnesium your body has stored in your bones and muscle tissue, however it’s still helpful for indicating whether you have hypomagnesemia. Blood test include blood calcium and potassium levels.
- A normal serum (blood) magnesium level is 1.8 to 2.2 milligrams per deciliter (mg/dL). Serum magnesium lower than 1.8 mg/dL is considered low. A magnesium level below 1.25 mg/dL is considered very severe hypomagnesemia.
- The average adult holds approximately 25 g magnesium. 50% to 60% is found in the bones and most of the rest is found in soft tissue, the remaining less than 1% of magnesium is found in blood serum. Normal serum magnesium levels fall between 0.75 and 0.95 mmol/L. Hypomagnesemia is characterized as serum levels falling below 0.75 mmol/L.[1]
Systemic Involvement[edit | edit source]
Hypomagnesemia has a systemic link to other electrolyte deficiencies, especially hypokalemia and hypocalcemia.
- Hypokalemia has been found to occur in 40-60% of cases of hypomagnesemia cases (related to underlying disorders that cause magnesium and potassium losses eg diuretic therapy and diarrhea).
2. Hypocalcemia.[12]
Physical Therapy Management[edit | edit source]
There are no direct physical therapy interventions for hypomagnesemia. Patient will be referred to physical therapy for treatment of impairments that may be a cause of hypomagnesemia such as decline in muscle strength, fatigue, or abnormal eye movements. (See Clinical Presentation)
Physical therapists can take a team approach with medical management through patient education on:
- Foods high in magnesium
- Importance of following medical recommendations for magnesium intake
A frequently asked question relates to magnesium and leg cramps. Inform the client that despite the availability of a vast number of medications, their efficacy is low and unpredictable. Educate patients on proper hydration and stretching prior to any physical activity. In addition, the patient's electrolyte status should be normal.[13]
Facts about Magnesium Deficiency[edit | edit source]
- Your body absorbs up to 30 percent less magnesium from foods as you age.
- Smoking and alcohol use reduce magnesium levels.
- Processed foods have lower levels of magnesium.
- Many common drugs, such as statins and antacids, reduce magnesium absorption.
- Low vitamin D levels reduce absorption of magnesium.[3]
- Magnesium is widely used to treat leg cramps, particularly in Latin America and Europe. But almost all of the many clinical studies of magnesium treatment for cramps found it to be ineffective.[3]
Resources[edit | edit source]
Magnesium Fact Sheet for Health Professionals (NIH)
[12]- Informational video on Hypomagnesemia
References[edit | edit source]
- ↑ 1.0 1.1 Office of Dietary Supplements - Magnesium [Internet]. Ods.od.nih.gov. 2016 [cited 5 April 2016]. Available from: https://ods.od.nih.gov/factsheets/Magnesium-HealthProfessional/
- ↑ West MPaz J. Acute Care Handbook for Physical Therapists (Fourth Edition). Elsevier Health Sciences; 2013.
- ↑ 3.0 3.1 3.2 3.3 Healthline Magnesium and your body Available from:https://www.healthline.com/nutrition/what-does-magnesium-do#dietary-sources (last accessed 17.11.2020)
- ↑ 4.0 4.1 Goodman C, Snyder T. Differential diagnosis for physical therapists. St. Louis, Mo.: Saunders/Elsevier; 2007.
- ↑ File:Mg-TableImage.png - Wikimedia Commons [Internet]. Commons.wikimedia.org. 2016 [cited 7 April 2016]. Available from: https://commons.wikimedia.org/wiki/File:Mg-TableImage.png#filelinks
- ↑ 6.0 6.1 6.2 6.3 DiNicolantonio JJ, O’Keefe JH, Wilson W. Subclinical magnesium deficiency: a principal driver of cardiovascular disease and a public health crisis. Open heart. 2018 Jan 1;5(1):e000668.Available from:https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5786912/ (accessed 17.11.2020)
- ↑ Rivlin RS. Magnesium deficiency and alcohol intake: mechanisms, clinical significance and possible relation to cancer development (a review). Journal of the American College of Nutrition. 1994 Oct 1;13(5):416-23.Available from;https://pubmed.ncbi.nlm.nih.gov/7836619/ (last accessed 17.11.2020)
- ↑ 8.0 8.1 8.2 8.3 Gragossian A, Friede R. Hypomagnesemia.6.9.2020 Available from:https://www.ncbi.nlm.nih.gov/books/NBK500003/ (last accessed 16.11.2020)
- ↑ Healthline Hypomagnesemia (Low Magnesium) Available from:https://www.healthline.com/health/hypomagnesemia#symptoms (last accessed 17.11.2020)
- ↑ Updated by: Laura J. Martin a. Low magnesium level: MedlinePlus Medical Encyclopedia [Internet]. Nlm.nih.gov. 2016 [cited 5 April 2016]. Available from: https://www.nlm.nih.gov/medlineplus/ency/article/000315.htm
- ↑ Martin K, Gonzalez E, Slatopolsky E. Clinical Consequences and Management of Hypomagnesemia. Journal of the American Society of Nephrology. 2008;20(11):2291-2295.
- ↑ 12.0 12.1 Hypomagnesemia Differential Diagnoses [Internet]. Emedicine.medscape.com. 2016 [cited 7 April 2016]. Available from: http://emedicine.medscape.com/article/2038394-differential
- ↑ Miller TM, Layzer RB. Muscle cramps. Muscle & Nerve: Official Journal of the American Association of Electrodiagnostic Medicine. 2005 Oct;32(4):431-42.Available from:https://www.statpearls.com/articlelibrary/viewarticle/25384/ (last accessed 17.11.2020)