Gluteal Tendinopathy: Difference between revisions
No edit summary |
|||
| Line 37: | Line 37: | ||
Lateral hip pain caused by tendinopathy may be challenging to diagnose because of the long list of referred pain possibilities<ref name=":0" />. | Lateral hip pain caused by tendinopathy may be challenging to diagnose because of the long list of referred pain possibilities<ref name=":0" />. | ||
Pain is the main characteristic of GT, frequently insidious, gradually worsens with time and with different loads and tasks<ref>Lequesne M. From “periarthritis” to hip “rotator cuff” tears. Trochanteric tendinobursitis. Joint Bone Spine. 2006;4(73):344-8.</ref>. The pain might be significant after a strong guarding contraction of the adductors during a slip or fall. It gets worse at | Pain is the main characteristic of GT, frequently insidious, gradually worsens with time and with different loads and tasks<ref>Lequesne M. From “periarthritis” to hip “rotator cuff” tears. Trochanteric tendinobursitis. Joint Bone Spine. 2006;4(73):344-8.</ref>. The pain might be significant after a strong guarding contraction of the adductors during a slip or fall. It gets worse at night and sleeping on the affected side worsens the symptoms<ref>Connell DA, Bass C, Sykes CJ, Young D, Edwards E. Sonographic evaluation of gluteus medius and minimus tendinopathy. European radiology. 2003 Jun 1;13(6):1339-47.</ref>, affecting the quality of sleeping. | ||
Assessing functional limitation and levels of discomfort is important. Patients usually report pain with single-loading tasks such as walking and stairs negotiation. Tasks that require active hip extension, such as sit to stand, are also accompanied with pain and stiffness. The latter is a mutual feature between GT and hip OA, however, patients with OA usually have difficulties manipulating shoes and socks (hip flexion) but this problem is not relevant with GT<ref name=":0" />. | Assessing functional limitation and levels of discomfort is important. Patients usually report pain with single-loading tasks such as walking and stairs negotiation. Tasks that require active hip extension, such as sit to stand, are also accompanied with pain and stiffness. The latter is a mutual feature between GT and hip OA, however, patients with OA usually have difficulties manipulating shoes and socks (hip flexion) but this problem is not relevant with GT<ref name=":0" />. | ||
== Diagnostic Procedures == | == Diagnostic Procedures == | ||
A thorough [[Hip Examination|hip examination]] is needed basically by obtaining patient's history to understand the nature of the symptoms and rule out Red Flags. Then, the assessor should go into PE with a hypothesis that to be confirmed with clinical tests. <u>The following tests,</u> although have weak diagnostic properties, are commonly used in MSK settings to confirm GT diagnosis: | A thorough [[Hip Examination|hip examination]] is needed basically by obtaining patient's history to understand the nature of the symptoms and rule out Red Flags. Then, the assessor should go into PE with a hypothesis that to be confirmed with clinical tests. <u>The following tests,</u> although have weak diagnostic properties, are commonly used in MSK settings to confirm GT diagnosis: | ||
* Ober's test | * [[Ober's Test|Ober's test]] | ||
* Single stance assessment for 30 sec: recommended over | * Single stance assessment for 30 sec: recommended over [[Trendelenburg Test|Trendelenberg's test]]. | ||
* Adduction/External Rotation with resistance | * Adduction/External Rotation with resistance | ||
* FABER test: the hip ROM is not limited in GT. | * [[FABER Test|FABER test]]: the hip ROM is not limited in GT. | ||
Pain provocation and reproduction of symptoms by loading abductors are the aims of these test. Assessing active abduction in a position of hip adduction may be more useful.Further provocation could be elicited by testing the glueal muscles internal rotation function at a 90 degree hip flexion and maximal external rotation<ref name=":0" />. The traditional Trendelenburg test was useful in diagnosing partial and complete abductor tendon<ref>Bird PA, Oakley SP, Shnier R, Kirkham BW. Prospective evaluation of magnetic resonance imaging and physical examination findings in patients with greater trochanteric pain syndrome. Arthritis & Rheumatism: Official Journal of the American College of Rheumatology. 2001 Sep;44(9):2138-45.</ref> tears at advanced stages of the pathology<ref name=":0" />. | Pain provocation and reproduction of symptoms by loading abductors are the aims of these test. Assessing active abduction in a position of hip adduction may be more useful.Further provocation could be elicited by testing the glueal muscles internal rotation function at a 90 degree hip flexion and maximal external rotation<ref name=":0" />. The traditional Trendelenburg test was useful in diagnosing partial and complete abductor tendon<ref>Bird PA, Oakley SP, Shnier R, Kirkham BW. Prospective evaluation of magnetic resonance imaging and physical examination findings in patients with greater trochanteric pain syndrome. Arthritis & Rheumatism: Official Journal of the American College of Rheumatology. 2001 Sep;44(9):2138-45.</ref> tears at advanced stages of the pathology<ref name=":0" />. | ||
| Line 66: | Line 64: | ||
The [https://www.researchgate.net/publication/304168478_Visa_G_with_scoring Victorian Institute of Sport Assessment-Gluteal tendon (VISA-G)] can be used to assess and track pain intensity and functional limitation<ref name=":2">Ganderton C, Semciw A, Cook J, Moreira E, Pizzari T. Gluteal Loading Versus Sham Exercises to Improve Pain and Dysfunction in Postmenopausal Women with Greater Trochanteric Pain Syndrome: A Randomized Controlled Trial. Journal of Women's Health. 2018 May 1.</ref>. | The [https://www.researchgate.net/publication/304168478_Visa_G_with_scoring Victorian Institute of Sport Assessment-Gluteal tendon (VISA-G)] can be used to assess and track pain intensity and functional limitation<ref name=":2">Ganderton C, Semciw A, Cook J, Moreira E, Pizzari T. Gluteal Loading Versus Sham Exercises to Improve Pain and Dysfunction in Postmenopausal Women with Greater Trochanteric Pain Syndrome: A Randomized Controlled Trial. Journal of Women's Health. 2018 May 1.</ref>. | ||
Cook and Purdam<ref>Cook JL, Purdam CR. The challenge of managing tendinopathy in competing athletes. Br J Sports Med. 2013 May 9:bjsports-2012.</ref> suggest functional loading tests to assess and track a tendon's response to therapy. Reduced pain on single leg standing and hopping indicates improved loading tolerance of the gluteal tendons. Longer standing time on one leg or increased number of hops to onset of pain reflect improvement. Inadequate eccentric pelvic control in single leg loading tasks indicates a greater hip adduction moment arm and possible gluteal tendons compression. Video analysis of is suggested for athletes to observe pelvic tilt and femoral adduction in running and changing direction<ref name=":0" />. | |||
{{#ev:youtube|k1hlY0EMYJw}}<ref>Video gait running analysis: alignment, issues, rear view. Available from: https://www.youtube.com/watch?v=k1hlY0EMYJw</ref> | {{#ev:youtube|k1hlY0EMYJw}}<ref>Video gait running analysis: alignment, issues, rear view. Available from: https://www.youtube.com/watch?v=k1hlY0EMYJw</ref> | ||
| Line 73: | Line 71: | ||
== Differential Diagnosis == | == Differential Diagnosis == | ||
[[Hip Osteoarthritis|Hip OA]] | * [[Hip Osteoarthritis|Hip OA]] | ||
* [[Avascular Necrosis]] | |||
[[Avascular Necrosis]] | * [[Femoroacetabular Impingement|Femoral-acetabular Impingement (FAI)]] | ||
* [[Greater Trochanteric Pain Syndrome|Greater Trochanter Pain Syndrome]] | |||
[[Femoroacetabular Impingement|Femoral-acetabular Impingement (FAI)]] | * [[Trochanteric Bursitis]] | ||
[[Greater Trochanteric Pain Syndrome|Greater Trochanter Pain Syndrome]] | |||
[[Trochanteric Bursitis]] | |||
== Management Strategies == | == Management Strategies == | ||
Tendon | Tendon [https://www.physio-pedia.com/Principles_of_Exercise_Rehabilitation#Re-loading_Rehabilitation.5B2.5D reloading principles] are suggested in managing tendonpathies in general<ref name=":0" /> <ref>Beyer R, Kongsgaard M, Hougs Kjær B, Øhlenschlæger T, Kjær M, Magnusson SP. Heavy slow resistance versus eccentric training as treatment for Achilles tendinopathy: a randomized controlled trial. The American journal of sports medicine. 2015 Jul;43(7):1704-11.</ref>. See [[Tendinopathy Rehabilitation|Tendon Rehabilitation]]. There are specific consideration when attempting to address GT. | ||
=== Load Management === | === Load Management === | ||
| Line 136: | Line 130: | ||
Removal of trochanteric bursae and ITB release is utilized in patients without gluteal tears. Studies report good to excellent short-medium term outcomes<ref>Craig RA, Gwynne Jones DP, Oakley AP, Dunbar JD. Iliotibial band Z‐lengthening for refractory trochanteric bursitis (greater trochanteric pain syndrome). ANZ journal of surgery. 2007 Nov;77(11):996-8.</ref>, however, most studies lacked control group and the rationale behind the mechanism of efficacy remains unclear<ref name=":0" />. | Removal of trochanteric bursae and ITB release is utilized in patients without gluteal tears. Studies report good to excellent short-medium term outcomes<ref>Craig RA, Gwynne Jones DP, Oakley AP, Dunbar JD. Iliotibial band Z‐lengthening for refractory trochanteric bursitis (greater trochanteric pain syndrome). ANZ journal of surgery. 2007 Nov;77(11):996-8.</ref>, however, most studies lacked control group and the rationale behind the mechanism of efficacy remains unclear<ref name=":0" />. | ||
== References == | == References == | ||
<references /> | <references /> | ||
Revision as of 07:56, 24 July 2018
Introduction[edit | edit source]
Gluteal Tendinopathy (GT) is defined as moderate to sever disabling pain over the Greater Trochanter (lateral hip pain). It is often referred to as Greater Trochanter Pain Syndrome (GTPS) and was traditionally diagnosed as Trochanteric Bursitis, however, recent research defines non-inflammatory tendinopathy of the gluteus medius(GMed) and/or gluteus minimus (GMin) muscles to be the main source of lateral hip pain[1].
This condition affects both athletes (particularly runners) and less active people[1]. One of four females over 50 years is likely to be affected by GT[2].
GT has significant impacts on the quality of life, with similar symptoms to those of hip OA. It interferes with sleep (side lying) and common weight bearing tasks[1].
Pathoanatomy/Pathomechanics[edit | edit source]
Tendon structure and loading capacity are influenced by mechanical loading which triggers physiological responses within the tendon. Under normal conditions, the tendon undergoes a cycle of balanced catabolic and anabolic processes. Changes in loading type, intensity or frequency disrupt this harmony. Eccentric contractions in outer ranges (when the muscle is active and the tendon is lengthening simultaneously) represent the greatest form of loading. Failure to adapt to loading, due to rapid increase in intensity and/or frequency with insufficient recovery time, results in a series of catabolic effects which in turn result in altering tenocyte behaviour, reducing load-bearing capacity and predisposing tendons to injury at relatively low tensile loads. A combination of both tensile loading and compression are found to be more damaging than either alone[3].
GMed and GMin tendons are subjected to compression due to several factors:
1- Joint position: the Iliotibial Band (ITB) presents a compressive force on gluteal tendons that magnifies as the hip moves into further adduction. Birnbaum et al. [4] reported a change from 4 to 106 N ITB compression as the angle of hip adduction increased from 0 to 40 degrees. Adopting a constant or a repetitive hip adduction during static and dynamic tasks possibly contribute to the development of GT.
Examples of activities and positions:
- standing with one hip in adduction
- sitting with knees together crossed in adduction
- excessive lateral pelvic tilt or shift during dynamic single leg loading tasks.
- Running with a midline or cross-midline foot-ground contact pattern
ITB tension also exert loads on GMed and GMin tendons at higher degrees of flexion through the fascial confluence of the ITB with the gluteal fascia . These findings suggest that combining adduction and flexion, such as in sitting with the knee crossed or adducted, further increases the exerted ITB tension, thus worsens the condition.
2-Muscle Force: an imbalance in controlling frontal plane movement between the trochanteric abductors (GMed and GMin) and the ITB-tensioners (upper abducting portion of gluteus maximus (UGM), tensor fascia lata (TFL) and vastus lateralis (VL) was observed in patients with GT[5][6]. Suggesting an an altered biomechanical force distribution and abnormal mechanical loading on gluteal tendons, however, further studies are needed to confirm this hypothesis.
3-Bony Factors: a biomechanical study using cadaveric modeling showed increased compressive force associated with reduced femoral neck angle[7]. Another study related the severity of GT to lower femoral neck-shaft angle compared with pain-free subjects with hip OA[8]. Lower neck-shaft angle is likely to contribute to greater offset (the difference between the width of the iliac wings and that of the greater trochanters). All these bony factors are suggested to influence ITB compression against gluteal tendons[1].
Females are more likely to develop GT. A study concluded that females, in general, tend to have a relatively smaller GMed insertion on the femur along with shorter moment arm resulting in reduced mechanical efficiency, particularly significant in those with smaller femoral neck shaft angle[9].
Clinical Presentation[edit | edit source]
Lateral hip pain caused by tendinopathy may be challenging to diagnose because of the long list of referred pain possibilities[1].
Pain is the main characteristic of GT, frequently insidious, gradually worsens with time and with different loads and tasks[10]. The pain might be significant after a strong guarding contraction of the adductors during a slip or fall. It gets worse at night and sleeping on the affected side worsens the symptoms[11], affecting the quality of sleeping.
Assessing functional limitation and levels of discomfort is important. Patients usually report pain with single-loading tasks such as walking and stairs negotiation. Tasks that require active hip extension, such as sit to stand, are also accompanied with pain and stiffness. The latter is a mutual feature between GT and hip OA, however, patients with OA usually have difficulties manipulating shoes and socks (hip flexion) but this problem is not relevant with GT[1].
Diagnostic Procedures[edit | edit source]
A thorough hip examination is needed basically by obtaining patient's history to understand the nature of the symptoms and rule out Red Flags. Then, the assessor should go into PE with a hypothesis that to be confirmed with clinical tests. The following tests, although have weak diagnostic properties, are commonly used in MSK settings to confirm GT diagnosis:
- Ober's test
- Single stance assessment for 30 sec: recommended over Trendelenberg's test.
- Adduction/External Rotation with resistance
- FABER test: the hip ROM is not limited in GT.
Pain provocation and reproduction of symptoms by loading abductors are the aims of these test. Assessing active abduction in a position of hip adduction may be more useful.Further provocation could be elicited by testing the glueal muscles internal rotation function at a 90 degree hip flexion and maximal external rotation[1]. The traditional Trendelenburg test was useful in diagnosing partial and complete abductor tendon[12] tears at advanced stages of the pathology[1].
| [13] | [14] |
| [15] | [16] |
Pain on palpation of the structures over the greater trochanter is considered a cardinal sign in diagnosing Greater Trochanter Pain Syndrome. If the direct compression over this area failed to elicit pain then GT may be excluded and other conditions would be considered[18]. The available literature has not yet provided a clear combination of diagnostic tests to confirm GT diagnosis. Further research is required to reach accurate and objective set of criteria and/or tests.
The Victorian Institute of Sport Assessment-Gluteal tendon (VISA-G) can be used to assess and track pain intensity and functional limitation[19].
Cook and Purdam[20] suggest functional loading tests to assess and track a tendon's response to therapy. Reduced pain on single leg standing and hopping indicates improved loading tolerance of the gluteal tendons. Longer standing time on one leg or increased number of hops to onset of pain reflect improvement. Inadequate eccentric pelvic control in single leg loading tasks indicates a greater hip adduction moment arm and possible gluteal tendons compression. Video analysis of is suggested for athletes to observe pelvic tilt and femoral adduction in running and changing direction[1].
Imaging could be indicated, particularly if there was trauma involved, to exclude sever injury, fracture or other sinister pathology. Ultrasound is superior to MRI in diagnosing bursae, however, MRI is the gold standard in distinguishing direct (soft tissue oedema, tendon thickening, intrasubstance signal abnormality and focal discontinuity or absence of tendon fibres) and indirect signs (fatty atrophy of the GMed and GMin muscles) of GT[1][22].
Differential Diagnosis[edit | edit source]
- Hip OA
- Avascular Necrosis
- Femoral-acetabular Impingement (FAI)
- Greater Trochanter Pain Syndrome
- Trochanteric Bursitis
Management Strategies[edit | edit source]
Tendon reloading principles are suggested in managing tendonpathies in general[1] [23]. See Tendon Rehabilitation. There are specific consideration when attempting to address GT.
Load Management[edit | edit source]
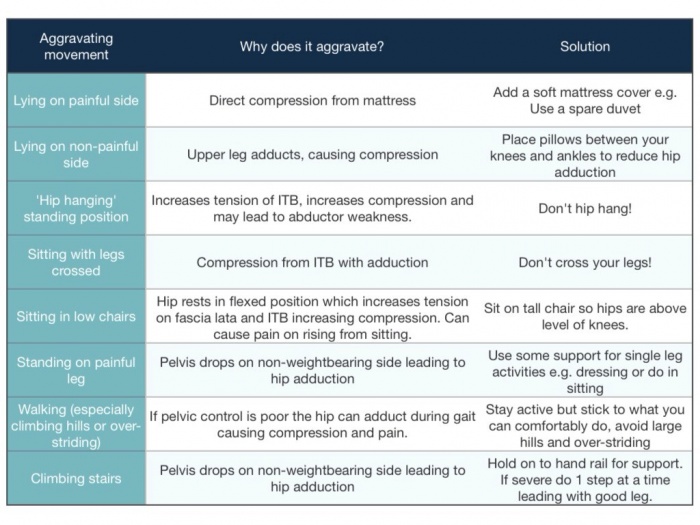
Education and training on obtaining optimal biomechanical positions and avoidance of provocative positions such as prolonged seating, sitting on low seat, crossed knee sitting, hanging on hip and sustained hip adduction positions.
As in the management of other tendinopathies, stretching should be avoided as it combines strong passive tensile loads. Therefore, Patients with GT should avoid hip adduction stretches either from flexed or extended hip. Massage and dry needling could replace stretching for pain management, however, strong ITB release could be pain provocative.
Night pain is a significant issue in GT patients. Teaching patients on using alternative postures such as supine or using a pillow under the knees to unload the anterolateral hip. Using an eggshell mattress with pillows between knees and shin reduces the compression on lateral hip.
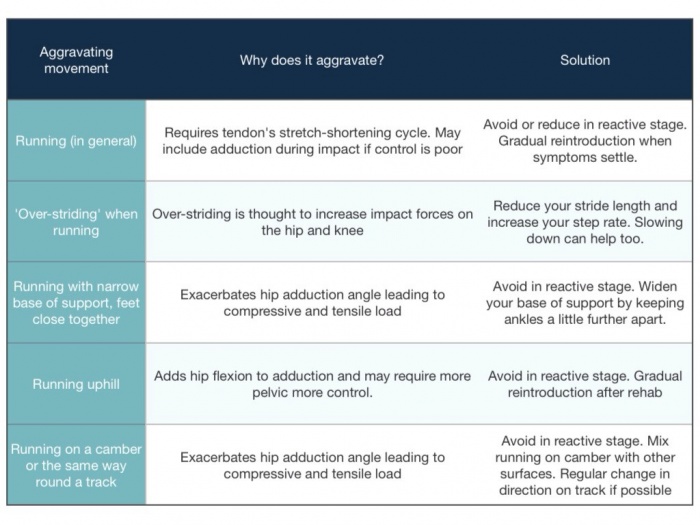
Load management also includes correcting movement patterns in functional and sports-related activities. Also, recreational and sports modifications, either by avoiding aggravating activities, such as, high tempo, hill running, and plyometric drills, in the short term or by altering exercise volume[24].
Exercise [edit | edit source]
Tensile loading program aiming to reduce pain and improving tendon loading capacity. Combined strengthening and functional exercises to optimize movement control patterns and obtain pelvic control.
Isometric exercises exhibit an analgesic effect due to activation of segmental and extra-segmental descending pain inhibitory pathway, Therefore they are used for pain management Low load, low velocity isometric hip abduction may be performed sidelying, supine and standing positions for multidirectional training.
Exercise should then progress to low velocity, high tensile loading to achieve gluteal tendons hypertrophy. Concentric-eccentric hip abductor exercises through mid to inner range of abduction allow for high tensile loading with minimal compression. Because this cannot be fully achieved in single-leg loading exercises, gradual and monitored progression are required with enough time between exercise sessions for recovery.
The overall hip abductors strength is not strongly correlated with hip adduction angle during functional tasks, therefore specific movement retraining in the frontal plane should be incorporated in GT management.
Feedback on reducing hip adduction moment during running can significantly reduce hip adduction and contralateral pelvic drop during running.
We should also identify associated mechanical dysfunctions in surrounding joints; lumbar, hip and knee and address them to correct the loading patterns on gluteal tendons.
A randomized clinical trial by Mellor et al. compared the effectiveness of load management education plus exercise with corticosteroid injection and a ''wait-and see'' approach. Education and exercise resulted in 77.3% success rate on the global rating of change and hip pain intensity on both short and long terms[2].
The exercise program suggested in Mellor et al. study utilized a combination of low load activation of abduction, pelvic control in frontal plane exercises and abductor loading in frontal plane. Bridging variations, squatting and lunges were used for functional Loading progressions and pelvic control training. It is important to integrate functional exercises at different positions to optimize the motor control. To load abductors in frontal plane. subjects in exercise group performed different abduction exercises against spring resistance. Motoring load appropriately is recommended by increasing load gradually without pain aggravation, particularly night pain.[2]. Slow and heavy loading. similar to tendon rehab by cook, but it isn't an eccentric only approach. VAS during activity. Symptom response over next 24-48 hours and pain during tendon load tests
Following this study, Ganderton et al.[19] compared gluteal Loading to sham Exercises on pain and dysfunction in women with GTPS. the study found differences in symptoms but no significant differences in hip abductor muscle torque was found between the two groups. Although the study had several limitations regarding the utilized exercise program the psychological factors were highlighted. Pain and limitation severity were associated with higher pain catastrophizing, pain self-efficacy and depression scores.
Fear and uncertainty are associated with achillis[25] and gluteal tendinopathoes[26]. Kinesiophobia is also a key factor influencing achillies tendon recovery[27]. These findings support the need for utilizing a bio-psychological management approach by addressing patients' concerns on returning to the basic level of activities, helping them identifying their barriers to recovery, exercise empathy, explaining tendinopathy in a positive way and knowing when to refer to other specialized healthcare professional[28].
| [29] | [30] |
Other Interventions[edit | edit source]
Steroid Injection
Corticosteriod injections provided analgesic effect,yet the pain doesn't resolve completely and and often recurrent[1]. Corticosteriods exhibit non-inflammatory effect. on the other hand, GT is reported to be a degenerative condition rather than inflammatory[31]. The pain relieving effect following crticosteriods might interfer with the tendon capacity to respond appropriately to loading[32].
Surgical Intervention
Surgery is considered in persistent pain and failed conservative treatment[1]. 90% long-term improvement was reported following GMed tendon repair in 72 patients[33]. Endoscopic repairs provide an accelerated rehabilitaion and less invasive approach with reduced rates of post-operative infection, scar tissue formation and pain. Patients with larger tears are not suitable for endoscopic techniques.
Removal of trochanteric bursae and ITB release is utilized in patients without gluteal tears. Studies report good to excellent short-medium term outcomes[34], however, most studies lacked control group and the rationale behind the mechanism of efficacy remains unclear[1].
References[edit | edit source]
- ↑ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 1.11 1.12 1.13 Grimaldi A, Mellor R, Hodges P, Bennell K, Wajswelner H, Vicenzino B. Gluteal tendinopathy: a review of mechanisms, assessment and management. Sports Medicine. 2015 Aug 1;45(8):1107-19.
- ↑ 2.0 2.1 2.2 Mellor, R., Bennell, K., Grimaldi, A., Nicolson, P., Kasza, J., Hodges, P., Wajswelner, H. and Vicenzino, B., 2018. Education plus exercise versus corticosteroid injection use versus a wait and see approach on global outcome and pain from gluteal tendinopathy: prospective, single blinded, randomised clinical trial. bmj, 361, p.k1662.
- ↑ Almekinders LC, Weinhold PS, Maffulli N. Compression etiology in tendinopathy. Clinics in sports medicine. 2003 Oct 1;22(4):703-10.
- ↑ Birnbaum K, Siebert CH, Pandorf T, Schopphoff E, Prescher A, Niethard FU. Anatomical and biomechanical investigations of the iliotibial tract. Surgical and Radiologic Anatomy. 2004 Dec 1;26(6):433-46.
- ↑ Sutter R, Kalberer F, Binkert CA, Graf N, Pfirrmann CW, Gutzeit A. Abductor tendon tears are associated with hypertrophy of the tensor fasciae latae muscle. Skeletal radiology. 2013 May 1;42(5):627-33.
- ↑ Pfirrmann CW, Notzli HP, Dora C, Hodler J, Zanetti M. Abductor tendons and muscles assessed at MR imaging after total hip arthroplasty in asymptomatic and symptomatic patients. Radiology. 2005 Jun;235(3):969-76.
- ↑ Birnbaum K, Prescher A, Niethard FU. Hip centralizing forces of the iliotibial tract within various femoral neck angles. Journal of Pediatric Orthopaedics B. 2010 Mar 1;19(2):140-9.
- ↑ Fearon AM, Stephens S, Cook JL, Smith PN, Neeman T, Cormick W, Scarvell JM. The relationship of femoral neck shaft angle and adiposity to greater trochanteric pain syndrome in women. A case control morphology and anthropometric study. Br J Sports Med. 2012 Sep 1;46(12):888-92.
- ↑ Woyski D, Olinger A, Wright B. Smaller insertion area and inefficient mechanics of the gluteus medius in females. Surgical and Radiologic Anatomy. 2013 Oct 1;35(8):713-9.
- ↑ Lequesne M. From “periarthritis” to hip “rotator cuff” tears. Trochanteric tendinobursitis. Joint Bone Spine. 2006;4(73):344-8.
- ↑ Connell DA, Bass C, Sykes CJ, Young D, Edwards E. Sonographic evaluation of gluteus medius and minimus tendinopathy. European radiology. 2003 Jun 1;13(6):1339-47.
- ↑ Bird PA, Oakley SP, Shnier R, Kirkham BW. Prospective evaluation of magnetic resonance imaging and physical examination findings in patients with greater trochanteric pain syndrome. Arthritis & Rheumatism: Official Journal of the American College of Rheumatology. 2001 Sep;44(9):2138-45.
- ↑ Classic Gluteal Tendinopathy Diagnosis. Available from: https://www.youtube.com/watch?v=216ZAxN4FNc
- ↑ Ober's Test/ITB tightness Available from: https://www.youtube.com/watch?v=Amjv6FzDeLE
- ↑ Patrick's/Faber/Figure four test. Available from: https://www.youtube.com/watch?v=89Qiht82zmg
- ↑ What single leg standing assessment can tell you Available from: https://www.youtube.com/watch?v=A9pi7_JRgwQ
- ↑ Resisted External Derotation Test/Gluteal Tendinopathy. Available from: https://www.youtube.com/watch?v=nwBnc3I53QY
- ↑ Bird PA, Oakley SP, Shnier R, Kirkham BW. Prospective evaluation of magnetic resonance imaging and physical examination findings in patients with greater trochanteric pain syndrome. Arthritis & Rheumatism: Official Journal of the American College of Rheumatology. 2001 Sep;44(9):2138-45.
- ↑ 19.0 19.1 Ganderton C, Semciw A, Cook J, Moreira E, Pizzari T. Gluteal Loading Versus Sham Exercises to Improve Pain and Dysfunction in Postmenopausal Women with Greater Trochanteric Pain Syndrome: A Randomized Controlled Trial. Journal of Women's Health. 2018 May 1.
- ↑ Cook JL, Purdam CR. The challenge of managing tendinopathy in competing athletes. Br J Sports Med. 2013 May 9:bjsports-2012.
- ↑ Video gait running analysis: alignment, issues, rear view. Available from: https://www.youtube.com/watch?v=k1hlY0EMYJw
- ↑ Kong A, Van der Vliet A, Zadow S. MRI and US of gluteal tendinopathy in greater trochanteric pain syndrome. European radiology. 2007 Jul 1;17(7):1772-83.
- ↑ Beyer R, Kongsgaard M, Hougs Kjær B, Øhlenschlæger T, Kjær M, Magnusson SP. Heavy slow resistance versus eccentric training as treatment for Achilles tendinopathy: a randomized controlled trial. The American journal of sports medicine. 2015 Jul;43(7):1704-11.
- ↑ Grimaldi A, Fearon A. Gluteal tendinopathy: Pathomechanics and implications for assessment and management. J Orthop Sports Phys Ther. 2015;45:910-22.
- ↑ Mc Auliffe S, Synott A, Casey H, Mc Creesh K, Purtill H, O'Sullivan K. Beyond the tendon: Experiences and perceptions of people with persistent Achilles tendinopathy. Musculoskeletal Science and Practice. 2017 Jun 1;29:108-14.
- ↑ Plinsinga ML, Coombes BK, Mellor R, Nicolson P, Grimaldi A, Hodges P, Bennell K, Vicenzino B. Psychological factors not strength deficits are associated with severity of gluteal tendinopathy: A cross‐sectional study. European Journal of Pain. 2018 Jul.
- ↑ Silbernagel KG, Brorsson A, Lundberg M. The majority of patients with Achilles tendinopathy recover fully when treated with exercise alone: a 5-year follow-up. The American journal of sports medicine. 2011 Mar;39(3):607-13.
- ↑ Gluteal tendinopathy, are psychological factors more important than strength?Available from:https://www.running-physio.com/gt-factors/
- ↑ Isometric hip abduction. Available from: https://www.youtube.com/watch?v=2OZ8hLR-NxM
- ↑ Bridging with progressions tightness Available from: https://www.youtube.com/watch?v=qaoa9V-bL9c
- ↑ Coombes BK, Bisset L, Vicenzino B. Thermal hyperalgesia distinguishes those with severe pain and disability in unilateral lateral epicondylalgia. The Clinical journal of pain. 2012 Sep 1;28(7):595-601.
- ↑ Coombes BK, Bisset L, Brooks P, Khan A, Vicenzino B. Effect of corticosteroid injection, physiotherapy, or both on clinical outcomes in patients with unilateral lateral epicondylalgia: a randomized controlled trial. Jama. 2013 Feb 6;309(5):461-9.
- ↑ Walsh MJ, Walton JR, Walsh NA. Surgical repair of the gluteal tendons: a report of 72 cases. The Journal of arthroplasty. 2011 Dec 1;26(8):1514-9.
- ↑ Craig RA, Gwynne Jones DP, Oakley AP, Dunbar JD. Iliotibial band Z‐lengthening for refractory trochanteric bursitis (greater trochanteric pain syndrome). ANZ journal of surgery. 2007 Nov;77(11):996-8.