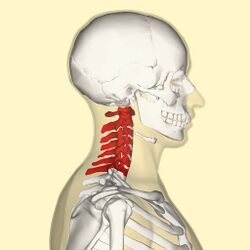
Functional Anatomy of the Cervical Spine
Introduction[edit | edit source]
The cervical spine supports and promotes movement of the head and neck. [1] [2] Intervertebral discs maintain the spaces between the vertebrae. These discs act like shock absorbers throughout the spinal column to cushion the bones as the body moves. Ligaments hold the vertebrae in place, and tendons attach the muscles to the spinal column. The cervical spine is subjected to extrinsic factors such as repetitive movements, whole body vibrations and static load.[3]
Key Terms[edit | edit source]
Axes: lines around which an object rotates. The rotation axis is a line that passes through the centre of mass. There are three axes of rotation: sagittal passing from posterior to anterior, frontal passing from left to right, and vertical passing from inferior to superior. The rotation axes of the foot joints are perpendicular to the cardinal planes. Therefore, motion at these joints results in rotations within three planes. Example: supination involves inversion, internal rotation, and plantarflexion.
Bursae: reduce friction between the moving parts of the body joints. A bursa is a fluid-filled sac. There are four types of bursae: adventitious, subcutaneous, synovial, and sub-muscular.
Capsule: one of the characteristics of the synovial joints. It is a fibrous connective tissue which forms a band that seals the joint space, provides passive and active stability and may even form articular surfaces for the joint. The capsular pattern is "the proportional motion restriction in range of motion during passive exercises due to tightness of the joint capsule."
Closed pack position: the position with the most congruency of the joint surfaces. In this position, joint stability increases. For example, the closed pack position for the interphalangeal joints is a full extension.
Degrees of freedom: the direction of joint movement or rotation; there is a maximum of six degrees of freedom, including three translations and three rotations.
Ligament: fibrous connective tissue that holds the bones together.
Open (loose) pack position: position with the least joint congruency where joint stability is reduced.
Planes of movement: describe how the body moves. Up and down movements (flexion/extension) occur in the sagittal plane. Sideway movements (abduction/adduction) occur in the frontal plane. The transverse plane movements are rotational (internal and external rotation).
Cervical Spine Structure[edit | edit source]
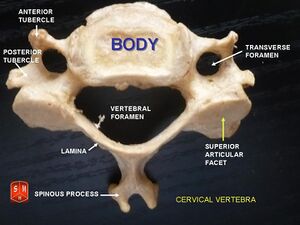
Cervical Vertebrae[edit | edit source]
There are seven lumbar vertebrae, which are known as C1-C7 whose role is to support and promote movement of the head. Considering the small weight-bearing load of the cervical spine, these vertebral bodies do not require height, just flexibility to facilitate movement. With increased range of motion in the cervical spine, there is heightened injury potential to the spinal cord and its associated neurovascular structures.[2]
The seven vertebral bodies have unique characteristics:
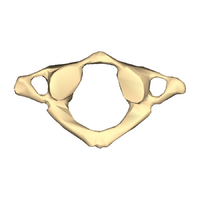
Atlas
- no vertebral body
- no spinous process
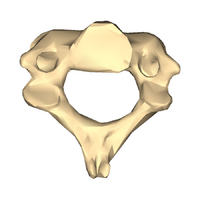
Axis
- odontoid process (dens) extending superiorly from anterior portion of the vertebra
C3-C6
- triangular vertebral foramen
- bifed spinous process
- transverse foramina (space for nerves and vasculature)
C7
- singular spinous process
- larger spinous process
**In supine: It may be difficult to palpate the spinous process of C3-C6 with normal cervical lordosis
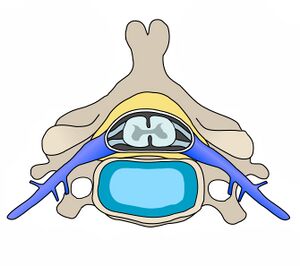
Intervertebral Disc (IVD)[edit | edit source]
Overall, intervertebral discs involve 25% of the height of the entire spine. In the cervical region, the discs compromise 40% of the height. This increased height compared to vertebral body height provides an advantage for mobility. [5] The nucleus pulposus of cervical discs dries out by the age of 30 to a firm, fibrocartilaginous plate.[6]
The following are characteristics of the cervical spine intervertebral discs:
- thicker anteriorly than posterior
- concave superior surface
- convex inferior surface
- movement limited by uncinate process
- anteroposterior translation does occur
** Due to location of uncinate process, posterolateral disk herniations are less frequent
Cervical Lordosis[edit | edit source]
The cervical spine has a normal lordotic posture. Biomechanically, this posture is able to resist large compressive loads and decrease stress on vertebral end plates. Compressive load distribution in the cervical spine takes place 36% by the anterior column and 64% by the posterior facet joints[7]
Kinematics and Joints of the Cervical Spine[edit | edit source]
Kinematics[edit | edit source]
The most mobile part of the vertebral column is the cervical spine.
Normal range of motion for flexion is around 40 degrees and extension 50 degrees. The largest contributor to flexion/extension is from segments C4C5 and C5C6 in sitting and C6C7 in supine. The segment with the least contribution to flexion/extension is C7T1. Lateral flexion normal range of motion is close to 30 degrees. The segment that allows for most movement in this plane is C3–C4 and C6–C7 segments.
Lastly, cervical rotation has the highest range of motion normal values close to 70 degrees. Flexibility in this plane is mainly achieved through C1C2 segment.[8]
| Joint | Disc Joint | Facet Joint or Zygapophyseal Joints | Uncovertebral Joint | Atlanto-Axial Joint | Atlanto-Occipital Joint |
|---|---|---|---|---|---|
| Location/articulations |
|
|
|
|
|
| Functions |
|
|
|
|
|
| Orientation/Composition |
|
|
|
Spinal Ligaments[edit | edit source]
| Ligament | Origin | Insertion | Role/Function |
|---|---|---|---|
| Nuchal ligament | occiput | tips of the spinous process from C1-C7 | limit hyperflexion |
| Transverse ligament | connects lateral masses of atlas | anchors dens in place | |
| Apical ligament | dens of the axis | foramen magnum | stabilises skull on spiine |
| Lar Ligament | dens of the axis | occiput | limits atlanto-axial rotation |
| Cruciform or Cruciate Ligament
1. superior longitudinal band 2. inferior longitudinal band 3. transverse band |
|
|
hold dens in place |
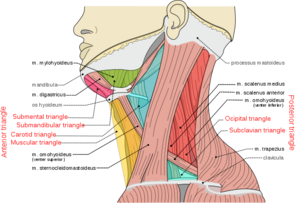
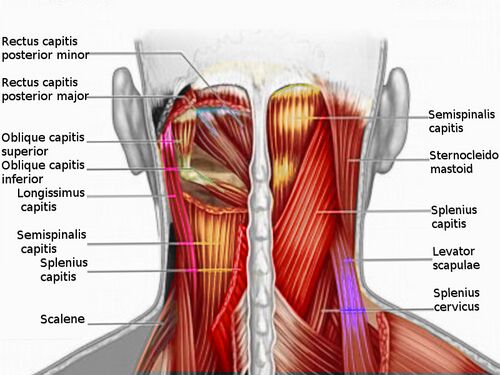
Muscles of the Cervical Spine[edit | edit source]
Muscles of the cervical spine can be divided by location or by the movement they create.
Anterior (Prevertebral) Vertebral Muscles[edit | edit source]
These are also termed Deep cervical flexor:
- Rectus Capitis Anterior
- Rectus Capitis Lateralis
- Longus capitis
- Longus colli/ Longus cervicis (3 portions: superior oblique, inferior oblique, vertical)
Lateral Vertebral Muscles[edit | edit source]
Scalenes - anterior, middle, posterior and minimus scalene muscles
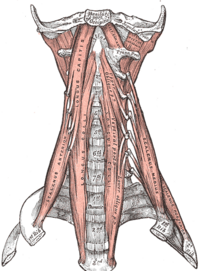
Posterior Vertebral Muscles[edit | edit source]
These can be further divided into intrinsic and extrinsic muscles.
Extrinsic muscles[edit | edit source]
Trapezius and Levator scapulae
Intrinsic muscles[edit | edit source]
- Superficial muscles :
- Deep muscles:
- Suboccipital group -
- Transversospinalis muscles -
- semispinalis capitis
- semispinalis cervicis
- rotatores cervicis
- multifidus (these are also known as deep neck extensors)
- Interspinales and intertransversarii
| Movement | Muscles |
|---|---|
| Flexion | Longus colli
Rectus capitis anterior (head only) |
| Extension | Iliocostal cervicis
Rectus capitis posterior, major and minor (head only) |
| Lateral flexion | Scalene anterior, medius and posterior
Sternocleidomastoid Splenius capitis Trapezius Erector spinae Rectus capitis lateralis (head only) |
| Rotation | Semispinalis cervicis
Multifidus Scalene anterior Splenius cervicis and capitis Sternocleidomastoid Inferior oblique (head only) Rectus captitis posterior major (head only) |
Cervical Spine Flexors[edit | edit source]
| Muscle | Origin | Insertion | Innervation | Action |
|---|---|---|---|---|
| rectus capitis anterior | Lateral mass and transverse process of atlas (C1) | Basilar part of occipital bone | Anterior rami of 1st and 2nd cervical spinal nerves (C1 - C2) | Flexion of head at atlanto-occipital joint |
| longus colli | transverse processes of C3 to C5 and the vertebral bodies of C5 to T3 | anterior tubercle of C1, the vertebral bodies of C2 to 4, and the transverse processes of C5 and C6. | Anterior rami of 2nd to 6th cervical spinal nerves (C2 - C6) | Unilateral contractions - neck lateral flexion (ipsilateral), neck rotation (contralateral)
Bilateral contractions - neck flexion |
| longus capitis | transverse processes of C3 to C6 | occipital bone | Anterior rami of 1st to 3rd cervical spinal nerves (C1 - C3) | Unilateral contractions - rotation of head (ipsilateral)
Bilateral contractions - flexion of head and neck |
| anterior scalene | transverse processes of C3 to C6 | first rib | Anterior rami of 4th to 6th cervical spinal nerves (C4 - C6) | Unilateral contractions - neck lateral flexion (ipsilateral), neck rotation (contralateral), elevation of first rib
Bilateral contractions - neck flexion |
| sternocleidomastoid | manubrium and the medial portion of the clavicle | mastoid process of the temporal bone | Accessory nerve (CN XI), branches of cervical plexus (C2 - C3) | Unilateral contractions - neck ipsilateral flexion, elevation of chin, head contralateral rotation
Bilateral contractions - extension of upper vertebral joints, extension of neck and head, elevation of head, elevation of sternum and clavicle, expansion of thoracic cavity |
| rectus capitis lateralis | Transverse process of atlas (C1) | Jugular process of occipital bone | Anterior rami of 1st and 2nd cervical spinal nerves (C1 - C2) | Lateral flexion of head (ipsilateral), stabilization of atlanto-occipital joint |
Cervical Spine Extensors[edit | edit source]
| Muscle | Origin | Insertion | Innervation | Action |
|---|---|---|---|---|
| obliques capitis superior | transverse process of the atlas | occipital bone | Suboccipital nerve (posterior ramus of 1st cervical spinal nerve (C1)) | stabilises atlanto-occipital joint |
| oblique capitis inferior | spinous process of the axis and inserts into the transverse process of the atlas, | tansverse process of atlas | Suboccipital nerve (posterior ramus of 1st cervical spinal nerve (C1)) | stabilises atlanto-occipital joint |
| rectus capitis posterior major | spinous process of C2 | occipital bone | Suboccipital nerve (posterior ramus of 1st cervical spinal nerve (C1)) | Unilateral contractions - head rotation (ipsilateral)
Bilateral contractions - head extension |
| rectus capitis posterior minor | posterior tubercle of the atlas | occipital bone | Suboccipital nerve (posterior ramus of 1st cervical spinal nerve (C1)) | head extension |
| iliocostal cervicis | ribs 3-6 | transverse process of C4-C6 | dorsal rami of the upper thoracic and lower cervical spinal nerves. | Laterally flexes and extends the lower cervical region |
| trapezius | occipital bone, nuchal ligament and spinous process C7-T12 | lateral third of clavicle, the acromian and the spine of s scapula |
|
supporting the spinal column to remain erect |
| spelnius cervicis | spinous process T3-T6 | transverse process of C1C3 | Dorsal rami of cervical spinal nerves (C5, 6, 7, and 8) | Bilaterally they extend the neck |
| splenius capitus | spinous process C7-T3 and nuchal ligament | occipital bone | posterior rami of the 2nd and 3rd cervical spinal nerves. | Acting bilaterally: extension of the head and cervical spine |
** The transversospinal muscles (rotatores, multifidus, semispinalis) are the deep muscle layers in the spine. They attach between the transverse and spinous process of the vertebrae. They stabilise and extend the spine. The rotatores also provide rotation.
Cervical Spine Lateral Flexors[edit | edit source]
| Muscle | Origin | Insertion | Innervation | Action |
|---|---|---|---|---|
| splenius cervicis | spinous process T3-T6 | transverse process C1-C3 | Dorsal rami of cervical spinal nerves (C5,6,7 and 8) | unilaterally they laterally flex and rotate the head and neck to the ipsilateral (same) side |
| splenius capitis | spinous process C7-T3 and nuchal ligament | occipital bone | posterior rami of the 2nd and 3rd cervical spinal nerves | Acting unilaterally: lateral flexion of the head and neck and rotation the head to the same side |
| sternocleidomastoid | manubrium and the medial portion of the clavicle | mastoid process of the temporal bone | Accessory nerve (CN XI), branches of cervical plexus (C2 - C3) | Unilateral contractions - neckpper vertebral joints, extension of neck and head, elevation of head, elevation of sternum and clavicle, expansion of thoracic cah cervical spinal nerves (C4 - C6) |
| middle scalene | posterior tubercles of the transverse processes of C2-C7 | scalene tubercle of the first rib. | Anterior rami of C3-C8. | Elevation of the first rib. Ipsilateral contraction causes ipsilateral lateral flexion of the neck |
| posterior scalene | posterior tubercles of the transverse processes of C5-C7 | 2nd rib | Anterior rami of C6-C8 | Elevation of the second rib, and ipsilateral lateral flexion of the neck |
| trapezius | occipital bone, nuchal ligament and spinous process C7-T12 | lateral third of clavicle, the acromian and the spine of s scapula |
|
side bending |
| rectus capitis lateralis | Superior surface of the transverse process of atlas | Inferior surface of the jugular process of the occipital bone | Anterior rami of C1-C2 spinal nerves | Stabilizes the atlanto-occipital joint; head lateral flexion (ipsilateral) |
Cervical Spine Rotators[edit | edit source]
| Muscle | Origin | Insertion | Innervation | Action |
|---|---|---|---|---|
| rectus capitis posterior major | spinous process of C2 | occipital bone | Suboccipital nerve (posterior ramus of 1st cervical spinal nerve (C1)) | Unilateral contractions - head rotation (ipsilateral)
Bilateral contractions - head extension |
| rectus capitis posterior major | spinous process of C2 | occipital bone | Suboccipital nerve (posterior ramus of 1st cervical spinal nerve (C1)) | Unilateral contractions - head rotation (ipsilateral)
Bilateral contractions - head extension |
| sternocleidomastoid | manubrium and the medial portion of the clavicle | mastoid process of the temporal bone | Accessory nerve (CN XI), branches of cervical plexus (C2 - C3) | Unilateral contractions - neck ipsilateral flexion, elevation of chin, head contralateral rotation
Bilateral contractions - extension of upper vertebral joints, extension of neck and head, elevation of head, elevation of sternum and clavicle, expansion of thoracic cah cervical spinal nerves (C4 - C6) |
| splenius capitis | spinous process C7-T3 and nuchal ligament | occipital bone | posterior rami of the 2nd and 3rd cervical spinal nerves | Acting unilaterally: lateral flexion of the head and neck and rotation the head to the same side |
| splenius cervicis | spinous process T3-T6 | transverse process C1-C3 | Dorsal rami of cervical spinal nerves (C5,6,7 and 8) | unilaterally they laterally flex and rotate the head and neck to the ipsilateral (same) side |
Innervation of the Cervical Spine[edit | edit source]
Nerves originating from the cervical plexus innervate the muscles of the neck. Each nerve root in the cervical spine exits above its corresponding nerve root. There are eight pairs of cervical nerves despite the presence of seven cervical vertebrae. The C8 nerve root exits below the seventh cervical vertebrae. The accessory nerve which is cranial nerve X1 innervates the sternocleidomastoid as well as the trapezius. [2]
| Nerve | Motor | Sensory |
|---|---|---|
| C1 | head and neck extensor;
rectus capitus anterior and lateral longus capitus |
|
| C2 | head and neck extensor;
rectus capitus anterior and lateral, longus capitus, longus colli |
lateral occiput and submandibular area |
| C3 | head and neck extensors,
longus capitus, longus colli, levator scapulae, scaleni, and trapezius |
lateral occiput and lateral neck, overlapping C2 |
| C4 | head and neck extensors,
longus coli, levator scapulae, scaleni, trapezius, and diaphragm. |
lower lateral neck and medial shoulder area |
| C5 | deltoid, biceps, bicep tendon reflex | clavicle level and lateral arm |
| C6 | biceps, wrist extensors, brachioradialis tendon reflex | lateral forearm, thumb, index and half of 2nd finger |
| C7 | wrist flexors, triceps, triceps tendon reflex | second finger |
| C8 | finger flexors, interossei | medial forearm, ring and little finger |
| T1 | interossei | medial arm |
Vascular Supply of the Cervical Spine[edit | edit source]
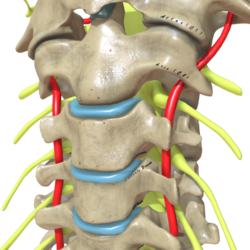
Vertebral arteries, veins and nerves pass through the transverse foramina of the cervical vertebrae. C7 is the only exception in that the vertebral artery passes around the vertebra instead of through the transverse foramen.[4]The neural components sit posterior to the vertebral artery.[11]
The cervical spine vascular supply is primarily provided by the vertebral arteries one on each side. These arteries arise from the subclavian arteries that originate directly from the arch of the aorta on the right side, and via the brachiocephalic trunk on the left side.
** The common carotid arteries bifurcates into the internal and external carotid arteries at the C3 segmental level. Only the external carotid artery provides any blood supply to the neck.
Clinical Relevance[edit | edit source]
A disc herniation is a condition where the nucleus pulposus, which is the gel-like centre of the disc, protrudes through the annulus fibrosis, which is the surrounding ring of collagen fibres. While disc herniations in the cervical spine are a lot less common than in the lumbar spine, it can still occur. Typically, it occurs at the level of C5 to 6 and C6 to 7.
Conditions like rheumatoid arthritis can affect the stability of the atlanto-axial joint, which can result in serious neurological consequences due to the proximity of the spinal cord. Laxity in the transverse ligament is also present in 14% to 22% of individuals with Down syndrome. sternocleidomastoid is wry neck, or torticollis, where the head appears to be tilted at an odd angle.
prevertebral cervical muscles, that can be thought of as the equivalent of the core of the neck and play an important role in the stabilisation of the neck. Dysfunction in these muscles can play a part in cervicogenic pain. Let's look at the flexion movement again.
Trigger points that develop in the suboccipital muscles can refer pain to the head causing headaches.
(daphne)
- Disc herniations are a common low back condition. They occur when the nucleus pulposus displaces from the intervertebral space. According to Yoon et al., when there is imaging confirmation of lumbar disc herniation that is "consistent with clinical findings, and failure to improve after six weeks of conservative care", surgical intervention may be required. You can read more about the management of disc herniation symptoms here.
- Spinal stenosis is a narrowing of the spinal canal. Spinal stenosis can be caused by a range of conditions, such as tumours or bone spurs. You can learn about low back pain assessment and prognosis by taking this course.
- Diastasis recti is a very common condition where the linea alba stretches and produces a gap between the two sides of the rectus abdominis muscle. Learn more about diastasis recti here.
References[edit | edit source]
- ↑ Frost BA, Camarero-Espinosa S, Foster EJ. Materials for the spine: anatomy, problems, and solutions. Materials. 2019 Jan;12(2):253
- ↑ 2.0 2.1 2.2 2.3 Kaiser JT, Lugo-Pico JG. Anatomy, Head and Neck, Cervical Vertebrae. 2019.
- ↑ Petersen JA, Brauer C, Thygesen LC, Flachs EM, Lund CB, Thomsen JF. Prospective, population-based study of occupational movements and postures of the neck as risk factors for cervical disc herniation. BMJ open. 2022 Feb 1;12(2):e053999.
- ↑ 4.0 4.1 Teach me anatomy The cervical Spine Available from:https://teachmeanatomy.info/neck/bones/cervical-spine/
- ↑ 5.0 5.1 Learn muscles . Cervical spine joints. Available from: https://learnmuscles.com/blog/2017/08/01/cervical-spinal-joints/ (last accessed 29.1.2020)
- ↑ Peng B, Bogduk N. Cervical discs as a source of neck pain. An analysis of the evidence. Pain Medicine. 2019 Mar 1;20(3):446-55.
- ↑ Guo GM, Li J, Diao QX, Zhu TH, Song ZX, Guo YY, Gao YZ. Cervical lordosis in asymptomatic individuals: a meta-analysis. Journal of orthopaedic surgery and research. 2018 Dec;13(1):1-7.
- ↑ Lindenmann S, Tsagkaris C, Farshad M, Widmer J. Kinematics of the Cervical Spine Under Healthy and Degenerative Conditions: A Systematic Review. Annals of Biomedical Engineering. 2022 Dec 10:1-29.
- ↑ RSNA Joints of Luschka Available from: https://pubs.rsna.org/doi/10.1148/66.2.181 (last accessed 28.1.2020)
- ↑ Palastanga, N., & Soames, R. (2012). Anatomy and human movement (6th ed.). Edinburgh: Churchill Livingstone.
- ↑ Joshi N, Klinger N, Halalmeh DR, Tubbs RS, Moisi MD. The Neural Sulcus of the Cervical Vertebrae: A Review of Its Anatomy and Surgical Perspectives. Cureus. 2020 Jan 18;12(1)