Diabetes Mellitus Type 1: Difference between revisions
No edit summary |
No edit summary |
||
| Line 4: | Line 4: | ||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | ||
</div> | </div> | ||
== Definition/Description | == Definition/Description == | ||
[[Image:6266469746 130fbca345 b.jpg|272x383px|alt=|right|frameless]]Type 1 diabetes mellitus (T1DM) is an [[Autoimmune Disorders|autoimmune disease]] that leads to the destruction of insulin-producing pancreatic beta cells. | |||
Insulin: is an essential anabolic [[Hormones|hormone]] that exerts multiple effects on glucose, lipid, protein, and mineral metabolism, as well as growth; importantly, insulin allows glucose to enter [[Muscle Cells (Myocyte)|muscle]] and adipose cells, stimulates the liver to store glucose as glycogen and synthesize fatty acids, stimulates the uptake of amino acids, inhibits the breakdown of fat in adipose tissue, and stimulates the uptake of potassium into cells. | |||
Individuals with type 1 diabetes mellitus require life-long [[Insulin in the Treatment of Diabetes Mellitus|insulin replacement therapy]]. Without insulin, diabetic [[ketoacidosis]] (DKA) develops and is life-threatening<ref name=":0">Lucier J, Weinstock RS, Doerr C. [https://www.ncbi.nlm.nih.gov/books/NBK507713/ Diabetes Mellitus Type 1] (Nursing).2021 Available: https://www.ncbi.nlm.nih.gov/books/NBK507713/ (accessed 28.9.2021)</ref>. | |||
(T1DM) can result in serious vascular complications and [[neuropathies]] and can be a major cause of [[Cardiovascular Disease|cardiovascular disease]] and [[Stroke|strokes]]. It is also the leading cause of [[Chronic Kidney Disease|end-stage renal (kidney) disease]], non-traumatic [[amputations]] in the lower extremity, and new cases of blindness.<ref name="Goodman and Snyder">Goodman CC, Snyder TEK. Differential Diagnosis for Physical Therapists: Screening for Referral. 5th ed. St. Louis, MO: Saunders/Elsevier; 2013: 425-432.</ref>. | |||
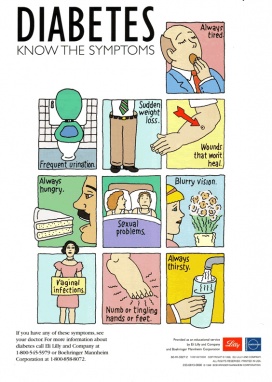
Image 1: Overview of possible symptoms of diabetes | |||
== Etiology == | |||
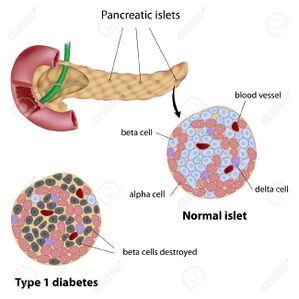
== | [[File:Pancreas.jpg|299x299px|alt=|right|frameless]]In T1DM, there is the immune destruction of the beta cells in the pancreatic islets over months or years, causing an absolute deficiency of insulin. Although the exact etiology of T1DM is still unknown, researchers believe there is a genetic predisposition. | ||
* | * In those at risk, it is generally believed that a virus or other environmental factors trigger the autoimmune beta-cell destruction. Some studies have found an increased development of T1DM in children born to a mother that had ''Coxsackievirus'' or another ''Enterovirus'' during pregnancy. | ||
* Environmental toxins have also been postulated to play a role. The hygiene hypothesis suggests that improved sanitation relates to the increased development of autoimmune-mediated disorders. It is proposed that the reduction of childhood exposure to infectious agents leads to the lack of proper immune system development. | |||
* Dietary factors have also been examined as potential triggers<ref name=":0" />. | |||
* | |||
== | == Epidemiology == | ||
T1DM is one of the most frequent chronic diseases in children but can start at any age. There has been a steady increase in the incidence and prevalence of T1DM, representing approximately 5% to 10% of people with diabetes. | |||
* | * In the United States, there are an estimated 1.24 million people with T1DM, and that number is expected to grow to 5 million by 2050. | ||
* | * Worldwide, there is also a considerable geographic variation in incidence. The highest reported incidences are in Finland and other Northern European nations with rates approximately 400-times greater than those seen in China and Venezuela<ref name=":0" />. | ||
* | |||
* | == Characteristics/Clinical Presentation == | ||
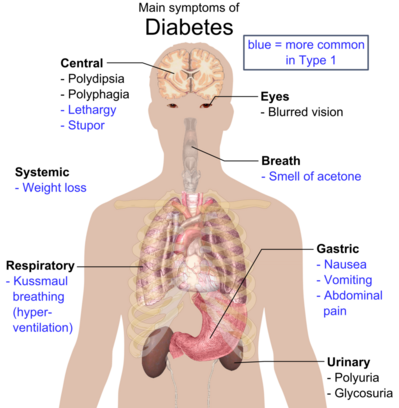
[[File:Diabetes signs.png|right|frameless|408x408px]] | |||
Symptoms for type 1 diabetes can include: | |||
* Extreme thirst | |||
* Frequent urination | |||
* Sudden unexplained weight loss | |||
* Extreme fatigue and weakness | |||
* Blurred vision | |||
* Nausea and vomiting | |||
* Constant hunger | |||
Image 2 : Overview of the most significant possible symptoms of diabetes | |||
The 4 T’s: A simple way to remember the four main symptoms of type 1 diabetes. | |||
# Tiredness | |||
# Toilet | |||
# Thinner | |||
# Thirsty<ref>Diabetes SA [https://www.diabetessa.com.au/Web/Signs_and_Symptoms/Type_1_Diabetes/Web/Signs_and_Symptoms/Type_1_Diabetes.aspx?hkey=d13c6e40-3678-4d80-b99d-2be4bba77188 Diabetes type 1] Available: https://www.diabetessa.com.au/Web/Signs_and_Symptoms/Type_1_Diabetes/Web/Signs_and_Symptoms/Type_1_Diabetes.aspx?hkey=d13c6e40-3678-4d80-b99d-2be4bba77188 (accessed 28.9.2021)</ref> | |||
== Associated Co-morbidities == | |||
* Neuropathy | |||
* Nephropathy | |||
* Retinopathy | |||
* Cardiomyopathy | |||
* Hypoglycemia | |||
* Diabetic ketoacidosis | |||
* Diabetic foot disease<ref name=":0" /> | |||
[[Image:Pompa-insulinova 600 5118.jpg|250x250px|thumb]] | |||
* | |||
== Diagnostic Tests == | == Diagnostic Tests == | ||
Diagnostic Criteria:<ref name="Goodman and Snyder" /><ref name="American Diabetes Association" /> | Diagnostic Criteria:<ref name="Goodman and Snyder" /><ref name="American Diabetes Association">American Diabetes Association. Type 1 Diabetes. Available from: http://www.diabetes.org/diabetes-basics/type-1/?loc=util-header_type1 (accessed 8 April 2016).</ref> | ||
*Fasting plasma glucose (FPG) ≥ 126 mg/dl on two different days | *Fasting plasma glucose (FPG) ≥ 126 mg/dl on two different days | ||
| Line 70: | Line 74: | ||
*Want to keep A1C levels below 7% | *Want to keep A1C levels below 7% | ||
*If A1C is >10%=medical attention immediately | *If A1C is >10%=medical attention immediately | ||
== Medical Management<ref name="Goodman and Snyder" /> == | == Medical Management<ref name="Goodman and Snyder" /> == | ||
| Line 135: | Line 104: | ||
Diabetic Ketoacidosis (DKA) can occur in type 1 DM patients . DKA usually occurs in children and young adults with undiagnosed DM, or when an individual with type 1 diabetes has increased insulin needs Be stress, trauma, surgery, infection, etc. Metabolic acidosis/HNNC (hyperglycemia hyperosmolar nonnegotiable acidosis) occurs more frequently in adults with type 2 diabetes. | Diabetic Ketoacidosis (DKA) can occur in type 1 DM patients . DKA usually occurs in children and young adults with undiagnosed DM, or when an individual with type 1 diabetes has increased insulin needs Be stress, trauma, surgery, infection, etc. Metabolic acidosis/HNNC (hyperglycemia hyperosmolar nonnegotiable acidosis) occurs more frequently in adults with type 2 diabetes. | ||
Signs/symptoms of Diabetic Ketoacidosis:<ref name="Medline Plus" /> | Signs/symptoms of Diabetic Ketoacidosis:<ref name="Medline Plus">Medline Plus. Diabetes Type 1. https://www.nlm.nih.gov/medlineplus/diabetestype1.html (accessed 6 April 2016).</ref> | ||
* Deep, rapid breathing | * Deep, rapid breathing | ||
* Fruity breath | * Fruity breath | ||
Revision as of 02:04, 28 September 2021
Original Editors - Collen Nalley and Abbye Senn from Bellarmine University's Pathophysiology of Complex Patient Problems project.
Top Contributors - Abbye Senn, Colleen Nalley, Lucinda hampton, Rachael Lowe, Elaine Lonnemann, Evan Thomas, WikiSysop, Fasuba Ayobami, Kim Jackson, Vidya Acharya and Amanda Ager
Definition/Description[edit | edit source]
Type 1 diabetes mellitus (T1DM) is an autoimmune disease that leads to the destruction of insulin-producing pancreatic beta cells.
Insulin: is an essential anabolic hormone that exerts multiple effects on glucose, lipid, protein, and mineral metabolism, as well as growth; importantly, insulin allows glucose to enter muscle and adipose cells, stimulates the liver to store glucose as glycogen and synthesize fatty acids, stimulates the uptake of amino acids, inhibits the breakdown of fat in adipose tissue, and stimulates the uptake of potassium into cells.
Individuals with type 1 diabetes mellitus require life-long insulin replacement therapy. Without insulin, diabetic ketoacidosis (DKA) develops and is life-threatening[1].
(T1DM) can result in serious vascular complications and neuropathies and can be a major cause of cardiovascular disease and strokes. It is also the leading cause of end-stage renal (kidney) disease, non-traumatic amputations in the lower extremity, and new cases of blindness.[2].
Image 1: Overview of possible symptoms of diabetes
Etiology[edit | edit source]
In T1DM, there is the immune destruction of the beta cells in the pancreatic islets over months or years, causing an absolute deficiency of insulin. Although the exact etiology of T1DM is still unknown, researchers believe there is a genetic predisposition.
- In those at risk, it is generally believed that a virus or other environmental factors trigger the autoimmune beta-cell destruction. Some studies have found an increased development of T1DM in children born to a mother that had Coxsackievirus or another Enterovirus during pregnancy.
- Environmental toxins have also been postulated to play a role. The hygiene hypothesis suggests that improved sanitation relates to the increased development of autoimmune-mediated disorders. It is proposed that the reduction of childhood exposure to infectious agents leads to the lack of proper immune system development.
- Dietary factors have also been examined as potential triggers[1].
Epidemiology[edit | edit source]
T1DM is one of the most frequent chronic diseases in children but can start at any age. There has been a steady increase in the incidence and prevalence of T1DM, representing approximately 5% to 10% of people with diabetes.
- In the United States, there are an estimated 1.24 million people with T1DM, and that number is expected to grow to 5 million by 2050.
- Worldwide, there is also a considerable geographic variation in incidence. The highest reported incidences are in Finland and other Northern European nations with rates approximately 400-times greater than those seen in China and Venezuela[1].
Characteristics/Clinical Presentation[edit | edit source]
Symptoms for type 1 diabetes can include:
- Extreme thirst
- Frequent urination
- Sudden unexplained weight loss
- Extreme fatigue and weakness
- Blurred vision
- Nausea and vomiting
- Constant hunger
Image 2 : Overview of the most significant possible symptoms of diabetes
The 4 T’s: A simple way to remember the four main symptoms of type 1 diabetes.
- Tiredness
- Toilet
- Thinner
- Thirsty[3]
Associated Co-morbidities[edit | edit source]
- Neuropathy
- Nephropathy
- Retinopathy
- Cardiomyopathy
- Hypoglycemia
- Diabetic ketoacidosis
- Diabetic foot disease[1]
Diagnostic Tests[edit | edit source]
- Fasting plasma glucose (FPG) ≥ 126 mg/dl on two different days
- A1C Levels≥ 6.5 % on two separate occasions (but must be confirmed by FPG)
- Oral glucose tolerance test ≥ 200 mg/dl
Other Information: [2]
- FPG >100mg/dl is a risk factor for future diabetes
- A1C is a measure of how diet, exercise, and/or medication/insulin have been controlling glucose over a period of time
- Normal FPG= 80-120 mg/dl
- Want to keep A1C levels below 7%
- If A1C is >10%=medical attention immediately
Medical Management[2][edit | edit source]
- Goal is to maintain blood glucose levels between 80 and 120 mg/dL. This is done through the modification of diet, exercise, and medication.
- Glucose monitoring
- Insulin injections or insulin pump
- Yearly eye and feet exams
- Daily foot inspections by patient
- A1C checked at least 2 times a year
- With retinopathy or nephropathy, avoid high intensity exercise that will significantly increase BP
- EDUCATION!
Physical Therapy Management (current best evidence) [2][edit | edit source]
- Screening examination should be done five years post diagnosis and annually thereafter; this screening includes reflexes, sensation in feet, questions about neuropathic symptoms, foot ulcers, calluses, etc
- Screening Activity Limitation and Safety Awareness Scale
- Exercise program
- EDUCATION
Important considerations:[edit | edit source]
- Should not exercise alone in case of hypoglycemic episode.
- Type 1 diabetics may need to decrease insulin dose or pump activity during exercise, as well as increase food intake, with prolonged activities (10-15g CHO with every 30 min. of exercise).[5]
- Exercise increases insulin, which can drop glucose levels to low dangerous ranges, especially with high intensity or prolonged duration exercise. Monitor glucose levels before, during, and after exercise.
- Watch for confused, lethargic state or change in mental status in DM patient - have patient do finger stick check for glucose levels if available and immediately refer to physician. IIf patient has an insulin pump, diabetic ketoacidosis (DK) can occur quicker if there is an interruption in insulin delivery. Monitor patient carefully for excess perspiration, increased motion at pump site, and temperature during exercise.
Watch for signs and symptoms of life threatening conditions:[edit | edit source]
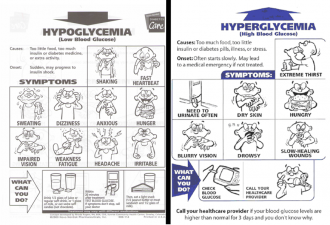
Hyperglycemia:
Diabetic Ketoacidosis (DKA) can occur in type 1 DM patients . DKA usually occurs in children and young adults with undiagnosed DM, or when an individual with type 1 diabetes has increased insulin needs Be stress, trauma, surgery, infection, etc. Metabolic acidosis/HNNC (hyperglycemia hyperosmolar nonnegotiable acidosis) occurs more frequently in adults with type 2 diabetes.
Signs/symptoms of Diabetic Ketoacidosis:[6]
- Deep, rapid breathing
- Fruity breath
- Dry skin and mouth
- Flushed face
- Nausea/vomiting
- Abdominal pain
Hypoglycemia:
<70 mg/dl is considered hypoglycemia; This is a major complication with insulin users (type 1 DM mainly). It usually occurs from decreased food intake or an increase in physical activity. Hypoglycemia interrupts oxygen consumption in nervous tissue. Patients using beta blockers are at a higher risk for developing hypoglycemia. If hypoglycemia is suspected, 10-15 g of carbohydrate (CHO) should be given ( this equals a ½ cup of juice/cola, 8 oz. milk, 2 sugar packets, or 2 oz. honey). It is good to keep these snacks in the clinic, but always ask patient about food allergies before administering food.
Blood glucose levels in relation to exercise that a PT should be aware of:[edit | edit source]
- <100 mg/dL= give 10-15 g CHO snack and retest glucose levels 15 minutes later
- 100-250 mg/dL= safe exercise levels; proceed with treatment
- 250-300 mg/dL @ start of exercise="caution zone"; postpone exercise until stable levels are achieved; ketones in urine are checked for at these levels
- >300 mg/dL= stop exercise immediately!!!! (NOT SAFE)
Differential Diagnosis[2][edit | edit source]
- Type 2 diabetes
- Cancer
- Diabetes Insipidus
- Dehydration
- Hypothyroidism
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 Lucier J, Weinstock RS, Doerr C. Diabetes Mellitus Type 1 (Nursing).2021 Available: https://www.ncbi.nlm.nih.gov/books/NBK507713/ (accessed 28.9.2021)
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 Goodman CC, Snyder TEK. Differential Diagnosis for Physical Therapists: Screening for Referral. 5th ed. St. Louis, MO: Saunders/Elsevier; 2013: 425-432.
- ↑ Diabetes SA Diabetes type 1 Available: https://www.diabetessa.com.au/Web/Signs_and_Symptoms/Type_1_Diabetes/Web/Signs_and_Symptoms/Type_1_Diabetes.aspx?hkey=d13c6e40-3678-4d80-b99d-2be4bba77188 (accessed 28.9.2021)
- ↑ American Diabetes Association. Type 1 Diabetes. Available from: http://www.diabetes.org/diabetes-basics/type-1/?loc=util-header_type1 (accessed 8 April 2016).
- ↑ Franc S, et al. Insulin-based strategies to prevent hypoglycaemia during and after exercise in adult patients with type 1 diabetes on pump therapy: the DIABRASPORT randomized study. Diabetes, Obesity, and Metabolism 2016; 12. http://www.ncbi.nlm.nih.gov/pubmed/26264812 (accessed 7 April 2016).
- ↑ Medline Plus. Diabetes Type 1. https://www.nlm.nih.gov/medlineplus/diabetestype1.html (accessed 6 April 2016).