Chondrosarcoma: Difference between revisions
mNo edit summary |
Kim Jackson (talk | contribs) No edit summary |
||
| (14 intermediate revisions by 6 users not shown) | |||
| Line 4: | Line 4: | ||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | ||
</div> | </div> | ||
== | == Introduction == | ||
[[File:Hip Chondrosarcoma.jpg|thumb|Chondrosarcoma - proximal femur]] | |||
Chondrosarcomas are malignant cartilaginous tumours, accounting for ~25% of all primary malignant [[bone]] tumours. They are most commonly found in [[Older People - Patterns of Illness, Physiological Changes and Multiple Pathology|older patients]], most commonly effecting the [[pelvis]], [[sternum]], [[scapula]], or [[cartilage]] of long bones in the extremities. | |||
Typically, chondrosarcoma forms within bone or cartilage cells around the articular surfaces and can be either slow-growing and form spontaneously, or due to malignant changes in a preexisting (secondary) bone tumour.<ref name="p1" /><ref name=":0">Radiopedia Chondrosarcoma Available:https://radiopaedia.org/articles/chondrosarcoma (accessed 12.9.2022)</ref> | |||
== Epidemiology == | |||
The typical presentation is in the 4th and 5th decades and there is a slight male predominance of 1.5-2:1. It is possible to develop chondrosarcoma at younger age groups, which usually leads to higher malignancy and metastases rates. The sites most often affected are the proximal [[femur]], followed by the proximal [[humerus]].<ref name="p1">Goodman C, Snyder T. Differential Diagnosis for Physical Therapists: Screening for Referral. 5th ed. St. Louis, Mo.: Saunders/Elsevier; 2013. Pg. 521.</ref><ref name="p3">Ferrer-Santacreu E, Ortiz-Cruz E, Díaz-Almirón M, Pozo Kreilinger J. Enchondroma versus Chondrosarcoma in Long Bones of Appendicular Skeleton: Clinical and Radiological Criteria—A Follow-Up. Journal Of Oncology [serial on the Internet]. (2016, Feb 23), [cited April 10, 2016]; 1-10. Available from: Academic Search Complete</ref><ref name=":0" /> | |||
== Clinical Presentation == | |||
== | Patients usually present with [[Pain Assessment|pain]], pathological [[fracture]], a palpable lump or local mass effect. Hyperglycaemia can occur as a [[Paraneoplastic Syndrome|paraneoplastic syndrome]].<ref name=":0" /> | ||
== Diagnosis == | |||
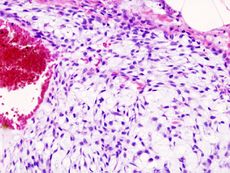
[[File:Chondrosarcoma_histopathic.jpg|alt=|thumb|230x230px|Chondrosarcoma histopathic]] | |||
Imaging tests include: | |||
* Bone scans: Show damage and where the cancer has spread. Hot spots, look dark gray or black on the image. | |||
* CT: Help detect the cancer and see if it moved into other areas. | |||
* MRIs: Show the outline of a tumor. | |||
* PET scans use radioactive tracers to look inside patient and help discover if a tumor is cancer or not. They can also see if it has spread and find its exact location. | |||
* X-rays: Show tumor's location, shape, and size. | |||
* Biopsy: Takes a sample of the tumor to test for cancer. Done with a needle or surgery.<ref>WebMD What Is Chondrosarcoma? Available:https://www.webmd.com/cancer/what-is-chondrosarcoma (accessed 12.9.2022)</ref> | |||
== Medical Management == | |||
== Medical Management | |||
Following a biopsy to confirm the diagnosis, surgery is the most common procedure to remove the tumor. Even for higher grade tumors, limb-sparing curettage (via cryotherapy) is more common, with amputation occurring in rare instances. | Following a biopsy to confirm the diagnosis, surgery is the most common procedure to remove the tumor. Even for higher grade tumors, limb-sparing curettage (via cryotherapy) is more common, with amputation occurring in rare instances. | ||
Unlike most cancers, typical chondrosarcoma does not respond to chemotherapy and is resistant to radiation therapy. Different forms of chondrosarcoma including ''dedifferentiated'' and ''mesenchymal'' may be trial chemotherapy before or after surgery and follow a similar protocol to osteosarcoma and Ewing's sarcoma respectively. Depending on the grading of the sarcoma, proton-beam radiation has had some success, but does require very high doses and is considered less frequently than surgical approaches.<ref name="p7">Treating specific bone cancers [Internet]. Cancer.org. 2016 [cited 10 April 2016]. Available from: http://www.cancer.org/cancer/bonecancer/detailedguide/bone-cancer-treating-treating-specific-bone-cancers</ref><ref name="p2"> | Unlike most cancers, typical chondrosarcoma does not respond to chemotherapy and is resistant to radiation therapy. Different forms of chondrosarcoma including ''dedifferentiated'' and ''mesenchymal'' may be trial chemotherapy before or after surgery and follow a similar protocol to osteosarcoma and Ewing's sarcoma respectively. Depending on the grading of the sarcoma, proton-beam radiation has had some success, but does require very high doses and is considered less frequently than surgical approaches.<ref name="p7">Treating specific bone cancers [Internet]. Cancer.org. 2016 [cited 10 April 2016]. Available from: http://www.cancer.org/cancer/bonecancer/detailedguide/bone-cancer-treating-treating-specific-bone-cancers</ref><ref name="p2">What is bone cancer? [Internet]. Cancer.org. 2016 [cited 10 April 2016]. Available from: http://www.cancer.org/cancer/bonecancer/detailedguide/bone-cancer-what-is-bone-cancer</ref> | ||
== Physical Therapy Management | == Physical Therapy Management == | ||
Physical therapy management will most often occur following surgery to excise the tumor. Depending on the site of the lesion, the surgeon may have different protocols, but physical therapy can focus on treatments that will decrease pain, decrease edema, and improve patients' quality of life. | Physical therapy management will most often occur following surgery to excise the tumor. Depending on the site of the lesion, the surgeon may have different protocols, but physical therapy can focus on treatments that will decrease pain, decrease [[Oedema Assessment|edema]], and improve patients' [[Quality of Life|quality of life]]. | ||
Following surgery, an acute care physical therapist will teach the patient skills like bed mobility, weight bearing precautions, ambulation, and stair negotitation. In outpatient physical therapy, the patient will undergo manual therapy and soft tissue mobilization to improve tissue extensibility, reduce edema, and improve range of motion. The patient will also perform | Following surgery, an acute care physical therapist will teach the patient skills like bed mobility, weight bearing precautions, ambulation, and stair negotitation. In outpatient physical therapy, the patient will undergo manual therapy and soft tissue mobilization to improve tissue extensibility, reduce edema, and improve range of motion. The patient will also perform t[[Therapeutic Exercise|herapuetic exercises]] to increase range of motion and muscle strength to address deficits normally seen following surgery. [[Gait]] training will continue to be incorportated and adapted to the changing weight bearing precautions set forth by the surgeon. As the patient progresses, the treatments will progress to become more functional and incorporate activities that are important to the patient.<ref name="p4">Heick J, Bustillo K, Farris J. Recognition of signs and symptoms of a Type 1 chondrosarcoma: a case report. Physiotherapy Theory & Practice [serial on the Internet]. (2014, Jan), [cited April 10, 2016]; 30(1): 49-55. Available from: Academic Search Complete</ref> | ||
== Alternative/Holistic Management | == Alternative/Holistic Management == | ||
Currently, there are no evidence based, documented reports of alternative/holistic management for chondrosarcoma. | Currently, there are no evidence based, documented reports of alternative/holistic management for chondrosarcoma. | ||
| Line 115: | Line 46: | ||
== Differential Diagnosis == | == Differential Diagnosis == | ||
Chondrosarcoma presents similarly to other musculoskeletal injuries/illnesses of the affected joint. For example, a patient with chondrosarcoma of the hip will complain of intermittenet anterior thigh/hip pain. The pain can present as either hip joint in origin or nonarticular hip origin. Other diagnoses with pain of hip joint origin include osseus necrosis, stress fracture, hip dysplasia, or intra-articular pathology (labral tear, ligamentum teres tear, or loose body in the joint). Diagnoses of nonarticular hip origin of pain include bursitis, tendonopathy, muscle strain, urogenital conditions, metabolic disease, vascular conditions, or infection.<ref name="p3" | Chondrosarcoma presents similarly to other musculoskeletal injuries/illnesses of the affected joint. For example, a patient with chondrosarcoma of the hip will complain of intermittenet anterior thigh/hip pain. The pain can present as either hip joint in origin or nonarticular hip origin. Other diagnoses with pain of hip joint origin include osseus necrosis, stress fracture, hip dysplasia, or intra-articular pathology (labral tear, ligamentum teres tear, or loose body in the joint). Diagnoses of nonarticular hip origin of pain include bursitis, tendonopathy, muscle strain, urogenital conditions, metabolic disease, vascular conditions, or infection.<ref name="p3" /> | ||
== Case Reports == | == Case Reports == | ||
Ferrer-Santacreu E, Ortiz-Cruz E, Díaz-Almirón M, Pozo Kreilinger J. Enchondroma versus Chondrosarcoma in Long Bones of Appendicular Skeleton: Clinical and Radiological Criteria—A Follow-Up. Journal Of Oncology [serial on the Internet]. (2016, Feb 23), [cited April 10, 2016]; 1-10. Available from: Academic Search Complete.<br> | Ferrer-Santacreu E, Ortiz-Cruz E, Díaz-Almirón M, Pozo Kreilinger J. Enchondroma versus Chondrosarcoma in Long Bones of Appendicular Skeleton: Clinical and Radiological Criteria—A Follow-Up. Journal Of Oncology [serial on the Internet]. (2016, Feb 23), [cited April 10, 2016]; 1-10. Available from: Academic Search Complete.<br> | ||
== References == | == References == | ||
| Line 140: | Line 57: | ||
<references /> | <references /> | ||
[[Category:Oncology]] | |||
[[Category:Bone - Conditions]] | |||
Latest revision as of 12:38, 16 September 2022
Original Editors - Students from Bellarmine University's Pathophysiology of Complex Patient Problems project.
Top Contributors - Dalton O'Brien, Corey Hardesty, Lucinda hampton, Nikhil Benhur Abburi, 127.0.0.1, Admin, WikiSysop, Kim Jackson, Elaine Lonnemann, Vidya Acharya and Rewan Elsayed Elkanafany
Introduction[edit | edit source]
Chondrosarcomas are malignant cartilaginous tumours, accounting for ~25% of all primary malignant bone tumours. They are most commonly found in older patients, most commonly effecting the pelvis, sternum, scapula, or cartilage of long bones in the extremities.
Typically, chondrosarcoma forms within bone or cartilage cells around the articular surfaces and can be either slow-growing and form spontaneously, or due to malignant changes in a preexisting (secondary) bone tumour.[1][2]
Epidemiology[edit | edit source]
The typical presentation is in the 4th and 5th decades and there is a slight male predominance of 1.5-2:1. It is possible to develop chondrosarcoma at younger age groups, which usually leads to higher malignancy and metastases rates. The sites most often affected are the proximal femur, followed by the proximal humerus.[1][3][2]
Clinical Presentation[edit | edit source]
Patients usually present with pain, pathological fracture, a palpable lump or local mass effect. Hyperglycaemia can occur as a paraneoplastic syndrome.[2]
Diagnosis[edit | edit source]
Imaging tests include:
- Bone scans: Show damage and where the cancer has spread. Hot spots, look dark gray or black on the image.
- CT: Help detect the cancer and see if it moved into other areas.
- MRIs: Show the outline of a tumor.
- PET scans use radioactive tracers to look inside patient and help discover if a tumor is cancer or not. They can also see if it has spread and find its exact location.
- X-rays: Show tumor's location, shape, and size.
- Biopsy: Takes a sample of the tumor to test for cancer. Done with a needle or surgery.[4]
Medical Management[edit | edit source]
Following a biopsy to confirm the diagnosis, surgery is the most common procedure to remove the tumor. Even for higher grade tumors, limb-sparing curettage (via cryotherapy) is more common, with amputation occurring in rare instances.
Unlike most cancers, typical chondrosarcoma does not respond to chemotherapy and is resistant to radiation therapy. Different forms of chondrosarcoma including dedifferentiated and mesenchymal may be trial chemotherapy before or after surgery and follow a similar protocol to osteosarcoma and Ewing's sarcoma respectively. Depending on the grading of the sarcoma, proton-beam radiation has had some success, but does require very high doses and is considered less frequently than surgical approaches.[5][6]
Physical Therapy Management[edit | edit source]
Physical therapy management will most often occur following surgery to excise the tumor. Depending on the site of the lesion, the surgeon may have different protocols, but physical therapy can focus on treatments that will decrease pain, decrease edema, and improve patients' quality of life.
Following surgery, an acute care physical therapist will teach the patient skills like bed mobility, weight bearing precautions, ambulation, and stair negotitation. In outpatient physical therapy, the patient will undergo manual therapy and soft tissue mobilization to improve tissue extensibility, reduce edema, and improve range of motion. The patient will also perform therapuetic exercises to increase range of motion and muscle strength to address deficits normally seen following surgery. Gait training will continue to be incorportated and adapted to the changing weight bearing precautions set forth by the surgeon. As the patient progresses, the treatments will progress to become more functional and incorporate activities that are important to the patient.[7]
Alternative/Holistic Management[edit | edit source]
Currently, there are no evidence based, documented reports of alternative/holistic management for chondrosarcoma.
Differential Diagnosis[edit | edit source]
Chondrosarcoma presents similarly to other musculoskeletal injuries/illnesses of the affected joint. For example, a patient with chondrosarcoma of the hip will complain of intermittenet anterior thigh/hip pain. The pain can present as either hip joint in origin or nonarticular hip origin. Other diagnoses with pain of hip joint origin include osseus necrosis, stress fracture, hip dysplasia, or intra-articular pathology (labral tear, ligamentum teres tear, or loose body in the joint). Diagnoses of nonarticular hip origin of pain include bursitis, tendonopathy, muscle strain, urogenital conditions, metabolic disease, vascular conditions, or infection.[3]
Case Reports[edit | edit source]
Ferrer-Santacreu E, Ortiz-Cruz E, Díaz-Almirón M, Pozo Kreilinger J. Enchondroma versus Chondrosarcoma in Long Bones of Appendicular Skeleton: Clinical and Radiological Criteria—A Follow-Up. Journal Of Oncology [serial on the Internet]. (2016, Feb 23), [cited April 10, 2016]; 1-10. Available from: Academic Search Complete.
References[edit | edit source]
see adding references tutorial.
- ↑ 1.0 1.1 Goodman C, Snyder T. Differential Diagnosis for Physical Therapists: Screening for Referral. 5th ed. St. Louis, Mo.: Saunders/Elsevier; 2013. Pg. 521.
- ↑ 2.0 2.1 2.2 Radiopedia Chondrosarcoma Available:https://radiopaedia.org/articles/chondrosarcoma (accessed 12.9.2022)
- ↑ 3.0 3.1 Ferrer-Santacreu E, Ortiz-Cruz E, Díaz-Almirón M, Pozo Kreilinger J. Enchondroma versus Chondrosarcoma in Long Bones of Appendicular Skeleton: Clinical and Radiological Criteria—A Follow-Up. Journal Of Oncology [serial on the Internet]. (2016, Feb 23), [cited April 10, 2016]; 1-10. Available from: Academic Search Complete
- ↑ WebMD What Is Chondrosarcoma? Available:https://www.webmd.com/cancer/what-is-chondrosarcoma (accessed 12.9.2022)
- ↑ Treating specific bone cancers [Internet]. Cancer.org. 2016 [cited 10 April 2016]. Available from: http://www.cancer.org/cancer/bonecancer/detailedguide/bone-cancer-treating-treating-specific-bone-cancers
- ↑ What is bone cancer? [Internet]. Cancer.org. 2016 [cited 10 April 2016]. Available from: http://www.cancer.org/cancer/bonecancer/detailedguide/bone-cancer-what-is-bone-cancer
- ↑ Heick J, Bustillo K, Farris J. Recognition of signs and symptoms of a Type 1 chondrosarcoma: a case report. Physiotherapy Theory & Practice [serial on the Internet]. (2014, Jan), [cited April 10, 2016]; 30(1): 49-55. Available from: Academic Search Complete