Breast Cancer Patients - Musculoskeletal Problems Experienced: Difference between revisions
Kim Jackson (talk | contribs) m (Text replacement - "[[Adhesive Capsulitis" to "[[Frozen Shoulder") |
Chloe Waller (talk | contribs) (Updated introduction) |
||
| Line 6: | Line 6: | ||
== Introduction == | == Introduction == | ||
[[File:MSK conditions group1.png|right|frameless|334x334px]] | [[File:MSK conditions group1.png|right|frameless|334x334px]] | ||
[[Breast Cancer|Breast cancer]] and its treatment, usually localised surgery with [[Chemotherapy Side Effects and Syndromes|chemotherapy]], radiotherapy and [[Endocrine System|endocrine]] therapy, increase the risk of [[Musculoskeletal Orthopaedic Assessment|musculoskeletal]] problems, especially in the upper limb<ref>Richmond H et al, [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6006920/ PROSPER Study Group. Development of an exercise intervention for the prevention of musculoskeletal shoulder problems after breast cancer treatment: the prevention of shoulder problems trial (UK PROSPER).] BMC Health Serv Res. 2018 Jun 18;18(1):463</ref>. Research suggests 67% of women may have shoulder or arm problems up to 3 years after treatment<ref name=":1">Bruce J, Williamson E, Lait C on behalf of the PROSPER Study Group'', et al.'' [https://bmjopen.bmj.com/content/8/3/e019078 Randomised controlled trial of exercise to prevent shoulder problems in women undergoing breast cancer treatment: study protocol for the prevention of shoulder problems trial (UK PROSPER).] ''BMJ Open'' 2018;'''8:'''e019078</ref>These include: | |||
* Acute or chronic [[Pain Assessment|pain]]<ref name=":2">Ballinger TJ, Thompson WR, Guise TA. [https://pubmed.ncbi.nlm.nih.gov/36419084/ The bone-muscle connection in breast cancer: implications and therapeutic strategies to preserve musculoskeletal health.] Breast Cancer Res. 2022 Nov 23;24(1):84.</ref> | |||
* [[Muscle]] weakness<ref name=":2" /> | |||
* [[Osteoporosis]] and osteoporotic [[Osteoporotic Vertebral Fractures|fractures]] - certain treatments, such as aromatase inhibitors, or chemotherapy-induced [[Ovarian Cancer|ovarian]] failure, decrease [[estrogen]] and lead to [[bone]] loss<ref>Suskin J, Shapiro CL. [https://pubmed.ncbi.nlm.nih.gov/30175057/ Osteoporosis and musculoskeletal complications related to therapy of breast cancer.] Gland Surg. 2018 Aug;7(4):411-423. </ref> | |||
* Reduced [[shoulder]] [[Range of Motion|range of motion]]<ref name=":1" />due to pain or fear of movement leading to adapting a flexed protective posture or avoidance of use, leading to muscles shortening (especially [[pectoralis major]]) and tightening of the joint capsule.<ref name=":3">Ebaugh, D., Spinelli, B. and Schmitz, K.H. [https://www.sciencedirect.com/science/article/abs/pii/S0306987711002738 Shoulder impairments and their association with symptomatic rotator cuff disease in breast cancer survivors.] 2011. Medical Hypotheses. Vol. 77, p.481–487.</ref> | |||
* Secondary to above, there is risk of shoulder conditions such as symptomatic [[Rotator Cuff|rotator cuff]] disease, [[Scapular Winging|scapula winging]], [[Adhesive Capsulitis|adhesive capsulitis]] or shoulder [[Internal Impingement of the Shoulder|impingement]]<ref name=":3" /><ref name=":0">Pacurar R, Miclaus C, Miclaus M. [https://www.semanticscholar.org/paper/Morbidity-associated-with-breast-cancer-therapy-and-P%C4%83curar-Micl%C4%83u%C5%9F/f4430b180079722a7ad62803bb6e1f64d697cbae Morbidity associated with breast cancer therapy and the place of physiotherapy in its management.] Timisoara Physical Education & Rehabilitation Journal 2011 05;3(6):46-54.</ref> | |||
* [[Lymphoedema]]<ref>Rafn BS, Christensen J, Larsen A, Bloomquist K. [https://pubmed.ncbi.nlm.nih.gov/35077194/ Prospective Surveillance for Breast Cancer-Related Arm Lymphedema: A Systematic Review and Meta-Analysis]. J Clin Oncol. 2022 Mar 20;40(9):1009-1026.</ref> | |||
* Increased [[Body Mass Index|body mass index]] (BMI), which can lead to or exacerbate other musculoskeletal conditions<ref>Leclerc AF et al. [https://pubmed.ncbi.nlm.nih.gov/28322035/ Multidisciplinary rehabilitation program after breast cancer: benefits on physical function, anthropometry and quality of life.] Eur J Phys Rehabil Med. 2017 Oct;53(5):633-642. doi: 10.23736/S1973-9087.17.04551-8. Epub 2017 Mar 20</ref> | |||
* [[Scar Management|Scar]] adhesion<ref name=":0" /> | |||
== Post-Mastectomy Pain Syndrome (PMPS) == | == Post-Mastectomy Pain Syndrome (PMPS) == | ||
Revision as of 13:17, 12 May 2023
Original Editor - Lucinda hampton
Top Contributors - Lucinda hampton, Chloe Waller and Kim Jackson
Introduction[edit | edit source]
Breast cancer and its treatment, usually localised surgery with chemotherapy, radiotherapy and endocrine therapy, increase the risk of musculoskeletal problems, especially in the upper limb[1]. Research suggests 67% of women may have shoulder or arm problems up to 3 years after treatment[2]These include:
- Acute or chronic pain[3]
- Muscle weakness[3]
- Osteoporosis and osteoporotic fractures - certain treatments, such as aromatase inhibitors, or chemotherapy-induced ovarian failure, decrease estrogen and lead to bone loss[4]
- Reduced shoulder range of motion[2]due to pain or fear of movement leading to adapting a flexed protective posture or avoidance of use, leading to muscles shortening (especially pectoralis major) and tightening of the joint capsule.[5]
- Secondary to above, there is risk of shoulder conditions such as symptomatic rotator cuff disease, scapula winging, adhesive capsulitis or shoulder impingement[5][6]
- Lymphoedema[7]
- Increased body mass index (BMI), which can lead to or exacerbate other musculoskeletal conditions[8]
- Scar adhesion[6]
Post-Mastectomy Pain Syndrome (PMPS)[edit | edit source]
Pain which lasts longer than what is usually expected following various breast cancer surgery types. Generally neuropathic in nature, and can be due but not limited to:
- Brachial nerve damage, *Intra-operative compromise of cutaneous innervating,
- Neuroma formation,
- Fibrotic entrapment. Patients often report neurological symptoms such as numbness or pins and needles, stabbing and burning pain to the same side as surgery in or around the surgical sites.
These symptoms can be exacerbated through a lack of pacing, or by lying on the side of surgery. Therefore, patient education, soft tissue massage, and other desensitising techniques are essential [6]. Other common problems include:
- Subacromial Impingement Syndrome.
- Frozen Shoulder (frozen shoulder) – idiopathic or traumatic (post-surgery).
- Rotator Cuff pathology (e.g Symptomatic Rotator Cuff Disease)
- Myofascial Dysfunction Lateral epicondylitis.
- Scapular winging secondary to damage of long thoracic nerve during surgery.
- Pain
Associated Neuromusculoskeletal Conditions Post Treatment[edit | edit source]
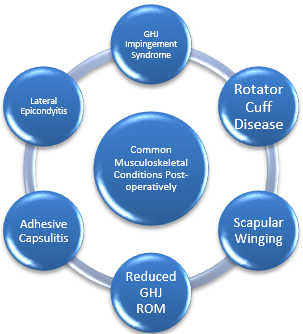
Neuromusculoskeletal conditions are common following surgery, some of which are illustrated in figure 1.4. Treatment protocols shall not be discussed, and the reader should refer to the basic principles of rehabilitation of musculoskeletal conditions. In light of this, it is important to briefly discuss a few points to consider.
- Depending on the type of surgery that the patient needs to undertake, radiotherapy may be necessary following surgery.
- A typical radiotherapy session will require the patient to position the treated arm to 90° flexion and abduction, as well as maximal external rotation, for up to 30 minutes [9]
- Shoulder mobility is commonly affected post-surgery [10]; [11]; [12] so it is vital that physiotherapy aims to restore this to improve patient functional ability and to be able to place the shoulder in the required positions for radiotherapy.
- Active, active assisted, and passive ROM exercises for the shoulder girdle are therefore good practice. Physiotherapy should aim to restore full shoulder ROM as well as minimising associated upper extremity morbidity [13].
- Manual therapy techniques with the aim of further increasing available ROM have been shown to not be of any significant benefit when used in conjunction with active upper limb exercises [14].
References[edit | edit source]
- ↑ Richmond H et al, PROSPER Study Group. Development of an exercise intervention for the prevention of musculoskeletal shoulder problems after breast cancer treatment: the prevention of shoulder problems trial (UK PROSPER). BMC Health Serv Res. 2018 Jun 18;18(1):463
- ↑ 2.0 2.1 Bruce J, Williamson E, Lait C on behalf of the PROSPER Study Group, et al. Randomised controlled trial of exercise to prevent shoulder problems in women undergoing breast cancer treatment: study protocol for the prevention of shoulder problems trial (UK PROSPER). BMJ Open 2018;8:e019078
- ↑ 3.0 3.1 Ballinger TJ, Thompson WR, Guise TA. The bone-muscle connection in breast cancer: implications and therapeutic strategies to preserve musculoskeletal health. Breast Cancer Res. 2022 Nov 23;24(1):84.
- ↑ Suskin J, Shapiro CL. Osteoporosis and musculoskeletal complications related to therapy of breast cancer. Gland Surg. 2018 Aug;7(4):411-423.
- ↑ 5.0 5.1 Ebaugh, D., Spinelli, B. and Schmitz, K.H. Shoulder impairments and their association with symptomatic rotator cuff disease in breast cancer survivors. 2011. Medical Hypotheses. Vol. 77, p.481–487.
- ↑ 6.0 6.1 6.2 Pacurar R, Miclaus C, Miclaus M. Morbidity associated with breast cancer therapy and the place of physiotherapy in its management. Timisoara Physical Education & Rehabilitation Journal 2011 05;3(6):46-54.
- ↑ Rafn BS, Christensen J, Larsen A, Bloomquist K. Prospective Surveillance for Breast Cancer-Related Arm Lymphedema: A Systematic Review and Meta-Analysis. J Clin Oncol. 2022 Mar 20;40(9):1009-1026.
- ↑ Leclerc AF et al. Multidisciplinary rehabilitation program after breast cancer: benefits on physical function, anthropometry and quality of life. Eur J Phys Rehabil Med. 2017 Oct;53(5):633-642. doi: 10.23736/S1973-9087.17.04551-8. Epub 2017 Mar 20
- ↑ Johnson, S. and Musa, I., 2004.Preparation of the breast cancer patient for radiotherapy planning. Physiotherapy. . Vol. 90, no. 4, pp. 195-203.
- ↑ Dahl AA, Nesvold I, Reinertsen KV, Fosså SD. Original Article: Arm/shoulder problems and insomnia symptoms in breast cancer survivors: Cross-sectional, controlled and longitudinal observations. Sleep Med 2011;12:584-590.
- ↑ Freitas-Silva R, de Freitas-Júnior, R. ( 1 ), Conde DM(2), Martinez EZ(3). Comparison of quality of life, satisfaction with surgery and shoulder-arm morbidity in breast cancer survivors submitted to breast-conserving therapy or mastectomy followed by immediate breast reconstruction. Clinics 2010 / 06 / 01 /;65(8):781-787.
- ↑ Harrington S(1), Padua D(2), Myers J(2), Battaglini C(3), Groff D(3), Michener LA(4), et al. Comparison of shoulder flexibility, strength, and function between breast cancer survivors and healthy participants. Journal of Cancer Survivorship 2011 / 06 / 01 /;5(2):167-174.
- ↑ Todd J, Topping A. A survey of written information on the use of post-operative exercises after breast cancer surgery. Physiotherapy 2005;91:87-93.
- ↑ Amaral MTPd, de Oliveira M,Maia Freire, Ferreira NdO, Guimarães R, Vidigal, Sarian L, Otávio, Gurgel MSC. Manual therapy associated with upper limb exercises vs. exercises alone for shoulder rehabilitation in postoperative breast cancer. PHYSIOTHER THEORY PRACT 2012 05;28(4):299-306.