Hypoglycemia
Original Editor - Lucinda hampton
Top Contributors - Lucinda hampton and Aminat Abolade
Introduction[edit | edit source]
Hypoglycaemia, sometimes called a hypo or low, is a condition that occurs when a person’s blood glucose level (BGL) has dropped too low, below 4mmol/L.
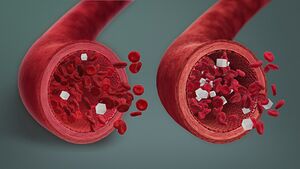
Image1: 3D medical animation still showing low blood sugar level(L) and normal blood sugar level(R).
- It is important to treat a hypo quickly to stop the BGL from falling even lower and the person becoming seriously unwell[1].
- Signs and symptoms may not occur until plasma glucose concentrations drop below 3mmol/L
Glucose is the primary metabolic fuel for the brain under physiologic conditions. Unlike other tissues of the body, the brain is very limited in supplying its glucose. Expectedly, the brain requires a steady supply of arterial glucose for adequate metabolic function. Potential complications can arise from an interruption in the glucose supply[2].
Hypoglycemia is common with type 1 diabetes, particularly in those patients receiving intensive insulin therapy. Patients with type II diabetes experience hypoglycemia relatively less frequently compared to patients with type I diabetes[2].
Pathophysiology[edit | edit source]
The body has inherent counter-regulatory mechanisms to prevent hypoglycemic episodes. All of these counter-regulatory mechanisms include an interplay of hormones and neural signals to regulate the release of endogenous insulin, to increase hepatic glucose output, and to alter peripheral glucose utilization. Among the counter-regulatory mechanisms, the regulation of insulin production plays a major role. Decreases in insulin production as a response to low serum glucose are the body's first line of defense against hypoglycemia.
The decrease in insulin production occurs while the glucose level is in the low-normal range. This serves as a distinctive feature compared to other counter-regulatory measures. Additional counter-regulatory measures typically occur once the serum glucose levels decrease beyond the physiologic range. Among the additional counter-regulatory mechanisms, pancreatic alpha cell secretion of glucagon is the next line of defense against hypoglycemia. Should increased glucagon fail to achieve normal blood sugar levels, adrenomedullary epinephrine is secreted. All three counter-regulatory measures occur in the acute stage of hypoglycemia.
The previously mentioned counter-regulatory mechanisms may fail to resolve the hypoglycemia. Further counter-regulatory measures are employed in the form of growth hormone and cortisol. Both the release of growth hormone and cortisol are seen in prolonged hypoglycemic states.[2]
Education[edit | edit source]
Patient education remains a pivotal component in the prevention of hypoglycemic episodes. Focus on preventing hypoglycemia should include patient education on signs and symptoms that constitute hypoglycemia and early recognition of these signs and symptoms. Patients may also need counsel on meal plans and exercise to manage their condition.[2]
Causes of Hypoglycaemia[edit | edit source]
In patients who do not have diabetes, hypoglycemia is uncommon, but when it occurs, there are a few major causes of hypoglycemia: pharmacologic, alcohol, critical illness, counter-regulatory hormone deficiencies, and non-islet cell tumors[2].
Causes include;
- Too much insulin or other glucose lowering diabetes tablets
- Delaying or missing a meal
- Not eating enough carbohydrate
- Unplanned physical activity
- More strenuous exercise than usual
- Drinking alcohol – the risk of hypoglycaemia is increased with more alcohol consumed[1]
Treatment[edit | edit source]
- Severe hypoglycemia can be treated with intravenous (IV) dextrose followed by infusion of glucose.
- For conscious patients able to take oral (PO) medications, readily absorbable carbohydrate sources (such as fruit juice) should be given.
- For patients unable to take oral agents, a 1-mg intramuscular (IM) injection of glucagon can be administered.
- Once the patient is more awake, a complex carbohydrate food source should be given to the patient to achieve sustained normal blood glucose levels. More frequent blood glucose monitoring should occur to rule out further drops in blood sugar.
Most cases of hypoglycemia can be managed conservatively. Recurrent episodes of hypoglycemia with no apparent or obvious cause may warrant specialty consultation with an endocrinologist. Consultation with a diabetic educator may also be beneficial for the long-term management of diabetes and hypoglycemia.
Physiotherapy[edit | edit source]
In treatment of diabetic clients - Whilst exercising, the therapist should watch the patient for symptoms of hypoglycemia including anxiety, tingling and numbness in the arms and legs, chills, sweats, and unsteady gait.
References[edit | edit source]
- ↑ 1.0 1.1 Diabetes Australia Hypoglycemia Available: https://www.diabetesaustralia.com.au/living-with-diabetes/managing-your-diabetes/hypoglycaemia/ (accessed 26.9.2021)
- ↑ 2.0 2.1 2.2 2.3 2.4 Mathew P, Thoppil D. Hypoglycemia.2018 Available: https://www.ncbi.nlm.nih.gov/books/NBK534841/ (accessed 26.9.2021)