Anticipatory Care for Long Term Conditions in Physiotherapy: Difference between revisions
No edit summary |
No edit summary |
||
| Line 15: | Line 15: | ||
=== Stats and Facts === | === Stats and Facts === | ||
* | *Long-term conditions are responsible for 41 million deaths each year, accounting for 70% of all deaths around the globe.<ref name=":0" /> The number is estimated to reach up to 52 million by 2030.<ref>Kelland K. Chronic disease to cost $47 trillion by 2030: WEF. Reuters 2011. Available from: https://www.reuters.com/article/us-disease-chronic-costs-idUSTRE78H2IY20110918 (Accessed 20 May 2020)</ref> | ||
* Based on information from the World Health Organization, [[Cardiovascular Disease| | * Based on information from the World Health Organization, [[Cardiovascular Disease|cardiovascular disease]]<nowiki/> accounts for most NCDs deaths, or 17.9 million people annually, followed by cancers (9.0 million), respiratory diseases (3.9 million), and diabetes (1.6 million)<ref name=":0" /> | ||
* 15% of young adults aged 11-15 have an LTCs<ref name=":1">Pharmaceutical Services Negotiating Committee. Essential facts, stats and quotes relating to long-term conditions. Available from:http://psnc.org.uk/services-commissioning/essential-facts-stats-and-quotes-relating-to-long-term-conditions/ (accessed 20 May 2020)</ref> | * 15% of young adults aged 11-15 have an LTCs<ref name=":1">Pharmaceutical Services Negotiating Committee. Essential facts, stats and quotes relating to long-term conditions. Available from:http://psnc.org.uk/services-commissioning/essential-facts-stats-and-quotes-relating-to-long-term-conditions/ (accessed 20 May 2020)</ref> | ||
* 15 million of all deaths attributed to NCDs occur between the ages of 30 and 69 years<ref name=":0" /> | * 15 million of all deaths attributed to NCDs occur between the ages of 30 and 69 years<ref name=":0" /> | ||
| Line 38: | Line 38: | ||
* Example: individuals from marginalised groups are more likely to smoke and have more difficulty quitting. While there is a general decline in the number of people smoking, "socioeconomic inequities in smoking prevalence and cancer mortality are widening."<ref>Potter LN, Lam CY, Cinciripini PM, Wetter DW. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7789945/ Intersectionality and smoking cessation: exploring various approaches for understanding health inequities]. Nicotine Tob Res. 2021 Jan 7;23(1):115-123. </ref> | * Example: individuals from marginalised groups are more likely to smoke and have more difficulty quitting. While there is a general decline in the number of people smoking, "socioeconomic inequities in smoking prevalence and cancer mortality are widening."<ref>Potter LN, Lam CY, Cinciripini PM, Wetter DW. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7789945/ Intersectionality and smoking cessation: exploring various approaches for understanding health inequities]. Nicotine Tob Res. 2021 Jan 7;23(1):115-123. </ref> | ||
<u>The World Health Organization | <u>The World Health Organization classifies LTCs contributing factors into the following categories</u><ref name=":0" /><u>:</u> | ||
'''Modifiable behavioral risk factors:''' | '''Modifiable behavioral risk factors:''' | ||
| Line 44: | Line 44: | ||
* Excess salt/sodium intake | * Excess salt/sodium intake | ||
* [[Alcoholism|Alcohol]] use | * [[Alcoholism|Alcohol]] use | ||
* Lack of, or [[Physical Inactivity| | * Lack of, or insufficient, [[Physical Inactivity|physical activity]] | ||
'''Metabolic risk factors:''' | '''Metabolic risk factors:''' | ||
* [[Blood Pressure|Hypertension]] | * [[Blood Pressure|Hypertension]] | ||
| Line 50: | Line 50: | ||
* [[hyperglycemia]] (high blood glucose levels) | * [[hyperglycemia]] (high blood glucose levels) | ||
* [[hyperlipidemia]] (high levels of fat in the blood) | * [[hyperlipidemia]] (high levels of fat in the blood) | ||
'''Environmental risk factors:''' | |||
* Air pollution | |||
** accounts for 6.7 million deaths globally, 5.7 million of which are due to NCDs, such as stroke, ischaemic heart disease, chronic obstructive pulmonary disease, and lung cancer | |||
== Impacts on Individual and Society == | == Impacts on Individual and Society == | ||
Revision as of 23:49, 29 October 2023
Original Editor - Mariam Hashem
Top Contributors - Mariam Hashem, Jess Bell, Kim Jackson, Lucinda hampton, Tony Lowe, Tarina van der Stockt, Vidya Acharya and Olajumoke Ogunleye
Introduction[edit | edit source]
Long-term conditions (LTCs), also known as chronic diseases or non-communicable diseases (NCDs),[1] are defined as a physical or mental health conditions that require management over a long period of time.[2] These conditions currently have no cure, but can be managed/controlled by medication and other interventions.[3] They are chronic conditions that cannot be passed on from one person to another. They are caused by various factors, including genetics, physiology, the environment and an individual's behaviour.[4]
Examples:
- Heart disease
- Stroke
- Cancer
- Diabetes
- Chronic lung diseases like chronic obstructive pulmonary disease and asthma
Stats and Facts[edit | edit source]
- Long-term conditions are responsible for 41 million deaths each year, accounting for 70% of all deaths around the globe.[1] The number is estimated to reach up to 52 million by 2030.[5]
- Based on information from the World Health Organization, cardiovascular disease accounts for most NCDs deaths, or 17.9 million people annually, followed by cancers (9.0 million), respiratory diseases (3.9 million), and diabetes (1.6 million)[1]
- 15% of young adults aged 11-15 have an LTCs[6]
- 15 million of all deaths attributed to NCDs occur between the ages of 30 and 69 years[1]
- An estimated 1·7 million (4% of NCD deaths) occurred in people aged less than 30 years[7]
- In Scotland, LTCs account for 80% of all GP consultations and patients with these conditions are twice as likely to be admitted to hospital[8]
- In England, it is estimated that only 59% of people living with LTCs are in work, compared with 72% of the general population[6]
- NCDs disproportionately affect people in low- and middle-income countries.[1][7][9][10] It has been projected that, by 2040, low- and middle-income countries will see significant increases in disability, illness, and premature deaths from NCDs[11]
Causes and Risk Factors[edit | edit source]
"The main aetiology of long-term conditions are unhealthy or harmful behaviours. [...] Another factor to take in consideration for long-term conditions are health inequalities, which refers to the unfair and avoidable repartition of health outcomes in the population."[12] -- Matthieu Haentjens
Unhealthy or harmful behaviours:
- Harmful behaviours contribute to LTCs. These include sedentary lifestyles, unhealthy diets, exposure to tobacco smoke or the harmful use of alcohol[1]
- A 2019 population-based cohort study found that the absence of three risk factors (smoking, hypertension, and being overweight) delayed the onset of NCDs by nine years in individuals aged more than 45 years[13]
- Similarly, a lack of smoking, hypertension, and being overweight is related to a longer life expectancy (around six years) and it reduces the amount of time spent living with a NCD by around 2 years[13]
"These findings underscore the potential to substantially reduce premature NCD morbidity and mortality in the general population through prevention of smoking, hypertension, and overweight."[13]
Health inequalities:
- Defined by the World Health Organization as: "avoidable inequalities in health between groups of people within countries and between countries. These inequities arise from inequalities within and between societies."[14]
- The COVID-19 pandemic helped uncover and highlight numerous health inequalities. In the United Kingdon, the pandemic disproportionately affected "individuals from black and minority ethnic groups, poorer socioeconomic backgrounds, urban and rurally deprived locations, and vulnerable groups of society"[15]
- Example: individuals from marginalised groups are more likely to smoke and have more difficulty quitting. While there is a general decline in the number of people smoking, "socioeconomic inequities in smoking prevalence and cancer mortality are widening."[16]
The World Health Organization classifies LTCs contributing factors into the following categories[1]:
Modifiable behavioral risk factors:
- Tobacco (including second-hand smoking)
- Excess salt/sodium intake
- Alcohol use
- Lack of, or insufficient, physical activity
Metabolic risk factors:
- Hypertension
- overweight/obesity
- hyperglycemia (high blood glucose levels)
- hyperlipidemia (high levels of fat in the blood)
Environmental risk factors:
- Air pollution
- accounts for 6.7 million deaths globally, 5.7 million of which are due to NCDs, such as stroke, ischaemic heart disease, chronic obstructive pulmonary disease, and lung cancer
Impacts on Individual and Society[edit | edit source]
Long-term conditions are associated with multimorbidities that impact the quality of life of the individual and burdens the healthcare system.
People with multimorbidities have poorer functional status, quality of life, working capacity and health outcomes than are those without multimorbidity[17].
LTCs can negatively affect the individual's mobility and result in social consequences such as home-bounding, self-care disability and bed-bounding, the ultimate consequences being social isolation, family conflicts and even stigma[18].
Coping with the long-term conditions might be difficult and can be stressing or disabling. Lost of interest, feeling guilty or responsible and low self-esteem can worsen the development of the disease. The person might also lose the ability to engage in activities that bring a sense of meaning and purpose to life[19].
The economic burden of LTCs is significant. The United Nations has estimated that the cumulative loss to the global economy could reach $47 trillion by 2030 due to LTCs[20].
The estimated cost of long-term conditions care in the UK was at £320 million in 2017[2].
Healthcare Policies[edit | edit source]
The role of behavioral factors in developing LTCs is significant. Altering these factors can help in the prevention and management of these conditions.
The healthcare model is supporting the prevention and anticipatory care of LTCs by preventive measures, health promotion and encouraging patient's advocacy[2].
Making every contact count (MECC) is an approach to behavior change that encourages healthcare professionals to utilise day to day interactions to promote changes in behavior that have a positive effect on the health and well being of individuals, communities and populations.[21][22]
MECC focuses on lifestyle changes that can influence the health of individuals such as:
- Stopping smoking
- Limit alcohol drinking to the recommended limits
- Healthy eating - healthy diets, such as the Mediterranean diet and the New Nordic diet have been proposed as ways of reducing risk factors associated with NCD[23]
- Physical Activity
- Keeping a healthy weight
- Mental health and well being
Read more about MECC here.
The MECC model was integrated into the physiotherapy practice by several organizations and had successful outcomes on improving the health conversation and promoting physical activities[24].
Physiotherapy and Health Promotion[edit | edit source]
Physiotherapy has an important role in the prevention of LTCs throughout different stages[2]:
- Medial Prevention by utilizing different intervention in cardiac rehabilitation for cardiac diseases
- Behavioral prevention by supporting individuals and encourage healthy lifestyle measures
- Social/environmental by education on environmental measures and supporting occupational policies
Making Every Contact Count model can be integrated into physiotherapy practise on four stages[2]:
- Screening of health status and identifying areas of change
- Agenda setting by discussing needed changes with the patient
- Readiness to change by discussing and assessing obstacles to change
- Goal setting using SMART goals
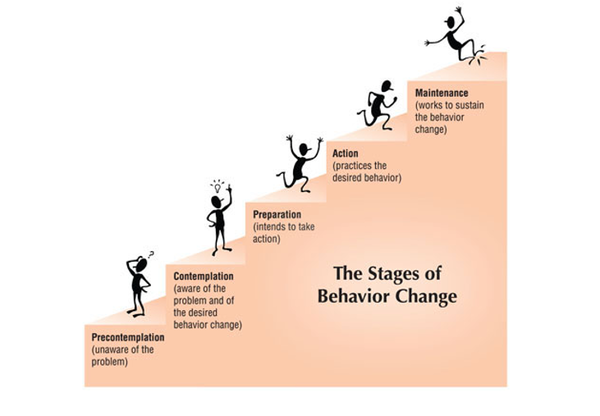
Mental readiness can be an obstacle to lifestyle changes. There are six stages of mental preparation that physiotherapists need to be aware of to help their patients improving their health and well being[2]:
- Precontemplation: the patient is aware of the problem but not willing to take an action
- Contemplation: the patient is aware of the road to change
- Preparation: physiotherapists can help by using SMART goals
- Action plan: based on identified goals
- Maintenance: where most people fail. Physiotherapists can help by encouraging and supporting the patient's commitment
- Relapse: if it happens, physiotherapists can help by reassessing and setting new goals
Self-management:[edit | edit source]
Self-management is a powerful tool that enables patients to take control of their treatment by actively cooperating to take actions toward their recovery.[2]
The role of physiotherapy in self-management:[2]
- support patients to get a proper diagnosis and understand the pathology clearly
- communicating with patients using open-ended questions that encourage patients to engage and reflect on their lifestyle and behavior
- setting goals to show patients their potentials
- Utilize digital/telehealth: to sympathize and connect with patients easily especially when traveling/commuting is challenging. The availability of videos and pictures can make treatment simpler and easy to understand. Smartphone applications offer an easy and accessible interface and offer a range of technologies that facilitate participation in the treatment plan such as exercise templates, online agenda, feedback in real-time and monitoring vitals. However, the use of digital health has some downside such as the risk of breaching data and compromising patient's privacy and the associated high cost, especially in low resource settings.
- Promoting the use of self-testing and vital signs kits for Diabetes and Blood Pressure
- Utilization of screening tests to help identify risks such as walking speed test and get up and go test
- Working in an integrated care team and using an effective referral scheme to connect patients with other services and direct them to support when needed[2]
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 World Health Organization. Noncommunicable diseases. Available from:https://www.who.int/news-room/fact-sheets/detail/noncommunicable-diseases (Accessed 20 May 2020)
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 2.6 2.7 2.8 Haentjens M. Anticipatory Care for Long Term Conditions in Physiotherapy. Plus course 2020
- ↑ Ambrosio L, Hislop-Lennie K, Barker H, Culliford D, Portillo MC. Living with Long term condition Scale: A pilot validation study of a new person centred tool in the UK. Nurs Open. 2021 Jul;8(4):1909-19.
- ↑ Tabish SA. Lifestyle diseases: consequences, characteristics, causes and control. Journal of Cardiology & Current Research. 2017;9(3): 326-9.
- ↑ Kelland K. Chronic disease to cost $47 trillion by 2030: WEF. Reuters 2011. Available from: https://www.reuters.com/article/us-disease-chronic-costs-idUSTRE78H2IY20110918 (Accessed 20 May 2020)
- ↑ 6.0 6.1 Pharmaceutical Services Negotiating Committee. Essential facts, stats and quotes relating to long-term conditions. Available from:http://psnc.org.uk/services-commissioning/essential-facts-stats-and-quotes-relating-to-long-term-conditions/ (accessed 20 May 2020)
- ↑ 7.0 7.1 NCD Countdown 2030 collaborators. NCD Countdown 2030: worldwide trends in non-communicable disease mortality and progress towards Sustainable Development Goal target 3.4. Lancet. 2018;392(10152):1072-88.
- ↑ Scotland A. Managing long-term conditions. Edinburgh: Audit Scotland. 2007.
- ↑ Kazibwe J, Tran PB, Annerstedt KS. The household financial burden of non-communicable diseases in low- and middle-income countries: a systematic review. Health Res Policy Syst. 2021 Jun 21;19(1):96.
- ↑ Bharatan T, Devi R, Huang PH, Javed A, Jeffers B, Lansberg P, et al. A methodology for mapping the patient journey for noncommunicable diseases in low- and middle-income countries. J Healthc Leadersh. 2021 Jan 29;13:35-46.
- ↑ Reeve B, Gostin LO. "Big" Food, Tobacco, and Alcohol: Reducing Industry Influence on Noncommunicable Disease Prevention Laws and Policies Comment on "Addressing NCDs: Challenges From Industry Market Promotion and Interferences". Int J Health Policy Manag. 2019;8(7):450-4.
- ↑ Haentjens M. Anticipatory Care for Long Term Conditions in Physiotherapy Course. Plus, 2020.
- ↑ 13.0 13.1 13.2 Licher S, Heshmatollah A, van der Willik KD, Stricker BHC, Ruiter R, de Roos EW et al. Lifetime risk and multimorbidity of non-communicable diseases and disease-free life expectancy in the general population: A population-based cohort study. PLoS Med. 2019;16(2):e1002741.
- ↑ World Health Organization. Social determinants of health: Key concepts. Available from: https://www.who.int/news-room/questions-and-answers/item/social-determinants-of-health-key-concepts (last accessed 30 October 2023).
- ↑ Mishra V, Seyedzenouzi G, Almohtadi A, Chowdhury T, Khashkhusha A, Axiaq A, et al. Health inequalities during COVID-19 and their effects on morbidity and mortality. J Healthc Leadersh. 2021 Jan 19;13:19-26.
- ↑ Potter LN, Lam CY, Cinciripini PM, Wetter DW. Intersectionality and smoking cessation: exploring various approaches for understanding health inequities. Nicotine Tob Res. 2021 Jan 7;23(1):115-123.
- ↑ Prevalence, expenditures, and complications of multiple chronic conditions in the elderly.Arch Intern Med. 2002; 162: 2269-2276
- ↑ Roca M, Mitu O, Roca IC, Mitu F. Chronic Diseases--Medical and Social Aspects. Revista de Cercetare si Interventie Sociala. 2015 Jun 1;49.
- ↑ Roberts L. Psychological Aspects of Chronic Illness. Sheffield APT.Available from: https://www.sth.nhs.uk/clientfiles/File/Mental%20Health%20Awareness%20presentation%20-%20based%20on%20Maria%20and%20Ian's%20POTS%20training.pdf (Accessed 20 May 2020)
- ↑ Institute for Global Health Sciences. Non-communicable Disease Could Cost Global Economy $47 Trillion by 2030. Available from:https://globalhealthsciences.ucsf.edu/news/non-communicable-disease-could-cost-global-economy-47-trillion-2030 (Last Accessed 20 May 2020)
- ↑ Lawrence W, Black C, Tinati T, Cradock S, Begum R, Jarman M,et al. 'Making every contact count': Evaluation of the impact of an intervention to train health and social care practitioners in skills to support health behaviour change. J Health Psychol. 2016 Feb;21(2):138-51.
- ↑ Lussiez A, Hallway A, Lui M, Perez-Escolano J, Sukhon D, Palazzolo W, et al. Evaluation of an Intervention to Address Smoking and Food Insecurity at Preoperative Surgical Clinic Appointments. JAMA Netw Open. 2022 Oct 3;5(10):e2238677.
- ↑ Iriti M, Varoni EM, Vitalini S. Healthy Diets and Modifiable Risk Factors for Non-Communicable Diseases-The European Perspective. Foods. 2020;9(7):940.
- ↑ Cooper-Ryan AM, Ure CM. Making Every Contact Count: Evaluation of the use of MECC within the outpatient MSK Physiotherapy service and Bury Integrated MSK Service at Fairfield General Hospital, part of the Bury and Rochdale Care Organisation which is part of the Northern Care Alliance Group.