Haemorrhoids: Difference between revisions
No edit summary |
Kim Jackson (talk | contribs) No edit summary |
||
| (5 intermediate revisions by 2 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox"> | <div class="editorbox"> | ||
'''Original Editor '''- [[User: | '''Original Editor '''- [[User:Khloud Shreif|Khloud Shreif]] | ||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | ||
</div> | </div> | ||
== Clinically Relevant Anatomy == | |||
The anal canal is the end part of the gastrointestinal tract (GIT), it is about 4cm in length in women and a bit longer in men reaching about 4.4 cm in length, passing downwards and backward forming the anorectal angle. The internal lining mucosa membrane of the anal canal is divided by the pectinate line into two portions: the upper one the vertical anal columns (8-10 anal fold), at there ends there are valves (anal valves), above each one of these anal valves there is a shallow mucosal pocket called the anal sinus. the lower part below the line is formed of nonkeratinized squamous epithelium with no ducts it is sensitive to pain and provides an internal moisturizing to the canal<ref>Bazira PJ. [https://www.sciencedirect.com/science/article/pii/S0263931922002344#sec8 Anatomy of the rectum and anal canal]. Surgery (Oxford). 2022 Dec 7.</ref>. | |||
The upper anal canal is lined by three main anal cushions they are very vascular, and their positions contribute to the anatomy of the anal canal to help with continence, the first one is located in the right anterior at 11 o'clock, the second at the right posterior at 7 o'clock and the last one on the left lateral aspect at 3 o'clock of the anal canal, they consist of [[Connective Tissue|connective tissue]]<nowiki/>s and connection of [[arteries]] and [[veins]], supported by [[Muscle: Smooth|smooth muscle]]<nowiki/>s and connective tissues and supplied by the rectal artery. In addition to the three main cushions, there are many minor cushions between them. | |||
The anal canal is described | The anal canal is described as an anatomical and surgical anal canal. The anatomical anal canal starts from the dentate line and ends at the anal verge, while the surgical anal canal extends from the anorectal ring (junction between the anal canal and rectum) to the anal verge<ref>Lee JM, Kim NK. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5951097/#:~:text=The%20dentate%20line%20is%20the,epithelium%20of%20the%20anal%20canal. Essential anatomy of the anorectum for colorectal surgeons focused on the gross anatomy and histologic findings]. Annals of Coloproctology. 2018 Apr;34(2):59.</ref>. | ||
== Mechanism of Injury / Pathological Process == | == Mechanism of Injury / Pathological Process == | ||
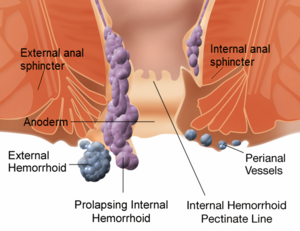
[[File:Internal and external hemorrhoids.png|thumb|Internal and external hemorrhoids]] | |||
Haemorrhoids are defined as a swollen/ enlargement/ or displacement of vascular anal cushions, it may be symptomatic condition or asymptomatic in others that affects millions of people. The exact pathophysiology is still unclear but there are many theories. | |||
'''<u>Sliding theory</u>''' | |||
Sliding of lining anal cushions theory, | Sliding of lining anal cushions theory, which was described in 1975, suggested that haemorrhoids happen when there is break down and downward displacement of structures of internal anal cushions when the supporting structures of anal cushions become weak this will this will predispose to prolapse of anal cushions such as during defecation or an increase of intra-abdominal pressure, theses displacement changes are associated with the [[Inflammation Acute and Chronic|inflammatory]] process of the internal canal, venous dilatation, the process of degeneration of the fibro-elastic and [[collagen]] tissues, vascular thrombosis and/ or anal sub-epithelial muscle this theory still accepted<ref name=":0">Lohsiriwat V. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3342598/ Hemorrhoids: from basic pathophysiology to clinical management.] World journal of gastroenterology: WJG. 2012 May 5;18(17):2009.</ref>. | ||
Hemodynamic | '''<u>Hemodynamic theory</u>''' | ||
Hemodynamic and hypervascularization theory, the anal cushions are supplied by terminal branches of the superior rectal artery, they are larger in diameter that are associated with an increase in the [[Blood Physiology|blood]] flow and venous backflow because of collapsed anastomosis of arteriovenous that lead to enlargement and prolapse of cushions<ref>Lalisang TJ. Hemorrhoid: Pathophysiology and Surgical Management Literature Review. The New Ropanasuri Journal of Surgery. 2016;1(1).</ref>. | |||
The smooth muscles around the arteriovenous plexus act as a sphincter to reduce the arterial inflow of the blood and improve venous drainage and so decreasing the enlargement of arteriovenous plexus and the risk of hemorrhoids is another possible explanation for the pathophysiology of hemorrhoids<ref>Aigner F, Gruber H, Conrad F, Eder J, Wedel T, Zelger B, Engelhardt V, Lametschwandtner A, Wienert V, Böhler U, Margreiter R. Revised morphology and hemodynamics of the anorectal vascular plexus: impact on the course of hemorrhoidal disease. International journal of colorectal disease. 2009 Jan;24:105-13.</ref>. | |||
In a large sample of heamorrhoidal tissues, there was an increase in microvascular density that support the phenomena of neovascularization especially when there is a thrombosis. Several [[enzymes]] and mediators play a role in the development of haemorrhoids such as; angiogenesis-related proteins such as VEGF, matrix metalloproteinase (MMP), and zinc-dependent proteinase that have a degradation and remodeling effect<ref name=":0" />. | |||
'''Internal | === Types of Haemorrhoids === | ||
Haemorrhoids are classified according to the location to pectinate line into: | |||
[[File:Exteranal hemorrhoids.jpg|thumb|External hemorrhoids]] | |||
'''Internal haemorrhoids''' originates from dilatation of the venous plexus above the dentate line and are classified into four grades according to Goligher’s classification: | |||
* Grade I, visible | * Grade I, visible haemorrhoids with no prolapse. | ||
* Grade II, prolapse of anal cushions through the anus at straining or increase of intra-abdominal pressure but they reduce spontaneously. | * Grade II, prolapse of anal cushions through the anus at straining or increase of intra-abdominal pressure but they reduce spontaneously. | ||
* Grade III, prolapse of anal cushions through the anus at straining or increase of intra-abdominal pressure but need manual reduction. | * Grade III, prolapse of anal cushions through the anus at straining or increase of intra-abdominal pressure but need manual reduction. | ||
* Grade IV, | * Grade IV, is nonreducible prolapse. | ||
'''External | '''External haemorrhoids''' originates from dilatation of the venous plexus below the dentate line | ||
=== Risk / Predisposing Factors === | === Risk / Predisposing Factors === | ||
* Activities that increase intra abdominal pressure like weight lifting, straining. | * Activities that increase intra-abdominal pressure like weight lifting, and straining. | ||
* Chronic constipation | * Chronic [[constipation]] | ||
* Pregnancy (constipation or decrease support of connective tissues due to elasticity during pregnancy) | * Pregnancy (constipation or decrease support of connective tissues due to elasticity during pregnancy) | ||
* Prolonged toileting in sitting position that | * Prolonged toileting in a sitting position that leads to disruption of blood backflow | ||
* Bad dietary habits | * Bad dietary habits | ||
* Hard feces (an increase in consistency of stool that make it difficult to pass) or | * Hard feces (an increase in consistency of stool that make it difficult to pass) or diarrhoea. | ||
== Clinical Presentation == | == Clinical Presentation == | ||
In patients | In patients who suffer from haemorrhoids approximately 4 out of 10 will have symptoms. Clinical presentation of the patient depends on the degree and type of haemorrhoids, external haemorrhoids maybe come with acute pain if there is thrombosis, feeling of swelling/lump around the anus, bleeding that is usually painless, bright red bleeding<ref>Aigner F, Gruber H, Conrad F, Eder J, Wedel T, Zelger B, Engelhardt V, Lametschwandtner A, Wienert V, Böhler U, Margreiter R. Revised morphology and hemodynamics of the anorectal vascular plexus: impact on the course of hemorrhoidal disease. International journal of colorectal disease. 2009 Jan;24:105-13.</ref> related to internal haemorrhoids and associated with bowel movement<ref>Margetis N. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6479658/ Pathophysiology of internal hemorrhoids. Annals of gastroenterology.] 2019 Apr 27:264-.</ref>. | ||
== Diagnostic Procedures == | == Diagnostic Procedures == | ||
With external examination to detect if there is any anal discharge, lumps out the anus, thrombosis associated with | * Detailed patient history and physical examination is important to diagnose haemorrhoids ad exclude any possible causes. | ||
* With external examination to detect if there is any anal discharge, lumps out the anus, or thrombosis associated with external haemorrhoids that feel firm, purplish nodule and tender with palpation, fecal soiling, or anal fissure. Digital/ Internal examination we can not detect internal hemorrhoids but we can detect if there is an abnormal internal mass, scar, fistula, or anal stenosis<ref name=":0" /><ref name=":1">Sun Z, Migaly J. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4755769/ Review of hemorrhoid disease: presentation and management. Clinics in colon and rectal surgery]. 2016 Mar;29(01):022-9.</ref>. | |||
* Anoscope procedure is important to be carried if there is bleeding or the digital exam revealed that there is an internal mass and to confirm internal haemorrhoids, it can detect the size, location, and severity of inflammation. In patients above 50 years old total colonoscopy can be done if there is bleeding for exclusion of causes<ref name=":1" />. | |||
== Management / Interventions == | == Management / Interventions == | ||
| Line 56: | Line 61: | ||
=== Conservative management === | === Conservative management === | ||
==== Medical Treatment ==== | |||
* Topical analgesic or anti-inflammatory for acute haemorrhoids | |||
* Phlebotonics that contains plant extracts, it improves lymphatic drainage, and capillary permeability used for 1st and 2nd degree of internal haemorrhoids and during thrombosis episodes. | |||
* [[Corticosteroid Medication|Corticosteroid]] and [[NSAIDs|NSAID]] treatment or laxatives<ref>Higuero T, Abramowitz L, Castinel A, Fathallah N, Hemery P, Duhoux CL, Pigot F, Pillant-Le Moult H, Senéjoux A, Siproudhis L, Staumont G. [https://www.sciencedirect.com/science/article/pii/S187878861600031X#sec0015 Guidelines for the treatment of hemorrhoids.] Journal of visceral surgery. 2016 Jun 1;153(3):213-8.</ref>. | |||
==== Physical Therapy ==== | |||
[[Therapeutic Exercise|Exercise therapy]] and a diet rich in fiber are important to improve and decrease the straining and bearing down with bowel movement. Teaching the patient the proper effective way to breathe in to help relax the pelvic floor muscles during defecation. | |||
==== Non- surgical intervention ==== | Assessment of the anal sphincter is important, and tracking any spasm or incoordination between muscles is important to be treated using [[biofeedback]], soft tissue [[massage]] of tight muscles, and [[Pelvic Floor Anatomy|pelvic floor]] muscle training. | ||
[[Transcutaneous Electrical Nerve Stimulation (TENS)|Transcutaneous electrical nerve stimulation]] (TENS) and other therapeutic pain modalities can be used to relieve pain in patients with haemorrhoids, it is effective for pain relief post-surgical procedures<ref>Chiu JH, Chen WS, Chen CH, Jiang JK, Tang GJ, Lui WY, Lin JK. Effect of transcutaneous electrical nerve stimulation for pain relief on patients undergoing hemorrhoidectomy: a prospective, randomized, controlled trial. Diseases of the colon & rectum. 1999 Feb;42(2):180-5.</ref>. | |||
{{#ev:youtube|qTcb55KOK9Y|300}}<ref>Michelle Kenway. 6 Hemorrhoid Fixes for PAIN & BLEEDING - Complete Physiotherapy Guide to HOME REMEDY Hemorrhoids. Available from: http://www.youtube.com/watch?v=qTcb55KOK9Y[last accessed 24/6/2023]</ref> | |||
==== Non-surgical intervention ==== | |||
* [https://www.nice.org.uk/guidance/ipg525/chapter/3-The-procedure '''Electrotherapy'''] | * [https://www.nice.org.uk/guidance/ipg525/chapter/3-The-procedure '''Electrotherapy'''] | ||
Known as | Known as electrocoagulation in the outpatient setting using an anoscope a probe carrying a direct electric current with intensity between 8 mA and 16 mA will be directed to the base of the hemorrhoid, the time of the session depends on the grade, it is used as an alternative procedure for grade I or II and can be used for grade III or IV as an alternative to surgery. | ||
* '''Sclerotherapy''' | * '''Sclerotherapy''' | ||
It uses chemicals such as zinc chloride, quinine, and polidocanol to be injected into hemorrhoidal tissues this is used to decrease the vascularity, and redundant tissue | It uses chemicals such as zinc chloride, quinine, and polidocanol to be injected into hemorrhoidal tissues this is used to decrease the vascularity, and redundant tissue and gradually hemorrhoid will shrink and obliterates over time, used in grade I and II internal hemorrhoids with no need to anesthesia during the procedure<ref>He A, Chen M. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9022405/ Sclerotherapy in hemorrhoids]. Indian Journal of Surgery. 2023 Apr;85(2):228-32. | ||
</ref>. | </ref>. | ||
| Line 76: | Line 89: | ||
* '''Rubber band ligation''' | * '''Rubber band ligation''' | ||
Using an anoscope the hemorrhoid will be tied at its base by a rubber band to cut the blood supply, within 3 to 7 days later. This prolapsed part of hemorrhoid will fall off<ref>Albuquerque A. Rubber band ligation of hemorrhoids: A guide for complications. World journal of gastrointestinal surgery. 2016 Sep 9;8(9):614.</ref>. | Using an anoscope the hemorrhoid will be tied at its base by a rubber band to cut the blood supply, within 3 to 7 days later. This prolapsed part of the hemorrhoid will fall off<ref>Albuquerque A. Rubber band ligation of hemorrhoids: A guide for complications. World journal of gastrointestinal surgery. 2016 Sep 9;8(9):614.</ref>. | ||
=== Surgical Intervention === | |||
'''Hemorrhoidectomy''' divided into two types; closed and open hemorrhoidectomy this procedure is associated with risk of complications and side effects when compared to non-invasive methods; severe pain, delay to return to normal activities may take weeks, bleeding that may occur in 1 to 2% of patients, urinary retention may also occur and reported to be as high as 34% after hemorrhoidectomy. It has a low risk of recurrence<ref name=":1" />. | |||
'''Stapled Hemorrhoidopexy''' in this procedure the internal hemorrhoids is fixed to the rectal wall after resection. It is associated with less pain as it is done above the dentate line and vice hemorrhoidectomy procedure, in female patients there is a risk of recto-vaginal fistula due to a blending of vaginal tissue into the purse-string<ref name=":1" />. | |||
'''Doppler-guided Hemorrhoidal Artery Ligation''' uses a guided doppler ultrasonic to identify and ligate the hemorrhoidal arteries<ref name=":1" />. | |||
== Differential Diagnosis == | == Differential Diagnosis == | ||
* | * Anal fissure, tear or opening of the moist thin tissues lining the anal canal that may cause bleeding and pain it is usually caused by stretching of the anal canal because of hard bowel movement, trauma to the lining tissues, | ||
* Fistula | * Fistula | ||
* Colorectal cancer is important to be excluded if there is bleeding. | * Colorectal cancer is important to be excluded if there is bleeding. | ||
| Line 88: | Line 108: | ||
[https://www.nice.org.uk/guidance/ipg525 Electrotherapy for the treatment of hemorrhoids NICE guidelines]. | [https://www.nice.org.uk/guidance/ipg525 Electrotherapy for the treatment of hemorrhoids NICE guidelines]. | ||
== References == | == References == | ||
<references /> | <references /> | ||
[[Category:Pelvic Health]] | |||
[[Category:Conditions]] | |||
[[Category:Pelvis - Conditions]] | |||
Latest revision as of 15:48, 24 July 2023
Original Editor - Khloud Shreif
Top Contributors - Khloud Shreif, Kim Jackson and Lucinda hampton
Clinically Relevant Anatomy[edit | edit source]
The anal canal is the end part of the gastrointestinal tract (GIT), it is about 4cm in length in women and a bit longer in men reaching about 4.4 cm in length, passing downwards and backward forming the anorectal angle. The internal lining mucosa membrane of the anal canal is divided by the pectinate line into two portions: the upper one the vertical anal columns (8-10 anal fold), at there ends there are valves (anal valves), above each one of these anal valves there is a shallow mucosal pocket called the anal sinus. the lower part below the line is formed of nonkeratinized squamous epithelium with no ducts it is sensitive to pain and provides an internal moisturizing to the canal[1].
The upper anal canal is lined by three main anal cushions they are very vascular, and their positions contribute to the anatomy of the anal canal to help with continence, the first one is located in the right anterior at 11 o'clock, the second at the right posterior at 7 o'clock and the last one on the left lateral aspect at 3 o'clock of the anal canal, they consist of connective tissues and connection of arteries and veins, supported by smooth muscles and connective tissues and supplied by the rectal artery. In addition to the three main cushions, there are many minor cushions between them.
The anal canal is described as an anatomical and surgical anal canal. The anatomical anal canal starts from the dentate line and ends at the anal verge, while the surgical anal canal extends from the anorectal ring (junction between the anal canal and rectum) to the anal verge[2].
Mechanism of Injury / Pathological Process[edit | edit source]
Haemorrhoids are defined as a swollen/ enlargement/ or displacement of vascular anal cushions, it may be symptomatic condition or asymptomatic in others that affects millions of people. The exact pathophysiology is still unclear but there are many theories.
Sliding theory
Sliding of lining anal cushions theory, which was described in 1975, suggested that haemorrhoids happen when there is break down and downward displacement of structures of internal anal cushions when the supporting structures of anal cushions become weak this will this will predispose to prolapse of anal cushions such as during defecation or an increase of intra-abdominal pressure, theses displacement changes are associated with the inflammatory process of the internal canal, venous dilatation, the process of degeneration of the fibro-elastic and collagen tissues, vascular thrombosis and/ or anal sub-epithelial muscle this theory still accepted[3].
Hemodynamic theory
Hemodynamic and hypervascularization theory, the anal cushions are supplied by terminal branches of the superior rectal artery, they are larger in diameter that are associated with an increase in the blood flow and venous backflow because of collapsed anastomosis of arteriovenous that lead to enlargement and prolapse of cushions[4].
The smooth muscles around the arteriovenous plexus act as a sphincter to reduce the arterial inflow of the blood and improve venous drainage and so decreasing the enlargement of arteriovenous plexus and the risk of hemorrhoids is another possible explanation for the pathophysiology of hemorrhoids[5].
In a large sample of heamorrhoidal tissues, there was an increase in microvascular density that support the phenomena of neovascularization especially when there is a thrombosis. Several enzymes and mediators play a role in the development of haemorrhoids such as; angiogenesis-related proteins such as VEGF, matrix metalloproteinase (MMP), and zinc-dependent proteinase that have a degradation and remodeling effect[3].
Types of Haemorrhoids[edit | edit source]
Haemorrhoids are classified according to the location to pectinate line into:
Internal haemorrhoids originates from dilatation of the venous plexus above the dentate line and are classified into four grades according to Goligher’s classification:
- Grade I, visible haemorrhoids with no prolapse.
- Grade II, prolapse of anal cushions through the anus at straining or increase of intra-abdominal pressure but they reduce spontaneously.
- Grade III, prolapse of anal cushions through the anus at straining or increase of intra-abdominal pressure but need manual reduction.
- Grade IV, is nonreducible prolapse.
External haemorrhoids originates from dilatation of the venous plexus below the dentate line
Risk / Predisposing Factors[edit | edit source]
- Activities that increase intra-abdominal pressure like weight lifting, and straining.
- Chronic constipation
- Pregnancy (constipation or decrease support of connective tissues due to elasticity during pregnancy)
- Prolonged toileting in a sitting position that leads to disruption of blood backflow
- Bad dietary habits
- Hard feces (an increase in consistency of stool that make it difficult to pass) or diarrhoea.
Clinical Presentation[edit | edit source]
In patients who suffer from haemorrhoids approximately 4 out of 10 will have symptoms. Clinical presentation of the patient depends on the degree and type of haemorrhoids, external haemorrhoids maybe come with acute pain if there is thrombosis, feeling of swelling/lump around the anus, bleeding that is usually painless, bright red bleeding[6] related to internal haemorrhoids and associated with bowel movement[7].
Diagnostic Procedures[edit | edit source]
- Detailed patient history and physical examination is important to diagnose haemorrhoids ad exclude any possible causes.
- With external examination to detect if there is any anal discharge, lumps out the anus, or thrombosis associated with external haemorrhoids that feel firm, purplish nodule and tender with palpation, fecal soiling, or anal fissure. Digital/ Internal examination we can not detect internal hemorrhoids but we can detect if there is an abnormal internal mass, scar, fistula, or anal stenosis[3][8].
- Anoscope procedure is important to be carried if there is bleeding or the digital exam revealed that there is an internal mass and to confirm internal haemorrhoids, it can detect the size, location, and severity of inflammation. In patients above 50 years old total colonoscopy can be done if there is bleeding for exclusion of causes[8].
Management / Interventions[edit | edit source]
Conservative management[edit | edit source]
Medical Treatment[edit | edit source]
- Topical analgesic or anti-inflammatory for acute haemorrhoids
- Phlebotonics that contains plant extracts, it improves lymphatic drainage, and capillary permeability used for 1st and 2nd degree of internal haemorrhoids and during thrombosis episodes.
- Corticosteroid and NSAID treatment or laxatives[9].
Physical Therapy[edit | edit source]
Exercise therapy and a diet rich in fiber are important to improve and decrease the straining and bearing down with bowel movement. Teaching the patient the proper effective way to breathe in to help relax the pelvic floor muscles during defecation.
Assessment of the anal sphincter is important, and tracking any spasm or incoordination between muscles is important to be treated using biofeedback, soft tissue massage of tight muscles, and pelvic floor muscle training.
Transcutaneous electrical nerve stimulation (TENS) and other therapeutic pain modalities can be used to relieve pain in patients with haemorrhoids, it is effective for pain relief post-surgical procedures[10].
Non-surgical intervention[edit | edit source]
Known as electrocoagulation in the outpatient setting using an anoscope a probe carrying a direct electric current with intensity between 8 mA and 16 mA will be directed to the base of the hemorrhoid, the time of the session depends on the grade, it is used as an alternative procedure for grade I or II and can be used for grade III or IV as an alternative to surgery.
- Sclerotherapy
It uses chemicals such as zinc chloride, quinine, and polidocanol to be injected into hemorrhoidal tissues this is used to decrease the vascularity, and redundant tissue and gradually hemorrhoid will shrink and obliterates over time, used in grade I and II internal hemorrhoids with no need to anesthesia during the procedure[12].
- Rubber band ligation
Using an anoscope the hemorrhoid will be tied at its base by a rubber band to cut the blood supply, within 3 to 7 days later. This prolapsed part of the hemorrhoid will fall off[13].
Surgical Intervention[edit | edit source]
Hemorrhoidectomy divided into two types; closed and open hemorrhoidectomy this procedure is associated with risk of complications and side effects when compared to non-invasive methods; severe pain, delay to return to normal activities may take weeks, bleeding that may occur in 1 to 2% of patients, urinary retention may also occur and reported to be as high as 34% after hemorrhoidectomy. It has a low risk of recurrence[8].
Stapled Hemorrhoidopexy in this procedure the internal hemorrhoids is fixed to the rectal wall after resection. It is associated with less pain as it is done above the dentate line and vice hemorrhoidectomy procedure, in female patients there is a risk of recto-vaginal fistula due to a blending of vaginal tissue into the purse-string[8].
Doppler-guided Hemorrhoidal Artery Ligation uses a guided doppler ultrasonic to identify and ligate the hemorrhoidal arteries[8].
Differential Diagnosis[edit | edit source]
- Anal fissure, tear or opening of the moist thin tissues lining the anal canal that may cause bleeding and pain it is usually caused by stretching of the anal canal because of hard bowel movement, trauma to the lining tissues,
- Fistula
- Colorectal cancer is important to be excluded if there is bleeding.
Resources[edit | edit source]
American Gastroenterological Association medical position statement: Diagnosis and treatment of hemorrhoids
Electrotherapy for the treatment of hemorrhoids NICE guidelines.
References[edit | edit source]
- ↑ Bazira PJ. Anatomy of the rectum and anal canal. Surgery (Oxford). 2022 Dec 7.
- ↑ Lee JM, Kim NK. Essential anatomy of the anorectum for colorectal surgeons focused on the gross anatomy and histologic findings. Annals of Coloproctology. 2018 Apr;34(2):59.
- ↑ 3.0 3.1 3.2 Lohsiriwat V. Hemorrhoids: from basic pathophysiology to clinical management. World journal of gastroenterology: WJG. 2012 May 5;18(17):2009.
- ↑ Lalisang TJ. Hemorrhoid: Pathophysiology and Surgical Management Literature Review. The New Ropanasuri Journal of Surgery. 2016;1(1).
- ↑ Aigner F, Gruber H, Conrad F, Eder J, Wedel T, Zelger B, Engelhardt V, Lametschwandtner A, Wienert V, Böhler U, Margreiter R. Revised morphology and hemodynamics of the anorectal vascular plexus: impact on the course of hemorrhoidal disease. International journal of colorectal disease. 2009 Jan;24:105-13.
- ↑ Aigner F, Gruber H, Conrad F, Eder J, Wedel T, Zelger B, Engelhardt V, Lametschwandtner A, Wienert V, Böhler U, Margreiter R. Revised morphology and hemodynamics of the anorectal vascular plexus: impact on the course of hemorrhoidal disease. International journal of colorectal disease. 2009 Jan;24:105-13.
- ↑ Margetis N. Pathophysiology of internal hemorrhoids. Annals of gastroenterology. 2019 Apr 27:264-.
- ↑ 8.0 8.1 8.2 8.3 8.4 Sun Z, Migaly J. Review of hemorrhoid disease: presentation and management. Clinics in colon and rectal surgery. 2016 Mar;29(01):022-9.
- ↑ Higuero T, Abramowitz L, Castinel A, Fathallah N, Hemery P, Duhoux CL, Pigot F, Pillant-Le Moult H, Senéjoux A, Siproudhis L, Staumont G. Guidelines for the treatment of hemorrhoids. Journal of visceral surgery. 2016 Jun 1;153(3):213-8.
- ↑ Chiu JH, Chen WS, Chen CH, Jiang JK, Tang GJ, Lui WY, Lin JK. Effect of transcutaneous electrical nerve stimulation for pain relief on patients undergoing hemorrhoidectomy: a prospective, randomized, controlled trial. Diseases of the colon & rectum. 1999 Feb;42(2):180-5.
- ↑ Michelle Kenway. 6 Hemorrhoid Fixes for PAIN & BLEEDING - Complete Physiotherapy Guide to HOME REMEDY Hemorrhoids. Available from: http://www.youtube.com/watch?v=qTcb55KOK9Y[last accessed 24/6/2023]
- ↑ He A, Chen M. Sclerotherapy in hemorrhoids. Indian Journal of Surgery. 2023 Apr;85(2):228-32.
- ↑ Albuquerque A. Rubber band ligation of hemorrhoids: A guide for complications. World journal of gastrointestinal surgery. 2016 Sep 9;8(9):614.