Upper Limb Management in C4 and C5 Spinal Cord Injury: Difference between revisions
No edit summary |
No edit summary |
||
| (45 intermediate revisions by 4 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox"> | |||
'''Original Editor '''- [[User: | <div class="editorbox">'''Original Editor '''- [[User:Ewa Jaraczewska|Ewa Jaraczewska]] based on the course by [https://members.physio-pedia.com/instructor/wendy-oelofse/ Wendy Oelofse] | ||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | ||
</div> | </div> | ||
== Introduction == | == Introduction == | ||
It has been found that restoring hand function is one of the most important goals for a person with [[tetraplegia]].<ref>Van Tuijl JH, Janssen-Potten YJ, Seelen HA. [https://www.nature.com/articles/3101261 Evaluation of upper extremity motor function tests in tetraplegics]. Spinal Cord. 2002 Feb;40(2):51-64.</ref> Upper extremity function in a person with a high-level spinal cord injury (SCI) can improve quality of life. It also has a direct psychological impact and helps individuals with SCI maintain social relationships.<ref>Deep V, Vijay V, Malik L. [http://s3-ap-southeast-1.amazonaws.com/ijmer/pdf/volume10/volume10-issue9(3)/5.pdf Relationship between capabilities of upper extremity and quality of life in chronic spinal cord injury]. International Journal of Multidisciplinary Educational Research, 2021;10: 9(3)</ref> | |||
Optimal [[Upper Limb Function in Spinal Cord Injury|upper limb]] functioning (UL) depends on neurological deficits. There may need to be a focus on preventing complications and creating ideal conditions for upper limb rehabilitation.<ref name=":0">Paralyzed Veterans of America Consortium for Spinal Cord Medicine. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1808273/pdf/i1079-0268-28-5-433.pdf Preservation of upper limb function following spinal cord injury: a clinical practice guideline for health-care professionals]. J Spinal Cord Med. 2005;28(5):434-70.</ref> Upper limb [[Pain Management in Spinal Cord Injury|pain]] is a common complication, occurring in 59 percent of individuals with tetraplegia,<ref name=":0" /> and it can delay progress. Therapy must always be tailored to the individual, and patient feedback is essential. This article will discuss various rehabilitative strategies for upper limb management in C4 and C5 spinal cord injuries performed by a multidisciplinary SCI team. <blockquote>"Tetraplegia: This term refers to impairment or loss of motor and/or sensory function in the cervical segments of the spinal cord due to damage of neural elements within the spinal canal. Tetraplegia results in impairment of function in the arms and typically in the trunk, legs, and pelvic organs (i.e., including the four extremities). It does not include brachial plexus lesions or injury to peripheral nerves outside the neural canal."<ref>Rupp R, Biering-Sørensen F, Burns SP, Graves DE, Guest J, Jones L, Read MS, Rodriguez GM, Schuld C, Tansey-Md KE, Walden K. [https://meridian.allenpress.com/tscir/article/27/2/1/465525/International-Standards-for-Neurological International standards for neurological classification of spinal cord injury: revised 2019]. Topics in spinal cord injury rehabilitation. 2021;27(2):1-22.</ref> </blockquote> | |||
== C4 Tetraplegia == | == C4 Tetraplegia == | ||
# No active movement of upper limb muscles | # No active movement of the upper limb muscles | ||
# Unable to use hand | # Unable to use hand | ||
# High risk of shoulder subluxation due to lack of innervation of shoulder girdle | # High risk of shoulder subluxation due to lack of innervation of the shoulder girdle | ||
| Line 19: | Line 20: | ||
* Prevent and control the development of deformities | * Prevent and control the development of deformities | ||
* Protect insensate areas from injury | * Protect insensate areas (i.e. areas lacking sensation) from injury | ||
* Prevent or reduce oedema | * Prevent or reduce [[Oedema Assessment|oedema]] | ||
* Maintain a supple hand for human contact | * Maintain a supple hand for human contact | ||
* Protect the limb from irreversible changes | * Protect the limb from irreversible changes | ||
| Line 27: | Line 28: | ||
=== Prevention === | === Prevention === | ||
==== Prevention of Development and Management of | ==== Prevention of Development and Management of Upper Limb Deformities ==== | ||
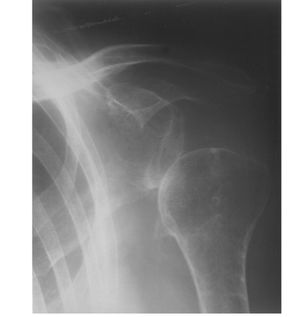
'''Shoulder | [[File:Glenohumeral Subluxation .jpg|thumb|Glenohumeral Subluxation]] | ||
'''[[Shoulder Subluxation]]:''' | |||
* Avoid extreme positions at the shoulder which can lead to shoulder injury. | * Avoid extreme positions at the shoulder, which can lead to a shoulder injury. For example, extreme internal rotation, forward flexion, and abduction can cause [[Impingement / Instability Differentiation|shoulder impingement]].<ref name=":0" /> | ||
* Maintain proper alignment of the glenohumeral joint while sitting in | * Maintain proper alignment of the [[Glenohumeral Joint|glenohumeral joint]] while sitting in a wheelchair during functional and weight-bearing activities. | ||
* Educate all caregivers on proper UL handling during transfers and all other daily activities. | * Educate all caregivers on proper UL handling during transfers and all other daily activities. | ||
| Line 37: | Line 39: | ||
'''Hand and wrist overstretched in extension or flexion:''' | '''Hand and wrist overstretched in extension or flexion:''' | ||
* Avoid extreme positions of the wrist, especially full wrist extension. Weight bearing through an extended wrist and flat hand | * Avoid extreme positions of the wrist, especially full wrist extension. Weight-bearing through an extended wrist and flat hand can cause nerve injury as it compresses the median nerve in the carpal tunnel/canal.<ref name=":0" /> | ||
* Use closed-fist hand position and neutral wrist while transferring between surfaces, but watch for wrist instability during these tasks. | * Use a closed-fist hand position and neutral wrist while transferring between surfaces, but watch for wrist instability during these tasks. | ||
* Avoid extended periods of volar flexion | * Avoid extended periods of volar (palmar) flexion. | ||
==== Prevention or Reduction of Oedema ==== | ==== Prevention or Reduction of Oedema ==== | ||
Limited | Limited muscle pump activity due to muscle paralysis after a spinal cord injury causes a reduction in venous and lymphatic return, leading to oedema. Chronic oedema can restrict the upper limb range of motion and decrease the patient's ability to use their hand for functional tasks when able. | ||
[[File:Wheelchair with Tray - Shutterstock Image - ID 1790659226.jpg|thumb|Wheelchair with Tray]] | |||
===== Interventions<ref>Dunn J, Wangdell J. Improving upper limb function. Rehabilitation in Spinal Cord Injuries. 2020 Feb 1:372.</ref> ===== | |||
There is no consensus on how to best manage UL oedema: | |||
* Elevate and position properly: UL elevation on a pillow when a patient lies supine in bed, UL support in glenohumeral joint alignment to prevent shoulder subluxation and associated pain. This can be achieved by applying the wheelchair tray or gutter armrests. | |||
* Avoid excessive wrist flexion, which can obstruct venous and lymphatic return. | |||
* Use splinting to facilitate conditions for adequate venous return. | |||
* Maintain range of motion in the joints, tendons and ligaments of the wrist and fingers. | |||
* Apply prolonged stretches using an orthosis in hand spasticity to prevent contractures. | |||
* Use compression gloves ([[Tenodesis Function in Spinal Cord Injury|tenodesis]] position should be maintained and compression applied on the palmar side of the hand) or wrap each finger individually with Coban or Danamull Haft. | |||
= | {{#ev:youtube|v=kXZsRYVreg4|300}}<ref>Compression Techniques for Edema: Coban Wrapping. Dr Borst's Occupational Therapy Classroom. Available from: https://www.youtube.com/watch?v=kXZsRYVreg4 [last accessed 22/11/2022]</ref> | ||
==== Protection of Insensate Areas ==== | ==== Protection of Insensate Areas ==== | ||
Pressure ulcers can occur due to multiple factors that include : | [[Pressure Ulcers|Pressure ulcers]] can occur due to multiple factors that include: | ||
* | * Sustained local pressure (elbows supported on the arm troughs or wheelchair tray) | ||
* | * Short periods of high pressure | ||
* | * Shearing forces | ||
* | * Friction | ||
* | * Moisture (hand contracture) | ||
Common | Common locations of UL pressure ulcers are: | ||
* | * Over a bony prominence | ||
* | * Medial surface of the [[elbow]] | ||
* | * [[Scapula]] | ||
===== Interventions: ===== | ===== Interventions: ===== | ||
* Proper positioning in bed and | * [[Wheelchair Fitting|Proper positioning]] in bed and wheelchair | ||
* UL protection from friction and shearing forces during wheelchair pressure relief | * UL protection from friction and shearing forces during wheelchair pressure relief when reclining or tilting in space | ||
* Proper hand hygiene | * Proper hand hygiene | ||
* | * Perform skin inspection twice a day<ref>Braden BJ, Blanchard S. [http://whywoundcare.s3.amazonaws.com/Files/Chapter+17.pdf Risk assessment in pressure ulcer prevention.] Krasner, DL, Rodeheaver, GT, Sibbeald, RG (Eds.) Chronic Wound Care: A Clinical Source Book for Healthcare Professionals (. 2001:641-51.</ref> | ||
==== Limb Protection ==== | ==== Limb Protection ==== | ||
Maintaining adequate range of motion in all UL joints: | Maintaining an adequate range of motion in all UL joints: | ||
* Positioning in bed and | * Positioning in bed and wheelchair | ||
* Shoulder pain prevention or shoulder pain management | * Shoulder pain prevention or shoulder pain management due to impingement syndrome, capsulitis, [[osteoarthritis]], recurrent dislocations, [[Rotator Cuff Tears|rotator cuff tear]], bicipital tendonitis, and [[Myofascial Pain|myofascial pain syndrome]]<ref name=":0" /> | ||
* Early and aggressive acute pain management | * Early and aggressive acute pain management for pain caused by acute musculoskeletal injuries to prevent the development of chronic pain<ref name=":0" /> | ||
=== Support for Function === | === Support for Function === | ||
Preserve range of motion and mobility for future treatment paradigms | Preserve range of motion and mobility for future treatment paradigms. | ||
== C5 Tetraplegia == | == C5 Tetraplegia == | ||
# Upper limb muscle innervation: deltoid, biceps, | # Upper limb muscle innervation: [[deltoid]], [[Biceps Brachii|biceps]], [[brachialis]], [[brachioradialis]] | ||
# Lack of elbow extension | # Lack of elbow extension | ||
# No wrist extension and no active movement of fingers or thumb | # No wrist extension and no active movement of the fingers or thumb | ||
# Supinated forearm | # Supinated forearm | ||
# Wrist extension achieved through orthosis | # Wrist extension achieved through orthosis | ||
| Line 102: | Line 107: | ||
* Prepare the limb for function (feeding) | * Prepare the limb for function (feeding) | ||
=== Prevention and Control the Development of Deformities === | === Prevention and Control of the Development of Deformities === | ||
With a C5 SCI, innervation of the shoulder and elbow flexors is preserved. Active elbow extension against gravity is impaired. The upper limb tends to be positioned in shoulder abduction, elbow flexion, forearm supination, and wrist extension. To avoid the range of motion limitations and the development of upper limb deformities, the following strategies should be implemented: | |||
* Individuals with an SCI and their caregivers should be ''educated'' to monitor range of motion (ROM) limitations and their impact on function.<ref>Frye SK, Geigle PR, York HS, Sweatman WM. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7054980/pdf/YSCM_43_1622239.pdf Functional passive range of motion of individuals with chronic cervical spinal cord injury.] J Spinal Cord Med. 2020 Mar;43(2):257-263.</ref> | |||
* ''Positional strategies and activity modifications'' should be emphasised during therapy sessions, as stretching may not improve ROM limitations.<ref>Harvey LA, Katalinic OM, Herbert RD, Moseley AM, Lannin NA, Schurr K. [https://reader.elsevier.com/reader/sd/pii/S1836955317300280?token=1AA0E5139FD4E9303F32C6DE2E445EAB672E458031FA211178381C3DFB5AD87094F17EAC0405CA8A82C6BDE49A5B0170&originRegion=eu-west-1&originCreation=20221119204056 Stretch for the treatment and prevention of contracture: an abridged republication of a Cochrane Systematic Review.] J Physiother. 2017 Apr;63(2):67-75. </ref> | |||
=== Limb Protection === | === Limb Protection === | ||
=== Preparation for | * Preservation of the shoulder's full active range of motion.<ref>Mateo S, Roby-Brami A, Reilly KT, Rossetti Y, Collet C, Rode G. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4417243/pdf/12984_2014_Article_715.pdf Upper limb kinematics after cervical spinal cord injury: a review.] J Neuroeng Rehabil. 2015 Jan 30;12:9.</ref> | ||
Adaptive Equipment trials: universal cuff, Mobile Arm Support (MAS) | ** Limitations in shoulder ROM may occur due to poor scapula stability | ||
** Poor scapula stability is characterised by a reduction in scapula lateral rotation and [[Scapulothoracic Joint|scapulothoracic]] instability | |||
** [[Serratus Anterior|Serratus anterior]] (innervation C5-C7) is not able to counteract the [[rhomboids]] (innervation C4-C5), which leads to scapula instability | |||
* Neck and shoulder pain prevention and management<ref>Waring WP, Maynard FM. [https://www.nature.com/articles/sc19915.pdf?origin=ppub Shoulder pain in acute traumatic quadriplegia.] Paraplegia. 1991 Jan;29(1):37-42. </ref> | |||
** Overused [[trapezius]] provides scapula elevation and retraction with no opposition from the shoulder protractors (serratus anterior, pectoralis major and minor) and depressors ([[Latissimus Dorsi Muscle|latissimus dorsi]], [[Pectoralis Minor|pectoralis minor]]). The trapezius becomes short and tight. | |||
Prevention strategies may include: | |||
* [[Passive Range of Motion: Shoulder flexion|Passive range of motion]] | |||
* Positional strategies | |||
* [[Taping]] <ref>Taylor RL, O'Brien L, Brown T. A scoping review of the use of elastic therapeutic tape for neck or upper extremity conditions. Journal of Hand Therapy. 2014 Jul 1;27(3):235-46.</ref> | |||
{{#ev:youtube|v=3USDcUbKuKE|300}}<ref>Length, Strength and Kinesio Tape: The Upper Trapezius. Available from: https://www.youtube.com/watch?v=3USDcUbKuKE [last accessed 22/11/2022]</ref> | |||
=== Preparation for Function === | |||
Adaptive Equipment trials: universal cuff, Mobile Arm Support (MAS). See [[Upper Limb Management in C4 and C5 SCI#Upper Limb Adaptive Equipment.2FAssistive Technologies|Upper Limb Adaptive Equipment]] section below. | |||
== Upper Limb Splinting == | == Upper Limb [[Splinting]] == | ||
Goals: | Goals: | ||
* To reduce pain | * To reduce pain | ||
* To slow | * To slow degradation | ||
* To recover joint space | * To recover joint space | ||
* To improve finger performance and hand functioning by increasing grip and pinch strength | * To improve finger performance and hand functioning by increasing grip and pinch strength<ref>Kaunnil A, Sansri V, Thongchoomsin S, Permpoonputtana K, Stanley M, Trevittaya P, Thawisuk C, Thichanpiang P. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9332612/pdf/ijerph-19-08995.pdf Bridging the Gap between Clinical Service and Academic Education of Hand-Splinting Practice: Perspectives and Experiences of Thai Occupational Therapists.] Int J Environ Res Public Health. 2022 Jul 24;19(15):8995.</ref> | ||
===== General Guidelines <ref name=":2" /> ===== | ===== General Guidelines<ref name=":2" /> ===== | ||
* | * The patient must participate in the decision-making process and treatment plan | ||
* | * The patient must demonstrate health literacy and an understanding of their condition | ||
* | * The splint must serve functional goals | ||
* Splint choice depends on cosmetic preferences of the patient | * Splint choice depends on the cosmetic preferences of the patient | ||
* | * The patient must tolerate the splint and find it comfortable to wear | ||
* | * The patient and caregiver must accept the splint and follow through with the wearing schedule and maintenance | ||
* | * The clinician must perform an ongoing review of current evidence for splinting in spinal cord injury | ||
===== Protocols ===== | ===== Protocols ===== | ||
Limited standard protocols exist across the continuum of care. | Limited standard protocols exist across the continuum of care. | ||
Protocol examples from the literature:<ref name=":2" /> | |||
# Goal: Optimal muscle shortening for tenodesis. | # Goal: Optimal muscle shortening for tenodesis. | ||
#* Splints issued immediately after injury and worn for 23 hours daily until the onset of rehabilitation with breaks only for range of motion exercises | #* Splints are issued immediately after injury and worn for 23 hours daily until the onset of rehabilitation, with breaks only for a range of motion exercises. | ||
# Goal: Optimal wrist and | # Goal: Optimal wrist and finger positioning. | ||
#* Resting hand splints for night time/rest when wrist and digit strength is 0–3/5 | #* Resting hand splints for night time/rest when wrist and digit strength is 0–3/5. | ||
#* Futuro wrist splints for daytime hand use for individuals with elbow flexion against gravity but weak wrists and hands | #* Futuro wrist splints for daytime hand use for individuals with elbow flexion against gravity but weak wrists and hands. | ||
#* Hand based or thumb splints and/or taping of the digits at night/rest for individuals with wrist extension against gravity but no digit movement. | #* Hand-based or thumb splints and/or taping of the digits at night/rest for individuals with wrist extension against gravity but no digit movement. | ||
===== Splints ===== | ===== Splints ===== | ||
'''Resting hand splint''':<ref name=":2">Frye SK, Geigle PR. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7298624/ Current U.S. splinting practices for individuals with cervical spinal cord injury.] Spinal Cord Ser Cases. 2020 Jun 17;6(1):49.</ref> | '''Resting hand splint''':<ref name=":2">Frye SK, Geigle PR. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7298624/ Current U.S. splinting practices for individuals with cervical spinal cord injury.] Spinal Cord Ser Cases. 2020 Jun 17;6(1):49.</ref> | ||
* | * Frequently used in C4 and C5 SCI | ||
* | * Custom-made is preferred over prefabricated | ||
* Clinical Practice Guidelines: mostly | * Maintains the hand in a functional position | ||
* typical position the | * Prevents deformity | ||
* '''Clinical Practice Guidelines''': mostly nighttime use when wrist and digit strength is 0-3/5 | |||
* The typical hand position in the resting hand splint is as follows: | |||
** Wrist in 10–40° extension (30° most frequent), | |||
** Metacarpophalangeal joint (MCP) at 0–90 (70–90 most typical) | |||
** Proximal interphalangeal (PIP) at 0–75 (10–30 most typical) | |||
** Distal interphalangeal (DIP) at 0–70 (10–20 most typical) | |||
** Thumb is positioned in opposition. | |||
'''Wrist splint''': | '''Wrist splint (Futuro splint)''': | ||
* Prefabricated wrist splints are preferred | * Prefabricated wrist splints are preferred | ||
* Clinical Practice Guidelines: for daytime use for individuals with elbow flexion 3-5/5, and wrist and hand 0-3/5 | * Worn during the day to increase functional activity participation | ||
* | * Dorsal varieties and a universal cuff (U-Cuff) are favourite options | ||
* The primary wrist splint goal is to prevent overstretching of the wrist extensors, and adding a universal cuff provides a stable base for activities of daily living (ADLs) | |||
* '''Clinical Practice Guidelines''': for daytime use for individuals with elbow flexion 3-5/5, and wrist and hand 0-3/5 | |||
* Most commonly used in a C5 SCI (73% of patients) and C4 (40% of patients) | |||
'''Long opponens''' | '''Long opponens''' | ||
* | * Used less frequently than other splints: 13% of patients with a C5 SCI and 6% of patients with a C4 SCI | ||
* Custom-fabricated splints preferred | |||
* Provides a stable post against which the index finger can pinch; positions thumb in a functional key pinch position | |||
* Potential interference with power wheelchair operation | |||
''' | '''Other''' | ||
* In addition, therapists commonly use the following devices:<ref name=":2" /> | |||
** Elbow extension splints, elbow pillow splints, or anti-spasticity splints to facilitate upper limb weight-bearing activities and assist with spasticity management | |||
** Palm splints for proper hand and wrist positioning | |||
** Tone and positioning splints to reduce upper limb spasticity | |||
** Tenodesis splints or orthotics to guide grasp and release movements | |||
** Finger flexion gloves or mitts to promote finger closure | |||
* In addition | |||
== Wheelchair Mobility == | == Wheelchair Mobility == | ||
[[File:Wheelchair Joystick Adaptations- Shutterstock - 2186607147.jpg|thumb|Wheelchair Joystick Adaptation]] | |||
Power wheelchair can be recommended for: | === Powered Wheelchair === | ||
* Powered wheelchairs help to protect the upper limb by reducing repetitive forceful activity. | |||
* They should be considered before a patient complains of upper limb pain. | |||
'''''But......''''' | |||
* Using powered mobility may lead to weight gain and upper limb deconditioning in a person with tetraplegia. | |||
A [[Power Wheelchair Maintenance|power wheelchair]] can be recommended for: | |||
* | * High-risk patients: | ||
** A person with a prior injury to the upper limb | |||
** person with a prior injury to the upper limb | ** Elderly | ||
** | ** A person living in a challenging environment (hills, uneven or rough terrain) | ||
** person living in a challenging environment (hills, uneven or rough terrain) | |||
=== Manual Wheelchair === | |||
* The optimal manual wheelchair should be high-strength, fully customisable and made of the lightest possible material. | |||
* The rear axle should be adjusted as far forward as possible without compromising the user's stability. | |||
* A more forward axle position decreases rolling resistance and increases propulsion efficiency.<ref name=":0" /> | |||
* Appropriate seated posture and stabilisation relative to balance and stability needs should be assessed. | |||
* Individuals with a C4 and higher SCI must be provided full support for the forearm and hand to decrease subluxation or dislocation.<ref name=":0" /> | |||
=== Wheelchair Modifications/Adaptive Equipment === | === Wheelchair Modifications/Adaptive Equipment === | ||
* Wrist extension splint with wheelchair glove over it | * Wrist extension splint with wheelchair glove over it | ||
* Arm trough support | |||
* Elbow blocks (to assist with arm support during tilt) | |||
* Modular hand pad | |||
* Various joystick options | |||
** Ball, enlarged ball | |||
** T-bar | |||
** U shaped | |||
** Cylinder | |||
** Carrot toggle | |||
* The slip-resistant grip on the wheelchair hand rims (plastic coated or rubber) | |||
* Rubber-coated projections off the push rim however, they impact the chair width | |||
* Extended brake levers | |||
== Upper Limb Adaptive Equipment/Assistive Technologies == | == Upper Limb Adaptive Equipment/Assistive Technologies == | ||
Universal cuff (C5) | Universal cuff (C5) | ||
* An adaptive device that helps patients with a high-level spinal cord injury grip small objects and perform activities of daily living | |||
* They are considered one of the most useful tools for people with limited control of their hands | |||
* The universal cuff is used to augment or provide upper extremity/hand function to perform activities | |||
* The items remain secure even when the patient cannot grip objects with their fingers - they can still eat a meal, draw, or groom themselves | |||
== Multidisciplinary | MAS (Mobile Arm Support)<ref name=":3">Readioff R, Siddiqui ZK, Stewart C, Fulbrook L, O'Connor RJ, Chadwick EK. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9662059/pdf/YSCM_45_1878342.pdf Use and evaluation of assistive technologies for upper limb function in tetraplegia. J Spinal Cord Med]. 2022 Nov;45(6):809-820. </ref> or BFO (Balanced Forearm Orthosis) | ||
* Patients using MAS have minimal strength in their deltoid and biceps muscles. | |||
** Motivated patients with biceps and deltoid muscle strength < 2/5 can benefit from MAS. | |||
* Patients are usually able to perform at least one ''new'' activity using a MAS, including eating, page-turning, driving a power wheelchair, brushing teeth, keyboarding, writing, name signing, drawing, painting, scratching nose, playing board games, accessing electronic devices, drinking, and grooming. | |||
* MAS attached to the wheelchair increases wheelchair width. In a reclining position, MAS can cause individuals to have problems managing their arms.<ref>Atkins MS, Baumgarten JM, Yasuda YL, Adkins R, Waters RL, Leung P, Requejo P. Mobile arm supports evidence-based benefits and criteria for use. The journal of spinal cord medicine. 2008 Jan 1;31(4):388-93.</ref> | |||
* According to Readioff et al.,<ref name=":3" /> MAS facilitates ADL tasks such as eating. | |||
{{#ev:youtube|v=z3ZENtlD93Q|300}}<ref>Mobile arm support. Available from: https://www.youtube.com/watch?v=z3ZENtlD93Q[last accessed 22/11/2022]</ref> | |||
== Multidisciplinary and Interdisciplinary SCI Teams == | |||
All multidisciplinary/interdisciplinary team members are responsible for the upper limb management of individuals with C4 and C5 tetraplegia. Management continues 24 hours/7 days a week. This team includes nursing staff, physicians, physiotherapists, occupational therapists, speech-language pathologists/therapists, family and all other caregivers. | |||
'''Education''' | '''Education''' | ||
* | * Education is tailored to the patient's needs with the expectation that this individualisation will improve the intervention results.<ref>Ricci L, Villegente J, Loyal D, Ayav C, Kivits J, Rat AC. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8849242/pdf/HEX-25-276.pdf Tailored patient therapeutic, educational interventions: A patient-centred communication mode]l. Health Expect. 2022 Feb;25(1):276-289. </ref> | ||
* | * It is important to educate healthcare providers, family, caregivers and persons with SCI about upper limb pain and injury risk. | ||
* | * Educate on the reduction of the frequency of repetitive upper limb tasks to decrease the risk of developing shoulder pain and shoulder dysfunction:<ref name=":0" /> | ||
** | ** Decreasing the number of transfers needed each day | ||
** | ** Altering between a manual wheelchair and a power wheelchair or switching to a power wheelchair as appropriate | ||
** | ** Frequency of propulsive stroke reduction during wheelchair propulsion | ||
** Consider alternative techniques for activities when upper limb pain or injury is present | ** Consider alternative techniques for activities when upper limb pain or injury is present | ||
'''Mandatory periodic reassessment of the patient's function, ergonomics, and equipment | '''Mandatory periodic reassessment of the patient's function, ergonomics, and equipment. Assess for''': | ||
* Changes in patient's medical status | * Changes in patient's medical status | ||
* Acquisition of new medical problems (heart disease) | * Acquisition of new medical problems (e.g. heart disease) | ||
* Changes in weight, muscle mass, pain level | * Changes in patient's weight, muscle mass, pain level | ||
* | * Effect of ageing on patient's functional status and mobility | ||
== ICF and Upper Limb Management == | |||
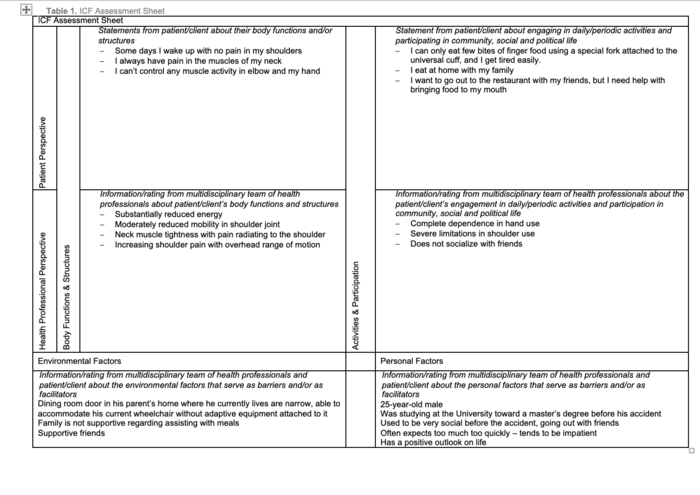
The [[Introduction to the International Classification of Functioning, Disability and Health (ICF)|International Classification of Functioning, Disability and Health (ICF) model]] should be utilised when managing the upper limbs of patients with a spinal cord injury. The ICF helps practitioners to interpret functional outcomes following therapeutic interventions and the provision of adaptive equipment.<ref>Cieza A, Kirchberger I, Biering-Sørensen F, Baumberger M, Charlifue S, Post MW, Campbell R, Kovindha A, Ring H, Sinnott A, Kostanjsek N, Stucki G. [https://www.nature.com/articles/sc2009183 ICF Core Sets for individuals with spinal cord injury in the long-term context]. Spinal Cord. 2010 Apr;48(4):305-12. </ref> The following image shows an example ICF assessment sheet for an individual with upper tetraplegia: | |||
[[File:ICF Assessment Tool for Upper Limb in SCI.png|center|thumb|700x700px|ICF Assessment Tool for Upper Limb Management in Tetraplegia|alt=]] | |||
Potential treatment interventions based on the results of the assessment using the ICF assessment tool: | |||
# Family and caregiver education on the importance of working towards achieving independence in eating | |||
# Family and caregiver education on choosing an appropriate diet to facilitate the patient's participation during meal times | |||
# Home visit to assess patient's home access for a wheelchair with MAS attachment | |||
# An exercise programme that focuses on neck muscle stretching and strengthening | |||
# Wheelchair seating and positioning assessment to ensure proper neck and head alignment | |||
== Resources == | == Resources == | ||
*[https:// | *Paralyzed Veterans of America Consortium for Spinal Cord Medicine. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1808273/pdf/i1079-0268-28-5-433.pdf Preservation of upper limb function following spinal cord injury: a clinical practice guideline for health-care professionals]. J Spinal Cord Med. 2005;28(5):434-70. | ||
*[http://whywoundcare.s3.amazonaws.com/Files/Chapter+17.pdf Risk Assessment in Pressure Ulcer Prevention] | *[http://whywoundcare.s3.amazonaws.com/Files/Chapter+17.pdf Risk Assessment in Pressure Ulcer Prevention] | ||
== References == | == References == | ||
<references /> | <references /> | ||
[[Category:Course Pages]] | |||
[[Category:Spinal Cord Injuries]] | |||
[[Category:Rehabilitation]] | |||
[[Category:ReLAB-HS Course Page]] | |||
Latest revision as of 21:08, 3 March 2023
Top Contributors - Ewa Jaraczewska, Jess Bell, Kim Jackson and Rishika Babburu
Introduction[edit | edit source]
It has been found that restoring hand function is one of the most important goals for a person with tetraplegia.[1] Upper extremity function in a person with a high-level spinal cord injury (SCI) can improve quality of life. It also has a direct psychological impact and helps individuals with SCI maintain social relationships.[2]
Optimal upper limb functioning (UL) depends on neurological deficits. There may need to be a focus on preventing complications and creating ideal conditions for upper limb rehabilitation.[3] Upper limb pain is a common complication, occurring in 59 percent of individuals with tetraplegia,[3] and it can delay progress. Therapy must always be tailored to the individual, and patient feedback is essential. This article will discuss various rehabilitative strategies for upper limb management in C4 and C5 spinal cord injuries performed by a multidisciplinary SCI team.
"Tetraplegia: This term refers to impairment or loss of motor and/or sensory function in the cervical segments of the spinal cord due to damage of neural elements within the spinal canal. Tetraplegia results in impairment of function in the arms and typically in the trunk, legs, and pelvic organs (i.e., including the four extremities). It does not include brachial plexus lesions or injury to peripheral nerves outside the neural canal."[4]
C4 Tetraplegia[edit | edit source]
- No active movement of the upper limb muscles
- Unable to use hand
- High risk of shoulder subluxation due to lack of innervation of the shoulder girdle
Goals for UL management:[5]
- Prevent and control the development of deformities
- Protect insensate areas (i.e. areas lacking sensation) from injury
- Prevent or reduce oedema
- Maintain a supple hand for human contact
- Protect the limb from irreversible changes
- Preserve the limb for future treatment paradigms
Prevention[edit | edit source]
Prevention of Development and Management of Upper Limb Deformities[edit | edit source]
- Avoid extreme positions at the shoulder, which can lead to a shoulder injury. For example, extreme internal rotation, forward flexion, and abduction can cause shoulder impingement.[3]
- Maintain proper alignment of the glenohumeral joint while sitting in a wheelchair during functional and weight-bearing activities.
- Educate all caregivers on proper UL handling during transfers and all other daily activities.
Hand and wrist overstretched in extension or flexion:
- Avoid extreme positions of the wrist, especially full wrist extension. Weight-bearing through an extended wrist and flat hand can cause nerve injury as it compresses the median nerve in the carpal tunnel/canal.[3]
- Use a closed-fist hand position and neutral wrist while transferring between surfaces, but watch for wrist instability during these tasks.
- Avoid extended periods of volar (palmar) flexion.
Prevention or Reduction of Oedema[edit | edit source]
Limited muscle pump activity due to muscle paralysis after a spinal cord injury causes a reduction in venous and lymphatic return, leading to oedema. Chronic oedema can restrict the upper limb range of motion and decrease the patient's ability to use their hand for functional tasks when able.
Interventions[6][edit | edit source]
There is no consensus on how to best manage UL oedema:
- Elevate and position properly: UL elevation on a pillow when a patient lies supine in bed, UL support in glenohumeral joint alignment to prevent shoulder subluxation and associated pain. This can be achieved by applying the wheelchair tray or gutter armrests.
- Avoid excessive wrist flexion, which can obstruct venous and lymphatic return.
- Use splinting to facilitate conditions for adequate venous return.
- Maintain range of motion in the joints, tendons and ligaments of the wrist and fingers.
- Apply prolonged stretches using an orthosis in hand spasticity to prevent contractures.
- Use compression gloves (tenodesis position should be maintained and compression applied on the palmar side of the hand) or wrap each finger individually with Coban or Danamull Haft.
Protection of Insensate Areas[edit | edit source]
Pressure ulcers can occur due to multiple factors that include:
- Sustained local pressure (elbows supported on the arm troughs or wheelchair tray)
- Short periods of high pressure
- Shearing forces
- Friction
- Moisture (hand contracture)
Common locations of UL pressure ulcers are:
Interventions:[edit | edit source]
- Proper positioning in bed and wheelchair
- UL protection from friction and shearing forces during wheelchair pressure relief when reclining or tilting in space
- Proper hand hygiene
- Perform skin inspection twice a day[8]
Limb Protection[edit | edit source]
Maintaining an adequate range of motion in all UL joints:
- Positioning in bed and wheelchair
- Shoulder pain prevention or shoulder pain management due to impingement syndrome, capsulitis, osteoarthritis, recurrent dislocations, rotator cuff tear, bicipital tendonitis, and myofascial pain syndrome[3]
- Early and aggressive acute pain management for pain caused by acute musculoskeletal injuries to prevent the development of chronic pain[3]
Support for Function[edit | edit source]
Preserve range of motion and mobility for future treatment paradigms.
C5 Tetraplegia[edit | edit source]
- Upper limb muscle innervation: deltoid, biceps, brachialis, brachioradialis
- Lack of elbow extension
- No wrist extension and no active movement of the fingers or thumb
- Supinated forearm
- Wrist extension achieved through orthosis
- No tenodesis grip
Goals:[5]
- Prevent and control the development of deformities
- Protect insensate areas from injury
- Prevent or reduce oedema
- Prepare the limb for function (feeding)
Prevention and Control of the Development of Deformities[edit | edit source]
With a C5 SCI, innervation of the shoulder and elbow flexors is preserved. Active elbow extension against gravity is impaired. The upper limb tends to be positioned in shoulder abduction, elbow flexion, forearm supination, and wrist extension. To avoid the range of motion limitations and the development of upper limb deformities, the following strategies should be implemented:
- Individuals with an SCI and their caregivers should be educated to monitor range of motion (ROM) limitations and their impact on function.[9]
- Positional strategies and activity modifications should be emphasised during therapy sessions, as stretching may not improve ROM limitations.[10]
Limb Protection[edit | edit source]
- Preservation of the shoulder's full active range of motion.[11]
- Limitations in shoulder ROM may occur due to poor scapula stability
- Poor scapula stability is characterised by a reduction in scapula lateral rotation and scapulothoracic instability
- Serratus anterior (innervation C5-C7) is not able to counteract the rhomboids (innervation C4-C5), which leads to scapula instability
- Neck and shoulder pain prevention and management[12]
- Overused trapezius provides scapula elevation and retraction with no opposition from the shoulder protractors (serratus anterior, pectoralis major and minor) and depressors (latissimus dorsi, pectoralis minor). The trapezius becomes short and tight.
Prevention strategies may include:
- Passive range of motion
- Positional strategies
- Taping [13]
Preparation for Function[edit | edit source]
Adaptive Equipment trials: universal cuff, Mobile Arm Support (MAS). See Upper Limb Adaptive Equipment section below.
Upper Limb Splinting[edit | edit source]
Goals:
- To reduce pain
- To slow degradation
- To recover joint space
- To improve finger performance and hand functioning by increasing grip and pinch strength[15]
General Guidelines[16][edit | edit source]
- The patient must participate in the decision-making process and treatment plan
- The patient must demonstrate health literacy and an understanding of their condition
- The splint must serve functional goals
- Splint choice depends on the cosmetic preferences of the patient
- The patient must tolerate the splint and find it comfortable to wear
- The patient and caregiver must accept the splint and follow through with the wearing schedule and maintenance
- The clinician must perform an ongoing review of current evidence for splinting in spinal cord injury
Protocols[edit | edit source]
Limited standard protocols exist across the continuum of care.
Protocol examples from the literature:[16]
- Goal: Optimal muscle shortening for tenodesis.
- Splints are issued immediately after injury and worn for 23 hours daily until the onset of rehabilitation, with breaks only for a range of motion exercises.
- Goal: Optimal wrist and finger positioning.
- Resting hand splints for night time/rest when wrist and digit strength is 0–3/5.
- Futuro wrist splints for daytime hand use for individuals with elbow flexion against gravity but weak wrists and hands.
- Hand-based or thumb splints and/or taping of the digits at night/rest for individuals with wrist extension against gravity but no digit movement.
Splints[edit | edit source]
Resting hand splint:[16]
- Frequently used in C4 and C5 SCI
- Custom-made is preferred over prefabricated
- Maintains the hand in a functional position
- Prevents deformity
- Clinical Practice Guidelines: mostly nighttime use when wrist and digit strength is 0-3/5
- The typical hand position in the resting hand splint is as follows:
- Wrist in 10–40° extension (30° most frequent),
- Metacarpophalangeal joint (MCP) at 0–90 (70–90 most typical)
- Proximal interphalangeal (PIP) at 0–75 (10–30 most typical)
- Distal interphalangeal (DIP) at 0–70 (10–20 most typical)
- Thumb is positioned in opposition.
Wrist splint (Futuro splint):
- Prefabricated wrist splints are preferred
- Worn during the day to increase functional activity participation
- Dorsal varieties and a universal cuff (U-Cuff) are favourite options
- The primary wrist splint goal is to prevent overstretching of the wrist extensors, and adding a universal cuff provides a stable base for activities of daily living (ADLs)
- Clinical Practice Guidelines: for daytime use for individuals with elbow flexion 3-5/5, and wrist and hand 0-3/5
- Most commonly used in a C5 SCI (73% of patients) and C4 (40% of patients)
Long opponens
- Used less frequently than other splints: 13% of patients with a C5 SCI and 6% of patients with a C4 SCI
- Custom-fabricated splints preferred
- Provides a stable post against which the index finger can pinch; positions thumb in a functional key pinch position
- Potential interference with power wheelchair operation
Other
- In addition, therapists commonly use the following devices:[16]
- Elbow extension splints, elbow pillow splints, or anti-spasticity splints to facilitate upper limb weight-bearing activities and assist with spasticity management
- Palm splints for proper hand and wrist positioning
- Tone and positioning splints to reduce upper limb spasticity
- Tenodesis splints or orthotics to guide grasp and release movements
- Finger flexion gloves or mitts to promote finger closure
Wheelchair Mobility[edit | edit source]
Powered Wheelchair[edit | edit source]
- Powered wheelchairs help to protect the upper limb by reducing repetitive forceful activity.
- They should be considered before a patient complains of upper limb pain.
But......
- Using powered mobility may lead to weight gain and upper limb deconditioning in a person with tetraplegia.
A power wheelchair can be recommended for:
- High-risk patients:
- A person with a prior injury to the upper limb
- Elderly
- A person living in a challenging environment (hills, uneven or rough terrain)
Manual Wheelchair[edit | edit source]
- The optimal manual wheelchair should be high-strength, fully customisable and made of the lightest possible material.
- The rear axle should be adjusted as far forward as possible without compromising the user's stability.
- A more forward axle position decreases rolling resistance and increases propulsion efficiency.[3]
- Appropriate seated posture and stabilisation relative to balance and stability needs should be assessed.
- Individuals with a C4 and higher SCI must be provided full support for the forearm and hand to decrease subluxation or dislocation.[3]
Wheelchair Modifications/Adaptive Equipment[edit | edit source]
- Wrist extension splint with wheelchair glove over it
- Arm trough support
- Elbow blocks (to assist with arm support during tilt)
- Modular hand pad
- Various joystick options
- Ball, enlarged ball
- T-bar
- U shaped
- Cylinder
- Carrot toggle
- The slip-resistant grip on the wheelchair hand rims (plastic coated or rubber)
- Rubber-coated projections off the push rim however, they impact the chair width
- Extended brake levers
Upper Limb Adaptive Equipment/Assistive Technologies[edit | edit source]
Universal cuff (C5)
- An adaptive device that helps patients with a high-level spinal cord injury grip small objects and perform activities of daily living
- They are considered one of the most useful tools for people with limited control of their hands
- The universal cuff is used to augment or provide upper extremity/hand function to perform activities
- The items remain secure even when the patient cannot grip objects with their fingers - they can still eat a meal, draw, or groom themselves
MAS (Mobile Arm Support)[17] or BFO (Balanced Forearm Orthosis)
- Patients using MAS have minimal strength in their deltoid and biceps muscles.
- Motivated patients with biceps and deltoid muscle strength < 2/5 can benefit from MAS.
- Patients are usually able to perform at least one new activity using a MAS, including eating, page-turning, driving a power wheelchair, brushing teeth, keyboarding, writing, name signing, drawing, painting, scratching nose, playing board games, accessing electronic devices, drinking, and grooming.
- MAS attached to the wheelchair increases wheelchair width. In a reclining position, MAS can cause individuals to have problems managing their arms.[18]
- According to Readioff et al.,[17] MAS facilitates ADL tasks such as eating.
Multidisciplinary and Interdisciplinary SCI Teams[edit | edit source]
All multidisciplinary/interdisciplinary team members are responsible for the upper limb management of individuals with C4 and C5 tetraplegia. Management continues 24 hours/7 days a week. This team includes nursing staff, physicians, physiotherapists, occupational therapists, speech-language pathologists/therapists, family and all other caregivers.
Education
- Education is tailored to the patient's needs with the expectation that this individualisation will improve the intervention results.[20]
- It is important to educate healthcare providers, family, caregivers and persons with SCI about upper limb pain and injury risk.
- Educate on the reduction of the frequency of repetitive upper limb tasks to decrease the risk of developing shoulder pain and shoulder dysfunction:[3]
- Decreasing the number of transfers needed each day
- Altering between a manual wheelchair and a power wheelchair or switching to a power wheelchair as appropriate
- Frequency of propulsive stroke reduction during wheelchair propulsion
- Consider alternative techniques for activities when upper limb pain or injury is present
Mandatory periodic reassessment of the patient's function, ergonomics, and equipment. Assess for:
- Changes in patient's medical status
- Acquisition of new medical problems (e.g. heart disease)
- Changes in patient's weight, muscle mass, pain level
- Effect of ageing on patient's functional status and mobility
ICF and Upper Limb Management[edit | edit source]
The International Classification of Functioning, Disability and Health (ICF) model should be utilised when managing the upper limbs of patients with a spinal cord injury. The ICF helps practitioners to interpret functional outcomes following therapeutic interventions and the provision of adaptive equipment.[21] The following image shows an example ICF assessment sheet for an individual with upper tetraplegia:
Potential treatment interventions based on the results of the assessment using the ICF assessment tool:
- Family and caregiver education on the importance of working towards achieving independence in eating
- Family and caregiver education on choosing an appropriate diet to facilitate the patient's participation during meal times
- Home visit to assess patient's home access for a wheelchair with MAS attachment
- An exercise programme that focuses on neck muscle stretching and strengthening
- Wheelchair seating and positioning assessment to ensure proper neck and head alignment
Resources[edit | edit source]
- Paralyzed Veterans of America Consortium for Spinal Cord Medicine. Preservation of upper limb function following spinal cord injury: a clinical practice guideline for health-care professionals. J Spinal Cord Med. 2005;28(5):434-70.
- Risk Assessment in Pressure Ulcer Prevention
References[edit | edit source]
- ↑ Van Tuijl JH, Janssen-Potten YJ, Seelen HA. Evaluation of upper extremity motor function tests in tetraplegics. Spinal Cord. 2002 Feb;40(2):51-64.
- ↑ Deep V, Vijay V, Malik L. Relationship between capabilities of upper extremity and quality of life in chronic spinal cord injury. International Journal of Multidisciplinary Educational Research, 2021;10: 9(3)
- ↑ 3.0 3.1 3.2 3.3 3.4 3.5 3.6 3.7 3.8 Paralyzed Veterans of America Consortium for Spinal Cord Medicine. Preservation of upper limb function following spinal cord injury: a clinical practice guideline for health-care professionals. J Spinal Cord Med. 2005;28(5):434-70.
- ↑ Rupp R, Biering-Sørensen F, Burns SP, Graves DE, Guest J, Jones L, Read MS, Rodriguez GM, Schuld C, Tansey-Md KE, Walden K. International standards for neurological classification of spinal cord injury: revised 2019. Topics in spinal cord injury rehabilitation. 2021;27(2):1-22.
- ↑ 5.0 5.1 Oelofse W. Upper Limb Management in Upper Tetraplegia - Occupational Therapy Course. Plus 2022
- ↑ Dunn J, Wangdell J. Improving upper limb function. Rehabilitation in Spinal Cord Injuries. 2020 Feb 1:372.
- ↑ Compression Techniques for Edema: Coban Wrapping. Dr Borst's Occupational Therapy Classroom. Available from: https://www.youtube.com/watch?v=kXZsRYVreg4 [last accessed 22/11/2022]
- ↑ Braden BJ, Blanchard S. Risk assessment in pressure ulcer prevention. Krasner, DL, Rodeheaver, GT, Sibbeald, RG (Eds.) Chronic Wound Care: A Clinical Source Book for Healthcare Professionals (. 2001:641-51.
- ↑ Frye SK, Geigle PR, York HS, Sweatman WM. Functional passive range of motion of individuals with chronic cervical spinal cord injury. J Spinal Cord Med. 2020 Mar;43(2):257-263.
- ↑ Harvey LA, Katalinic OM, Herbert RD, Moseley AM, Lannin NA, Schurr K. Stretch for the treatment and prevention of contracture: an abridged republication of a Cochrane Systematic Review. J Physiother. 2017 Apr;63(2):67-75.
- ↑ Mateo S, Roby-Brami A, Reilly KT, Rossetti Y, Collet C, Rode G. Upper limb kinematics after cervical spinal cord injury: a review. J Neuroeng Rehabil. 2015 Jan 30;12:9.
- ↑ Waring WP, Maynard FM. Shoulder pain in acute traumatic quadriplegia. Paraplegia. 1991 Jan;29(1):37-42.
- ↑ Taylor RL, O'Brien L, Brown T. A scoping review of the use of elastic therapeutic tape for neck or upper extremity conditions. Journal of Hand Therapy. 2014 Jul 1;27(3):235-46.
- ↑ Length, Strength and Kinesio Tape: The Upper Trapezius. Available from: https://www.youtube.com/watch?v=3USDcUbKuKE [last accessed 22/11/2022]
- ↑ Kaunnil A, Sansri V, Thongchoomsin S, Permpoonputtana K, Stanley M, Trevittaya P, Thawisuk C, Thichanpiang P. Bridging the Gap between Clinical Service and Academic Education of Hand-Splinting Practice: Perspectives and Experiences of Thai Occupational Therapists. Int J Environ Res Public Health. 2022 Jul 24;19(15):8995.
- ↑ 16.0 16.1 16.2 16.3 Frye SK, Geigle PR. Current U.S. splinting practices for individuals with cervical spinal cord injury. Spinal Cord Ser Cases. 2020 Jun 17;6(1):49.
- ↑ 17.0 17.1 Readioff R, Siddiqui ZK, Stewart C, Fulbrook L, O'Connor RJ, Chadwick EK. Use and evaluation of assistive technologies for upper limb function in tetraplegia. J Spinal Cord Med. 2022 Nov;45(6):809-820.
- ↑ Atkins MS, Baumgarten JM, Yasuda YL, Adkins R, Waters RL, Leung P, Requejo P. Mobile arm supports evidence-based benefits and criteria for use. The journal of spinal cord medicine. 2008 Jan 1;31(4):388-93.
- ↑ Mobile arm support. Available from: https://www.youtube.com/watch?v=z3ZENtlD93Q[last accessed 22/11/2022]
- ↑ Ricci L, Villegente J, Loyal D, Ayav C, Kivits J, Rat AC. Tailored patient therapeutic, educational interventions: A patient-centred communication model. Health Expect. 2022 Feb;25(1):276-289.
- ↑ Cieza A, Kirchberger I, Biering-Sørensen F, Baumberger M, Charlifue S, Post MW, Campbell R, Kovindha A, Ring H, Sinnott A, Kostanjsek N, Stucki G. ICF Core Sets for individuals with spinal cord injury in the long-term context. Spinal Cord. 2010 Apr;48(4):305-12.