Men's Health Physiotherapy Pelvic Assessment: Difference between revisions
No edit summary |
(added one updated reference) |
||
| (33 intermediate revisions by 4 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox"> '''Original Editor '''- [[User:Stacy Schiurring|Stacy Schiurring]] based on the course by [https://members.physio-pedia.com/course_tutor/pierre-roscher/ Pierre Roscher]<br> | <div class="editorbox"> '''Original Editor '''- [[User:Stacy Schiurring|Stacy Schiurring]] based on the course by [https://members.physio-pedia.com/course_tutor/pierre-roscher/ Pierre Roscher]<br> | ||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}}</div> | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}}</div> | ||
== Introduction == | == Introduction == | ||
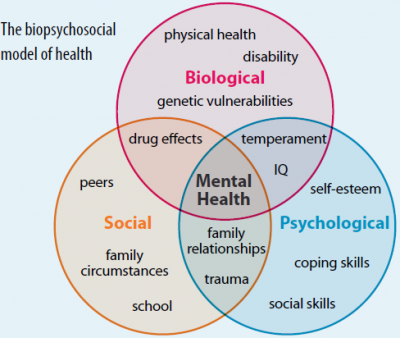
''Disclaimer: This page aims to provide an introductory discussion of men's health physiotherapy assessment techniques. Please note that further training is required through a reputable pelvic health education company before attempting the techniques discussed in this page. See the Resources section at the bottom of this page for links to pelvic and men's health special interest groups.''[[File:Biopsychosocial-model-of-health.PNG|thumb|400x400px|Biopsychosocial Model]] | |||
New information and research is being published frequently on men's pelvic health. Men's health physiotherapy is a quickly expanding and growing speciality area of practice. It is important to practise within a physiotherapy scope of practice and refer to other medical and therapeutic specialities as needed for proper treatment of this medically complex patient population. | |||
Please read here for more in-depth information on the [https://www.physio-pedia.com/Male_Pelvic_Pain#Biopsychosocial_Framework biopsychosocial model with regards to men's health]. Please read here for more general information on the [[Biopsychosocial Model|biopsychosocial model]]. | |||
The use of assessment tools in men's health physiotherapy allows the therapist to track changes over time, but can also serve as a motivator for the patient to see their progress over multiple treatment sessions.<ref name=":0" /> | |||
== The Therapeutic Relationship == | == The Therapeutic Relationship == | ||
It can be uncomfortable for patients to talk about issues related to [[Male Urinary Incontinence|urinary incontinence]] and [[Male Sexual Dysfunction|sexual dysfunction]]. Patients may be embarrassed about discussing these intimate details with their healthcare provider. The development of a strong therapeutic relationship is beneficial as it can help patients feel comfortable and at ease. Confidentiality and privacy are important for pelvic health patients. A private treatment room will allow the patient to feel more comfortable to share sensitive information. It is also advisable to ask whether the patient would like their partner to be present during the session. Patients who have the support of their partners tend to have better therapeutic outcomes.<ref name=":0">Roscher, P. Men's Health Physiotherapy Pelvic Assessment. Men's Health Course. Plus. 2022</ref> | |||
== Subjective Examination/ The Interview == | == Subjective Examination/ The Interview == | ||
Physiotherapy assessments start with a well-structured [[Subjective Assessment|subjective assessment]] to gain insight into the patient's past and current medical and mental state. Subjective interviews should start with well-phrased open-ended question such as ”what can I help you with?" or "what has brought you in to see me today?” Allow the patient time to answer questions without interruption and listen carefully to their ideas, concerns and expectations. After carefully listening to their story, the therapist can then start asking more specific questions to gain further insight into their condition. | |||
=== Questionnaires === | === Questionnaires === | ||
The use of questionnaires may provide a non-threatening strategy for a patient to express their concerning symptoms and highlight areas of concern for the physiotherapist to focus on during the rest of the assessment. Questionnaires may be sent to patients before a scheduled appointment or they may complete them in the room with you.<ref name=":0" /><blockquote>'''Useful Questionnaires for Men's Pelvic Assessments:''' | |||
=== | *'''[https://medicine.umich.edu/sites/default/files/content/downloads/EPIC-2.2002.pdf Expanded Prostate Cancer Index Composite]''' (EPIC): a health-related [[Quality of Life|quality of life]] instrument that measures a wide spectrum of urinary, bowel, sexual, and hormonal symptoms.<ref>Wei JT, Dunn RL, Litwin MS, Sandler HM, Sanda MG. [https://medicine.umich.edu/sites/default/files/content/downloads/Development%20and%20Validation%20of....pdf Development and validation of the expanded prostate cancer index composite (EPIC) for comprehensive assessment of health-related quality of life in men with prostate cancer.] Urology. 2000 Dec 1;56(6):899-905.</ref> The EPIC is a validated instrument recommended by the Fourth International Consultation for Sexual Medicine in 2015.<ref name=":1">Salonia A, Adaikan G, Buvat J, Carrier S, El-Meliegy A, Hatzimouratidis K, McCullough A, Morgentaler A, Torres LO, Khera M. [https://pubmed.ncbi.nlm.nih.gov/28262099/ Sexual rehabilitation after treatment for prostate cancer—part 1: recommendations from the Fourth International Consultation for Sexual Medicine (ICSM 2015]). The journal of sexual medicine. 2017 Mar 1;14(3):285-96.</ref> | ||
*'''[https://files.sld.cu/urologia/files/2011/08/iief.pdf International Index of Erectile Function]''' (IIEF): a self-reported [[Outcome Measures|outcome measure]] to evaluate erectile dysfunction and other sexual problems in men. There is a 5- and 15-question version of this outcome measure.<ref>Neijenhuijs KI, Holtmaat K, Aaronson NK, Holzner B, Terwee CB, Cuijpers P, Verdonck-de Leeuw IM. [https://research.vu.nl/ws/portalfiles/portal/101697857/The_Female_Sexual_Function_Index_FSFI_.pdf The International Index of Erectile Function (IIEF)—a systematic review of measurement properties.] The Journal of Sexual Medicine. 2019 Jul 1;16(7):1078-91.</ref> The IIEF is a validated instrument recommended by the Fourth International Consultation for Sexual Medicine in 2015.<ref name=":1" /> | |||
*'''[https://prd-medweb-cdn.s3.amazonaws.com/documents/transplant/files/Sexual_Health_Survey(men).pdf Erection Hardness Scale]''' (EHS): a self-reported outcome measure to evaluate subjective erection hardness. Research has found that this scale has merit for use in clinical practice, and can complement and supplement other assessment questionnaires.<ref>Yafi FA, Huynh LM, Ahlering T, Rosen R. What is a “validated questionnaire”? A critical review of erectile function assessment. The Journal of Sexual Medicine. 2020 May 1;17(5):849-60.</ref> | |||
*'''[http://www.epicore.ualberta.ca/Documents/PILUTS/Questionnaires/ICIQ-UI%20Short%20Form%20(UK%20English).pdf International Consultation on Incontinence Questionnaire]''' (ICIQ): a questionnaire for evaluating the effect of urinary incontinence frequency and severity on quality of life. This questionnaire has been found to have good validity and reliability.<ref>Uren AD, Cotterill N, Hashim H, Worthington J, Kapoor D, Abrams P. International Consultation on Incontinence Questionnaire‐Satisfaction: psychometric testing of a new patient‐reported outcome measure for the evaluation of satisfaction after urological surgery. BJU international. 2020 Aug;126(2):286-91.</ref> | |||
*'''[https://www.cottagehealth.org/app/files/public/7869d282-4e46-4889-94f9-406ace4f4310/CRH_Chronic_Prostatitis_Symptom_Index.pdf NIH Chronic Prostatitis Symptom Index]''': a questionnaire for the assessment of symptom severity in men with chronic prostatitis/[[Chronic Pelvic Pain Syndrome - Male|chronic pelvic pain syndrome]]. Research has shown this questionnaire to be reliable, valid, and responsive to change.<ref>Litwin MS. [https://citeseerx.ist.psu.edu/viewdoc/download?doi=10.1.1.383.6766&rep=rep1&type=pdf A review of the development and validation of the National Institutes of Health Chronic Prostatitis Symptom Index]. Urology. 2002 Dec 1;60(6):14-8.</ref> | |||
*'''[https://www.scu.edu.au/media/scueduau/current-students/services/counselling/downloads/Depression-Anxiety-Stress-Scales-DASS3481.pdf Depression Anxiety Stress Scales]''' (DASS): an outcome measure designed to assess the fundamental symptoms of [[depression]], anxiety, and [[Stress and Health|stress]]/tension. Research has found this scale to have strong convergent, discriminant, and nomological validity.<ref>Lee D. The convergent, discriminant, and nomological validity of the Depression Anxiety Stress Scales-21 (DASS-21). Journal of affective disorders. 2019 Dec 1;259:136-42.</ref> | |||
*[[Pelvic Floor Distress Inventory (PFDI - 20)|'''Pelvic Floor Distress Inventory''']] (PFDI): a health-related quality of life questionnaire for [[Pelvic Floor Disorders|pelvic floor condition]]<nowiki/>s. The PFDI is recommended by the International Consultation on Incontinence for assessing pelvic floor dysfunction.<ref>de Arruda GT, dos Santos Henrique T, Virtuoso JF. [https://www.researchgate.net/profile/Guilherme-Arruda/publication/350030786_Pelvic_floor_distress_inventory_PFDI-systematic_review_of_measurement_properties/links/60d3727992851c8f7995a767/Pelvic-floor-distress-inventory-PFDI-systematic-review-of-measurement-properties.pdf Pelvic floor distress inventory (PFDI)—systematic review of measurement properties.] International Urogynecology Journal. 2021 Oct;32(10):2657-69.</ref> | |||
*'''[https://kathewallace.com/wp-content/uploads/sites/16/2021/08/Self_Evaluation_of_Breathing_Questionnaire.pdf Self Evaluation of Breathing Questionnaire]''' (SEBQ): was developed to measure breathing-related symptoms and their severity.<ref>Mitchell AJ, Bacon CJ, Moran RW. Reliability and determinants of Self-Evaluation of Breathing Questionnaire (SEBQ) score: a symptoms-based measure of dysfunctional breathing. Applied psychophysiology and biofeedback. 2016 Mar;41(1):111-20.</ref> | |||
</blockquote> | |||
=== Medical History === | |||
It is important to establish a timeline when asking about pelvic health symptoms.<ref name=":0" /> | |||
Gather information about the specific interventions a client has had. It is important to find out all the details of each procedure. For example, if the patient has a history of [[Prostate Cancer|prostate cancer]], ask about specifics such as: the dosage of [[Radiation Side Effects and Syndromes|radiotherapy]] that was given; whether the nerves were spared during a radical prostatectomy; what was the time frame between the diagnosis and intervention for their prostate cancer? | |||
Ask about the timeline for any [[Pain Assessment|pain]], erectile dysfunction or [[Urinary Incontinence|incontinence]]. Is there a history of spinal pain, hip pain or pelvic pain? Are there any psychiatric conditions or other medical conditions for which they are being treated? Have they introduced any new activities or have there been changes in their activities?<ref name=":0" /> | |||
Ask for a complete list of all medication a patient is taking, especially specific medicines for erectile dysfunction<ref name=":0" /> as well as any “herbal” products they may be taking. While the prescription of medication is not within a physiotherapist's scope of practice, it is important to know what the patient is taking to be aware of any interactions or side effects. | |||
== Symptoms == | == Symptoms == | ||
=== Bladder === | === Bladder === | ||
For more information on incontinence, urgency, frequency or any other bladder problems related to men's health physiotherapy, please read [[Male Urinary Incontinence|this article]]. | |||
Once the type of incontinence is recognised, the cause of the incontinence must be identified. Creating a full clinical picture of the patient's incontinence symptoms will help identify the root cause of the incontinence and aid in the creation of an adequate physiotherapy plan of care. <blockquote>'''Examples of assessment questions:''' | |||
* Do they leak with activity e.g. coughing, sneezing, running, jumping or simply just transferring from sitting to standing? (stress incontinence) | |||
* When they leak, is it a lot or a small dribble? | |||
* How frequently do they urinate? (frequency, urgency) | |||
* Do they get a sudden urge and are they unable to delay passing [[urine]]? (frequency, urgency) | |||
* How much is leaking, how many pads are they using per day? | |||
* Do they use pads just in case? (behavioural) | |||
</blockquote>Objective testing of incontinence may involve weighing incontinence pads and keeping strict fluid intake and output measurements over a specific time frame. Weighing of pads is helpful to determine the amount of leakage that is occurring. | |||
Dietary habits play a role in both bladder and bowel health. The volume of fluid intake affects bladder health. Men may restrict fluids to help prevent leaking, but this can result in more concentrated urine that can irritate the bladder and subsequently cause frequency, urgency or urge incontinence. Certain fluids can also irritate the bladder lining such as caffeine, citric juices and alcohol. | |||
A bladder diary is a useful tool to monitor volumes, as well as types of fluid intake. | |||
==== Bladder Diary ==== | |||
A bladder diary is a helpful assessment tool to identify the patient’s pattern and frequency of urination over a 24-hour period.<ref>Mehta S, Geng B, Xu X, Harmanli O. Current state of bladder diary: a survey and review of the literature. International Urogynecology Journal. 2022 Nov 2:1-5.</ref> <blockquote>'''Features of a bladder diary:''' | |||
* Self-reported | |||
* Tracks three-consecutive 24-hour periods | |||
* Patient records all meals and drinks | |||
* Patient records all eliminations (bowel and bladder): | |||
** They should record if they are using male incontinence pads | |||
** If possible, it is preferable that they get an accurate measurement of how much urine they are passing (e.g. use a measuring cup) | |||
* Keeps track of daily activities / activity levels | |||
</blockquote> | |||
Example of how a bladder diary can be useful clinically: | |||
A | * A patient with stress incontinence may record low urine outputs and a high number of used incontinence pads because they are leaking urine throughout the day | ||
* A patient with urge incontinence will record a high number of urinary voids with small output volumes. | |||
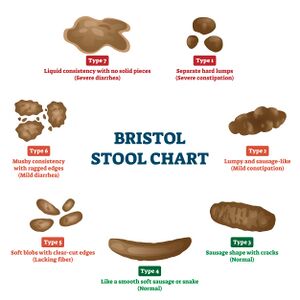
[[File:Bristol stool chart.jpeg|thumb|The Bristol Stool Chart can be helpful in determining if a patient is constipated.]] | |||
=== Bowel Habits === | === Bowel Habits === | ||
When questioning a patient about their bowel habits, it is important to ask about dietary factors, as well as toilet positioning. The ideal position for defecation involves sitting with a forward lean and legs supported in a squat-like position. This allows the anatomical sling of the puborectalis around the rectum to relax and enables a bowel movement.<ref>George SE, Borello-France DF. [https://watermark.silverchair.com/20160110.pdf?token=AQECAHi208BE49Ooan9kkhW_Ercy7Dm3ZL_9Cf3qfKAc485ysgAAAsEwggK9BgkqhkiG9w0BBwagggKuMIICqgIBADCCAqMGCSqGSIb3DQEHATAeBglghkgBZQMEAS4wEQQMpyRueI7fdw2XC3gaAgEQgIICdFGYg6QxUMQkbBdOqWAfdbcqUytE6hnyYu9k7BrRwJ2YcX_Jq1IucFFtQlrKsM3NEZalzF8MLLFWY6woCIKfl0Z2v3HiPPM8uD0Jb2ZDlVoavNKho1xL5U8lGBGfwAdJMntX_SvZBJPfi7_LhJdJohT6VnrPQqU_iTCHSuzBjIU61_K3_qufhN_tIE89tX6xWlJ-Kb77hG1nNwZ6G8dgZ4W0z3Ovg14R_srmVWSoqFCeCSOBTo2ooxWUC-kGpNa5vUshjiKe6PN93HqCaw_jTsLe_plF0zZAM8JNr7eB3cmCuvDhNLy2pb3prPv42u6ACzdPip_SFIGXGPladkwDNv8CNkiPojbQK4KehW6bC4fp-J5dNhRi4q7JwLn6Aw8s-iix7S-tIScpbwe-bM2GkY8MoNReFvmPEPl03hXzbRTstAXiHSEqsResYaf7nMy_seRCor7yaWj59_ILXelCg9zDa-hwo9Q2aMabK6DW4ntQZzzRVCvZMxtZxv2cjilYcLlIPRDvwKNolUAYZGdKBplXjLsHkGYCS-bx6M8yoimsGlMZeS5JecIHMsu9yFThngxqz1PvHW-QvxeMYkv7FyXDb7u6fHNkmi2FFMdWgzqW_v6C26-gGNuwoHkqTe5YuuRSdz3yInsoDfjTN0kvrDLV4yEiNZ_O7vaMwrVk7oXKO_zTaOV5AYfg1KhNxZLqafR92j9O2sjQWwJMrRV52T4Z2-ZxXbP9xb44Lt3OXd5SGsvSjPsG1J1G_69j4dQISds4rYCK8lD5gPFcD1cgvF8EbyPkIUjk6b9GT1M4X5HfExcnHd_LgD8vkRi8qNXG1rGeKN8 Perspective on physical therapist management of functional constipation.] Physical therapy. 2017 Apr 1;97(4):478-93.</ref> | |||
=== Sexual Dysfunction === | === Sexual Dysfunction === | ||
Men can be uncomfortable talking about specific issues related to sexual dysfunction. Using the EPIC and IIEF questionnaires is particularly helpful to open up a dialogue about what type of dysfunction a patient is experiencing.<ref>Heidenreich A, Bellmunt J, Bolla M, Joniau S, Mason M, Matveev V, Mottet N, Schmid HP, van der Kwast T, Wiegel T, Zattoni F. [https://www.academia.edu/download/41881536/EAU Guidelines on Prostate Cancer. Part 20160202-3844-5587l1.pdf EAU guidelines on prostate cancer. Part 1: screening, diagnosis, and treatment of clinically localised disease]. European urology. 2011 Jan 1;59(1):61-71.</ref> A clear clinical picture of the causes of sexual dysfunction is key for successful sexual rehabilitation. | |||
Sexual dysfunction symptoms to screen for | For more information on sexual dysfunction, please read [[Male Sexual Dysfunction|this article]].<blockquote>'''Sexual dysfunction symptoms to screen for:''' | ||
* Erectile dysfunction (ED) | * Erectile dysfunction (ED) | ||
| Line 65: | Line 94: | ||
* Orgasm-associated incontinence | * Orgasm-associated incontinence | ||
* Urinary incontinence in relation to sexual stimulation | * Urinary incontinence in relation to sexual stimulation | ||
* Altered perception of orgasm | * Altered perception of orgasm | ||
* Orgasm associated pain | * Orgasm associated pain | ||
* Penile shortening | * Penile shortening | ||
* Penile deformity | * Penile deformity | ||
</blockquote> | |||
=== | === Pain === | ||
Pain can occur after treatment for | Men can experience different types of pelvic and sexual related pain. Use of questionnaires can help open conversations about a patient's pain. It can be helpful to have the patient's partner present during these conversations for moral support and patient comfort. | ||
Pain can occur after treatment for prostate cancer. Post-operative pain after a radical prostatectomy typically resolves. However, pain can become persistent for a few reasons. Continued spasm in the pelvic floor muscles can result in persistent [[Nociception|nociceptive pain]] and injury to the surrounding nerves can result in [[Neuropathic Pain|neuropathic pain]]. Focused questioning around the type of pain, area of pain, aggravating and easing factors, as well as a 24-hour pattern can help to determine the source of the painful symptoms. | |||
Pain can come from the pelvic floor due to chronic prostatitis e.g. [[Chronic Pelvic Pain Syndrome - Male|chronic pelvic pain syndrome]] (CPPS). For more information on pelvic floor pain as related to men's health physiotherapy, please read [[Male Pelvic Pain|this article]]. | |||
A patient can experience penile or scrotal pain. [http://peterdornanphysio.com.au/pudendal.html Peter Dornan PT] published a map of the [[Pudendal Neuralgia|pudendal nerve]] which outlines different dysfunctions of each of the three branches and how each branch can influence pelvic pain. This can be very useful in the differential diagnosis for pelvic pain. [https://www.pelvicpain.org.au/the-pudendal-nerve/ The Pelvic Pain Foundation of Australia] shares information on pudendal neuralgia (PN), as well as a useful [https://www.pelvicpain.org.au/wp-content/uploads/2019/04/Pudendal-nerve-50.jpg diagram] adapted from Peter Dornan's work. See this article for more information on [[Pudendal Neuralgia|pudendal neuralgia]]. | |||
== Objective Assessment or Physical Examination == | == Objective Assessment or Physical Examination == | ||
The physiotherapy physical examination is important to assess | The physiotherapy physical examination is important to assess pelvic floor function. Assessment of the male pelvic floor will determine if it has adequate muscle strength, length, coordination and endurance to function optimally. The objective examination should be based on the findings from the subjective interview and used to determine the origins of reported symptoms. | ||
There are a few ways to assess the male pelvic floor objectively. | There are a few ways to assess the male pelvic floor objectively. | ||
=== External Observation === | === External Observation === | ||
External observation of the scrotum, testicles and penis during a pelvic floor muscle | External observation of the scrotum, testicles and penis during a pelvic floor muscle contraction can be observed. In men, a correct pelvic floor contraction will result in a lifting action of the penis. <blockquote>'''Male pelvic floor contraction, external observation of genitals:''' | ||
* Incorrect technique: any bearing down during contraction | |||
* Correct technique: a lifting action during contraction | |||
</blockquote> | |||
== | === Musculoskeletal and Neuromuscular Assessments === | ||
Musculoskeletal and / or neuromuscular assessments may not be necessary for all men's health patients. It is important to use your clinical judgment to determine when these assessments may be appropriate. For example, when examining a patient with pelvic pain, it is often helpful to assess the [[Lumbar Anatomy|lumbar spine]] and [[Hip Anatomy|hips]], and do a [[Neurological Assessment|neurological examination]] of the spine.<ref name=":0" /> | |||
Breathing assessments are also helpful, especially in men's health patients who have pressure issues, such as urinary or faecal incontinence. For these patients, an assessment of the [[Thoracic Examination|thoracic spine]] and [[Ribs|rib]] mobility would be indicated.<ref name=":0" /> | |||
[[Abdominal Muscles|Abdominal]] assessments may be indicated as well. Recall that the abdominal [[fascia]] is continuous with the groin, scrotum, and penile tissue. Any sort of injury or abdominal surgery could affect the mobility of the fascia.<ref name=":0" /> | |||
=== Real-Time Ultrasound Testing (RTUS) === | |||
Transabdominal RTUS is a valid and reliable objective method of measuring the function of the male pelvic floor.<ref name=":2">Stafford RE, Ashton-Miller JA, Constantinou CE, Hodges PW. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4106154/ Novel insight into the dynamics of male pelvic floor contractions through transperineal ultrasound imaging.] The Journal of urology. 2012 Oct;188(4):1224-30.</ref> | |||
'''Supra-pubic method:''' An ultrasound (US) probe is placed on the lower abdomen supra-pubically in a mid-sagittal location. A clear transverse image of the bladder is seen if the bladder has enough urine in it. If the patient is asked to perform a pelvic floor contraction, a bladder base (floor) lift in the cephalad direction can be visualised.<ref>Nahon I, Waddington G, Adams R, Dorey G. Assessing muscle function of the male pelvic floor using real time ultrasound. Neurourology and urodynamics. 2011 Sep;30(7):1329-32.</ref> | |||
'''Trans-perineal method:''' The US probe is placed on the perineum, mid-sagittal between the anus and the penis. Sagittal images of the bladder are obtained. From this view, it is possible to assess and focus on anterior structures of the male pelvic floor. This can be useful for visualising pelvic floor contractions, which is helpful for both the clinician (i.e. for the assessment) and as a tool for patient education.<ref name=":2" /> <blockquote>'''Limitations of RTUS:''' | |||
=== | * The supra-pubic method cannot identify specific components of the pelvic floor<ref name=":3">Milios JE. [https://api.research-repository.uwa.edu.au/portalfiles/portal/54573972/THESIS DOCTOR OF PHILOSOPHY MILIOS Joanne Elizabeth 2019.pdf Therapeutic interventions for patients with prostate cancer undergoing radical prostatectomy: A focus on urinary incontinence, erectile dysfunction and Peyronie’s disease]. Thesis Document University of Western Australia. 2019</ref> | ||
* For the supra-pubic method, the bladder must be relatively full of urine which can be a problem for men with more severe continence problems<ref name=":3" /> | |||
* Regardless of which method is used, RTUS cannot differentiate if an absence of pelvic floor movement is due to a lack of mobility (e.g. tightness or spasm of the pelvic floor muscles) or weakness / absence of active muscle contraction<ref>Stafford RE, Coughlin G, Lutton NJ, Hodges PW. Validity of estimation of pelvic floor muscle activity from transperineal ultrasound imaging in men. PLoS One. 2015;10(12).</ref> | |||
</blockquote>In light of these limitations, it is clear that clinicians must look at the full clinical picture of the patient, and not only at isolated findings. | |||
The following short video demonstrates supra-pubic transabdominal RTUS. Please watch at time 5:30 to see the sustained endurance test discussed below. | |||
{{#ev:youtube| 122YOTqA5as |500}}<ref>YoutTube. Real Time Ultrasound Rehabilitation of the Pelvic Floor. Available from: https://www.youtube.com/watch?v=122YOTqA5as&t=38s [last accessed 03/04/2022]</ref> | |||
=== Internal Assessment === | |||
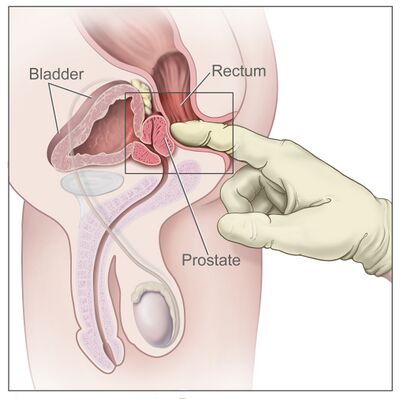
[[File:Digital rectal exam nci-vol-7136-300.jpg|thumb|400x400px|Digital Rectal Exam]] | |||
''An internal assessment of the pelvic floor is a highly skilled procedure which requires specialisation and advanced training. An internal assessment should not be performed until the physiotherapist is clinically competent.'' | |||
A digital rectal examination (DRE) can be performed to evaluate the effectiveness of a pelvic floor muscle contraction and to determine if there are any tight or painful internal structures. This is a relatively invasive assessment option and can be quite painful, especially in patients who are post-radical prostatectomy.<ref>Romero FR, Romero KR, Brenny Filho T, Pilati R, Kulysz D, de Oliveira Júnior FC. [https://www.redalyc.org/pdf/1810/181013948019.pdf Reasons why patients reject digital rectal examination when screening for prostate cancer.] Archivos espanoles de urologia. 2008;61(6):759-65.</ref> DRE is not recommended for urinary incontinence assessment as it may not be reliable in assessing the muscles primarily responsible for urethral closure pressure.<ref>Frawley HC, Galea MP, Phillips BA, Sherburn M, Bø K. [https://www.academia.edu/download/47096496/nau.2020120160707-4818-p9pcff.pdf Reliability of pelvic floor muscle strength assessment using different test positions and tools.] Neurourology and Urodynamics: Official Journal of the International Continence Society. 2006;25(3):236-42.</ref> For patients after radiation that are experiencing tightness and spasm of the pelvic floor, a DRE can be helpful to feel the soft tissue limitations and muscle trigger points. | |||
RTUS is an alternative to DRE. It can be used when DRE is contraindicated<ref>Nahon I, Waddington G, Adams R, Dorey G. Assessing muscle function of the male pelvic floor using real time ultrasound. Neurourology and urodynamics. 2011 Sep;30(7):1329-32.</ref> or when male patients are uncomfortable or reluctant to have a DRE. <blockquote>'''DRE Contraindications:''' | |||
If a prostate infection is suspected, the examination should be deferred until the infection has resolved. | |||
'''Absolute:''' | |||
* Absence of anus | |||
* Immunosuppressed patient | |||
* Imperforate anus | |||
* Prolapsed thrombosed internal haemorrhoids | |||
* Stricture | |||
* Severe anal pain | |||
* Unwilling patient | |||
'''Relative:''' | |||
* Acute abdomen | |||
* Coagulopathy | |||
* Major rectal trauma | |||
* Post-operative anal surgery | |||
* Recent acute myocardial infarction | |||
* Valvular heart disease or prosthetic valves | |||
</blockquote><ref>JA VH, Abdussalam A, Kasi A. [https://europepmc.org/article/nbk/nbk537356 Rectal Exam]. 07 Feb 2019</ref> | |||
=== Standardised Tests === | |||
<blockquote>'''The following standardised tests can be used to assess pelvic floor muscle ability:''' | |||
* '''Rapid Response Test''' (RRT): patients are instructed to “perform 10 maximal pelvic floor muscle contractions and relaxations as fast as possible” with the elapsed time recorded as the outcome measure. | |||
* '''Sustained Endurance Test''' (SET): patients are instructed to “hold a maximal contraction for as long as possible, whilst continuing to breathe” with the clasped time recorded as the outcome measure. | |||
</blockquote>Verbal instructions to perform a correct pelvic floor muscle contraction are: “stop the flow of urine and shorten the penis while continuing to breathe.”<ref>Milios JE, Atkinson CL, Naylor LH, Millar D, Thijssen DH, Ackland TR, Green DJ. [https://centralspecialistcentre.com/wp-content/uploads/2018/11/Pelvic-floor-muscle-assessment-in-men-post-prostatectomy.pdf Pelvic floor muscle assessment in men post prostatectomy: comparing digital rectal examination and real-time ultrasound approaches.] Australian and New Zealand Continence Journal, The. 2018 Dec;24(4):105-11.</ref> | |||
== Patient Education == | == Patient Education == | ||
Pelvic floor disorders, incontinence and sexual dysfunction can be very overwhelming. Providing patient education on these conditions is helpful and empowering to the patient. Establishing the patient's base knowledge is important to ensure appropriate knowledge is being shared in the most beneficial manner. <blockquote>'''When sharing information:''' | |||
* Do not to use complex medical jargon | |||
* Give information the patient is ready to understand | |||
* Use visual aids and pictures to help with the explanations | |||
* Provide take home resources | |||
* Ask if the patient would like their partner present during education sessions | |||
</blockquote> | |||
== Resources | == Resources == | ||
'''Links to questionnaires and assessment forms:''' | |||
* [https://medicine.umich.edu/sites/default/files/content/downloads/EPIC-2.2002.pdf Expanded Prostate Cancer Index Composite] | |||
* [https://files.sld.cu/urologia/files/2011/08/iief.pdf International Index of Erectile Function] | |||
* [https://prd-medweb-cdn.s3.amazonaws.com/documents/transplant/files/Sexual_Health_Survey(men).pdf Erection Hardness Scale] | |||
* [http://www.epicore.ualberta.ca/Documents/PILUTS/Questionnaires/ICIQ-UI%20Short%20Form%20(UK%20English).pdf International Consultation on Incontinence Questionnaire] | |||
* [https://www.cottagehealth.org/app/files/public/7869d282-4e46-4889-94f9-406ace4f4310/CRH_Chronic_Prostatitis_Symptom_Index.pdf NIH Chronic Prostatitis Symptom Index] | |||
* [https://www.scu.edu.au/media/scueduau/current-students/services/counselling/downloads/Depression-Anxiety-Stress-Scales-DASS3481.pdf Depression Anxiety Stress Scales] | |||
* [https://kathewallace.com/wp-content/uploads/sites/16/2015/06/PFDI-20.pdf Pelvic Floor Distress Inventory] | |||
* [https://kathewallace.com/wp-content/uploads/sites/16/2021/08/Self_Evaluation_of_Breathing_Questionnaire.pdf Self Evaluation of Breathing Questionnaire] | |||
* [https://www.urologyhealth.org/educational-resources/bladder-diary Bladder Diary Form] | |||
'''Patient Education Handouts:''' | |||
* Johns Hopkins Medicine list of [https://www.hopkinsmedicine.org/johns_hopkins_bayview/_docs/medical_services/gynecology_obstetrics/bladder_irritants.pdf dietary bladder irritants] | |||
* Kaiser Permanente Medicine list of [https://mydoctor.kaiserpermanente.org/ncal/Images/Bladder_Irritants_MDO_tcm75-287907.pdf dietary bladder irritants] | |||
'''Clinical Resources:''' | |||
* [https://www.pelvicpain.org.au/wp-content/uploads/2019/04/Pudendal-nerve-50.jpg Pudendal Nerve Map] | |||
'''Professional Associations and Formal Continuing Education Courses:''' | |||
*American Physical Therapy Association: [https://aptapelvichealth.org/ Academy of Pelvic Health] | |||
* American Physical Therapy Association: [https://apta.site-ym.com/store/ViewProduct.aspx?id=14929266 On-Demand: Male Pelvic Pain Course] | |||
*Australian Physiotherapy Association: [https://choose.physio/your-lifestage/adults/mens-health Men's Health] | |||
* Australian Physiotherapy Association: [https://australian.physio/inmotion/physiotherapy-and-male-pelvic-health Male Pelvic Health] | |||
== References == | == References == | ||
<references /> | <references /> | ||
[[Category:Course Pages]] | |||
[[Category:Mens Health]] | |||
[[Category:Plus Content]] | |||
Latest revision as of 07:00, 30 January 2023
Top Contributors - Stacy Schiurring, Kim Jackson, Jess Bell and Lucinda hampton
Introduction[edit | edit source]
Disclaimer: This page aims to provide an introductory discussion of men's health physiotherapy assessment techniques. Please note that further training is required through a reputable pelvic health education company before attempting the techniques discussed in this page. See the Resources section at the bottom of this page for links to pelvic and men's health special interest groups.
New information and research is being published frequently on men's pelvic health. Men's health physiotherapy is a quickly expanding and growing speciality area of practice. It is important to practise within a physiotherapy scope of practice and refer to other medical and therapeutic specialities as needed for proper treatment of this medically complex patient population.
Please read here for more in-depth information on the biopsychosocial model with regards to men's health. Please read here for more general information on the biopsychosocial model.
The use of assessment tools in men's health physiotherapy allows the therapist to track changes over time, but can also serve as a motivator for the patient to see their progress over multiple treatment sessions.[1]
The Therapeutic Relationship[edit | edit source]
It can be uncomfortable for patients to talk about issues related to urinary incontinence and sexual dysfunction. Patients may be embarrassed about discussing these intimate details with their healthcare provider. The development of a strong therapeutic relationship is beneficial as it can help patients feel comfortable and at ease. Confidentiality and privacy are important for pelvic health patients. A private treatment room will allow the patient to feel more comfortable to share sensitive information. It is also advisable to ask whether the patient would like their partner to be present during the session. Patients who have the support of their partners tend to have better therapeutic outcomes.[1]
Subjective Examination/ The Interview[edit | edit source]
Physiotherapy assessments start with a well-structured subjective assessment to gain insight into the patient's past and current medical and mental state. Subjective interviews should start with well-phrased open-ended question such as ”what can I help you with?" or "what has brought you in to see me today?” Allow the patient time to answer questions without interruption and listen carefully to their ideas, concerns and expectations. After carefully listening to their story, the therapist can then start asking more specific questions to gain further insight into their condition.
Questionnaires[edit | edit source]
The use of questionnaires may provide a non-threatening strategy for a patient to express their concerning symptoms and highlight areas of concern for the physiotherapist to focus on during the rest of the assessment. Questionnaires may be sent to patients before a scheduled appointment or they may complete them in the room with you.[1]
Useful Questionnaires for Men's Pelvic Assessments:
- Expanded Prostate Cancer Index Composite (EPIC): a health-related quality of life instrument that measures a wide spectrum of urinary, bowel, sexual, and hormonal symptoms.[2] The EPIC is a validated instrument recommended by the Fourth International Consultation for Sexual Medicine in 2015.[3]
- International Index of Erectile Function (IIEF): a self-reported outcome measure to evaluate erectile dysfunction and other sexual problems in men. There is a 5- and 15-question version of this outcome measure.[4] The IIEF is a validated instrument recommended by the Fourth International Consultation for Sexual Medicine in 2015.[3]
- Erection Hardness Scale (EHS): a self-reported outcome measure to evaluate subjective erection hardness. Research has found that this scale has merit for use in clinical practice, and can complement and supplement other assessment questionnaires.[5]
- International Consultation on Incontinence Questionnaire (ICIQ): a questionnaire for evaluating the effect of urinary incontinence frequency and severity on quality of life. This questionnaire has been found to have good validity and reliability.[6]
- NIH Chronic Prostatitis Symptom Index: a questionnaire for the assessment of symptom severity in men with chronic prostatitis/chronic pelvic pain syndrome. Research has shown this questionnaire to be reliable, valid, and responsive to change.[7]
- Depression Anxiety Stress Scales (DASS): an outcome measure designed to assess the fundamental symptoms of depression, anxiety, and stress/tension. Research has found this scale to have strong convergent, discriminant, and nomological validity.[8]
- Pelvic Floor Distress Inventory (PFDI): a health-related quality of life questionnaire for pelvic floor conditions. The PFDI is recommended by the International Consultation on Incontinence for assessing pelvic floor dysfunction.[9]
- Self Evaluation of Breathing Questionnaire (SEBQ): was developed to measure breathing-related symptoms and their severity.[10]
Medical History[edit | edit source]
It is important to establish a timeline when asking about pelvic health symptoms.[1]
Gather information about the specific interventions a client has had. It is important to find out all the details of each procedure. For example, if the patient has a history of prostate cancer, ask about specifics such as: the dosage of radiotherapy that was given; whether the nerves were spared during a radical prostatectomy; what was the time frame between the diagnosis and intervention for their prostate cancer?
Ask about the timeline for any pain, erectile dysfunction or incontinence. Is there a history of spinal pain, hip pain or pelvic pain? Are there any psychiatric conditions or other medical conditions for which they are being treated? Have they introduced any new activities or have there been changes in their activities?[1]
Ask for a complete list of all medication a patient is taking, especially specific medicines for erectile dysfunction[1] as well as any “herbal” products they may be taking. While the prescription of medication is not within a physiotherapist's scope of practice, it is important to know what the patient is taking to be aware of any interactions or side effects.
Symptoms[edit | edit source]
Bladder[edit | edit source]
For more information on incontinence, urgency, frequency or any other bladder problems related to men's health physiotherapy, please read this article.
Once the type of incontinence is recognised, the cause of the incontinence must be identified. Creating a full clinical picture of the patient's incontinence symptoms will help identify the root cause of the incontinence and aid in the creation of an adequate physiotherapy plan of care.
Examples of assessment questions:
- Do they leak with activity e.g. coughing, sneezing, running, jumping or simply just transferring from sitting to standing? (stress incontinence)
- When they leak, is it a lot or a small dribble?
- How frequently do they urinate? (frequency, urgency)
- Do they get a sudden urge and are they unable to delay passing urine? (frequency, urgency)
- How much is leaking, how many pads are they using per day?
- Do they use pads just in case? (behavioural)
Objective testing of incontinence may involve weighing incontinence pads and keeping strict fluid intake and output measurements over a specific time frame. Weighing of pads is helpful to determine the amount of leakage that is occurring.
Dietary habits play a role in both bladder and bowel health. The volume of fluid intake affects bladder health. Men may restrict fluids to help prevent leaking, but this can result in more concentrated urine that can irritate the bladder and subsequently cause frequency, urgency or urge incontinence. Certain fluids can also irritate the bladder lining such as caffeine, citric juices and alcohol.
A bladder diary is a useful tool to monitor volumes, as well as types of fluid intake.
Bladder Diary[edit | edit source]
A bladder diary is a helpful assessment tool to identify the patient’s pattern and frequency of urination over a 24-hour period.[11]
Features of a bladder diary:
- Self-reported
- Tracks three-consecutive 24-hour periods
- Patient records all meals and drinks
- Patient records all eliminations (bowel and bladder):
- They should record if they are using male incontinence pads
- If possible, it is preferable that they get an accurate measurement of how much urine they are passing (e.g. use a measuring cup)
- Keeps track of daily activities / activity levels
Example of how a bladder diary can be useful clinically:
- A patient with stress incontinence may record low urine outputs and a high number of used incontinence pads because they are leaking urine throughout the day
- A patient with urge incontinence will record a high number of urinary voids with small output volumes.
Bowel Habits[edit | edit source]
When questioning a patient about their bowel habits, it is important to ask about dietary factors, as well as toilet positioning. The ideal position for defecation involves sitting with a forward lean and legs supported in a squat-like position. This allows the anatomical sling of the puborectalis around the rectum to relax and enables a bowel movement.[12]
Sexual Dysfunction[edit | edit source]
Men can be uncomfortable talking about specific issues related to sexual dysfunction. Using the EPIC and IIEF questionnaires is particularly helpful to open up a dialogue about what type of dysfunction a patient is experiencing.[13] A clear clinical picture of the causes of sexual dysfunction is key for successful sexual rehabilitation.
For more information on sexual dysfunction, please read this article.
Sexual dysfunction symptoms to screen for:
- Erectile dysfunction (ED)
- Sexual interest dysfunctions
- Sexual arousal dysfunctions
- Premature/rapid/early or delayed ejaculation
- Anejaculation
- Orgasmic dysfunction
- Sexual aversion disorder
- Priapism (prolonged erection of the penis)
- Peyronie’s disease (a painful curvature of the penis)
- Orgasm-associated incontinence
- Urinary incontinence in relation to sexual stimulation
- Altered perception of orgasm
- Orgasm associated pain
- Penile shortening
- Penile deformity
Pain[edit | edit source]
Men can experience different types of pelvic and sexual related pain. Use of questionnaires can help open conversations about a patient's pain. It can be helpful to have the patient's partner present during these conversations for moral support and patient comfort.
Pain can occur after treatment for prostate cancer. Post-operative pain after a radical prostatectomy typically resolves. However, pain can become persistent for a few reasons. Continued spasm in the pelvic floor muscles can result in persistent nociceptive pain and injury to the surrounding nerves can result in neuropathic pain. Focused questioning around the type of pain, area of pain, aggravating and easing factors, as well as a 24-hour pattern can help to determine the source of the painful symptoms.
Pain can come from the pelvic floor due to chronic prostatitis e.g. chronic pelvic pain syndrome (CPPS). For more information on pelvic floor pain as related to men's health physiotherapy, please read this article.
A patient can experience penile or scrotal pain. Peter Dornan PT published a map of the pudendal nerve which outlines different dysfunctions of each of the three branches and how each branch can influence pelvic pain. This can be very useful in the differential diagnosis for pelvic pain. The Pelvic Pain Foundation of Australia shares information on pudendal neuralgia (PN), as well as a useful diagram adapted from Peter Dornan's work. See this article for more information on pudendal neuralgia.
Objective Assessment or Physical Examination[edit | edit source]
The physiotherapy physical examination is important to assess pelvic floor function. Assessment of the male pelvic floor will determine if it has adequate muscle strength, length, coordination and endurance to function optimally. The objective examination should be based on the findings from the subjective interview and used to determine the origins of reported symptoms.
There are a few ways to assess the male pelvic floor objectively.
External Observation[edit | edit source]
External observation of the scrotum, testicles and penis during a pelvic floor muscle contraction can be observed. In men, a correct pelvic floor contraction will result in a lifting action of the penis.
Male pelvic floor contraction, external observation of genitals:
- Incorrect technique: any bearing down during contraction
- Correct technique: a lifting action during contraction
Musculoskeletal and Neuromuscular Assessments[edit | edit source]
Musculoskeletal and / or neuromuscular assessments may not be necessary for all men's health patients. It is important to use your clinical judgment to determine when these assessments may be appropriate. For example, when examining a patient with pelvic pain, it is often helpful to assess the lumbar spine and hips, and do a neurological examination of the spine.[1]
Breathing assessments are also helpful, especially in men's health patients who have pressure issues, such as urinary or faecal incontinence. For these patients, an assessment of the thoracic spine and rib mobility would be indicated.[1]
Abdominal assessments may be indicated as well. Recall that the abdominal fascia is continuous with the groin, scrotum, and penile tissue. Any sort of injury or abdominal surgery could affect the mobility of the fascia.[1]
Real-Time Ultrasound Testing (RTUS)[edit | edit source]
Transabdominal RTUS is a valid and reliable objective method of measuring the function of the male pelvic floor.[14]
Supra-pubic method: An ultrasound (US) probe is placed on the lower abdomen supra-pubically in a mid-sagittal location. A clear transverse image of the bladder is seen if the bladder has enough urine in it. If the patient is asked to perform a pelvic floor contraction, a bladder base (floor) lift in the cephalad direction can be visualised.[15]
Trans-perineal method: The US probe is placed on the perineum, mid-sagittal between the anus and the penis. Sagittal images of the bladder are obtained. From this view, it is possible to assess and focus on anterior structures of the male pelvic floor. This can be useful for visualising pelvic floor contractions, which is helpful for both the clinician (i.e. for the assessment) and as a tool for patient education.[14]
Limitations of RTUS:
- The supra-pubic method cannot identify specific components of the pelvic floor[16]
- For the supra-pubic method, the bladder must be relatively full of urine which can be a problem for men with more severe continence problems[16]
- Regardless of which method is used, RTUS cannot differentiate if an absence of pelvic floor movement is due to a lack of mobility (e.g. tightness or spasm of the pelvic floor muscles) or weakness / absence of active muscle contraction[17]
In light of these limitations, it is clear that clinicians must look at the full clinical picture of the patient, and not only at isolated findings.
The following short video demonstrates supra-pubic transabdominal RTUS. Please watch at time 5:30 to see the sustained endurance test discussed below.
Internal Assessment[edit | edit source]
An internal assessment of the pelvic floor is a highly skilled procedure which requires specialisation and advanced training. An internal assessment should not be performed until the physiotherapist is clinically competent.
A digital rectal examination (DRE) can be performed to evaluate the effectiveness of a pelvic floor muscle contraction and to determine if there are any tight or painful internal structures. This is a relatively invasive assessment option and can be quite painful, especially in patients who are post-radical prostatectomy.[19] DRE is not recommended for urinary incontinence assessment as it may not be reliable in assessing the muscles primarily responsible for urethral closure pressure.[20] For patients after radiation that are experiencing tightness and spasm of the pelvic floor, a DRE can be helpful to feel the soft tissue limitations and muscle trigger points.
RTUS is an alternative to DRE. It can be used when DRE is contraindicated[21] or when male patients are uncomfortable or reluctant to have a DRE.
DRE Contraindications:
If a prostate infection is suspected, the examination should be deferred until the infection has resolved.
Absolute:
- Absence of anus
- Immunosuppressed patient
- Imperforate anus
- Prolapsed thrombosed internal haemorrhoids
- Stricture
- Severe anal pain
- Unwilling patient
Relative:
- Acute abdomen
- Coagulopathy
- Major rectal trauma
- Post-operative anal surgery
- Recent acute myocardial infarction
- Valvular heart disease or prosthetic valves
Standardised Tests[edit | edit source]
The following standardised tests can be used to assess pelvic floor muscle ability:
- Rapid Response Test (RRT): patients are instructed to “perform 10 maximal pelvic floor muscle contractions and relaxations as fast as possible” with the elapsed time recorded as the outcome measure.
- Sustained Endurance Test (SET): patients are instructed to “hold a maximal contraction for as long as possible, whilst continuing to breathe” with the clasped time recorded as the outcome measure.
Verbal instructions to perform a correct pelvic floor muscle contraction are: “stop the flow of urine and shorten the penis while continuing to breathe.”[23]
Patient Education[edit | edit source]
Pelvic floor disorders, incontinence and sexual dysfunction can be very overwhelming. Providing patient education on these conditions is helpful and empowering to the patient. Establishing the patient's base knowledge is important to ensure appropriate knowledge is being shared in the most beneficial manner.
When sharing information:
- Do not to use complex medical jargon
- Give information the patient is ready to understand
- Use visual aids and pictures to help with the explanations
- Provide take home resources
- Ask if the patient would like their partner present during education sessions
Resources[edit | edit source]
Links to questionnaires and assessment forms:
- Expanded Prostate Cancer Index Composite
- International Index of Erectile Function
- Erection Hardness Scale
- International Consultation on Incontinence Questionnaire
- NIH Chronic Prostatitis Symptom Index
- Depression Anxiety Stress Scales
- Pelvic Floor Distress Inventory
- Self Evaluation of Breathing Questionnaire
Patient Education Handouts:
- Johns Hopkins Medicine list of dietary bladder irritants
- Kaiser Permanente Medicine list of dietary bladder irritants
Clinical Resources:
Professional Associations and Formal Continuing Education Courses:
- American Physical Therapy Association: Academy of Pelvic Health
- American Physical Therapy Association: On-Demand: Male Pelvic Pain Course
- Australian Physiotherapy Association: Men's Health
- Australian Physiotherapy Association: Male Pelvic Health
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 1.7 1.8 Roscher, P. Men's Health Physiotherapy Pelvic Assessment. Men's Health Course. Plus. 2022
- ↑ Wei JT, Dunn RL, Litwin MS, Sandler HM, Sanda MG. Development and validation of the expanded prostate cancer index composite (EPIC) for comprehensive assessment of health-related quality of life in men with prostate cancer. Urology. 2000 Dec 1;56(6):899-905.
- ↑ 3.0 3.1 Salonia A, Adaikan G, Buvat J, Carrier S, El-Meliegy A, Hatzimouratidis K, McCullough A, Morgentaler A, Torres LO, Khera M. Sexual rehabilitation after treatment for prostate cancer—part 1: recommendations from the Fourth International Consultation for Sexual Medicine (ICSM 2015). The journal of sexual medicine. 2017 Mar 1;14(3):285-96.
- ↑ Neijenhuijs KI, Holtmaat K, Aaronson NK, Holzner B, Terwee CB, Cuijpers P, Verdonck-de Leeuw IM. The International Index of Erectile Function (IIEF)—a systematic review of measurement properties. The Journal of Sexual Medicine. 2019 Jul 1;16(7):1078-91.
- ↑ Yafi FA, Huynh LM, Ahlering T, Rosen R. What is a “validated questionnaire”? A critical review of erectile function assessment. The Journal of Sexual Medicine. 2020 May 1;17(5):849-60.
- ↑ Uren AD, Cotterill N, Hashim H, Worthington J, Kapoor D, Abrams P. International Consultation on Incontinence Questionnaire‐Satisfaction: psychometric testing of a new patient‐reported outcome measure for the evaluation of satisfaction after urological surgery. BJU international. 2020 Aug;126(2):286-91.
- ↑ Litwin MS. A review of the development and validation of the National Institutes of Health Chronic Prostatitis Symptom Index. Urology. 2002 Dec 1;60(6):14-8.
- ↑ Lee D. The convergent, discriminant, and nomological validity of the Depression Anxiety Stress Scales-21 (DASS-21). Journal of affective disorders. 2019 Dec 1;259:136-42.
- ↑ de Arruda GT, dos Santos Henrique T, Virtuoso JF. Pelvic floor distress inventory (PFDI)—systematic review of measurement properties. International Urogynecology Journal. 2021 Oct;32(10):2657-69.
- ↑ Mitchell AJ, Bacon CJ, Moran RW. Reliability and determinants of Self-Evaluation of Breathing Questionnaire (SEBQ) score: a symptoms-based measure of dysfunctional breathing. Applied psychophysiology and biofeedback. 2016 Mar;41(1):111-20.
- ↑ Mehta S, Geng B, Xu X, Harmanli O. Current state of bladder diary: a survey and review of the literature. International Urogynecology Journal. 2022 Nov 2:1-5.
- ↑ George SE, Borello-France DF. Perspective on physical therapist management of functional constipation. Physical therapy. 2017 Apr 1;97(4):478-93.
- ↑ Heidenreich A, Bellmunt J, Bolla M, Joniau S, Mason M, Matveev V, Mottet N, Schmid HP, van der Kwast T, Wiegel T, Zattoni F. EAU guidelines on prostate cancer. Part 1: screening, diagnosis, and treatment of clinically localised disease. European urology. 2011 Jan 1;59(1):61-71.
- ↑ 14.0 14.1 Stafford RE, Ashton-Miller JA, Constantinou CE, Hodges PW. Novel insight into the dynamics of male pelvic floor contractions through transperineal ultrasound imaging. The Journal of urology. 2012 Oct;188(4):1224-30.
- ↑ Nahon I, Waddington G, Adams R, Dorey G. Assessing muscle function of the male pelvic floor using real time ultrasound. Neurourology and urodynamics. 2011 Sep;30(7):1329-32.
- ↑ 16.0 16.1 Milios JE. Therapeutic interventions for patients with prostate cancer undergoing radical prostatectomy: A focus on urinary incontinence, erectile dysfunction and Peyronie’s disease. Thesis Document University of Western Australia. 2019
- ↑ Stafford RE, Coughlin G, Lutton NJ, Hodges PW. Validity of estimation of pelvic floor muscle activity from transperineal ultrasound imaging in men. PLoS One. 2015;10(12).
- ↑ YoutTube. Real Time Ultrasound Rehabilitation of the Pelvic Floor. Available from: https://www.youtube.com/watch?v=122YOTqA5as&t=38s [last accessed 03/04/2022]
- ↑ Romero FR, Romero KR, Brenny Filho T, Pilati R, Kulysz D, de Oliveira Júnior FC. Reasons why patients reject digital rectal examination when screening for prostate cancer. Archivos espanoles de urologia. 2008;61(6):759-65.
- ↑ Frawley HC, Galea MP, Phillips BA, Sherburn M, Bø K. Reliability of pelvic floor muscle strength assessment using different test positions and tools. Neurourology and Urodynamics: Official Journal of the International Continence Society. 2006;25(3):236-42.
- ↑ Nahon I, Waddington G, Adams R, Dorey G. Assessing muscle function of the male pelvic floor using real time ultrasound. Neurourology and urodynamics. 2011 Sep;30(7):1329-32.
- ↑ JA VH, Abdussalam A, Kasi A. Rectal Exam. 07 Feb 2019
- ↑ Milios JE, Atkinson CL, Naylor LH, Millar D, Thijssen DH, Ackland TR, Green DJ. Pelvic floor muscle assessment in men post prostatectomy: comparing digital rectal examination and real-time ultrasound approaches. Australian and New Zealand Continence Journal, The. 2018 Dec;24(4):105-11.