Patellar Tendinopathy: Difference between revisions
No edit summary |
Kim Jackson (talk | contribs) No edit summary |
||
| (242 intermediate revisions by 28 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox"> | |||
'''Original Editors '''- [[User:Dorien De Ganck|Dorien De Ganck]] | '''Original Editors '''- [[User:Dorien De Ganck|Dorien De Ganck]] | ||
''' | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | ||
</div> | |||
== Description == | |||
Patellar [http://www.physio-pedia.com/Tendinopathy tendinopathy] is a source of anterior knee pain, characterised by pain localised to the inferior pole of the patella.<ref>Aicale R, Oliviero A, Maffulli N. [https://jfootankleres.biomedcentral.com/articles/10.1186/s13047-020-00418-8 Management of Achilles and patellar tendinopathy: what we know, what we can do.] Journal of Foot and Ankle Research. 2020 Dec;13(1):1-0.</ref> Pain is aggravated by loading and increased with the demand on the knee extensor musculature, notably in activities that store and release energy in the patellar tendon<ref name="malli">Malliaras P, Cook J, Purdam C, Rio E. Patellar Tendinopathy: [https://mtitx.com/wp-content/uploads/2016/05/Journal-of-orthopaedic-and-Sports-Physical-Therapy-2015-Malliaras.pdf Clinical Diagnosis, Load Management, and Advice for Challenging Case Presentations. The Journal of orthopaedic and sports physical therapy.] 2015 Sep:1-33. (level of evidence: 2a)</ref><ref>Breda SJ, Oei EH, Zwerver J, Visser E, Waarsing E, Krestin GP, de Vos RJ. [https://bjsm.bmj.com/content/55/9/501 Effectiveness of progressive tendon-loading exercise therapy in patients with patellar tendinopathy: a randomised clinical trial]. British journal of sports medicine. 2021 May 1;55(9):501-9.</ref>. | |||
Patellar tendinopathy is primarily a condition of relatively young (15-30 years old) athletes, especially men, who participate in sports such as basketball, volleyball, athletic jump events, tennis, and football, which require repetitive loading of the patellar tendon<ref>Lian ØB, Engebretsen L, Bahr R. [https://core.ac.uk/download/pdf/148237042.pdf Prevalence of jumper’s knee among elite athletes from different sports a cross-sectional study.] The American journal of sports medicine. 2005 Apr 1;33(4):561-7. level of evidence 4</ref>. The prevalence of this condition in elite volleyball and basketball players has been found to be over 40 percent.<ref>Maffulli N, Oliva F, Loppini M, Aicale R, Spiezia F, King JB. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5725181/ The Royal London Hospital Test for the clinical diagnosis of patellar tendinopathy.] ''Muscles Ligaments Tendons J''. 2017;7(2):315-22. </ref> While certain intrinsic risk factors for patellar tendinopathy have been identified, such as gender, weight and body mass index, the most significant risk factor appears to be training load (i.e. an extrinsic risk factor).<ref>Maciel Rabello L, Zwerver J, Stewart RE, van den Akker-Scheek I, Brink MS. [https://www.researchgate.net/publication/332205199_Patellar_tendon_structure_responds_to_load_over_a_7-week_preseason_in_elite_male_volleyball_players Patellar tendon structure responds to load over a 7-week preseason in elite male volleyball players.] Scand J Med Sci Sports. 2019;29(7):992-9. </ref> | |||
== Clinically Relevant Anatomy == | |||
[[File:TendonCS.JPG|thumb|250x250px|Cross section of a tendon.<br>Collagen fibres make up the pale<br>pink background. The fine lines<br>separate fibre bundles. The black<br>dots are the tenocyte nuclei.<ref>Kumc.edu. (2017). ''JayDoc HistoWeb''. [online] Available at: <nowiki>http://www.kumc.edu/instruction/medicine/anatomy/histoweb/</nowiki> [Accessed 16 Sep. 2017].</ref> | |||
]] | |||
The quadriceps muscles are connected to the inferior pole of the patella by the common quadriceps tendon through a sesmoid bone, the patella. The patellar ligament then connects the bottom of the patella to the tibial tuberosity. The force generated from the quadriceps muscles acts through the patellar as a pulley, causing the knee to extend<ref>Palastanga N, Field D, Soames R. Anatomy and human movement: structure and function. Elsevier Health Sciences; 2012.</ref> | |||
== | A healthy tendon is composed mostly of parallel collagen fibers closely packed together (86%)<ref>Lin TW, Cardenas L, Soslowsky LJ. [https://d1wqtxts1xzle7.cloudfront.net/47268775/j.jbiomech.2003.11.00520160715-26199-fyizgv-libre.pdf?1468590042=&response-content-disposition=inline%3B+filename%3DBiomechanics_of_tendon_injury_and_repair.pdf&Expires=1672494124&Signature=B9Y3wSSWJG6PuWxU80nB1UZhh0ZWvNcDEHoJZPD-LHjXDHqpBxQ37mL9Csal7ZroINKIsSzFsytyDiY6I~RWG4UJ8-OuT8IKtQtPJIEFT2rJ0a3quXOAI3b4d6NLJKUr6XRLy-zD4RUQhloZR7KsgxVgNIfnD~yMqj3jcen~gjP382nhyP2zc-FIz~u7qyDiYFl0-scFhlHnyqvckHak9cfQfhaE8llIbppLkZ95IqFuEKEQzwF8q9YmyuL6AURF7B6dWH~RZxRmxprZat-4SOojV3rqLOChhm67H5jt5ZRH5QoFXXjzpVC4NfTB5ZZOPhu2Wx~qCFkG66OkRdjwjA__&Key-Pair-Id=APKAJLOHF5GGSLRBV4ZA Biomechanics of tendon injury and repair.] Journal of biomechanics. 2004 Jun 1;37(6):865-77.</ref>. Collagen is predominantly type I. Other components of the tendon matrix are elastin (2%), proteoglycans (1–5%), and inorganic components (0.2%). The collagen in tendons are held together with proteoglycan components Decorin and Aggrecan, which bind to the collagen fibrils at specific locations<ref>Zhang G, Ezura Y, Chervoneva I, Robinson PS, Beason DP, Carine ET, Soslowsky LJ, Iozzo RV, Birk DE. [https://d1wqtxts1xzle7.cloudfront.net/43121506/Decorin_regulates_assembly_of_collagen_f20160226-5377-xenpez-libre.pdf?1456554438=&response-content-disposition=inline%3B+filename%3DDecorin_regulates_assembly_of_collagen_f.pdf&Expires=1672494177&Signature=Qs3oi49qeeRkSTFxAktqBKpCeBnfNcdCaoOcjua9dKbNV94csKmABG9TRYqD4oWT3njU7~P6pfWx-2oXIIZEPHpBuUYgMWjLzRL8PA7UW7t405moRcApxqcGVqZADiJ~I2fZWngtC5OHARyeuq58qTSTZ30ZyABycLc0NckY7Kfd3NaAoB~EAxxtAsB47d2CWOKWpB3g45SQpQ64UEAyQTO4CpyLVE3lwEYHGJV81Qjfbyf30ncs~PvsHG1stLp5Gs8Nu2nNwdmlfGrSlT-RM~FHfVVVFFY3AH1G7k0ZAozght~n3XpcsHIzMzWx2QG3X6YP91CMIlq3~YdkqJJhfQ__&Key-Pair-Id=APKAJLOHF5GGSLRBV4ZA Decorin regulates assembly of collagen fibrils and acquisition of biomechanical properties during tendon development.] Journal of cellular biochemistry. 2006 Aug 15;98(6):1436-49.</ref> | ||
Tenocytes are a tendon specific fibroblast type cells that produce the collagen molecules, which cluster together to form collagen fibrils. Fibril bundles are organized to form fibres with the elongated tenocytes closely packed between them. The cells communicate with each other through gap junctions, and this signalling gives them the ability to detect and respond to mechanical load<ref>McNeilly CM, Banes AJ, Benjamin M, Ralphs JR. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1167702/pdf/janat00125-0113.pdf Tendon cells in vivo form a three dimensional network of cell processes linked by gap junctions]. Journal of anatomy. 1996 Dec;189(Pt 3):593</ref>. | |||
Blood vessels run parallel to collagen fibres within the tendon with some branching transverse anastomoses. There is thought to be no nerve supply to the internal tendon but adjacent to the tendon are nerve endings and Golgi tendon organs are present at the junction between tendon and muscle. | |||
& | == Pathological Process == | ||
Cook &Purdam described a continuum model of tendon pathology with three distinct stages<ref name=":0">Cook JL, Purdam CR. [https://clinicalphysiosolutions.com.au/wp-content/uploads/2020/08/article7.pdf Is tendon pathology a continuum? A pathology model to explain the clinical presentation of load-induced tendinopathy.] British journal of sports medicine. 2009 Jun 1;43(6):409-16.</ref>: | |||
#Reactive tendinopathy | |||
#Tendon disrepair | |||
#Degenerative tendinopathy | |||
Load is considered to be the primary stimulus which drives tendon health forward and back along the continuum. | |||
=== Reactive tendinopathy === | |||
A non-inflammatory proliferative response in the cell and matrix, occurs with acute tensile or compressive overload. Tenocytes proliferate and protein production increases in this stage.<ref>Knapik JJ, Pope R. Achilles Tendinopathy: Pathophysiology, Epidemiology, Diagnosis, Treatment, Prevention, and Screening. J Spec Oper Med. 2020 Spring;20(1):125-40. </ref> This causes a short-term adaptation to the tendon and thickening of a portion of the tendon that either allows adaptation to compression or reduces stress by increasing cross-sectional area.<ref name=":0" /> This is different from the normal tendon response to load, which generally occurs through tendon stiffening.<ref name=":0" /> Clinically, reactive tendinopathies occur with unaccustomed physical activity or acute overload and also after a direct blow (e.g. a direct fall onto the patellar tendon).<ref name=":0" /> | |||
== | === Tendon disrepair === | ||
The continued attempt of tendon healing following the reactive stage but with greater matrix breakdown. There is an increase in the number of cells present in the matrix, resulting in an increase in protein production (proteoglycan and collagen). The proteoglycan increase causes collagen separation and matrix disorganisation.<ref name=":0" /> An increase in vascularity and neuronal ingrowth may also be present.<ref name=":0" /> Clinically, this stage of the pathology is seen in chronically overloaded tendons and appears across a spectrum of ages and loading environments.<ref name=":0" /> | |||
=== Degenerative tendinopathy === | |||
Degenerative tendinopathy is characterised by areas of cell death due to apoptosis, tenocyte exhaustion or exhaustion.<ref name=":0" /> There are large areas of the matrix that are disordered and filled with matrix breakdown products, little collagen and vessels.<ref name=":0" /> There is little room for the pathological changes to be reversed at this stage.<ref name=":0" /> This stage is primarily seen in the older person. | |||
== | == Clinical Presentation == | ||
Patellar tendinopathy, is one of many potential diagnoses for a patient presenting with anterior knee pain. There is considered to be two defining clinical features<ref name="malli" />: | |||
#Pain localized to the inferior pole of the patella | |||
#Load-related pain that increases with the demand on the knee extensors, notably in activities that store and release energy in the patellar tendon. | |||
The patient may complain of pain with prolonged sitting, squatting, and stairs, but these complaints are features of other pathologies such as [[Patellofemoral Pain Syndrome|patellofemoral pain]]. Pain is rarely experienced in a resting state. Pain occurs instantly with loading and usually ceases almost immediately when the load is removed. The pain may improve with repeated loading. An important feature of tendinopathies is that they are dose-dependent, pain increases as the magnitude or rate of application of the load on the tendon increases<ref>Kountouris A, Cook J. Rehabilitation of Achilles and patellar tendinopathies. Best practice & research clinical rheumatology. 2007 Apr 1;21(2):295-316.</ref>.The practical application of this is in an examination of pain should increase when progressing from a shallow to a deeper squat, or from a smaller to a greater hop height. | |||
Aggravating activities are predominantly loading activities, such as walking down stairs or when performing a decline squat. | |||
== Diagnostic Procedures == | == Diagnostic Procedures == | ||
[[Image:JElanding.jpg|200px|thumb|Jumper's knee]] | |||
[[Knee Examination|Knee examination]] | |||
Dose-dependent pain, see previous section. Deficits in energy-storage activities can be assessed clinically by observing jumping and hopping. Stiff-knee vertical jump-landing strategy may be used by individuals with a past history of patellar tendinopathy<ref>Bisseling RW, Hof AL, Bredeweg SW, Zwerver J, Mulder T. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2465350/ Relationship between landing strategy and patellar tendinopathy in volleybal]l. British journal of sports medicine. 2007 Jul 1;41(7):e8-.</ref>. | |||
Examination of the complete lower extremity is necessary to identify relevant deficits at the hip, knee, and ankle/foot regions. Atrophy, reduced strength, malaligned foot posture, quadriceps and hamstring inflexibility, reduced ankle dorsiflexion have been associated with patellar tendinopathy and should also be assessed<ref name="malli" />. | |||
Patellar tendon imaging does not confirm patellar tendon pain, as pathology observed via ultrasound imaging may be present in asymptomatic individuals<ref>Malliaras P, Cook J, Ptasznik R, Thomas S. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2491992/ Prospective study of change in patellar tendon abnormality on imaging and pain over a volleyball season]. British journal of sports medicine. 2006 Mar 1;40(3):272-4.</ref>. | |||
== Outcome Measures == | |||
*VISA scale (Victorian Institute of Sport Assessment-patella<ref>Visentini PJ, Khan KM, Cook JL, Kiss ZS, Harcourt PR, Wark JD, [https://d1wqtxts1xzle7.cloudfront.net/41956780/The_VISA_score_An_index_of_severity_of_s20160203-21623-l7j6yg-libre.pdf?1454513717=&response-content-disposition=inline%3B+filename%3DThe_VISA_score_An_index_of_severity_of_s.pdf&Expires=1672494713&Signature=GSQD64v0J~mQv59-D-9tsxaXgm17hZzkNjcbtf5fF2Zwk8rc1k-ZMpkjmvKUrQCPIcGwGnraHk6mvCb8jPwEDWs0-gCzvfo9hXw301WCYdQkTzs0unCjPotxEIh7ms5Ob0Xae7PX1qZ3V~B25wD6CPpw-o0nW8nX6ek9oNRAyYDEhHrDmfUsp0scmsJ9pegTdHgnf2BkX~qOq08OhbqvJouGel-fdEPIq-ymHkFNbMOXNuJXLrYl1lrFMcwtL7dSnAqjFZQxFNqSKhWblMT3Y15c7Uj9CbJQqsEy-O9gTQOObPjMIGM6WEZxTuuKf5rSkN1aqV7uA4gDx6rdI8F6wQ__&Key-Pair-Id=APKAJLOHF5GGSLRBV4ZA Victorian Institute of Sport Tendon Study Group. The VISA score: an index of severity of symptoms in patients with jumper's knee (patellar tendinosis).] Journal of Science and Medicine in Sport. 1998 Jan 31;1(1):22-8.</ref>) | |||
== Medical Management == | |||
[[File:Drug.jpg|thumb]] | |||
=== Non-steroidal anti-inflammatory drugs === | |||
The use of non-steroidal anti-inflammatory drugs (NSAID’s) in the treatment of tendinopathy remains controversial both in the acute stage and in the chronic stage. NSAIDs have been reported to impede soft tissue healing. Although pain may be reduced, they have a negative effect on tendon repair<ref>Ferry ST, Dahners LE, Afshari HM, Weinhold PS. [https://d1wqtxts1xzle7.cloudfront.net/84932788/ferry-libre.pdf?1650946251=&response-content-disposition=inline%3B+filename%3DThe_Effects_of_Common_Anti_Inflammatory.pdf&Expires=1672494850&Signature=fJBhwbWdBrOKjEQWQSjORmgbWTrEGqPd71Cxh2RNg5E2FsJ97PB7hvLrP8tRY92wse19ovAdk82z2-0S7D9t0dv70EYCL~YBBoGPMyUWGR5imTbkpw-11rrxjW2yOWcM2244ibsUDTGCBmROhSH1ZwxYF7-EHzizB~tSUMcJyvl23IDKrTXpifQ8Zlw5njnwvfyg3lwHfzElUorz2s0xZ4hP~bwtxShN4A34gU1zrUPypNy~1qiAYTlIhtxlJf-qUaU4rqrf-3AfoGcHZg5YlDakbgQLUcZly60UaszYERSy7V0QPkngNtvy8BT8ngQRyubZLiiyM7BsgAj1WnlS9g__&Key-Pair-Id=APKAJLOHF5GGSLRBV4ZA The effects of common anti-inflammatory drugs on the healing rat patellar tendon]. The American journal of sports medicine. 2007 Aug 1;35(8):1326-33.</ref>. In reactive tendinopathy, this may be a preferred effect, as this may inhibit proteins responsible for tendon swelling<ref>Riley GP, Cox M, Harrall RL, Clements S, Hazleman BL. [https://ueaeprints.uea.ac.uk/id/eprint/30756/1/Riley_-_Journal_of_Hand_Surgery%2C_2001%2C_26B%2C_224-228.pdf Inhibition of tendon cell proliferation and matrix glycosaminoglycan synthesis by non-steroidal anti-inflammatory drugs in vitro.] Journal of Hand Surgery (British and European Volume). 2001 Jun 1;26(3):224-8.</ref>. | |||
== | === Corticosteroid injections === | ||
Corticosteroids are used to decrease pain but also decrease cell proliferation and protein production and therefore could be used in the reactive tendinopathies. Repeated peritendinous corticosteroid has been shown to reduce tendon diameter at 7 and 21 days after injection in tendons<ref>Fredberg U, Bolvig L, Pfeiffer‐Jensen M, Clemmensen D, Jakobsen BW, Stengaard‐Pedersen K. [https://www.researchgate.net/profile/Mogens-Pfeiffer-Jensen/publication/8543568_Ultrasonography_as_a_tool_for_diagnosis_guidance_of_local_steroid_injection_and_together_with_pressure_algometry_monitoring_of_the_treatment_of_athletes_with_chronic_jumper's_knee_and_Achilles_tendini/links/0912f512c4059b552b000000/Ultrasonography-as-a-tool-for-diagnosis-guidance-of-local-steroid-injection-and-together-with-pressure-algometry-monitoring-of-the-treatment-of-athletes-with-chronic-jumpers-knee-and-Achilles-tendi.pdf Ultrasonography as a tool for diagnosis, guidance of local steroid injection and, together with pressure algometry, monitoring of the treatment of athletes with chronic jumper's knee and Achilles tendinitis: a randomized, double‐blind, placebo‐controlled study.] Scandinavian journal of rheumatology. 2004 Mar 1;33(2):94-101.</ref>. | |||
=== Surgical treatment === | |||
Surgery for chronic painful tendons has produced varied outcomes, with 50–80% of athletes able to return to sport at their previous level<ref>Tallon C, Coleman BD, Khan KM, Maffulli N. Outcome of surgery for chronic Achilles tendinopathy a critical review. The American Journal of Sports Medicine. 2001 May 1;29(3):315-20.</ref>. Surgery in nonathletic people produced poorer results than in active people<ref>Maffulli N, Testa V, Capasso G, Oliva F, Sullo A, Benazzo F, Regine R, King JB. [https://www.researchgate.net/profile/Mogens-Pfeiffer-Jensen/publication/8543568_Ultrasonography_as_a_tool_for_diagnosis_guidance_of_local_steroid_injection_and_together_with_pressure_algometry_monitoring_of_the_treatment_of_athletes_with_chronic_jumper's_knee_and_Achilles_tendini/links/0912f512c4059b552b000000/Ultrasonography-as-a-tool-for-diagnosis-guidance-of-local-steroid-injection-and-together-with-pressure-algometry-monitoring-of-the-treatment-of-athletes-with-chronic-jumpers-knee-and-Achilles-tendi.pdf Surgery for chronic Achilles tendinopathy yields worse results in nonathletic patients.] Clinical Journal of Sport Medicine. 2006 Mar 1;16(2):123-8.</ref>. Surgery is considered a reasonable option in those who have failed all conservative interventions. | |||
== | == Physiotherapy Management == | ||
[[Image:Legextension.jpg|250px|thumb|]] | |||
Advice regarding selective rest should be provided to allow appropriate tendon healing following a period of acute overloading or unaccustomed exercise (level of evidence: 2a) <ref name="Simpson & Smith">Simpson M, Smith T. Quadriceps tendinopathy-a forgotten pathology for physiotherapists? A systematic review of the current evidence-base. Phys Ther Rev. 2011;16(6):455-61. (level of evidence: 2a)</ref> . There should be a focus on an early return to activities. | |||
Use of patellar strap and sports tape has short term effect on pain.<ref>Reinking MF. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5095939/ Current concepts in the treatment of patellar tendinopathy.] International journal of sports physical therapy. 2016 Dec;11(6):854. </ref> | |||
== | === Pain relief === | ||
Isometrics have been suggested as a possible analgesic exercise where isotonic exercises are not possible due to fatigue and high SIN. In a systematic review by Naugle et al. (level of evidence: 2a) <ref name="Naugle et al.">Naugle KM, Fillingim RB, Riley JL 3rd. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3578581/ A meta-analytic review of the hypoalgesic effects of exercise]. J Pain. 2012 Dec;13(12):1139-50. doi: 10.1016/j.jpain.2012.09.006. Epub 2012 Nov 8. PMID: 23141188; PMCID: PMC3578581.</ref> isometric exercise has been found to be superior to aerobic and resistance exercises at reducing pain. | |||
== | === Rehabilitation === | ||
Exercise is an important component of the management of patellar tendinopathy.<ref>van Rijn D, van den Akker-Scheek I, Steunebrink M, Diercks RL, Zwerver J, van der Worp H. Comparison of the Effect of 5 Different Treatment Options for Managing Patellar Tendinopathy: A Secondary Analysis. Clin J Sport Med. 2019;29(3):181-7. </ref> A variety of loading programs have been suggested for the treatment of patella tendinopathy with the main types being (level of evidence: 1a) <ref name="Malliaras et al.">Malliaras P, Barton CJ, Reeves ND, Langberg H. [https://physiovelo.com/wp-content/uploads/2016/12/loadingprogrammes.pdf Achilles and patellar tendinopathy loading programmes]. Sports medicine. 2013 Apr;43(4):267-86.</ref>: | |||
< | #Eccentric loading | ||
#Eccentric-concentric loading | |||
{| class="wikitable" | |||
! colspan="6" |Adapted from Malliaras et al. 2013 (level of evidence: 2a) <ref name="Malliaras et al." /> | |||
|- | |||
!Programme | |||
!Exercise type | |||
!Sets & reps | |||
!Frequency | |||
!Progression | |||
!Pain | |||
|- | |||
|Alfredson | |||
|Eccentric | |||
|3x15 | |||
|Twice daily | |||
|Load | |||
|Enough load to achieve with moderate pain | |||
|- | |||
|Stanish and Curwin/Silbernagel | |||
|Eccentric-concentric | |||
|3x10-20 | |||
|Daily | |||
|Speed then load, type of exercise | |||
|Enough load to be painful in third set | |||
|- | |||
|Heavy slow resistance training | |||
|Eccentric-concentric | |||
|4x6-15 | |||
|3x/week | |||
|6-15RM | |||
|Acceptable if was not worse after | |||
|} | |||
Eccentric loading has been the most dominant approach for rehabilitation. Evidence suggests that all loading programs are beneficial in reducing pain and returning function however the eccentric-concentric type has greater patient subjective satisfaction (level of evidence: 1a) <ref name="Malliaras et al." />. This is perhaps due to time commitment and pain required from eccentric programs. Eccentric-concentric exercises can begin with body weight squats but a significant load is important. Gym machines such as leg press or knee extension provides control to the amount of loading. If suitable for the patient a barbell squat or lunge can be an excellent progression. | |||
== | === Protocol === | ||
{| class="wikitable" | |||
! colspan="3" |Protocol as described by Malliaris et al. (2015) (level of evidence: 2a) <ref name="malli" /> | |||
|- | |||
!Stage | |||
!Indication | |||
!Dosage | |||
|- | |||
|1. Isometric loading | |||
|More than minimal pain during isometric exercise | |||
|5 repetitions of 45 seconds, 2 to 3 times per day; progress to 70% maximal voluntary contraction as pain allows | |||
|- | |||
|2. Isotonic loading | |||
|Minimal pain during isotonic exercise | |||
|3 to 4 sets at a load of 15RM, progressing to a load of 6RM, every second day; fatiguing load | |||
|- | |||
|3. Energy-storing loading | |||
|Adequate strength and consistent with other side and load tolerance with initial-level energy storage exercise (ie, minimal pain during exercise and pain on load tests returning to baseline within 24 hours) | |||
|Progressively develop volume and then intensity of relevant energy-storage exercise to replicate demands of sport | |||
|- | |||
|4. Return to sport | |||
|Load tolerance to energy-storage exercise progression that replicates demands of training | |||
|Progressively add training drills, then competition, when tolerant to full training | |||
|} | |||
Malliaris and colleagues report common management pitfalls, which are worth considering when planning treatment: | |||
*Unrealistic rehabilitation time frames | |||
*Inaccurate beliefs and expectations about pain | |||
*Failure to identify central sensitization | |||
*Over-reliance on passive treatments | |||
*Not addressing isolated muscle deficits | |||
*Failure to address kinetic-chain deficits | |||
*Not adequately addressing biomechanics | |||
=== Tendon neuroplastic training<ref>Rio E, Kidgell D, Moseley GL, Gaida J, Docking S, Purdam C, Cook J. [https://bjsm.bmj.com/content/50/4/209 Tendon neuroplastic training: changing the way we think about tendon rehabilitation: a narrative review]. Br J Sports Med. 2015 Sep 25:bjsports-2015. </ref> === | |||
Rio et al found that current rehabilitation uses self-paced strength training (for e.g. a patient does 3x10 contractions lifting a weight - without any external cues/advice on timing). This type of training may lead to recurrence of tendinopathy, as it does not address motor control sufficiently and thus does not change the corticospinal drive to the muscle. | |||
Externally paced training would be when the patient contract the muscle, concentrically and eccentrically on auditory (like using a metronome) or on visual cues. Externally paced strength training was shown to alter tendon pain and corticospinal control of the muscle. | |||
Tendon neuroplastic training uses strength-based training with external cues as a strategy to optimise neuroplasticity. This was shown effective with patellar tendinopathy and further research is required into other tendinopathies. | |||
=== Other forms of therapy === | |||
Alternative therapies like administering shockwaves were also investigated. It has been shown that shockwave therapy is a safe method for patients who are unresponsive to coventional therapy, and it should always be used in combination with other methods. (level of evidence:1a)<ref>Kertzman, P., Lenza, M., Pedrinelli, A., & Ejnisman, B.(2015). [https://reader.elsevier.com/reader/sd/pii/S225549711500004X?token=5B6931609096716A35167BA5AAA7D873F341E2BD5ECB3E5CB6E30B4E86111B9B9981EE087BBCEAE961BD89247B71A506&originRegion=eu-west-1&originCreation=20221231130553 Shockwave treatment for musculoskeletal diseases and bone consolidation: qualitative analysis of the literature]. Revista Brasileira de Ortopedia, 50(1), 3–8. </ref> Recording to F. Abat et al. USGET (Guided-Galvanic Electrolysis Technique) provides better results than shockwave therapy, but also combined with eccentric exercise therapy. (level of evidence: 1b)<ref>Abat, F., Sánchez-Sánchez, J. L., Martín-Nogueras, A. M., Calvo-Arenillas, J. I., Yajeya, J., Méndez-Sánchez, R., … Gelber, P. E. (2016). [https://jeo-esska.springeropen.com/articles/10.1186/s40634-016-0070-4 Randomized controlled trial comparing the effectiveness of the ultrasound- guided galvanic electrolysis technique (USGET) versus conventional electro- physiotherapeutic treatment on patellar tendinopathy.] ''Journal of Experimental Orthopaedics'', ''3'', 34.</ref> | |||
== | == Differential Diagnosis == | ||
*Infrapatellar bursitis | |||
*Fat pad impingement | |||
*[[Patellofemoral Pain Syndrome|Patellofemoral pain]] | |||
*[[Plica Syndrome|Plica injuries]] | |||
*[[Osgood-Schlatter Disease|Osgood-Schlatter syndrome]] | |||
*[[Sinding Larsen Johansson Syndrome|Sinding-Larsen-Johansson syndrome]] | |||
== | == Key Evidence == | ||
*Isometric exercise induces analgesia and reduces inhibition in patellar tendinopathy. (Rio 2015) (Level of evidence 1b) | |||
*Patellar Tendinopathy: Clinical Diagnosis, Load Management, and Advice for Challenging Case Presentations. (Malliaris 2015) (Level of evidence 1a) | |||
*Physiotherapy management of patellar tendinopathy (jumper's knee). (Rudavsky 2014) (Level of evidence 1a) | |||
*Achilles and patellar tendinopathy loading programmes. (Malliaris 2013) (Level of evidence 1a) | |||
*Abat, F. et al. “Randomized Controlled Trial Comparing the Effectiveness of the Ultrasound-Guided Galvanic Electrolysis Technique (USGET) versus Conventional Electro-Physiotherapeutic Treatment on Patellar Tendinopathy.” ''Journal of Experimental Orthopaedics'' 3 (2016): 34. ''PMC''. Web. 19 Dec. 2017. (Level of evidence 1b) | |||
== | == Resources == | ||
<div class="row"> | |||
<div class=" | <div class="col-md-6"> {{#ev:youtube|mik90mAS6fU|250}} <div class="text-right"><ref>The Knee Resource. Spanish Squats - Isometric Exercise for Patellar Tendinopathy. Available from: https://youtu.be/mik90mAS6fU [last accessed 01/03/2018]</ref></div></div> | ||
< | <div class="col-md-6"> {{#ev:youtube|g0XPFL1IwEc|250}} <div class="text-right"><ref>The Knee Resource. Patellar Tendinopathy Rehab - Isotonic Exercises. Available from: https://youtu.be/g0XPFL1IwEc [last accessed 01/03/2018]</ref></div></div> | ||
<div class="col-md-6"> {{#ev:youtube|ppBl9L-OlH4|250}} <div class="text-right"><ref>The Knee Resource. Patellar Tendinopathy Rehab - Energy Storage Exercises. Available from: https://youtu.be/ppBl9L-OlH4 [last accessed 01/03/2018]</ref></div></div> | |||
<div class="col-md-6"> {{#ev:youtube|t1blThXvLIk|250}} <div class="text-right"><ref>Patellar Tendinopathy Rehab - Kinetic Chain Strengthening Exercise. Available from: https://youtu.be/t1blThXvLIk [last accessed 01/03/2018]</ref></div></div> | |||
</div> | </div> | ||
== References | Click on [https://www.youtube.com/watch?v=5lj9Yq0ETr0&list=PLTHRWnWbCOmhpYOtdkoR2hTL3y4Ofvt69 Patellar Tendinopathy] YouTube Playlist for more videos | ||
== Case Studies == | |||
*[http://www.sportsinjurybulletin.com/archive/anterior-knee-pain.html High jumper] | |||
== References == | |||
<references /> | |||
[[Category:Knee - Conditions]] | |||
[[Category:Conditions]] | |||
[[Category:Knee]] | |||
[[Category:Tendons]] | |||
[[Category:Rehabilitation Protocols]] | |||
[[Category:Musculoskeletal/Orthopaedics|Musculoskeletal/Orthopaedics]] | |||
[[Category:Sports_Injuries]] | |||
[[Category:Sports Medicine]] | |||
[[Category:Tendinopathy]] | |||
Latest revision as of 14:10, 5 January 2023
Original Editors - Dorien De Ganck
Top Contributors - George Prudden, Admin, Mathieu Henrotte, Dorien De Ganck, Kim Jackson, Derycker Andries, Chelsy De Bruyn, Vanessa Rhule, Rachael Lowe, Yarne Leuckx, Wendy Walker, Evan Thomas, Jess Bell, WikiSysop, Simisola Ajeyalemi, Joris De Pot, Fee Waveryns, Alexandre Effinger, Wanda van Niekerk, Tarina van der Stockt, 127.0.0.1, Claire Knott, Scott Buxton, Oyemi Sillo, Wendy Snyders, Naomi O'Reilly, Robin Tacchetti, Wajeeha Hassan and Mariam Hashem
Description[edit | edit source]
Patellar tendinopathy is a source of anterior knee pain, characterised by pain localised to the inferior pole of the patella.[1] Pain is aggravated by loading and increased with the demand on the knee extensor musculature, notably in activities that store and release energy in the patellar tendon[2][3].
Patellar tendinopathy is primarily a condition of relatively young (15-30 years old) athletes, especially men, who participate in sports such as basketball, volleyball, athletic jump events, tennis, and football, which require repetitive loading of the patellar tendon[4]. The prevalence of this condition in elite volleyball and basketball players has been found to be over 40 percent.[5] While certain intrinsic risk factors for patellar tendinopathy have been identified, such as gender, weight and body mass index, the most significant risk factor appears to be training load (i.e. an extrinsic risk factor).[6]
Clinically Relevant Anatomy[edit | edit source]
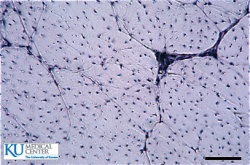
Collagen fibres make up the pale
pink background. The fine lines
separate fibre bundles. The black
dots are the tenocyte nuclei.[7]
The quadriceps muscles are connected to the inferior pole of the patella by the common quadriceps tendon through a sesmoid bone, the patella. The patellar ligament then connects the bottom of the patella to the tibial tuberosity. The force generated from the quadriceps muscles acts through the patellar as a pulley, causing the knee to extend[8]
A healthy tendon is composed mostly of parallel collagen fibers closely packed together (86%)[9]. Collagen is predominantly type I. Other components of the tendon matrix are elastin (2%), proteoglycans (1–5%), and inorganic components (0.2%). The collagen in tendons are held together with proteoglycan components Decorin and Aggrecan, which bind to the collagen fibrils at specific locations[10]
Tenocytes are a tendon specific fibroblast type cells that produce the collagen molecules, which cluster together to form collagen fibrils. Fibril bundles are organized to form fibres with the elongated tenocytes closely packed between them. The cells communicate with each other through gap junctions, and this signalling gives them the ability to detect and respond to mechanical load[11].
Blood vessels run parallel to collagen fibres within the tendon with some branching transverse anastomoses. There is thought to be no nerve supply to the internal tendon but adjacent to the tendon are nerve endings and Golgi tendon organs are present at the junction between tendon and muscle.
Pathological Process[edit | edit source]
Cook &Purdam described a continuum model of tendon pathology with three distinct stages[12]:
- Reactive tendinopathy
- Tendon disrepair
- Degenerative tendinopathy
Load is considered to be the primary stimulus which drives tendon health forward and back along the continuum.
Reactive tendinopathy[edit | edit source]
A non-inflammatory proliferative response in the cell and matrix, occurs with acute tensile or compressive overload. Tenocytes proliferate and protein production increases in this stage.[13] This causes a short-term adaptation to the tendon and thickening of a portion of the tendon that either allows adaptation to compression or reduces stress by increasing cross-sectional area.[12] This is different from the normal tendon response to load, which generally occurs through tendon stiffening.[12] Clinically, reactive tendinopathies occur with unaccustomed physical activity or acute overload and also after a direct blow (e.g. a direct fall onto the patellar tendon).[12]
Tendon disrepair[edit | edit source]
The continued attempt of tendon healing following the reactive stage but with greater matrix breakdown. There is an increase in the number of cells present in the matrix, resulting in an increase in protein production (proteoglycan and collagen). The proteoglycan increase causes collagen separation and matrix disorganisation.[12] An increase in vascularity and neuronal ingrowth may also be present.[12] Clinically, this stage of the pathology is seen in chronically overloaded tendons and appears across a spectrum of ages and loading environments.[12]
Degenerative tendinopathy[edit | edit source]
Degenerative tendinopathy is characterised by areas of cell death due to apoptosis, tenocyte exhaustion or exhaustion.[12] There are large areas of the matrix that are disordered and filled with matrix breakdown products, little collagen and vessels.[12] There is little room for the pathological changes to be reversed at this stage.[12] This stage is primarily seen in the older person.
Clinical Presentation[edit | edit source]
Patellar tendinopathy, is one of many potential diagnoses for a patient presenting with anterior knee pain. There is considered to be two defining clinical features[2]:
- Pain localized to the inferior pole of the patella
- Load-related pain that increases with the demand on the knee extensors, notably in activities that store and release energy in the patellar tendon.
The patient may complain of pain with prolonged sitting, squatting, and stairs, but these complaints are features of other pathologies such as patellofemoral pain. Pain is rarely experienced in a resting state. Pain occurs instantly with loading and usually ceases almost immediately when the load is removed. The pain may improve with repeated loading. An important feature of tendinopathies is that they are dose-dependent, pain increases as the magnitude or rate of application of the load on the tendon increases[14].The practical application of this is in an examination of pain should increase when progressing from a shallow to a deeper squat, or from a smaller to a greater hop height.
Aggravating activities are predominantly loading activities, such as walking down stairs or when performing a decline squat.
Diagnostic Procedures[edit | edit source]
Dose-dependent pain, see previous section. Deficits in energy-storage activities can be assessed clinically by observing jumping and hopping. Stiff-knee vertical jump-landing strategy may be used by individuals with a past history of patellar tendinopathy[15].
Examination of the complete lower extremity is necessary to identify relevant deficits at the hip, knee, and ankle/foot regions. Atrophy, reduced strength, malaligned foot posture, quadriceps and hamstring inflexibility, reduced ankle dorsiflexion have been associated with patellar tendinopathy and should also be assessed[2].
Patellar tendon imaging does not confirm patellar tendon pain, as pathology observed via ultrasound imaging may be present in asymptomatic individuals[16].
Outcome Measures[edit | edit source]
- VISA scale (Victorian Institute of Sport Assessment-patella[17])
Medical Management[edit | edit source]
Non-steroidal anti-inflammatory drugs[edit | edit source]
The use of non-steroidal anti-inflammatory drugs (NSAID’s) in the treatment of tendinopathy remains controversial both in the acute stage and in the chronic stage. NSAIDs have been reported to impede soft tissue healing. Although pain may be reduced, they have a negative effect on tendon repair[18]. In reactive tendinopathy, this may be a preferred effect, as this may inhibit proteins responsible for tendon swelling[19].
Corticosteroid injections[edit | edit source]
Corticosteroids are used to decrease pain but also decrease cell proliferation and protein production and therefore could be used in the reactive tendinopathies. Repeated peritendinous corticosteroid has been shown to reduce tendon diameter at 7 and 21 days after injection in tendons[20].
Surgical treatment[edit | edit source]
Surgery for chronic painful tendons has produced varied outcomes, with 50–80% of athletes able to return to sport at their previous level[21]. Surgery in nonathletic people produced poorer results than in active people[22]. Surgery is considered a reasonable option in those who have failed all conservative interventions.
Physiotherapy Management[edit | edit source]
Advice regarding selective rest should be provided to allow appropriate tendon healing following a period of acute overloading or unaccustomed exercise (level of evidence: 2a) [23] . There should be a focus on an early return to activities.
Use of patellar strap and sports tape has short term effect on pain.[24]
Pain relief[edit | edit source]
Isometrics have been suggested as a possible analgesic exercise where isotonic exercises are not possible due to fatigue and high SIN. In a systematic review by Naugle et al. (level of evidence: 2a) [25] isometric exercise has been found to be superior to aerobic and resistance exercises at reducing pain.
Rehabilitation[edit | edit source]
Exercise is an important component of the management of patellar tendinopathy.[26] A variety of loading programs have been suggested for the treatment of patella tendinopathy with the main types being (level of evidence: 1a) [27]:
- Eccentric loading
- Eccentric-concentric loading
| Adapted from Malliaras et al. 2013 (level of evidence: 2a) [27] | |||||
|---|---|---|---|---|---|
| Programme | Exercise type | Sets & reps | Frequency | Progression | Pain |
| Alfredson | Eccentric | 3x15 | Twice daily | Load | Enough load to achieve with moderate pain |
| Stanish and Curwin/Silbernagel | Eccentric-concentric | 3x10-20 | Daily | Speed then load, type of exercise | Enough load to be painful in third set |
| Heavy slow resistance training | Eccentric-concentric | 4x6-15 | 3x/week | 6-15RM | Acceptable if was not worse after |
Eccentric loading has been the most dominant approach for rehabilitation. Evidence suggests that all loading programs are beneficial in reducing pain and returning function however the eccentric-concentric type has greater patient subjective satisfaction (level of evidence: 1a) [27]. This is perhaps due to time commitment and pain required from eccentric programs. Eccentric-concentric exercises can begin with body weight squats but a significant load is important. Gym machines such as leg press or knee extension provides control to the amount of loading. If suitable for the patient a barbell squat or lunge can be an excellent progression.
Protocol[edit | edit source]
| Protocol as described by Malliaris et al. (2015) (level of evidence: 2a) [2] | ||
|---|---|---|
| Stage | Indication | Dosage |
| 1. Isometric loading | More than minimal pain during isometric exercise | 5 repetitions of 45 seconds, 2 to 3 times per day; progress to 70% maximal voluntary contraction as pain allows |
| 2. Isotonic loading | Minimal pain during isotonic exercise | 3 to 4 sets at a load of 15RM, progressing to a load of 6RM, every second day; fatiguing load |
| 3. Energy-storing loading | Adequate strength and consistent with other side and load tolerance with initial-level energy storage exercise (ie, minimal pain during exercise and pain on load tests returning to baseline within 24 hours) | Progressively develop volume and then intensity of relevant energy-storage exercise to replicate demands of sport |
| 4. Return to sport | Load tolerance to energy-storage exercise progression that replicates demands of training | Progressively add training drills, then competition, when tolerant to full training |
Malliaris and colleagues report common management pitfalls, which are worth considering when planning treatment:
- Unrealistic rehabilitation time frames
- Inaccurate beliefs and expectations about pain
- Failure to identify central sensitization
- Over-reliance on passive treatments
- Not addressing isolated muscle deficits
- Failure to address kinetic-chain deficits
- Not adequately addressing biomechanics
Tendon neuroplastic training[28][edit | edit source]
Rio et al found that current rehabilitation uses self-paced strength training (for e.g. a patient does 3x10 contractions lifting a weight - without any external cues/advice on timing). This type of training may lead to recurrence of tendinopathy, as it does not address motor control sufficiently and thus does not change the corticospinal drive to the muscle.
Externally paced training would be when the patient contract the muscle, concentrically and eccentrically on auditory (like using a metronome) or on visual cues. Externally paced strength training was shown to alter tendon pain and corticospinal control of the muscle.
Tendon neuroplastic training uses strength-based training with external cues as a strategy to optimise neuroplasticity. This was shown effective with patellar tendinopathy and further research is required into other tendinopathies.
Other forms of therapy[edit | edit source]
Alternative therapies like administering shockwaves were also investigated. It has been shown that shockwave therapy is a safe method for patients who are unresponsive to coventional therapy, and it should always be used in combination with other methods. (level of evidence:1a)[29] Recording to F. Abat et al. USGET (Guided-Galvanic Electrolysis Technique) provides better results than shockwave therapy, but also combined with eccentric exercise therapy. (level of evidence: 1b)[30]
Differential Diagnosis[edit | edit source]
- Infrapatellar bursitis
- Fat pad impingement
- Patellofemoral pain
- Plica injuries
- Osgood-Schlatter syndrome
- Sinding-Larsen-Johansson syndrome
Key Evidence[edit | edit source]
- Isometric exercise induces analgesia and reduces inhibition in patellar tendinopathy. (Rio 2015) (Level of evidence 1b)
- Patellar Tendinopathy: Clinical Diagnosis, Load Management, and Advice for Challenging Case Presentations. (Malliaris 2015) (Level of evidence 1a)
- Physiotherapy management of patellar tendinopathy (jumper's knee). (Rudavsky 2014) (Level of evidence 1a)
- Achilles and patellar tendinopathy loading programmes. (Malliaris 2013) (Level of evidence 1a)
- Abat, F. et al. “Randomized Controlled Trial Comparing the Effectiveness of the Ultrasound-Guided Galvanic Electrolysis Technique (USGET) versus Conventional Electro-Physiotherapeutic Treatment on Patellar Tendinopathy.” Journal of Experimental Orthopaedics 3 (2016): 34. PMC. Web. 19 Dec. 2017. (Level of evidence 1b)
Resources[edit | edit source]
Click on Patellar Tendinopathy YouTube Playlist for more videos
Case Studies[edit | edit source]
References[edit | edit source]
- ↑ Aicale R, Oliviero A, Maffulli N. Management of Achilles and patellar tendinopathy: what we know, what we can do. Journal of Foot and Ankle Research. 2020 Dec;13(1):1-0.
- ↑ 2.0 2.1 2.2 2.3 Malliaras P, Cook J, Purdam C, Rio E. Patellar Tendinopathy: Clinical Diagnosis, Load Management, and Advice for Challenging Case Presentations. The Journal of orthopaedic and sports physical therapy. 2015 Sep:1-33. (level of evidence: 2a)
- ↑ Breda SJ, Oei EH, Zwerver J, Visser E, Waarsing E, Krestin GP, de Vos RJ. Effectiveness of progressive tendon-loading exercise therapy in patients with patellar tendinopathy: a randomised clinical trial. British journal of sports medicine. 2021 May 1;55(9):501-9.
- ↑ Lian ØB, Engebretsen L, Bahr R. Prevalence of jumper’s knee among elite athletes from different sports a cross-sectional study. The American journal of sports medicine. 2005 Apr 1;33(4):561-7. level of evidence 4
- ↑ Maffulli N, Oliva F, Loppini M, Aicale R, Spiezia F, King JB. The Royal London Hospital Test for the clinical diagnosis of patellar tendinopathy. Muscles Ligaments Tendons J. 2017;7(2):315-22.
- ↑ Maciel Rabello L, Zwerver J, Stewart RE, van den Akker-Scheek I, Brink MS. Patellar tendon structure responds to load over a 7-week preseason in elite male volleyball players. Scand J Med Sci Sports. 2019;29(7):992-9.
- ↑ Kumc.edu. (2017). JayDoc HistoWeb. [online] Available at: http://www.kumc.edu/instruction/medicine/anatomy/histoweb/ [Accessed 16 Sep. 2017].
- ↑ Palastanga N, Field D, Soames R. Anatomy and human movement: structure and function. Elsevier Health Sciences; 2012.
- ↑ Lin TW, Cardenas L, Soslowsky LJ. Biomechanics of tendon injury and repair. Journal of biomechanics. 2004 Jun 1;37(6):865-77.
- ↑ Zhang G, Ezura Y, Chervoneva I, Robinson PS, Beason DP, Carine ET, Soslowsky LJ, Iozzo RV, Birk DE. Decorin regulates assembly of collagen fibrils and acquisition of biomechanical properties during tendon development. Journal of cellular biochemistry. 2006 Aug 15;98(6):1436-49.
- ↑ McNeilly CM, Banes AJ, Benjamin M, Ralphs JR. Tendon cells in vivo form a three dimensional network of cell processes linked by gap junctions. Journal of anatomy. 1996 Dec;189(Pt 3):593
- ↑ 12.0 12.1 12.2 12.3 12.4 12.5 12.6 12.7 12.8 12.9 Cook JL, Purdam CR. Is tendon pathology a continuum? A pathology model to explain the clinical presentation of load-induced tendinopathy. British journal of sports medicine. 2009 Jun 1;43(6):409-16.
- ↑ Knapik JJ, Pope R. Achilles Tendinopathy: Pathophysiology, Epidemiology, Diagnosis, Treatment, Prevention, and Screening. J Spec Oper Med. 2020 Spring;20(1):125-40.
- ↑ Kountouris A, Cook J. Rehabilitation of Achilles and patellar tendinopathies. Best practice & research clinical rheumatology. 2007 Apr 1;21(2):295-316.
- ↑ Bisseling RW, Hof AL, Bredeweg SW, Zwerver J, Mulder T. Relationship between landing strategy and patellar tendinopathy in volleyball. British journal of sports medicine. 2007 Jul 1;41(7):e8-.
- ↑ Malliaras P, Cook J, Ptasznik R, Thomas S. Prospective study of change in patellar tendon abnormality on imaging and pain over a volleyball season. British journal of sports medicine. 2006 Mar 1;40(3):272-4.
- ↑ Visentini PJ, Khan KM, Cook JL, Kiss ZS, Harcourt PR, Wark JD, Victorian Institute of Sport Tendon Study Group. The VISA score: an index of severity of symptoms in patients with jumper's knee (patellar tendinosis). Journal of Science and Medicine in Sport. 1998 Jan 31;1(1):22-8.
- ↑ Ferry ST, Dahners LE, Afshari HM, Weinhold PS. The effects of common anti-inflammatory drugs on the healing rat patellar tendon. The American journal of sports medicine. 2007 Aug 1;35(8):1326-33.
- ↑ Riley GP, Cox M, Harrall RL, Clements S, Hazleman BL. Inhibition of tendon cell proliferation and matrix glycosaminoglycan synthesis by non-steroidal anti-inflammatory drugs in vitro. Journal of Hand Surgery (British and European Volume). 2001 Jun 1;26(3):224-8.
- ↑ Fredberg U, Bolvig L, Pfeiffer‐Jensen M, Clemmensen D, Jakobsen BW, Stengaard‐Pedersen K. Ultrasonography as a tool for diagnosis, guidance of local steroid injection and, together with pressure algometry, monitoring of the treatment of athletes with chronic jumper's knee and Achilles tendinitis: a randomized, double‐blind, placebo‐controlled study. Scandinavian journal of rheumatology. 2004 Mar 1;33(2):94-101.
- ↑ Tallon C, Coleman BD, Khan KM, Maffulli N. Outcome of surgery for chronic Achilles tendinopathy a critical review. The American Journal of Sports Medicine. 2001 May 1;29(3):315-20.
- ↑ Maffulli N, Testa V, Capasso G, Oliva F, Sullo A, Benazzo F, Regine R, King JB. Surgery for chronic Achilles tendinopathy yields worse results in nonathletic patients. Clinical Journal of Sport Medicine. 2006 Mar 1;16(2):123-8.
- ↑ Simpson M, Smith T. Quadriceps tendinopathy-a forgotten pathology for physiotherapists? A systematic review of the current evidence-base. Phys Ther Rev. 2011;16(6):455-61. (level of evidence: 2a)
- ↑ Reinking MF. Current concepts in the treatment of patellar tendinopathy. International journal of sports physical therapy. 2016 Dec;11(6):854.
- ↑ Naugle KM, Fillingim RB, Riley JL 3rd. A meta-analytic review of the hypoalgesic effects of exercise. J Pain. 2012 Dec;13(12):1139-50. doi: 10.1016/j.jpain.2012.09.006. Epub 2012 Nov 8. PMID: 23141188; PMCID: PMC3578581.
- ↑ van Rijn D, van den Akker-Scheek I, Steunebrink M, Diercks RL, Zwerver J, van der Worp H. Comparison of the Effect of 5 Different Treatment Options for Managing Patellar Tendinopathy: A Secondary Analysis. Clin J Sport Med. 2019;29(3):181-7.
- ↑ 27.0 27.1 27.2 Malliaras P, Barton CJ, Reeves ND, Langberg H. Achilles and patellar tendinopathy loading programmes. Sports medicine. 2013 Apr;43(4):267-86.
- ↑ Rio E, Kidgell D, Moseley GL, Gaida J, Docking S, Purdam C, Cook J. Tendon neuroplastic training: changing the way we think about tendon rehabilitation: a narrative review. Br J Sports Med. 2015 Sep 25:bjsports-2015.
- ↑ Kertzman, P., Lenza, M., Pedrinelli, A., & Ejnisman, B.(2015). Shockwave treatment for musculoskeletal diseases and bone consolidation: qualitative analysis of the literature. Revista Brasileira de Ortopedia, 50(1), 3–8.
- ↑ Abat, F., Sánchez-Sánchez, J. L., Martín-Nogueras, A. M., Calvo-Arenillas, J. I., Yajeya, J., Méndez-Sánchez, R., … Gelber, P. E. (2016). Randomized controlled trial comparing the effectiveness of the ultrasound- guided galvanic electrolysis technique (USGET) versus conventional electro- physiotherapeutic treatment on patellar tendinopathy. Journal of Experimental Orthopaedics, 3, 34.
- ↑ The Knee Resource. Spanish Squats - Isometric Exercise for Patellar Tendinopathy. Available from: https://youtu.be/mik90mAS6fU [last accessed 01/03/2018]
- ↑ The Knee Resource. Patellar Tendinopathy Rehab - Isotonic Exercises. Available from: https://youtu.be/g0XPFL1IwEc [last accessed 01/03/2018]
- ↑ The Knee Resource. Patellar Tendinopathy Rehab - Energy Storage Exercises. Available from: https://youtu.be/ppBl9L-OlH4 [last accessed 01/03/2018]
- ↑ Patellar Tendinopathy Rehab - Kinetic Chain Strengthening Exercise. Available from: https://youtu.be/t1blThXvLIk [last accessed 01/03/2018]









