ACL Rehabilitation: Re-injury and Return to Sport Tests: Difference between revisions
No edit summary |
No edit summary |
||
| Line 83: | Line 83: | ||
| [[File:Wall squat with stability ball.jpg]] | | [[File:Wall squat with stability ball.jpg]] | ||
|} | |} | ||
Each athlete will need individualized variations according to individual characteristics and sport. | Each athlete will need individualized variations according to individual characteristics and sport. | ||
Exercise intensity should be changed constantly to challenge balance and proprioception. Modifications of body posture, switching between various unstable surfaces, speed modifications, adding a sport-specific skill and/or adding unanticipated movement can all be ways of challenging stability and balance. | |||
Exercise intensity should be changed constantly to challenge | |||
=== Stage II: Functional strengthening === | === Stage II: Functional strengthening === | ||
| Line 118: | Line 117: | ||
Examples of exercises to be used in this stage: | Examples of exercises to be used in this stage: | ||
{| class="wikitable" width="100%" cellspacing="6" cellpadding="0" border="0" | |||
|- | |||
| [[File:Single leg X hop.jpg]] | |||
| [[File:Barbell back squat.gif]] | |||
|- | |||
| [[File:Nordic hamstring curls.gif]] | |||
| [[File:Lateral crunches.jpg]] | |||
|- | |||
| [[File:Forward and backward jump.gif]] | |||
| [[File:Swiss ball back extension.gif]] | |||
|} | |||
=== Stage IV: Sport Performance Symmetry === | === Stage IV: Sport Performance Symmetry === | ||
| Line 128: | Line 137: | ||
Examples of exercises to be used in this stage: | Examples of exercises to be used in this stage: | ||
{| class="wikitable" width="100%" cellspacing="6" cellpadding="0" border="0" | |||
|- | |||
| [[File:Lunge jump.jpg]] | |||
| {{#ev:youtube|zh1v8jINBZ0}}<ref>Tuck Jump. Available from: https://www.youtube.com/watch?v=zh1v8jINBZ0</ref> | |||
|- | |||
| {{#ev:youtube|KDwzB6xuZ9o}}<ref>TFW Explosive Box Step Up. Available from:https://www.youtube.com/watch?v=KDwzB6xuZ9o </ref> | |||
| {{#ev:youtube|5EztcmA0Amc}}<ref>Depth jump to box jump - Increase vertical jump - Volleyball. Available from: https://www.youtube.com/watch?v=5EztcmA0Amc</ref> | |||
|- | |||
| {{#ev:youtube|HwPCpzLmSYQ}}<ref>Four Corner Drill. Available from: https://www.youtube.com/watch?v=HwPCpzLmSYQ</ref> | |||
| {{#ev:youtube|hXNuP6ohxwQ}}<ref>SPEED TRAINING: Quick Cut "W" Drill. Available from: https://www.youtube.com/watch?v=hXNuP6ohxwQ</ref> | |||
|} | |||
=== Psychological factors === | === Psychological factors === | ||
Revision as of 12:57, 17 December 2018
Original Editor - Mariam Hashem
Top Contributors - Mariam Hashem, Kim Jackson, Uchechukwu Chukwuemeka, Tarina van der Stockt, Rucha Gadgil, Chelsea Mclene, Leana Louw, Wanda van Niekerk, Jess Bell, Olajumoke Ogunleye and Carin Hunter
Page is under work:
ACL Re-injury[edit | edit source]
Despite advancement in surgical procedures, the outcomes following ACL-reconstruction continue to be poor. Less than 50% of athletes are able to regain their pre-injury level of performance[1]. For those who returned successfully to sport, re-injury remains a risk factor.
The incidence of re-injury in the first two years following reconstruction is estimated to be 6 times greater than those who didn't suffer ACL injury. This incidence is much higher in female athletes[2]. A study reported 29.5% ACL re-injury in the second year with 20% sustaining contralateral injury[2]. The risk of re-injury extends up to 5 years following injury[3].
Re-injury Risk Factors[edit | edit source]
Risk factors of primary and second ACL injury have been investigated widely in the literature. Biomechanical factors such as abnormal loading distribution patters around the knee, increased external knee abduction moment in females[4], side-to-side differences in lower extremities, frontal-plane displacement of the trunk[5] and reduced lower extremity flexor activation in vertical jump[6] have been associated with ACL injury.
Deficits in Quadriceps weakness is a common persisting issue after surgery[7] which is manifested through abnormal loading patterns in gait and sports activities.A deficit of about 20% of quadriceps strength compared to the opposite side is found in athletes after ACL recosntruction. However, even a 90% quadriceps index is not necessarily associated with normal neuromuscular control.
Asymmetry in the kinematics and differences in moment arm between involved side joints compared to the other side is another factor that continues to manifest years following surgery[8].
Abnormal movement patterns are often present bilaterally. changes in kinetics and kinematics of both knees. Studies report higher peak knee angles, moments, and joint powers relative to controls[7]. 3-dimensional biomechanical analyses and postural stability testing reported hip rotation moment changes during landing in the uninvolved side, frontal-plane knee motion during landing, sagittal plane knee moment asymmetries at initial contact, and deficits in postural stability on the reconstructed limb[9].
The development of compensatory strategies of the uninvolved hip is considered to be the primary predictor of risk in athletes who sustained a second ACL injury within the first year of return to play[9]. Therefore, engaging both limbs in rehabilitation is a necessity[7].
Sex may be a contributing factor to secondary ACL injury. Graft rupture is more likely to occur in men, according to a 15 year cohort[10]. Another study reported no difference between sexes in graft rupture, however, contralateral injury was higher in female athletes[11].
Young athletes are at a higher risk of re-injury and also to contralateral injury [7].
Prevention of Re-injury[edit | edit source]
Re-injury and the need to undergo a second ACL-reconstruction place the knee joint under devastating complications of developing OA, knee instability and difficulty in returning to sport. About 25% of athletes undergo a second revision within 6 years of the primary ACL revision[12].
Understanding risk factors associated with re-injury is important to target all deficits in the rehabilitation program.
Four neuromuscular control deficits were considered to be risk factors for second ACL injury[4]:
- Hip rotational control deficits
- Excessive frontal-plane knee mechanics
- Knee flexor deficits
- Postural control deficits
Quadriceps symmetry is essential to return to sport and prevention of future re-injury. Hasmtrins/Quadriceps strength ratio is another important factor to be considered in rehabilitation. The aim is to achieve at least 85% strength symmetry before returning to sport[7].
Single-leg plyometric tests can give the clinician an overview on how the injured limb is functioning and the differences between both sides. Findings in these tests should be considered when setting up the rehabilitation plan[7].
Return to Sport[edit | edit source]
With the high incidence of re-injury and the evidence of poor outcomes of ACL-reconstruction revision, a need for a return to sport protocol has developed.
Myer et al [13] proposed four stages of advanced rehabilitation protocol to address common deficits found in athletes after ACL-reconstruction:
Stage 1: Dynamic stabilization and core strengthening
Stage 2: Functional strengthening
Stage 3:Power development
Stage 4: Sports performance symmetry.
The aim of this protocol is to recondition athletes to function optimally by targeting neurmuscular deficits to minimize rates of re-injury.
Monitoring signs of overload in all stages is critical to prevent adverse effects[13].
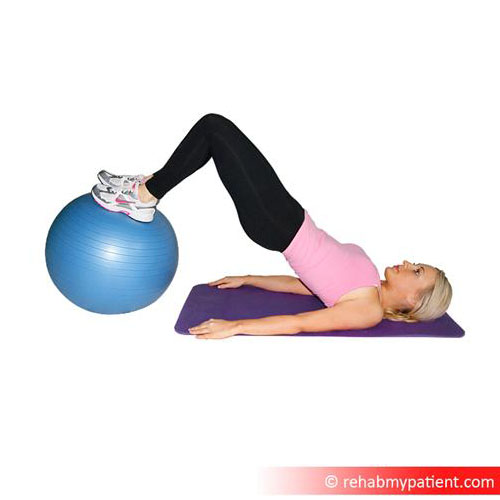
Stage I :Dynamic Stabilization and CORE Strengthening[edit | edit source]
Goals of this stage:
1. Improving single-limb weight-bearing function to tolerate greater knee flexion angles.
2. Improving symmetry of lower extremity in running.
3. Enhancement of closed chain single-limb postural balance.
A strong CORE will allow the athlete to control the deceleration of the center of mass with balanced posture and accelerate their mass rapidly by controlled force. Weakness and deficits in trunk and hip musculature are correlated with biomechanical abnormalities and ACL injuries, particularly in female athletes[4][14].
Prior to CORE strengthening training, balance, proprioception and gait deviations should be well-addressed.
It is important to note that an athlete may have full anatomical ROM but with functional activities, asymmetries and deficits may be present[13]. Addressing these deficits will allow progression in speed and intensity of running without pain and re-injury. Deficits in rhythmic strides and symmetry can be detected by audible monitoring of foot contact. Pain, particularly patellofemoral pain, or ROM deficits are contributing factors to unbalanced sprinting gait. Backward gait is a way of decreasing patellofemoral pain and help the athlete to progress in this stage and may also increase quad strength[13].
Examples of exercises to be used in this stage:

|

|
|
|
Each athlete will need individualized variations according to individual characteristics and sport. Exercise intensity should be changed constantly to challenge balance and proprioception. Modifications of body posture, switching between various unstable surfaces, speed modifications, adding a sport-specific skill and/or adding unanticipated movement can all be ways of challenging stability and balance.
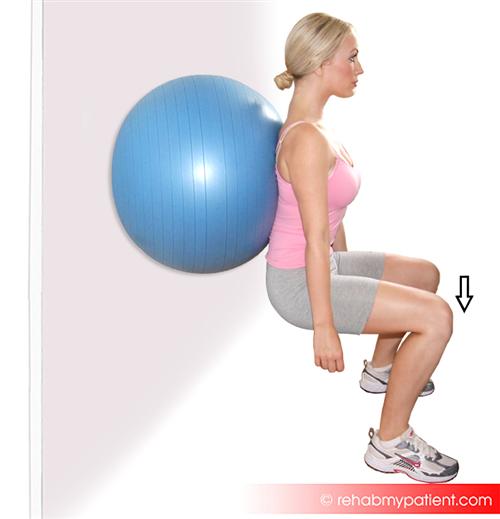
Stage II: Functional strengthening[edit | edit source]
Goals of this stage:
- Increasing lower extremity non weight-bearing strength.
- Improving load distribution pattern over both lower extremities in activities requiring double-leg stance.
- Improvement of single-limb landing force attenuation strategies.
With CORE strengthening and dynamic stabilization exercises continuing throughout this stage, progressive lower extremity strengthening is introduced. Gradually and frequently adding more resistance without compromising good form.
Retrograde training, for example backward running on treadmill or backward jumping, has been shown to increase functional quadriceps activation and to limit patellofemoral pain[15][16]
Examples of exercises to be used in this stage:

|

|
|
File:Single leg bridges on BOSU.gif |
|
|
Stage III: Power development[edit | edit source]
At this stage, power production of lower extremity is the main aim. Additionally, athletes are trained to resist fatigue and perform plyomterics with good biomechanics[13]. Training incorporates mid-level intensity double-limb multi-planar plyometric jumps and low-intensity single-limb hops.
Provide feedback and educate the athlete to land softly with coronal plane knee control.
Combining plyometrics with strength training improved jump performance and leg strength[17]. The addition of neuromuscular training with plyomterics, CORE and speed training resulted in great outcomes in performance measures[13].
Examples of exercises to be used in this stage:

|

|
|

|
| File:Forward and backward jump.gif | File:Swiss ball back extension.gif |
Stage IV: Sport Performance Symmetry[edit | edit source]
At this stage athletes are trained to utilize safe biomechanics (increased knee flexion and decreased knee abduction angles with symmetrical forces and motions between limbs) in high-intensity plyometric exercises, produce symmetrical power between both lower extremities and learn to improve confidence to maintain dynamic knee stability with high-intensity change of direction activities[13].
Verbal and visual feedback are important at this stage.
Increased valgus angle is a factor contributing to injuries, particularly in femals. Valgus loads on the knee can double during unanticipated cutting maneuvers. By teaching athletes to use movement techniques that produce low knee abduction moments during movements that can produce high loads on the joint, they can ultimately reduce the risk of injury[13].
Examples of exercises to be used in this stage:

|
[18] |
| [19] | [20] |
| [21] | [22] |
Psychological factors[edit | edit source]
may play a role at this stage. An athlete may become less motivated to go through the last stages of return-to-sport training as their level of function is improving, they may feel they're able to return to competition level.
Predicting Outcomes after Surgery[edit | edit source]
Age, sex, body mass index (BMI), smoking, concomitant injuries, and physical impairments before and after surgery are important determinants of expected and final outcomes after ACL reconstruction[23][24] but do not fully explain the observed variance in knee function after ACL reconstruction and rehabilitation
Clearance to Return to Sport[edit | edit source]
According to Myer et al[13], an athlete is able to return to sport when they meet the following criteria:
- Drop vertical jump landing force with bilateral symmetry (within 15%).
- Modified Agility T-test (MAT) test time (within 10%).
- Single-limb average peak power test for 10 seconds (bilateral symmetry within 15%).
- Re-assessment of tuck jump (20 percentage points of improvement from initial test score or perfect 80-point score).
Evidence of deficits in musclular strenght and balance exist months postoperatively in ACL-reconstructed knee and contralateral limb[25]. Abnormal knee kinematics was found up to a year following surgery[26]. the need for setting criteria to return to sport.
A systematic review by Barber-Westin and colleagues investigated return to sport criteria in many studies and concluded that in order to give clearance to return to sport an athlete must have:
less than 10% deficit in strength of the quadriceps and hamstring on isokinetic testing at 180°/s and 300°/s,
less than 15% deficit in lower limb symmetry on single-leg hop testing (single hop, triple hop, crossover hop, and timed hop),
less than 3 mm of increased anterior-posterior tibial displacement on Lachman or knee arthrometer testing,
greater than 60% normalized knee separation distance on a video drop-jump test,
no effusion,
full knee motion,
normal patellar mobility,
no or only slight patellar crepitus,
no pain or swelling with all activities.
Other tests to consider are the single-leg squat test to determine postural and lower limb control as well as hip muscular function,30,31 the multistage fitness test to determine maximal oxygen uptake, and the 60-second sit-up test33 or other core strength measures.34 If isokinetic test equipment is not available, a 1-repetition maximum bench press and leg press are recommended if weight room equipment is available, along with an experienced test administrator and a sufficient amount of time to safely conduct these tests.
The International Knee Documentation Committee is a great tool to assess knee function and deffrientiate high knee function from low knee function[24].
Single-legged hop tests are performance-based measures used to assess the combination of muscle strength, neuromuscular control, confidence in the limb, and the ability to tolerate loads related to sports-specific activities. In addition, involved limb deficits can be detected with single-legged hop tests, indicating that those individuals may need more targeted interventions to reduce limb-to-limb differences.
hop tests conducted 6 months postoperatively statistically significantly predicted self-reported knee function
Logerstedt et al[24] concluded that hop tests conducted 6 months postoperatively statistically significantly predicted self-reported knee function. Of the 4 hop tests, the 6-m timed hop and the crossover hop were the best predictors. the 6-m timed hop test was the most useful test for identifying patients with self-reported knee function below normal ranges at 1 year. The crossover hop test had a sensitivity of 88% (Table 6) and was thus the test that most accurately identified patients with knee function within normal ranges. In the current study, the 6-m timed hop was the strongest independent predictor and had the highest discriminatory accuracy. Patients with knee function below normal ranges were more than 5 times more likely to have 6-m timed hop LSI lower than 88% at 6 months than those with knee function within normal ranges.
The 6-m timed hop, the least demanding hop,23,46 can effectively challenge neuromuscular control in patients who have deficits in limb-to-limb differences. These asymmetries strongly predict those who will have knee function below normal ranges at 1 year. Limb asymmetries may be the result of underlying impairments, such as quadriceps weakness,26,53 that may contribute to low hop performance and should be identified and corrected. In addition, limb asymmetries in athletes may result in suboptimal performance on the playing field and are linked with an increased risk of a second ACL injury. Patients with minimal side-to-side differences on the crossover hop test at 6 months possibly will have good knee function at 1 year if they continue with their current training regimen.
Six months after surgery is a typical time point in which patients begin to transition to sports or preinjury activities,30 so administering hop testing at this time point provides clinicians valuable information relevant to patients’ current function, their progress during rehabilitation and the necessity for additional rehabilitation, and their readiness to return to sporting activities.
Patient demographics, health behaviors, concomitant injuries, meniscal surgery, and knee extension range-of-motion loss have been identified as predictors of self-reported knee function.21,29,44 Lower knee function based on self-report outcomes after ACL reconstruction has been associated with lower patient satisfaction and fear of reinjury.28,31
Patients reporting return to preinjury levels of sports participation were more likely to have had less knee joint effusion, fewer episodes of knee instability, lower knee pain intensity, higher quadriceps peak torque-body weight ratio, higher score on the International Knee Documentation Committee Subjective Knee Evaluation Form, and lower levels of kinesiophobia. Knee joint effusion, episodes of knee instability, and score on the International Knee Documentation Committee Subjective Knee Evaluation Form were identified as the factors most strongly associated with self-reported returnto-sport status[27]
These findings support prior studies that have failed to show a strong relationship between demographic measures and function[27]
Six months after ACLR, subjects demonstrated asymmetrical gait patterns despite restoring symmetrical quadriceps strength. Two years after surgery, the majority of gait impairments had diminished, long after sufficient quadriceps strength had been achieved. These data suggest that neuromuscular impairments are common in non-copers even several months after surgery, and that abnormal movement strategies are not resolved solely by addressing their quadriceps strength deficits[28].
Elevated pain-related fear of movement/reinjury, quadriceps weakness, and reduced IKDC score distinguish patients who are unable to return to preinjury sports participation because of fear of reinjury/lack of confidence. Despite low average pain ratings, fear of pain may influence function in this subgroup. Assessment of fear of reinjury, quadriceps strength, and self-reported function at 6 months may help identify patients at risk for not returning to sports at 1 year and should be considered for inclusion in return-to-sport guidelines[29]
Patient psychological factors are predictive of ACL reconstruction outcomes. Self-confidence, optimism, and self-motivation are predictive of outcomes, which is consistent with the theory of self-efficacy. Stress, social support, and athletic self-identity are predictive of outcomes, which is consistent with the global relationship between stress, health, and the buffering hypothesis of social support.[30] theories explaining this finding may be related to the fear-avoidance model of pain, The theory of self-efficacy was originally proposed by Bandura [6]. In this theory, individuals have intrinsic levels of self-efficacy, optimism, and self-motivation, which are considered to be stable personality traits (unchanging from year to year) and are strongly associated with higher rates of task completion in rehabilitation [1, 48] and exercise adherence [18]. Finally, stress, health, and the buffering hypothesis of social support were developed by Cohen [12, 13]. In this model, psychological stress is believed to globally affect physical and mental health [63], and an individual’s degree of social support is believed to modulate this effect[30].
Additionally, patients must be ready and willing to overcome the fear of re-injury to return to their original level of activity and
The reinjury rate was significantly reduced by 51% for each month RTS was delayed until 9 months after surgery, after which no further risk reduction was observed. 38.2% of those who failed RTS criteria suffered reinjuries versus 5.6% of those who passed
Our findings support the use of both time-based and functional RTS criteria. There was an estimated 84% lower knee reinjury rate in patients who passed RTS criteria, a magnitude of high clinical relevance[31].
The most important findings of this present study are that limb-to-limb asymmetries are reduced and limb symmetry indexes are restored to greater than 90% after pre-operative perturbation training and aggressive quadriceps strengthening. The limb-to-limb differences and indexes return to pre-operative levels by 6 months after ACL reconstruction and continue to improve 12 months after ACLR[32]\
optimizing rehabilitation. A shift towards non-operative approaches, The difference in achieving outstanding functional outcomes, irrespective of surgical or non-surgical management, was physical performance (one-leg rise).6 Preventing a delayed ACL reconstruction in those starting with rehabilitation alone was also related to higher physical performance (vertical hop).6. 45% of community-level athletes discontinuing supervised rehabilitation by 3months post-ACLR.7 Targeting patient buy-in through quality individualised patient education, goal-setting and repeated functional testing to provide feedback and enhance motivation to complete adequate exercise and ‘sport-specific rehabilitation’ based on accepted resistance training principles should be a priority for all clinicians. In particular, identification of individual patient needs, co-creation of patient-specific goals and co-design of rehabilitation between clinician and patient[33].
References[edit | edit source]
- ↑ Dunn WR, Spindler KP, Moon Consortium. Predictors of Activity Level 2 Years After Anterior Cruciate Ligament Reconstruction (ACLR) A Multicenter Orthopaedic Outcomes Network (MOON) ACLR Cohort Study. The American journal of sports medicine. 2010 Oct;38(10):2040-50.
- ↑ 2.0 2.1 Paterno MV, Rauh MJ, Schmitt LC, Ford KR, Hewett TE. Incidence of second ACL injuries 2 years after primary ACL reconstruction and return to sport. The American journal of sports medicine. 2014 Jul;42(7):1567-73.
- ↑ Salmon L, Russell V, Musgrove T, Pinczewski L, Refshauge K. Incidence and risk factors for graft rupture and contralateral rupture after anterior cruciate ligament reconstruction. Arthroscopy: The Journal of Arthroscopic & Related Surgery. 2005 Aug 1;21(8):948-57.
- ↑ 4.0 4.1 4.2 Hewett, T.E., Myer, G.D., Ford, K.R., Heidt Jr, R.S., Colosimo, A.J., McLean, S.G., Van den Bogert, A.J., Paterno, M.V. and Succop, P., 2005. Biomechanical measures of neuromuscular control and valgus loading of the knee predict anterior cruciate ligament injury risk in female athletes: a prospective study. The American journal of sports medicine, 33(4), pp.492-501.
- ↑ Zazulak BT, Hewett TE, Reeves NP, Goldberg B, Cholewicki J. Deficits in neuromuscular control of the trunk predict knee injury risk: prospective biomechanical-epidemiologic study. The American journal of sports medicine. 2007 Jul;35(7):1123-30.
- ↑ Hewett TE, Myer GD, Ford KR, Heidt Jr RS, Colosimo AJ, McLean SG, Van den Bogert AJ, Paterno MV, Succop P. Biomechanical measures of neuromuscular control and valgus loading of the knee predict anterior cruciate ligament injury risk in female athletes: a prospective study. The American journal of sports medicine. 2005 Apr;33(4):492-501.
- ↑ 7.0 7.1 7.2 7.3 7.4 7.5 Hewett TE, Di Stasi SL, Myer GD. Current concepts for injury prevention in athletes after anterior cruciate ligament reconstruction. The American journal of sports medicine. 2013 Jan;41(1):216-24.
- ↑ Castanharo R, Da Luz BS, Bitar AC, D’Elia CO, Castropil W, Duarte M. Males still have limb asymmetries in multijoint movement tasks more than 2 years following anterior cruciate ligament reconstruction. Journal of Orthopaedic Science. 2011 Sep 1;16(5):531.
- ↑ 9.0 9.1 Paterno MV, Schmitt LC, Ford KR, Rauh MJ, Myer GD, Huang B, Hewett TE. Biomechanical measures during landing and postural stability predict second anterior cruciate ligament injury after anterior cruciate ligament reconstruction and return to sport. The American journal of sports medicine. 2010 Oct;38(10):1968-78.
- ↑ Leys T, Salmon L, Waller A, Linklater J, Pinczewski L. Clinical results and risk factors for reinjury 15 years after anterior cruciate ligament reconstruction: a prospective study of hamstring and patellar tendon grafts. The American journal of sports medicine. 2012 Mar;40(3):595-605.
- ↑ Shelbourne KD, Gray T, Haro M. Incidence of subsequent injury to either knee within 5 years after anterior cruciate ligament reconstruction with patellar tendon autograft. The American journal of sports medicine. 2009 Feb;37(2):246-51.
- ↑ Battaglia MJ, Cordasco FA, Hannafin JA, Rodeo SA, O'brien SJ, Altchek DW, Cavanaugh J, Wickiewicz TL, Warren RF. Results of revision anterior cruciate ligament surgery. The American journal of sports medicine. 2007 Dec;35(12):2057-66.
- ↑ 13.0 13.1 13.2 13.3 13.4 13.5 13.6 13.7 13.8 Myer GD, Paterno MV, Ford KR, Hewett TE. Neuromuscular training techniques to target deficits before return to sport after anterior cruciate ligament reconstruction. The Journal of Strength & Conditioning Research. 2008 May 1;22(3):987-1014.
- ↑ Padua DA, Marshall SW, Beutler AI, DeMaio M, Boden BP, Yu B, Garrett WE. Predictors of knee valgus angle during a jump-landing task. Medicine & Science in Sports & Exercise. 2005 May 1;37(5):S398.
- ↑ Flynn TW, Soutas-Little RW. Mechanical power and muscle action during forward and backward running. Journal of Orthopaedic & Sports Physical Therapy. 1993 Feb;17(2):108-12.
- ↑ Flynn TW, Soutas-Little RW. Patellofemoral joint compressive forces in forward and backward running. Journal of Orthopaedic & Sports Physical Therapy. 1995 May;21(5):277-82.
- ↑ Fatouros IG, Jamurtas AZ, Leontsini D, Taxildaris K, Aggelousis N, Kostopoulos N, Buckenmeyer P. Evaluation of plyometric exercise training, weight training, and their combination on vertical jumping performance and leg strength. The Journal of Strength & Conditioning Research. 2000 Nov 1;14(4):470-6.
- ↑ Tuck Jump. Available from: https://www.youtube.com/watch?v=zh1v8jINBZ0
- ↑ TFW Explosive Box Step Up. Available from:https://www.youtube.com/watch?v=KDwzB6xuZ9o
- ↑ Depth jump to box jump - Increase vertical jump - Volleyball. Available from: https://www.youtube.com/watch?v=5EztcmA0Amc
- ↑ Four Corner Drill. Available from: https://www.youtube.com/watch?v=HwPCpzLmSYQ
- ↑ SPEED TRAINING: Quick Cut "W" Drill. Available from: https://www.youtube.com/watch?v=hXNuP6ohxwQ
- ↑ Kocher MS, Steadman JR, Briggs K, Zurakowski D, Sterett WI, Hawkins RJ. Determinants of patient satisfaction with outcome after anterior cruciate ligament reconstruction. JBJS. 2002 Sep 1;84(9):1560-72.
- ↑ 24.0 24.1 24.2 Logerstedt D, Grindem H, Lynch A, Eitzen I, Engebretsen L, Risberg MA, Axe MJ, Snyder-Mackler L. Single-legged hop tests as predictors of self-reported knee function after anterior cruciate ligament reconstruction: the Delaware-Oslo ACL cohort study. The American journal of sports medicine. 2012 Oct;40(10):2348-56.
- ↑ Barber-Westin SD, Noyes FR. Factors used to determine return to unrestricted sports activities after anterior cruciate ligament reconstruction. Arthroscopy: The Journal of Arthroscopic & Related Surgery. 2011 Dec 1;27(12):1697-705.
- ↑ Deneweth JM, Bey MJ, McLean SG, Lock TR, Kolowich PA, Tashman S. Tibiofemoral joint kinematics of the anterior cruciate ligament-reconstructed knee during a single-legged hop landing. The American journal of sports medicine. 2010 Sep;38(9):1820-8.
- ↑ 27.0 27.1 Lentz TA, Zeppieri Jr G, Tillman SM, Indelicato PA, Moser MW, George SZ, Chmielewski TL. Return to preinjury sports participation following anterior cruciate ligament reconstruction: contributions of demographic, knee impairment, and self-report measures. journal of orthopaedic & sports physical therapy. 2012 Nov;42(11):893-901.
- ↑ Roewer BD, Di Stasi SL, Snyder-Mackler L. Quadriceps strength and weight acceptance strategies continue to improve two years after anterior cruciate ligament reconstruction. Journal of biomechanics. 2011 Jul 7;44(10):1948-53.
- ↑ Lentz TA, Zeppieri Jr G, George SZ, Tillman SM, Moser MW, Farmer KW, Chmielewski TL. Comparison of physical impairment, functional, and psychosocial measures based on fear of reinjury/lack of confidence and return-to-sport status after ACL reconstruction. The American journal of sports medicine. 2015 Feb;43(2):345-53.
- ↑ 30.0 30.1 Everhart JS, Best TM, Flanigan DC. Psychological predictors of anterior cruciate ligament reconstruction outcomes: a systematic review. Knee Surgery, Sports Traumatology, Arthroscopy. 2015 Mar 1;23(3):752-62.
- ↑ Grindem H, Snyder-Mackler L, Moksnes H, Engebretsen L, Risberg MA. Simple decision rules can reduce reinjury risk by 84% after ACL reconstruction: the Delaware-Oslo ACL cohort study. Br J Sports Med. 2016 May 9:bjsports-2016.
- ↑ Logerstedt D, Lynch A, Axe MJ, Snyder-Mackler L. Symmetry restoration and functional recovery before and after anterior cruciate ligament reconstruction. Knee Surgery, Sports Traumatology, Arthroscopy. 2013 Apr 1;21(4):859-68.
- ↑ Culvenor AG, Barton CJ. ACL injuries: the secret probably lies in optimising rehabilitation. Br J Sports Med. 2018 Mar 16:bjsports-2017.






