ACL Rehabilitation: Acute Management after Surgery: Difference between revisions
No edit summary |
No edit summary |
||
| Line 72: | Line 72: | ||
#Self-Mobilization : posterior capsule stretch using an inverted axillary crutch, heel on axillary pad and leg on arm the patient moves his/her leg into maximum available ROM. | #Self-Mobilization : posterior capsule stretch using an inverted axillary crutch, heel on axillary pad and leg on arm the patient moves his/her leg into maximum available ROM. | ||
#Patellofeomral mobilization: up to 10 minutss of patella on femur mobilization in medial-lateral and superior-inferior directions. This facilitates its mobility, scar mobilization and helps maintaining the integrity of the suprapatellar pouch. | #Patellofeomral mobilization: up to 10 minutss of patella on femur mobilization in medial-lateral and superior-inferior directions. This facilitates its mobility, scar mobilization and helps maintaining the integrity of the suprapatellar pouch. | ||
|} | |||
{| class="wikitable" width="100%" cellspacing="6" cellpadding="0" border="0" | |||
|- | |||
{{#ev:youtube|Vb_FRyydYyI}}<ref>Knee Mobilization (Anterior to Posterior Femur on Tibia Mobilization). Available from: https://www.youtube.com/watch?v=Vb_FRyydYyI</ref> | {{#ev:youtube|Vb_FRyydYyI}}<ref>Knee Mobilization (Anterior to Posterior Femur on Tibia Mobilization). Available from: https://www.youtube.com/watch?v=Vb_FRyydYyI</ref> | ||
{{#ev:youtube|uNWkHPcpDfY}}<ref>Restoring Knee Screw Home Mechanism. Available from: https://www.youtube.com/watch?v=uNWkHPcpDfY</ref> | {{#ev:youtube|uNWkHPcpDfY}}<ref>Restoring Knee Screw Home Mechanism. Available from: https://www.youtube.com/watch?v=uNWkHPcpDfY</ref> | ||
|- | |||
{{#ev:youtube|OLvJwe5GAfg}}<ref>CPM Machine in Use. Available from: https://www.youtube.com/watch?v=OLvJwe5GAfg</ref> | {{#ev:youtube|OLvJwe5GAfg}}<ref>CPM Machine in Use. Available from: https://www.youtube.com/watch?v=OLvJwe5GAfg</ref> | ||
{{#ev:youtube|kcYDCDbsh3s}}<ref>Knee Capsular Stretch. Available from:https://www.youtube.com/watch?v=kcYDCDbsh3s </ref> | {{#ev:youtube|kcYDCDbsh3s}}<ref>Knee Capsular Stretch. Available from:https://www.youtube.com/watch?v=kcYDCDbsh3s </ref> | ||
{{#ev:youtube|sGVbR1EiJzs}}<ref>Treat Knee Cap Pain (Patellar Mobilization Technique). Available from: https://www.youtube.com/watch?v=sGVbR1EiJzs</ref> | |- | ||
{{#ev:youtube|sGVbR1EiJzs}}<ref>Treat Knee Cap Pain (Patellar Mobilization Technique). Available from: https://www.youtube.com/watch?v=sGVbR1EiJzs</ref>|} | |||
=== Restoring Quad Strength=== | === Restoring Quad Strength=== | ||
Revision as of 14:14, 7 November 2018
Original Editor - Mariam Hashem
Top Contributors - Mariam Hashem, Kim Jackson, Tarina van der Stockt, Tony Lowe, Chelsea Mclene, Rachael Lowe, Leana Louw, Wanda van Niekerk, Jess Bell, Robin Tacchetti and Jorge Rodríguez Palomino
Introduction[edit | edit source]
Anterior Cruciate Ligament injury is one of the most common injuries among different sports. In football , the range of ACL injuries has been estimated to range from 0.06 to 10 injuries per 1000 game hours. Professional athletes are more prone to ACL injures[1]. Most injuries occur when the opposite tam has the ball and the players are defending with tackling and cutting are considered the most common playing actions assosiated with the injury (51% and 15% respectively).
Females are at a higher risk for ACL injury[2] due to many factors such as higher valgus stress and loading in females when performing tasks, differences in hamstring/quadriceps strength ratio and vastus lateralis/semitendinous strength ratio, lateral and posterior hip insufficiencies, and nondominant leg strength differences[3]. In contrast, a case series report by Brophy et al reported no differences between the genders[4]. The difference between male ad female athletes according to this report was in the mechanism of injury; males were more likely to suffer contact injuries (56%) while noncontact injuries were dominant among female players.
In other sports, the incidence rates vary. In skiing, ACL injury represent 30.9 per 100,000 skiers per day[5]. While in basketball, 17 per 100,000 athletic exposures were repoted between 1989 and 2004 in the USA[6].
Instability, knee OA, inability to return to sport(only 65% of NFL players are able to regain pre-injury performance)[7] and recurrent injuries are among the short and long term list of consequences that follow ACL injury. OA after injury is reported to be very high, reaching 100%, in both conservative and surgical treatment[8].
Considerations Before Desigining a Rehabilitation Program[edit | edit source]
ACL injury is often a complex presentation with other associated damages such as mensicus injury, medial collateral injury, bone contusion and chondral injury.
The highest recurrence rates of ACL injury and the fact that many players may not be able to return to their proir level of performance challenges the rehabilitation strategy. It is recommended that oucome measures should not be based on a timely manner, instead a clearence to return to sport should be given according to performance levels as we will discuss later.
Since it is not a simple injury, a multidisciplinary team is needed to help athletes recover and maintain their level of performance. Inaddition to physiotherapy you should keep communication channels open with the following professionals and know when to refer your patient to them:
- Orthopedic Surgeon to track your patient progress.
- Sports Psychologist; when he athletes are struggling to return to sport.
- Sports Nutritionist; the time spent away from the field has devastating consequences on muscle mass and body composition. An individualized nutrition plan is also needed to facilitate recovery and return to sport.
Despite the rich body of literature on ACL rehabilitation, the evidence regarding rehabilitation characteristics is still inconclusive.
Acute Management Goals[edit | edit source]
At this stage (0-6 wks) after surgery, the aim is to protect the surgical repai/reconstruction and prepare patient for restoring function. The acute management has its specific goals that need to be considered:
- Joint Homeostasis
- Scar management
- ROM in all directions
- Quadriceps independent work and terminal extension range
- A long term plan for 6-9 months of recovery. To draw a map for your patient and explain the process to them, engage them in setting goals and also to det time-specific milestones that would help in desigining your program.
Protection of the post surgical repair is done by the following:
- Limiting ROM to 90° until femoral and/or adductor nerve block is gone (usually it takes 48-72 hours). Once patient can report accurate sensation, ROM is allowed with regard to patient comfort. Passive ROM is allowed in all directions, since it doesn't place any negative stress on the ligament[9].
- Bracing in a mobilizer until femoral/adductor nerve block is off then change to a hinged-knee brace for 3-7 days or until the patient is able to perform terminal knee extension, depending on the time you see your patient.
- Partial Weight Bearing is recommended for two weeks after surgery to minimize swelling and inflammation and allow full resolution of effusion.
- Stationary Bike without resistance is introduced on day 10, or when the patient achives >110° passive flexion[8]
- Complete weight bearning strength training is delayed up to 6 weeks.
Homeostasis[edit | edit source]
A joint with abnormal homeostasis would typically be painful, swollen and stiff. Loading a normal joint will result in normal responses, however, in the presence of post-surgical inflammation the loading response will be devastating and can result in drastic events. Frequent evaluation of activities and slowing down whenever a sign of overloading is present is required to restore homeostasis as soon as possible[10].
- Restored homeostasis is crucial to prevent the following consequences:
- Limited ROM, particularly flexion. Extension could be limited due to other factors such as meniscus injury.
- Inhibited neuromuscular firing pattern of quadriceps.
- Normal scar healing as a result of prolonged inflammatory phase.
- Unrestored homeostasis can lengthen the entire rehab process.
To restore homeostasis, activities and exercises should be within normal or low load to avoid stressing the heeling tissue. You can also incorporate various modalities in the rehabililtation program such as lymphedema massage, pneumatic compressive devices, elevation, and active muscle pump from the quadriceps and calves[8].
Scar Management and ROM[edit | edit source]
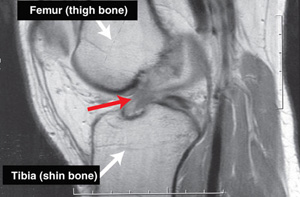
The Anterior Interval, between the tibia and the inferior border of the patella, and the suprapatella pouch, between femur and quadriceps tendon, both have a role to play in providing volume for the joint to move freely throughout the entire ROM. Scar formation, particularly in the proliferation phase up to 6 wks postsurgical, may form in these gaps in a rigid texture resulting in negative consequences such as:
- Restricting ROM and hindering joint’s ability to move freely by binding patellar tendon and quadriceps tendon gap to the femur and tibia respectively.
- Increases the joint contact pressure, which maybe a contributing factor to anterior knee pain and the long term development of knee OA 10-15 years after surgery.
- Patellofemoral OA, could be developed as early as five years after surgery. Scar may contribute to this through restricting the anterior knee mobility causing cartilage breakdown when loaded with normal or sport activities.
Scar also decreases the moment arm of the extensor mechanism, reducing the extension force produced by the quad. This is an important clinical note, because it is a frequent observation that some ACL injured athlets may not be able to regain their quadriceps performance even after 9 months of post-surgical rehabilitation. The reason is simple because of the reduced moment arm due to scar formation. Our role at this pont is to guide an organized proliferation of the scar without later consequences on ROM and mobility, this can be facilitated through:
- Early ROM exercises, from the first day after surgery, to create a pressure gradient within the knee; flushing blood and inflammatory cells created after surgery. Passive ROM exercises such as therapist assisted at the end of the bed full knee flexion or wall slides, patient lying on their back assisting with opposite leg to allow maximum available ROM up to the level of patient’s comfort. Also, a bonus from the elevated position in flushing effusion.
Another example of Passive ROM exercise: flexion of swiss ball, leg lying straight on table therapist flex the knee till the patient starts reporting symptoms of discomfort or pain or you begin to feel tissue tension. Small oscillations at the end range will eventually help in regaining ROM with time.
- Stationary bike as a low load activity is a great tool in the acute phase management. Repeated flexion and extension motions facilitates mobility and smoothes the scar proliferation.
- Loss of extension is one of the most common complications. A small degree of knee flexion contracture will restrict the quads ability to regain full strength which is important for functional outcomes. For the quads to work with maximum efficiency , the knee must be able to sustain full extention. Full extension is also necessary for reducing the surface area of load distribution on the entire joint surface. Unlike in a flexion contracture case, point loading will lead to arthritis development.
Methods of restoring Extension:
- Manual therapy/mobilization (posterior femoral glides, screw home mobilizations
- PROM external devices.
- Soft tissue massage
- Self-Mobilization : posterior capsule stretch using an inverted axillary crutch, heel on axillary pad and leg on arm the patient moves his/her leg into maximum available ROM.
- Patellofeomral mobilization: up to 10 minutss of patella on femur mobilization in medial-lateral and superior-inferior directions. This facilitates its mobility, scar mobilization and helps maintaining the integrity of the suprapatellar pouch.
|}
[12][13][14][15][16]|}
Restoring Quad Strength[edit | edit source]
Facilitating isolated quadriceps contraction by teaching patient how to fire the muscle independently will prevent overlapped firing patterns and compensations from other muscles. Ask patient to glide patella superiorly. This simple exercise, even if it's only a flicker contraction, triggers quadriceps isolated contraction. Building progression from here will aid in performing terminal knee extension which if lost might manifest itself in a flexed knee gait pattern. Terminal Knee exension is facilitated by asking patient to pop their heel off table.
Create a plan[edit | edit source]
A multi-phasic ACL rehab plan has nine essential milestones, each phase requires a relevant time frame that should be individualized according to athletic needs. Remember: Don’t rush rehabilitation. Let it take its time.
ACL rehabilitation plan have 9 phases, around wich a suitable time frame should be allowed to prevent recurrece/re-injnury:
- ROM restoration and protection
- Weight Bearing Tolerance
- Endurance
- Strength
- Power
- Running
- Speed and Agility
- Return to Training
- Return to Play
Progression to Next Phase[edit | edit source]
The patient is ready to move to the next stage of rehabilitation once is able to demonestrate the following[8]:
- Full active terminal knee extension (0°)
- Flexion within 10° of the contra-lateral side.
- Resolved knee effusion (0.5 cm of contra-lateral knee)
- Able to walk without assistive devices.
References[edit | edit source]
- ↑ Rochcongar P, Laboute E, Jan J, Carling C. Ruptures of the anterior cruciate ligament in soccer. International journal of sports medicine. 2009 May;30(05):372-8.
- ↑ Brophy R, Silvers HJ, Gonzales T, Mandelbaum BR. Gender influences: the role of leg dominance in ACL injury among soccer players. British journal of sports medicine. 2010 Jun 1:bjsports51243.
- ↑ Hewett TE, Myer GD, Ford KR, Heidt Jr RS, Colosimo AJ, McLean SG, Van den Bogert AJ, Paterno MV, Succop P. Biomechanical measures of neuromuscular control and valgus loading of the knee predict anterior cruciate ligament injury risk in female athletes: a prospective study. The American journal of sports medicine. 2005 Apr;33(4):492-501.
- ↑ Brophy RH, Stepan JG, Silvers HJ, Mandelbaum BR. Defending puts the anterior cruciate ligament at risk during soccer: a gender-based analysis. Sports health. 2015 May;7(3):244-9.
- ↑ Demirağ B, Oncan T, Durak K. An evaluation of knee ligament injuries encountered in skiers at the Uludag Ski Center. Acta orthopaedica et traumatologica turcica. 2004;38(5):313-6.
- ↑ Mihata LC, Beutler AI, Boden BP. Comparing the incidence of anterior cruciate ligament injury in collegiate lacrosse, soccer, and basketball players: implications for anterior cruciate ligament mechanism and prevention. The American journal of sports medicine. 2006 Jun;34(6):899-904.
- ↑ Ardern CL, Taylor NF, Feller JA, Webster KE. Fifty-five per cent return to competitive sport following anterior cruciate ligament reconstruction surgery: an updated systematic review and meta-analysis including aspects of physical functioning and contextual factors. Br J Sports Med. 2014 Nov 1;48(21):1543-52.
- ↑ 8.0 8.1 8.2 8.3 Bousquet BA, O'Brien L, Singleton S, Beggs M. POST-OPERATIVE CRITERION BASED REHABILITATION OF ACL REPAIRS: A CLINICAL COMMENTARY. International Journal of Sports Physical Therapy. 2018 Apr 1;13(2).
- ↑ Wright RW, Preston E, Fleming BC, Amendola A, Andrish JT, Bergfeld JA, Dunn WR, Kaeding C, Kuhn JE, Marx RG, McCarty EC. ACL reconstruction rehabilitation: a systematic review part I. The journal of knee surgery. 2008 Jul;21(3):217.
- ↑ Van Grinsven S, Van Cingel RE, Holla CJ, Van Loon CJ. Evidence-based rehabilitation following anterior cruciate ligament reconstruction. Knee Surgery, Sports Traumatology, Arthroscopy. 2010 Aug 1;18(8):1128-44.
- ↑ After Knee Injury or Surgery - Wall Slide Exercises to increase Knee Range of Motion. Available from: https://www.youtube.com/watch?v=b00UCkvYgzE
- ↑ Knee Mobilization (Anterior to Posterior Femur on Tibia Mobilization). Available from: https://www.youtube.com/watch?v=Vb_FRyydYyI
- ↑ Restoring Knee Screw Home Mechanism. Available from: https://www.youtube.com/watch?v=uNWkHPcpDfY
- ↑ CPM Machine in Use. Available from: https://www.youtube.com/watch?v=OLvJwe5GAfg
- ↑ Knee Capsular Stretch. Available from:https://www.youtube.com/watch?v=kcYDCDbsh3s
- ↑ Treat Knee Cap Pain (Patellar Mobilization Technique). Available from: https://www.youtube.com/watch?v=sGVbR1EiJzs