Thyroid Cancer
Top Contributors - Adam Hooten, Andrew Stethen, Lucinda hampton, Kim Jackson, Vidya Acharya, WikiSysop, Elaine Lonnemann, 127.0.0.1, Wendy Walker and Adam Vallely Farrell
Introduction[edit | edit source]
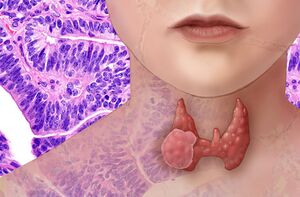
Thyroid cancer is a malignancy arising from the thyroid parenchymal cells.
- Its incidence is steadily increasing worldwide while the mortality rate has remained stable over the past several years.
- The clinical behavior of thyroid cancer is highly variable ranging from indolent slowly progressing tumors to highly aggressive tumors with high mortality rates. [1]
Types of Thyroid Cancer[edit | edit source]
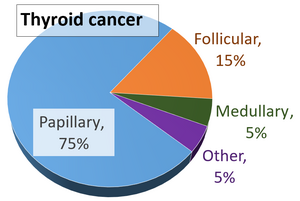
Common types of thyroid cancer include:
- Papillary (about 70 to 80% of all thyroid cancer cells) – develops from the follicular cells and tends to grow slowly
- Follicular (about 15 to 20%) – develops from the follicular cells and includes Hürthle cell carcinoma, a less common subtype.
Rarer types of thyroid cancer include: medullary (about 4%) – develops from the parafollicular cells (C-cells). It can run in families and may be associated with tumours in other glands; anaplastic (about 1%) – may develop from papillary or follicular thyroid cancer. It tends to grow quickly and usually occurs in people over 60 years old[2].
Epidemiology[edit | edit source]
Thyroid Cancer represents 1% to 4% of all malignancies and is the fifth most common cancer in women in the United States.
- Females are more commonly effected than male (around 3:1).
- There has been a steady rise in the incidence of thyroid cancer globally, in both genders and among all races and is thought to be primarily due to an increasing trend in the rate of diagnostic imaging.[1]
- Thyroid cancer is more commonly diagnosed at a younger age than most other adult cancers. Nearly 70% of new cases are found in people younger than 55 and about 2% are found in children and teens.
- The death rate for thyroid cancer remains low compared to other cancers. [3]
Etiology[edit | edit source]
The cause of thyroid cancer is unknown, however, people who have their thyroid gland exposed to high doses of radiation or have a family history of thyroid cancer are at a higher risk of developing thyroid cancer. The risk of thyroid cancer also increases as we age. High doses of radiation such as from reoccurring chest x-rays, especially in childhood, can lead to thyroid cancer.
Treatments and X-rays for Hodgkin's disease and breast cancer have been shown to have a greater risk for thyroid cancer. Generally, exposure form routine x-rays such as a simple chest x-ray and dental x-rays have not been linked to increasing the risk for thyroid cancer.
Radioactive iodine has also been linked to causing thyroid cancer. Examples of radioactive iodine causing thyroid cancer would include Chernobyl, a Russian nuclear power plant accident in 1986, and the tsunami-related nuclear power plant disaster in 2011 in Japan. [4]
Characteristics/Clinical Presentation[edit | edit source]
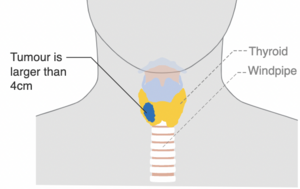
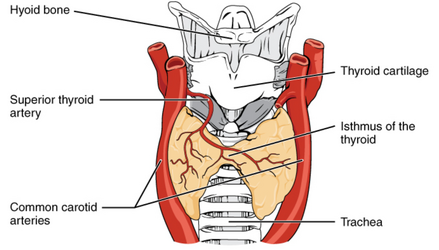
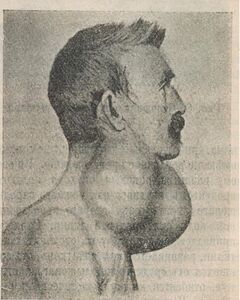
Generally, Thyroid cancer does not cause any symptoms, but a person may have a lump or nodule around the thyroid in the neck area. The most common sign of thyroid cancer is a nodule that may be noticed by a physician, or even the patient themselves as they put on a necklace, button a shirt or coat, or looking in the mirror. On rare occasions, thyroid cancer may actually present with symptoms such as pain in the jaw, neck or ear areas. The nodule can compress the airway if it gets large enough which can lead to difficulty breathing or swallowing and hoarseness. The patient may complain of a "tickle in the throat". [4]
Systemic Involvement: The most common places in the body for thyroid cancer to spread to are the lungs, liver, and bones. [5]
Diagnostic Tests[edit | edit source]
Thyroid cancer is commonly diagnosed using a fine needle aspiration biopsy of a thyroid nodule. The biopsy can also be done after the nodule has been removed during surgery. [4]Other tests can include:
- Ultrasound – to get detailed information about the thyroid including the size of any thyroid nodule and whether it is full of fluid or solid.
- Blood tests – to check hormone levels and function of the thyroid. Calcitonin levels may also be checked.
- CT scans
- PET scans – uses an injection of a glucose (sugar) solution to help cancer cells show up more brightly on the scan[2].
Staging[edit | edit source]
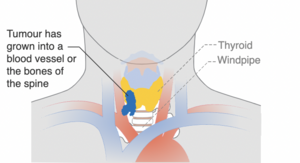
The stage of a cancer means how far it has grown in your body. Often the information needed for accurate staging is available only after surgery. The most common way to decide on a stage for thyroid cancer is the TNM system (tumour-nodes-metastasis). This system describes if the:
- Cancer is smaller and remains inside the thyroid or if it is larger and has spread to other parts of the neck
- Cancer has spread to nearby lymph nodes
- Cancer has spread to other parts of the body, such as the lungs or bones.[2]
Medical Management[edit | edit source]
There are various types of treatment options available for those diagnosed with thyroid cancer. There are standard treatments and some that are being tested in clinical trials. There are currently five standard treatments:
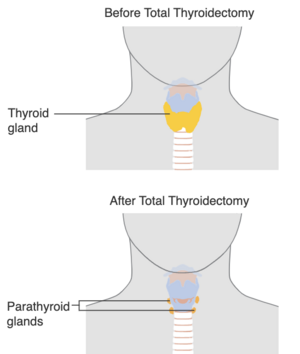
Surgery: Most common form of treatment - Lobectomy (Removal of the lobe of the lung with the cancer)
- Near-toal thyroidectomy (Removal of nearly all the thyroid gland)
- Total thyroidectomy (Removal of all the thyroid gland)
- Lymphadenectomy (Removal of cancerous lymph nodes in the neck)
Radiation therapy: (including radioactive iodine therapy or RAI)
- RAI is used for follicular and papillary thyroid cancers. This is taken by mouth and will collect any remaining thyroid cancer cells that may have spread. Since only the thyroid gland takes up iodine, no other tissue is harmed.
- Radiation uses high energy x-rays to kill cancer cells and keep them from growing (depends on stage and type of cancer).
Chemotherapy: Uses drugs (by mouth or injection) to stop the growth of cancer cells. (Depends on type and stage of cancer).
Thyroid hormone therapy: Hormone therapy removes hormones or blocks their action to stop cancer cells from growing. For thyroid cancer, drugs are given to prevent the body from making Thyroid-stimulating hormone (TSH) because this hormone increases the chance that the thyroid cancer will grow or recur.
Targeted therapy: Uses drugs or other substances to kill cancerous cells and avoid harming normal cells. Vandetanib, a type of Tyrosine Kinase Inhibitor (TKI), is used to block signals needed for thyroid tumors to grow. [6]
Patients with thyroid cancer may want to think about participating in a clinical trial. More information can be found at: http://www.cancer.gov/clinicaltrials
Physical Therapy Management[edit | edit source]
Exercise has recently been shown through research to be safe and possible during cancer treatment.[7] Research suggests there is a decrease in neck range of motion and increase in trigger points in neck muscles after thyroidectomy.[8] Physical Therapy for cancer treatment can include exercises to improve flexibility, strength, and endurance. Massage may also be used to help decrease stress, pain, and scar tissue during and after cancer treatment. It is important to maintain an active lifestyle to help improve quality of life and reduce stress and fatigue.
Physical Therapy can help build the body's tolerance to cancer treatments like chemotherapy and radiation through the use of exercise to increase heart rate, muscular strength, and range of motion.[9] Lack of activity can lead to muscle weakness, decreased range of motion, and decreased body function. [7]
Ways regular exercise may help you during cancer treatment [7]
• Keep or improve your physical abilities
• Better balance, lower risk of falls and broken bones
• Keep muscles from wasting due to inactivity
• Lower the risk of heart disease
• Lessen the risk of osteoporosis
• Improve blood flow to your legs and lower the risk of blood clots
• Make you less dependent on others for help with normal activities of daily living
• Improve your self-esteem
• Lower the risk of being anxious and depressed
• Lessen nausea
• Improve your ability to keep social contacts
• Fewer symptoms of fatigue
• Help you control your weight
• Improve your quality of life
References[edit | edit source]
- ↑ 1.0 1.1 Lee K, Anastasopoulou C, Chandran C, Cassaro S. Thyroid Cancer. StatPearls [Internet]. 2021 May 3.Available:https://www.ncbi.nlm.nih.gov/books/NBK459299/ (accessed 24.2.2022)
- ↑ 2.0 2.1 2.2 Better health Channel Thyroid Cancer Available: https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/thyroid-cancer(accessed 25.2.2022)
- ↑ American Cancer Society. Thyroid Cancer. http://www.cancer.org/acs/groups/cid/documents/webcontent/003144-pdf.pdf. Updated March 20, 2014. Accessed March 25, 2014.
- ↑ 4.0 4.1 4.2 American Thyroid Association. Thyroid Cancer. http://www.thyroid.org/cancer-of-the-thyroid-gland/. Accessed March 20, 2014.
- ↑ National Cancer Institute. Metastatic Cancer. http://www.cancer.gov/cancertopics/factsheet/Sites-Types/metastatic. Updated March 28, 2013. Accessed March 25, 2014.
- ↑ National Cancer Institute. Thyroid Cancer. http://www.cancer.gov/cancertopics/types/thyroid. Accessed March 6, 2014.
- ↑ 7.0 7.1 7.2 American Society of Clinical Oncology. Thyroid Cancer. http://www.cancer.net/cancer-types/thyroid-cancer. Reviewed 7/2013. Accessed March 6, 2014.
- ↑ Rodríguez‐Torres J, López‐López L, Cabrera‐Martos I, Torres‐Sánchez I, Ortíz‐Rubio A, Valenza MC. Musculoskeletal neck disorders in thyroid cancer patients after thyroidectomy. European journal of cancer care. 2019 Jul;28(4):e13053.
- ↑ American Cancer Society. How is Thyroid Cancer Staged?http://www.cancer.org/cancer/thyroidcancer/detailedguide/thyroid-cancer-staging. Revised March 20, 2014. Accessed March 25, 2014.