Peroneus (Fibularis) Longus Muscle
Original Editor - Jenny Lim
Top Contributors - Jenny Lim, Beverly Klinger, Vidya Acharya, Patti Cavaleri, Kim Jackson, Leana Louw and Oyemi SilloDescription[edit | edit source]
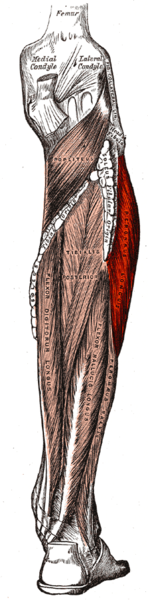
The Peroneus (Fibularis) Longus muscle, along with the Fibularis Brevis muscle make up the lateral compartment of the lower leg. The Fibularis Longus lies superficial to the Fibularis Brevis and is the largest of the Fibularis muscles.[1] The Fibularis Longus extends down the lateral compartment of the lower limb where at the midpoint it tapers in to a long tendon that descends in to the foot.[1][2]
Anatomy[edit | edit source]
Origin[edit | edit source]
- Lateral condyle of tibia
- Head and proximal two-thirds of the lateral surface of fibula
- Intermuscular septa
- Adjacent deep fascia[3][4]
Insertion[edit | edit source]
While traveling distally, the peroneus longus tendon turns at the retromalleolar region and in the cuboid tunnel. In the retro-malleolar groove, the tendon is secured in place, along with the peroneus brevis tendon, by the superior peroneal retinaculum[2].
- Lateral base of first metatarsal
- Medial cuneiform bone[3]
Nerve[edit | edit source]
Superficial Peroneal (Fibular) nerve - L5, S1, S2.[1]
Artery[edit | edit source]
Anterior Tibial and Peroneal (Fibular) arteries.[1][3]
Function[edit | edit source]
- Eversion the ankle and foot
- Assists in ankle plantar flexion
- In weight-bearing position depresses head of first metatarsal due to the strong pull on its insertion
- Maintains the transverse arch of the foot as a result of how it crosses the sole of the foot.
- Steadies the leg on the foot in single leg stance by drawing on the lateral leg, and stops it from collapsing medially.[3]
Clinical relevance[edit | edit source]
Peroneal tendon injuries are most commonly present in patients that are young, active, and in those who participate in sports such as football, soccer, and running. Injury to the peroneus longus tendon can cause lateral ankle pain and may lead to ankle instability.[1] The retromalleolar turn and cuboid tunnel turns are common injury sites[2].

The fibularis longus muscle is susceptible to several pathologies, including:
- Peroneal tendinopathy
- Peroneal Tendon Subluxation or instability
- Weakness:
- Lessens the ability to stand on the toes
- Decreases the lateral stability of the ankle
- Allows a varus position of the foot
- Contracture/shortening: Results into an everted or valgus foot.
- Fibularis longus muscles and tendon tears: Tears most commonly longitudinal due to subluxation over the fibula, however can also present as transverse.[1]
- Fibular avulsion fractures as a result of peroneus longus tendon tearing
- Painful os peroneum syndrome[7]
- Compartment Syndrome[1]
- Muscle herniation through the overlying fascia may appear as a mass over the lateral calf[2]
- Best assessed through dynamic ultrasound and muscle contraction
Assessment[edit | edit source]
A physical exam should be performed to assess the range of motion and motor strength of the ankle. Weakened or absent motor strength with plantar flexion and eversion could indicate muscle or nerve damage to the peroneus longus and/or peroneus brevis muscles. Pain may be present during palpation of the tendon proximal and posterior to the lateral malleolus.[1]
Treatment[edit | edit source]
Most patient who present with a Fibularis Longus injury are treated conservatively:[2]
- Rest
- Ice
- Compression
- Non-steroidal anti-inflammatory medications (NSAIDs)
- Activity Modification
- Physiotherapy:
- Strengthening
- Stretching
- Manual techniques such as massage, specific soft tissue mobilizations and myofascial release
- Dry Needling
| [8] | [9] |
If conservative treatment fails or a patient presents with a peroneal tendon tear, surgical treatment may be required. Surgical techniques may include tendon debridement and/or tenosynovectomy for tendinitis.[1][2] If a peroneal tendon tear is present, surgical treatment may include an end to end repair, side-to-side anastomosis or Pulvertaft weave (chronic tears), tendon transfer, or an allograft reconstruction.[1]
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 1.7 1.8 1.9 Lezak B, Summers S. Anatomy, Bony Pelvis and Lower Limb, Extensor Hallucis Longus Muscle. August 2020
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 Hallinan JT, Wang W, Pathria MN, Smitaman E, Huang BK. The peroneus longus muscle and tendon: a review of its anatomy and pathology. Skeletal radiology. 2019 Sep;48(9):1329-44.
- ↑ 3.0 3.1 3.2 3.3 Moore KL, Dalley AF, Agur AMR. Clinial oriented anatomy. Philadelphia: Wolters Kluwer, 2010.
- ↑ Peroneus Longus and Brevis. In: Kendall FP, McCreary EK, Provance PG. Muscle Testing and Function, 4th edition. Philadelphia: Lippincott Williams & Wilkins, 1993. p.203.
- ↑ Ebraheim N. Anatomy Of The Peroneus Longus Muscle - Everything You Need To Know - Dr. Nabil Ebraheim. Available from: https://www.youtube.com/watch?v=v_0TSoPzd3A (accessed 17/06/2018).
- ↑ Case courtesy of Dr Andrew Dixon, Radiopaedia.org, rID: 30218
- ↑ Hallinan JT, Wang W, Pathria MN, Smitaman E, Huang BK. The peroneus longus muscle and tendon: a review of its anatomy and pathology. Skeletal radiology. 2019 Sep;48(9):1329-44.
- ↑ ReBalance Physiotherapy. Day -69: Peroneal Strengthening. Available from: https://www.youtube.com/watch?v=3Xpwd5gTzXw (accessed 17/06/2018).
- ↑ Trevail T. Dry Needling: Peroneus Longus & Brevis. Available from: https://www.youtube.com/watch?v=ON0s8OFXfOs (accessed 17/06/2018).