Duchenne Muscular Dystrophy - Young Adult Case Study
Abstract:
Duchenne muscular dystrophy (DMD) is a neurological disorder that affects both the skeletal and heart muscle, leading to muscle degeneration. It is noticed in early childhood and is primarily seen in males. [1]For the purposes of education, a fictitious case study has been created involving an 18-year old university student Breydon King, who was diagnosed with DMD at the age of five, and is being referred to physiotherapy to address current problems.
Over the past few weeks, Breydon has had trouble participating in his extracurriculars and with his school related work. He reports having difficulty opening his hands, preventing him from taking notes with his keyboard, and practicing the guitar. He also reports that he is experiencing shortness of breath while speaking and while sleeping during the night. Breydon expresses that his health is making him very anxious, along with the added stress from school. He is hoping physiotherapy will allow him to better himself so that he can focus on his school work and participate in hobbies.
Breydon’s physiotherapy treatment included respiratory training, postural training, stretching of the upper limbs, and orthotics prescription. A multidisciplinary approach was used to assist Breydon in reaching all his goals. Through Breydon’s story, this case outlines the many challenges and lifestyle changes of an individual living with DMD as a young adult.
Introduction:
Duchenne Muscular Dystrophy(DMD) is an X-linked recessive disorder caused by mutations in the dystrophin gene.[2] The mutation causes a defect in the synthesis of the protein dystrophin, leading to progressive degeneration of muscles all over the body.[2] DMD has an incidence of about 1 in 3500 live male births. Most patients are diagnosed at approximately 5 years of age, when they lag behind their peers in physical abilities.[2]
This disease results in progressive deterioration in limb and trunk strength, resulting in loss of independent ambulation by age 12.[2] In milder forms of the disease such as intermediate muscular dystrophy and Becker muscular dystrophy, the process of degeneration is slow and loss of ambulation occurs at around age 16.[2]
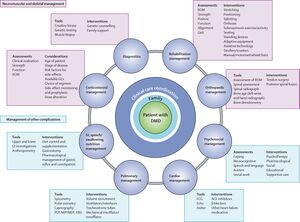
The genetic basis of DMD has been known for over 30 years and many encouraging therapeutic strategies have been developed.[2] Advancements in corticosteroid, respiratory, cardiac, orthopedic, and rehabilitative interventions have led to improvements in function, quality of life, health, and longevity.[2] Children diagnosed with DMD today have the possibility of living into their 40s. [2]An interdisciplinary approach (Figure: 1) is critical for management of DMD in which the individual and family can access the expertise for the required multi-system. [3]The interdisciplinary team would include a wide range of health-care professionals depending on local services, including (but not limited to) primary care Physicians, pediatricians, neurologists, physiotherapists and occupational therapists.[2]
Client Characteristics:
Breydon King is an 18-year-old freshman studying Political Science at the University of Toronto. At five years of age he was diagnosed with DMD after his parents noticed multiple falls, difficulty going up a flight of stairs, and the inability to keep up with his teammates on the soccer field. At the age of twelve, Breydon became fully dependent on an electric wheelchair. Being mobile allows him to get around a lot easier and pursue his passions, such as participating in his weekly guitar club, and giving motivational speeches. He currently lives with his family near his university campus and receives help with his activities of daily living with a daily Personal Support Worker (PSW). With the added pressure from university, Breydon has reported feelings of anxiousness; he is feeling a lot more tired sitting for longer periods, and difficulty with fine finger movements while playing his guitar and typing notes on his computer after a short period of time. He states that he has been able to take notes using his speech to text dictation technology system since he attends lectures on zoom from home, but fears he will not be able to do so once classes return to in person in the fall.
Examination Findings:
Subjective
History of Present Illness Breydon reports feeling tightness and loss of range of motion in both hands but more in his right wrist, hand and fingers starting 2 months ago, soon after he started university. He notices that he experiences more tightness in his index finger compared to other fingers. The discomfort has gotten progressively worse since then and lingers for longer periods of time. This stiffness not only affects his range of motion, but also limits his speed in typing, writing, playing guitar, and other daily tasks requiring fine motor movement of his hands. Increased tightness presents early in the morning and at the end of the day. Breydon has also been experiencing more than usual pain in the same areas of tightness. Braydon reports headaches in the morning and waking up several times during the night because of shortness of breath. He also reports increased shortness of breath when giving his biweekly motivational speeches at the elementary and high schools around his city. He experiences shortness of breath during the speech followed by increased fatigue for the rest of the day. Breydon expresses frustration and increased anxiety as these recent problems greatly interfere with his school life and extracurricular hobbies.
Past Medical History Breydon was diagnosed with scoliosis (left thoracic curve) 11 years ago, and was surgically treated to stabilize the spine. He reports feeling more of an imbalance between his left and right side each year. He was diagnosed with mild sleep apnea two years ago and currently uses a BiPAP machine to aid with breathing at night. Breydon was diagnosed with anxiety disorder 3 years ago, and occasionally experiences depressive symptoms. He underwent gastrectomy 3 years ago after several bouts of his flu became pneumonia.
Medications Fluoxetine (Prozac) - 40mg daily (anxiety management) Ibuprofen (Advil) - 200mg as needed, approx. once every 1-2 weeks (short-term pain relief) Emflaza (Deflazacourt) - 0.9mg/kg orally once per day (improve muscle strength and slow disease progression)
Current Interventions Breydon requires an assist of 1 to help with transfers to and from his wheelchair. He also requires assistance with eating, brushing his teeth, and with bathing. He currently receives this support at home from either his parents, older brother, and/or his PSW. He is unable to ambulate and uses an electric wheelchair for mobility. He utilizes a voice to text software when needed while completing school work on the computer.
Health Habits Breydon does not drink alcohol, smoke cigarettes or use recreational drugs.
Social History Breydon lives in a three bedroom condominium, with an elevator, on the tenth floor with his very supportive mother, father, and older brother. They also have a five year old Shih Tzu dog. His family has changed all the door knobs in the suite to lever-style handles. Breydon’s mother is a stay at home mom committed to helping Breydon get through his university degree. Prior to COVID-19, she drove him to his seminars and extracurriculars. His family prepares meals for him, and assists him with his activities of daily living. He also receives daily personal support assistance (PSW) from the Toronto Central LHIN twice a day for one hour each. His hobbies include learning to play the guitar at the community centre, bird watching, taking his dog out for walks down the valley, and public speaking at elementary schools/health seminars.
Current Functional History Breydon requires an assistance of 1 with both his basic and instrumental activities of daily living. As a child, Breydon’s upper extremity strength allowed him to perform independent anterior to posterior transfers, however due to decrease in U/E strength he is also dependent on an assist with transfers. He is unable to stand even on smooth surfaces, therefore is fully dependent on an electric wheelchair for mobility.Breydon’s last wheelchair assessment was conducted 3 years ago.
Family History No known family history of DMD. Breydon’s father has chronic hypertension and mother has asthma.
Chief Concern Breydon would like to complete his schoolwork (typing, writing) and play guitar at the same speed and with minimal error, like he used to be able to. He would like to complete daily fine motor tasks without the feeling of pain and discomfort.
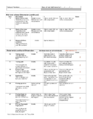
Patient Self Reported Measures:
The Patient Health Questionnaire (PHQ-9): The Patient Health Questionnaire (PHQ-9) is a useful tool for assessing mental health and quality of life in DMD patients, specifically in the adult population[4]. This questionnaire consists of 9 questions each are scored from 0-3, for a total score out of 27[4]. These questions were taken from a longer version of the questionnaire and condensed into this self-administered version. The higher a patient’s score, the greater their depression severity, which has been shown to correlate with decreased functional status and increased symptom-related issues in life.[4]
12- Item Short Form Survey (SF12): The SF-12 is a self-reported outcome measure assessing the impact of health on an individual's everyday life. It is often used as a quality of life measure.[5] Two summary scores are reported from the SF-12 – a mental component score (MCS-12) and a physical component score (PCS-12)[5]. The scores are reported as Z-scores. The United States population average PCS-12 and MCS-12 are both 50 points and the standard deviation is 10 points.[5]
Compared to the US population Breydon scored about 2 standard deviations below the average for physical component score and about 1 standard deviation below the average for mental component score. Detailed version of the patient’s SF-12 is attached below. The score on the PCS-12 is consistent with his functional dependence and the score on MCS12 is indicative of the decline in his mental health.
- Retrieved from https://orthopowertools.com/SF12 +https://uhs.fsu.edu/sites/g/files/upcbnu1651/files/docs/PHQ-9%20and%20GAD-7%20Form_a.pdf
Objective:
Postural Analysis: Breydon sits in a wheelchair with increased thoracic kyphosis. He leans towards his right side - likely due to his left thoracic scoliosis and right hand dominance. His right wrist and fingers are flexed in the resting position. He sits in a posterior pelvic tilt position. His right pelvis sits slightly higher than his left pelvis.
Balance: Breydon is able to maintain balance with eyes open and eyes closed and with decreased base of support while sitting in his wheelchair. He can weight shift laterally and anteriorly with internal perturbations, but has difficulty with axial rotation and reaching posteriorly. He cannot maintain his balance with external perturbations.
Range of Motion (ROM)
*WNL = Within Normal Limits
| Dermatomes | UE and LE equal bilaterally, sensation intact |
| Myotomes | UE and LE equal bilaterally |
| Muscle Tone | Further assessment of LE muscles indicated decreased muscle tone in quadriceps, hamstrings, soleus, and gastrocnemius bilaterally |
| Deep Tendon Reflexes | S1-S2 Achilles tendon = 2 (normal)
L3-L4 Patellar tendon = 1 (hyporeflexia) C6 Brachioradialis = 2 (normal) C6 Triceps = 1 (hyporeflexia) |
Performance of the Upper Limb (PUL 2.0)
The PUL 2.0 was developed specifically for DMD in order to assess the UE functioning in both ambulant and non-ambulant patients[6]. The PUL 2.0 was created to reflect disease progression and subsequent UE functional loss and weakness [6] This is a useful device for tracking disease progression and potential treatment efficacy, especially in non-ambulant patients such as Breydon. This measure addresses 3 domains of the UE: the high level shoulder, mid level elbow, and distal wrist and hand dimensions[6] A higher score indicates better UE functional ability, with a maximum total score of 42[6]
Breydon scored a total of 18/42 on the PUL, a decrease of 7 points since last year when he scored 25/42, indicating a significant reduction in UE functioning. When comparing Breydon’s current score to non-ambulant DMD patients of similar ages, Breydon scored in the lower range, which further indicates that Breydon’s UE functioning is slightly lower than expected at point in the disease progression and has declined significantly over the past year.
- Retrieved from: https://www.musculardystrophyuk.org/wp-content/uploads/2017/06/PUL2.0-Worksheet-V1.0-1st-May-2016.pdf
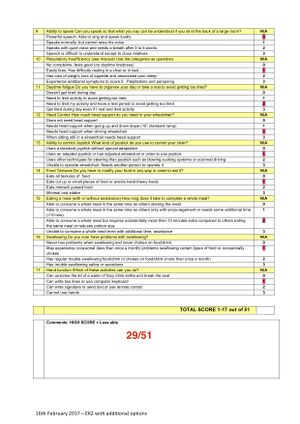
EK Scale
The Egen Klassifikation (EK) Scale measures functional ability in non-ambulatory patients with DMD.[7] It examines activities such as trunk mobility, transfers, wheelchair use, bed mobility, cough and general well-being[7]. The scale was updated in 2008 in order to capture functional ability specifically related to feeding, bulbar issues and distal hand function[7]. Also, items 1–10 were revised to update the scale in relation to updates in equipment and respiratory management[7]. Higher score= Decreased functional ability.[7]
Breydon scored 29/51 on the EK scale which is indicative of decline in functional ability. His score on the EK scale last year was 20/51, the current score indicates that his functional ability is progressively getting worse. Specifically his score on item 4,5,6,8,10,12 have decreased (detailed score is attached below).
MIP = -51 cmH2O MEP = 68cm H2O FVC = 2.2L (41% predicted) FEV1 = 1.96L (45% predicted) FEV1/FVC = 89% (normal/high)
When FVC is reduced below 50% of reference values (such as Breydon's case), respiratory assessments are supplemented with sleep studies once a year to assess hypercapnia during the night.
Clinical Impression
Breydon King is an 18-year old male, ambulating in a power wheelchair, presenting with a diagnosis of Duchenne Muscular Dystrophy. Breydon lives in an accessible house with his supportive family, and receives most of his care from his stay-at-home mother. His reports are of trouble with fine-motor tasks caused by increased bilateral symptoms of weakness, tightness, and pain in his hands. He is motivated to do well in school and enjoys playing guitar as a hobby, but is unable to do both of those things due to his discomfort. This has played a huge role in his recent spikes of anxiety. He is also passionate about sharing his DMD experience to motivate those around him and does so by giving motivational speeches around the city. However, he is lately experiencing shortness of breath and fatigue when delivering them. He may be at risk for a lung infection and further respiratory complications.
Problem List (ICF model)
Body Structure and Function
- Loss of mobility/range of motion in wrists and fingers
- Pain, weakness, and tightness in hands
- Increased thoracic kyphosis and recurrent progressive scoliosis
- Shortness of breath and fatigue (decreased FVC and FEV1)
Activity Limitations
- Loss of functional mobility when completing ADLs (grasping objects, using tools, putting on buttons) due to limitations in fine motor movements
Participation Restrictions
- Unable to type and write without pain therefore difficulty completing school work
- Trouble playing guitar because of tightness in fingers, especially his right hand (dominant hand)
- Unable to give speeches comfortably - shortness of breath and fatigue onset
Personal Factors
- Suffers from anxiety disorder
- Sedentary lifestyle - uses a wheelchair permanently
- Enrolled in a university program - likely to have a high workload
Intervention
Short Term Goals
- Breydon’s right hand ROM will increase by 5 degrees of extension at the MCP, PIP, and DIP joints of digits 2-5 and the MCP and CMC joints of the 1st digit by 4 weeks in order to prevent further contractures.
- Breydon’s right hand ROM in digit 1 will improve by 10 degrees of abduction at the CMC joint by 4 weeks
- Prevent further limitation in bilateral knee extension (more than 40 degree limitation) in four weeks
- The physiotherapist will perform a postural assessment (likely with an ergonomic assessment with the occupational therapist) and provide Breydon with improved seating/ cushioning and an orthotic brace to treat scoliosis by the end of the second visit.
Long Term Goals
- Breydon’s right hand ROM will improve since initial assessment by a total of 10 degrees of extension in digits 2-5 at the MCP, PIP, and DIP joints and the 1st digit at the MCP and CMC joints by week 8
- Breydon’s right hand ROM in digit 1 will improve by 20 degrees of abduction since initial assessment at the CMC joint by 8 weeks
- Maintain/improve knee extension bilaterally by 10 degrees extension from the initial assessment by the end of 8 weeks
- Breydon will be able to attend and participate as usual in a complete virtual guitar class with minimal/no breaks to rest his hands, by 8 weeks
- Breydon will be able to return to note taking manually on his keyboard as usual by the end of 8 weeks
- Bredyon will demonstrate normal ventilatory muscle recruitment with exertion by 6 weeks
- Breydon will present a normal breathing pattern ( 70% diaphragmatic, 30% lateral costal, decrease use of abdominals and accessory muscles,) by 6 weeks
- Breydon will be comfortable to participate in public speaking (motivational speaking at elementary schools) without the fear of fatigue/exhaustion by 10 weeks
Management Program
Respiratory Training
Breydon’s symptoms of shortness of breath and fatigue combined with pulmonary measures (FVC and FEV1 scores) indicate that he could benefit from respiratory training. This training will increase his lung volume, improve respiratory muscle strength and endurance, and reduce complications of a future lung infection. As a whole, reducing his work of breathing and enhancing breathing patterns will have a positive effect on his quality of life.
The diaphragm is a muscle that progressively becomes weaker than other inspiratory muscles in DMD, therefore it is important to add interventions to strengthen it so that it does not approach fatigue as easily. Breydon will be introduced to deep diaphragmatic breathing to target his diaphragm. Breath stacking is a simple deep diaphragmatic breathing technique that minimizes risk of chest infection by increasing lung expansion, which then helps mobilize secretions.[8] Breydon will benefit from this because of his restriction of chest movement (due to altered posture, scoliosis, and muscle weakness) and decreased lung capacity. Breydon will also begin ventilatory muscle training. Strength and endurance training of his ventilatory muscles will improve his respiratory muscle function and reduce shortness of breath and fatigue (performed using a device called POWERbreathe).

Respiratory Training Parameters
| Exercise | Frequency | Intensity | Duration | Type |
|---|---|---|---|---|
| Breath stacking | Twice a day | Take breaths in (2-4 times) until lungs are full | 3-5 cycles | Assisted using an ambu-bag |
| Ventilatory Muscle Strength Training | 3-4 times per week | 50-85% PImax | 8-12 reps, 2-3 sets | Targeted inspiratory muscle trainer (threshold device or electronic device) |
| Ventilatory Muscle Endurance Training | 3-5 times per week | 40-85% MSV (maximum sustainable ventilation) | >15 minutes (initiate at a tolerable level) | Targeted inspiratory muscle trainer (threshold device or electronic device) |
Symptoms of tightness in Breyden’s hands could indicate a risk of him developing a contracture, which is why stretching is crucial at this stage. Knowing that contractures are one of the major side effects of DMD [9], it is important to prevent or delay the progression of early symptoms into full development of a contracture.
The stretching program below should be done every day, at least twice a day but recommended 3 times per day for better results
- Each stretch is done bilaterally
- All of these stretches can be done independently
- Breydon’s family will be educated on assisting him when at home - passive stretching could better improve flexibility and range of motion
- Myofascial release and PNF stretching is added with physiotherapy sessions
Stretching Parameters
| Stretch | Parameter | Notes |
|---|---|---|
| Elbow flexor stretch | 2 reps x 30 second hold each, 2-3x/day, every day | Sit perpendicular to a wall, extend your arm back with your wrist on the wall. Extend your elbow fully. Hold the position, then repeat the stretch with your other arm.
Stretch to the point of slight discomfort and light pull but no pain |
| Wrist flexor stretch
(Praying hands) |
2 reps x 30 second hold each ,2-3x/day, every day | Stretch to the point of slight discomfort and light pull but no pain |
| Long finger flexor stretch | 2 reps x 30 second hold each, 2-3x/day, every day | Stretch to the point of slight discomfort and light pull but no pain |
| Forearm pronator stretch | 2 reps x 30 second hold each
2-3x/day, every day |
Bend one elbow next to your body and place the other hand on the back of your hand.
With help from the other hand, rotate your forearm to bring the palm of your hand facing the ceiling until you feel a stretch in the forearm. Stretch to the point of slight discomfort and light pull but no pain |
Postural Training
While scoliosis may have presented in Breyden before he was on a wheelchair, transitioning to permanently using a wheelchair can speed up muscular imbalances and the severity of the curvature in his spine. Breydon’s postural assessment indicates he has imbalances in a seated position by which he leans towards his right side more. It will be extremely difficult to reverse any changes in spinal curvature through physiotherapy alone, but the severity of scoliosis progression can be minimized through postural education and seating adjustments.
Breydon will receive education on how scoliosis may impact his posture and can put him at risk for other complications. He will be informed on maintaining an upright and balanced posture when sitting, and will be given cues that can help him stay mindful of it. Breydon mentioned that his last wheelchair assessment was 3 years ago. The time in between has likely brought on a change in his status and special needs, especially in regards to seating. Breydon will be referred to an occupational therapist who can conduct a wheelchair assessment and make seating adjustments according to his postural requirements. These modifications could include adding lateral support via thoracic pads to accommodate for scoliosis, or suggesting Breydon to wear a spinal jacket. The occupational therapist will ensure Breydon is supported with the right cushion and may even choose to use a specialist cushion to accommodate for pelvic asymmetry. Neck and thoracic support will also be assessed as Breydon presents with thoracic kyphosis that may have increased over the last 3 years.
Breydon has used ankle foot orthotics (AFOs) at night time to prevent plantar flexion contractures when he was able to ambulate without a wheelchair. Since he moved to permanent wheelchair ambulation, he solely uses lower profile-orthoses to control plantar varus. He says he has never needed orthotics for his upper extremity before but is willing to incorporate orthotic intervention if needed to preserve his hand function and minimize the risk of a contracture.
Breydon will now use a hand splint at night time to prevent the development of a contracture. This will maintain the length of long wrist and finger flexors and release some of the tightness in his hands. He is suggested to wear dynamic hand orthosis with the purpose of increasing motion by providing a stretch to the wrist. Figures 1 and 2 show examples of the types of splints that could improve function related to Breydon’s primary concerns. Figure 1 allows for more joint relaxation while placing low load passive stretch at the wrist to re-lengthen shortened tissue[10]. This works well in earlier stages of deformities. Figure 2 shows a splint that provides a stabilizing force through the hand and digits by placing the wrist and fingers in extension[11] . This splint places a greater load passive stretch in comparison to Figure 1. Breydon is recommended Figure 1 because it is the more comfortable option and is most likely to show benefits when paired with his daily stretches.
Outcome
Select outcome measures were re-performed 10 weeks after implementing Breydon’s intervention program in order to track his improvements as well as to refer back to in the future when tracking disease progression. Throughout the 10 weeks of intervention, Breydon performed foundational respiratory training concurrently with functional (strength and endurance) training. Upon reassessment, Breydon demonstrated proper breathing pattern and ventilatory muscle recruitment. His MIP increased from -50cm H2O to -62cm H2O, with no change in MEP, indicating improved ventilatory muscle strength in association with decreased fatigue when speaking. When assessing ROM, Breydon demonstrated improved right hand ROM in digits 2-5 through increasing extension by 10 degrees at the MCP, PIP, and DIP joints. He also improved right hand ROM in the 1st digit through increasing extension by 10 degrees at the MCP and CMC joints and increasing abduction by a total of 20 degrees at the CMC joint. Additionally, Breydon reports improved endurance when playing guitar, typing on the computer, and public speaking. Breydon also demonstrated improved performance on the PUL 2.0, indicating improved UE functioning, as well as the SF-12 and PHQ-9, indicating improved mental health and self-perceived quality of life.
The patient has met all of their goals and is ready to be discharged with the intention of scheduling ongoing physical therapy appointments every 4-6 months. During the last appointment the patient was provided with instructions to continue performing inspiratory muscle training and UE stretching exercises by following the same previous parameters. Various referrals were made to additional health care providers, including a Neurologist, Dietician, Physiatrist (for anxiety medication management), Occupational Therapist (to maximize independence and identify appropriate assistive devices/equipment), and Psychologist/Therapist (for mental health management).
Discussion
This case study explores the presentation of Breydon King, a fictitious 18 year old male diagnosed with Duchenne Muscular Dystrophy (DMD) from the age of 5 years old. Breydon presented to physiotherapy complaining of recent stiffness and difficulty opening his hands, restricting his ability to play guitar and type on his keyboard. He also has been experiencing shortness of breath during the day and throughout the night while sleeping. Through a thorough subjective and objective assessment, Breydon demonstrated significant declines over the last year, with various assessments conducted, including: PHQ-9, SF-12, AROM, MMT, neurological exam, PUL 2.0, EKScale, PFTs. Several interventions were employed in order to further prevent DMD progression, including respiratory training and stretching for contracture prevention, as well as to maximize the patient’s independence and participation in activities.
Management of DMD not only involves physical therapy rehabilitation to maximize functional independence, but requires an entire interdisciplinary team focused on patient-centred care. Various other healthcare providers should be included in patient treatment, including the patient’s primary-care physician and neurologist. Additional team members should be included to target maintaining and improving patient mental health, such as a physiatrist, psychotherapist, or social worker. Mental health conditions are prevalent in DMD populations, so at least one of these health care professionals should be included in their treatment team on a regular basis. Additionally, the physical therapist should work closely with an occupational therapist in order to maximize the patient’s functional independence.
Self Study Questions
- What is the inheritance pattern of the gene for DMD?
- X-linked dominant
- X-linked recessive
- Autosomal dominant
- Autosomal recessive
- A patient with DMD will typically lose independent ambulation during which of the following age ranges?
- 5-8 years old
- 8-11 years old
- 11-14 years old
- 14-18 years old
- Which of the following is not a common occurrence resulting from DMD?
- Limb contracture
- Scoliosis
- Respiratory/pulmonary function impairments
- Upper extremity paralysis
Answer Key: 1. b) 2. c) 3. d)
Additional Resources
Duchenne Muscular Dystrophy by WebMd
Dr. Phil Interview - Duchenne Muscular Dystrophy
References
[1]Duchenne Muscular Dystrophy, 2020, November 02. Rare Genetics and Disorders. Retrieved 22:45, May 13, 2021 from https://rarediseases.info.nih.gov/diseases/6291/duchenne-muscular-dystrophy
[2]Bushby, K, Finkel, R, Birnkrant, D, Case, L, Clemens, P, Cripe, L. Diagnosis and management of Duchenne muscular dystrophy, part 1: diagnosis and pharmacological and psychosocial management. The Lancet. 2010; 9(1): 77-93. Doi: https://doi.org/10.1016/S1474-4422(09)70271-6
[3]Birnkrant, D, Bushby, K, Bann, C, Alman, B, Apkon, S, Blackwell, A. Diagnosis and management of Duchenne muscular dystrophy, part 2: respiratory, cardiac, bone health, and orthopaedic management.. THe Lancet. 2018; 17 (4): 347-361. Doi: 10.1016/S1474-4422(18)30025-5
[4] Kroenke K, Spitzer RL, Williams JBW. The PHQ-9: Validity of a Brief Depression Severity Measure. Journal of General Internal Medicine. 2001Sep;16(9):606–13. doi: 10.1046/j.1525-1497.2001.016009606.x
[5]SF-12 Calculator. Orthopowertools. Retrieved from https://orthopowertools.com/SF12
[6] Han JJ, de Bie E, Nicorici A, Abresch RT, Anthonisen C, Bajcsy R, et al. Reachable workspace and performance of upper limb (PUL) in duchenne muscular dystrophy. Muscle Nerve. 2016Apr;53(4):545–54. doi: 10.1002/mus.24894
[7]Egen Klassifikation Scale Version 2 (EK2) [Internet]. NINDS. 2021 [cited 14 May 2021]. Available from: https://www.commondataelements.ninds.nih.gov/report-viewer/24329/Egen%20Klassifikation%20Scale%20Version%202%20(EK2)
[8]Breath Stacking. (2020, March 26). Physiopedia, . Retrieved 23:49, May 14, 2021 from https://physio-pedia.com/index.php?title=Breath_Stacking&redirect=no%3Futm_source%3Dphysiopedia&utm_medium=search&utm_campaign=ongoing_internal
[9] Duchenne Muscular Dystrophy. (2021, February 24). Physiopedia, . Retrieved 23:47, May 14, 2021 from https://www.physio-pedia.com/index.php?title=Duchenne_Muscular_Dystrophy&oldid=267589.
[10] Restorative hand. (n.d.). Retrieved from https://www.neurorehabdirectory.com/rehab-products/restorative-hand/
[11]Finger Extension Orthosis. (n.d.). Retrieved from https://www.neurorehabdirectory.com/rehab-products/finger-extension-orthosis/
- ↑ 1.0 1.1 https://rarediseases.info.nih.gov/diseases/6291/duchenne-muscular-dystrophy
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 2.6 2.7 2.8 2.9 https://doi.org/10.1016/S1474-4422(09)70271-6
- ↑ 3.0 3.1 https://doi.org/10.1016/s1474-4422(18)30025-5
- ↑ 4.0 4.1 4.2 4.3 https://link.springer.com/article/10.1046%2Fj.1525-1497.2001.016009606.x
- ↑ 5.0 5.1 5.2 5.3 https://orthopowertools.com/SF12
- ↑ 6.0 6.1 6.2 6.3 6.4 https://onlinelibrary.wiley.com/doi/abs/10.1002/mus.24894
- ↑ 7.0 7.1 7.2 7.3 7.4 7.5 https://www.commondataelements.ninds.nih.gov/report-viewer/24329/Egen%20Klassifikation%20Scale%20Version%202%20(EK2)
- ↑ 8.0 8.1 https://physio-pedia.com/index.php?title=Breath_Stacking&redirect=no%3Futm_source%3Dphysiopedia&utm_medium=search&utm_campaign=ongoing_internal
- ↑ 9.0 9.1 https://www.physio-pedia.com/index.php?title=Duchenne_Muscular_Dystrophy&oldid=267589.
- ↑ 10.0 10.1 10.2 https://www.neurorehabdirectory.com/rehab-products/restorative-hand/
- ↑ 11.0 11.1 11.2 https://www.neurorehabdirectory.com/rehab-products/finger-extension-orthosis/