Diastasis Recti Abdominis
Original Editor - Marianne Ryan
Top Contributors - Nicole Hills, Sivapriya Ramakrishnan, Lucinda hampton, Admin, Vidya Acharya, Victoria Geropoulos, Regan Haley, Rachael Lowe, Laura Ritchie, Marianne Ryan, Oyemi Sillo, Kim Jackson, Michelle Walsh, WikiSysop, Tarina van der Stockt and Claire Knott
Introduction[edit | edit source]
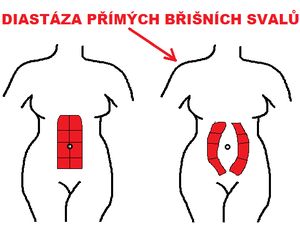
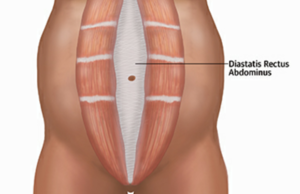
Diastasis recti (rectus diastasis) or divarication of the recti is a stretching of the linea alba with abnormal widening of the gap between the two medial sides of the rectus abdominis muscle (increased inter-recti distance).
The degree of widening needed for the diagnosis is controversial, with the degree of abdominal protrusion (rather than the degree of widening) often defining whether it is pathological. However, >15-25 mm is usually considered abnormal depending on gender, parity and if postpartum, time since birth. Additionally, the normal width varies depending on the level at which the linea alba is measured (narrower at the xiphoid and inferiorly approaching the pubic symphysis, and widest at the level of the umbilicus).[1]
The reason for variation in the Diastasis is attachment of the rectus muscles to the bony prominences like pubic symphysis and muscle attachments from internal and external oblique (lower), the upper and middle portion of the rectus muscle does not have any bony attachments and in a radiographic assessment the widest diastasis was felt above at the level of the umbilicus[2]
Epidemiology[edit | edit source]
Diastasis recti occurs primarily in newborns (see image 2) and pregnant women, although it can also occur in men and postpartum women.[1]
Etiology[edit | edit source]
Excessive inner-abdominal pressure causes diastasis recti. During pregnancy, the abdominal muscles and connective tissues are stretched out from the expanding uterus. They’re helped along by the pregnancy hormones relaxin and estrogen. Pushing during delivery can also lead to diastasis recti. Experiencing some abdominal separation during and following pregnancy is expected.
In the past, body mass index (BMI), weight gain during pregnancy, weight of the baby, and maternal age were considered risk factors. But a 2015 study found no connection between these factors and pregnant women being more or less likely to experience the condition.
Newborn babies are sometimes born with diastasis recti, especially if they’re premature. That’s because their abdominal muscles aren’t fully developed and connected. The condition usually corrects itself with time[3].
Pathology[edit | edit source]
1.Newborn
- rectus abdominis is not fully developed and may not be sealed together at midline
- more common in premature and black newborns
2.Pregnant or postpartum women
- growing uterus stretches the rectus abdominis
- diastasis is more common in multiparous women due to repeated stretching[1]
Diastasis Recti Abdominis and Pregnancy[edit | edit source]
During pregnancy, the linea alba (LA) softens due to hormones and the mechanical stretch resulting from the accommodation of the growing fetus.[4] Because of this, there will be a progressive increase in the width of the linea alba (or IRD) throughout the trimesters, with the highest incidence occurring in the third trimester.[4]
- A recent study by da Mota and colleagues (2015)[5] which studied 84 first-time pregnant women, found that 100% of these women had DRA by gestational week 35 when using a diagnostic criterion of 1.6cm at 2cm below the umbilicus. The prevalence decreased to 52.4% at 4-6 weeks postpartum and continued to decrease to 39% at 6 months.[5]
- While this agrees with other studies that have also found a decreased prevalence at 4 weeks[6][7] and 8 weeks postpartum,[4] a study by Coldron and colleagues (2008)[8] found that healing reached a plateau at 8 weeks postpartum and that IRD and rectus abdominis thickness and width did not return to the control values one year later.
Diagnosis[edit | edit source]
An adult is considered to have DRA when they present with an increased inter-recti distance (IRD), characterized by an observable and palpable separation between the two bellies of the rectus abdominis muscle.[9]
- There is no agreement as to the size of IRD considered to be pathological. The following parameters are given: 10 mm above the umbilicus, 27 mm at the umbilical ring and 9 mm below the umbilicus (below 45 years of age) and 15 mm, 27 mm and 14 mm respectively (above 45 years of age), above 2 cm, and in some older studies a less precise parameter — above the 2 — finger width when measured in a crook lying position. Another study shows a criterion to diagnosis Diastasis, an IRD of >2 mm at 3 cm below the umbilicus, >20 mm at the umbilicus, and >14 mm at 3 cm above the umbilicus is considered as Diastasis[10]. In the clinical practice, different measurement methods of IRD are applied.[11]
Physical Therapy Management[edit | edit source]
Our abdominal muscles play an important role in postural control, trunk and pelvic stability, trunk movement and respiration.[13]
- A study by Gilleard and Brown (1996) reported that the structural changes that occur to the abdominal muscles during pregnancy can limit abdominal muscle function, decreasing the ability of the abdominals to provide stability to the pelvis against resistance during pregnancy and up to 8 weeks postpartum.[6]
- In support of this, a study by Liaw and colleagues suggested that the size of IRD was negatively associated with abdominal muscle function.[14]
- A study by Hills and colleagues (2018) determined that women with DRA had a lower capacity to generate trunk rotation torque and perform sit-ups (supported by a negative correlation between IRD and trunk rotation peak torque generating capacity and sit-up test scores).[15]
- Some studies have implicated weak abdominal muscles in causing abdominal[16] and lumbo-pelvic pain and dysfunction during pregnancy.[17] [18]
It has also been hypothesized that weak abdominal muscles can result in ineffective pelvic floor muscle (PFM) contraction.[17]
Beginning exercises prenatally may help to maintain the tone and control over abdominal musculature to decrease some stress of the linea alba.[19]
Early literature suggests that functional capacity of abdominal musculature may be compromised due to a change in the muscle’s line of action.[6] Since then, Chiarello and colleagues (2005)[20] found that the occurrence and size of DRA is greater in pregnant women who do not exercise and that, since the abdominals play an important functional role in exercise, women must be screened for the presence of DRA. More recent evidence supports deep core stability-strengthening 3 times a week for 8 weeks, in addition to bracing, to improve inter-recti separation and quality of life as measured by the Physical Functioning Scale (PF10).[21] The exercises included diaphragmatic breathing, pelvic floor contraction, plank, isometric abdominal contractions, and traditional abdominal exercises.[21] Lee and Hodges (2016)[22] proposed that narrowing the IRD may not be optimal and that pre-activation of TrA can increase the tension and decrease the distortion of the linea alba, which will allow for the force to be transmitted across the midline. However, Gluppe and colleagues (2018)[23] found that a supervised exercise class once a week for 16 weeks, in addition to daily home training, did not reduce the prevalence of DRA at 6 months postpartum. The exercises focused on strengthening the pelvic floor, but also relaxation and stretching, as well as strengthening of the abdominals, back, arms, and thighs.[23]
Patient Education[edit | edit source]
It is important to educate our patients on diastasis recti abdominis during and after pregnancy in order to manage patient expectations, limit fear and anxiety, and best prepare our patients for the pregnancy and birth-related changes their bodies will experience. Mota and colleagues (2015) have suggested that 100% of women will exhibit an increased IRD in the third trimester,[5] characterized as DRA. This statistic, as well as DRA language such as “gap” and “separation”, can be extremely fear-inducing and has the potential of increasing stress and anxiety in our patients, which can have negative physiological and psychological effects on both mom and baby.[24] Therefore, it is important to remind patients that are trying to get pregnant, and those who already are, that women’s bodies have been designed to grow and expand in order to accommodate a growing fetus. Hormonal changes in pregnancy result in increased laxity and softening of connective tissue,[25] resulting in the widening of the LA to create space for the baby. Not only is this process a natural part of pregnancy, it is also necessary in order for the baby to have adequate room to grow.
In the postpartum phase, patients and PT’s will often direct focus to the management of DRA in order to optimize function. The definition of DRA describes a pathological increase in the distance between the two rectus abdominis muscles, or an increase in the IRD, due to a stretching, thinning, and/or widening of the LA. Therefore, decreasing the IRD appears to be the most obvious rehabilitation objective or management strategy,[22] and is widely supported by clinicians based on the assumption that restoring the alignment of the rectus abdominis muscles, by decreasing the IRD, will also restore the function of these muscles.[26] However, Lee and Hodges (2016) suggest that LA tension, as opposed to a decrease in IRD, may be more important to support abdominal contents and to effectively transfer force between opposing abdominal muscles.[22] In patients with DRA, the LA is distorted and slackened (reduction of tension), when the IRD is reduced. Reducing LA tension could result in a bulging or distorted LA while pre-activation of the TrA before the rectus abdominis muscles results in an increase in IRD but also an increase in LA tension.[22] It is important to educate patients on the potential that increasing LA tension could be a more effective management and rehabilitation plan than closing the “gap” and decreasing the IRD as it “is unlikely to optimally support the abdominal contents (potentially producing less desirable cosmetic appearance), and could induce less effective mechanical function”.[22]
The video below by a Canadian physiotherapist uses a great analogy to explain the concept of diastasis recti abdominis.
Cosmetic appearance can be affected by DRA due to extension and loss of tension of the LA causing a bulging of the abdominal wall.[28] This bulging, “tenting”, or “coning” is commonly referred to as “mummy tummy” and can be seen when women are going from lying down to sitting, when exercising, or even at rest. An increased IRD is positively associated with worse body image in women with DRA, and therefore, it may be indicated to include body image and body satisfaction outcome measures and management when treating pregnant and postpartum women with DRA.[29]
There is a growing consensus suggesting that DRA is not necessarily a condition physiotherapists and patients need to prevent and treat, but in fact a very normal part of pregnancy that women’s bodies are naturally designed to do to create space for the growing baby. However, there are multiple techniques physiotherapists can prescribe to their pregnant and postpartum patients to help maintain and optimize strength and function. Pelvic floor physiotherapists are qualified to develop exercise and movement strategies that are warranted “to promote optimal physical function through the pregnancy, limit potential functional impairment and prepare for birth” and manage postpartum recovery.[30] Furthermore, it is crucial for physiotherapists to discuss patient concerns, expectations, and goals in order to create individualized and targeted management and treatment plans. Individualized rehabilitation for DRA and any postpartum concerns is a necessity,[22] and taking a full and well-round subjective history and asking questions about expected outcomes and goals, can help physiotherapists create individualized management and rehabilitation plans for each patient.
Common Postpartum Exercises[edit | edit source]
Exercises for the Inner Unit:[edit | edit source]
The consensus study conducted by Dufour and colleagues (2019) emphasized the use of inner unit exercises during the prenatal, early postpartum and late postpartum periods for the management of DRA.[30]This is consistent with a study by Mesquita and colleagues (1999), who suggested inner unit exercises should be performed immediately post-delivery.[31] Similarly, a more recent study by Thabet and Alshehri (2019) concluded that a deep core stability exercise program (i.e. diaphragmatic breathing, pelvic floor contraction, plank and isometric abdominal contraction) was effective in treating DRA and improving quality of life postpartum.[21]
The inner unit muscles, which include the transverse abdominis, multifidus, diaphragm and pelvic floor muscles, provide stabilization to the core. When commencing inner unit exercises, emphasis should first be placed on achieving controlled isolation of each muscle in the unit, followed by controlled co-activation of the inner unit.[30] While trying to achieve control of the inner unit in the prenatal, early postpartum and late postpartum periods, it is important to remember that exercises that engage the superficial abdominal muscles should be avoided (i.e. sit-ups).[30] Once isolation of the inner unit is achieved, exercises should be progressed to include the outer unit (one such method is described below), as well as, exercises that are more functionally based.[30]
- Step 1: Tupler technique. [Isolated Contraction of Transverse abdominis only][32]
- Step 2: Step 1+ Posterior pelvic tilt [33]
- Step 3: Step 2+ approximating both sides of the abdomen to the center
- Step 4: Step 4+ lifting the head up[30]
Transverse Abdominis (TA):
Patient Position: First, have the individual position themselves in supine crook-lying or in side-lying with a neutral spine. Once in the proper position, instruct the patient to palpate their TA muscle using their index and middle fingers just medial to their front pelvic bones (or ASIS).[34]
Technique: Following this, have the individual draw in their abdomen and contract their TA muscle while preforming relaxed breathing. The following cues can be used to isolate the transverse abdominis: “imagine you are pulling your pelvic bones together in a straight line” or “bring your belly button towards your spine”.[34] The individual should hold the contraction for 3-5 seconds while they exhale and relax their TA as they inhale.[34] The individual can perform 3 sets of 10 repetitions, 3-4 times per week.[34] Ensure there is no compensatory strategies such as posterior tilting of the pelvis, depression of the ribcage, breath-holding or bulging of the abdomen.[34]
Multifidus:
Patient Position: With the individual positioned in supine or side-lying with a neutral spine, have them imagine a line that connects their left and right sides of their posterior pelvis.[34]
Technique: Next, tell the individual to contract their multifidus to try draw together their left and right halves along this line.[34] The individual should practice relaxed breathing, ensuring to recruit their multifidus during exhalation. The contraction should be held for 3-5 seconds, 3 sets of 10, 3-4 times per week.[34] No anterior tilting of the pelvis, flexion of the hips and movement of the thorax and lower back should be observed.[34]
Pelvic Floor Muscle (PFM):
Patient Position: Supine, crook-lying or side-lying.
Technique: Instruct the individual to imagine closing off their urethra as if they are trying to stop the flow of urine.[34] Alternatively, have the individual imagine that they are lifting their anus up towards their pubic bone.[34] As suggested by Diane Lee (2019), an alternative position for isolating the PFM is to sit on a small, softball as the ball can help provide feedback to your brain.[34] Notice what happens with a deep inhalation and on exhalation. Ideally, one should feel the PFM moving down and into the ball on inhalation and moving up away from the ball although retaining contact with the ball on exhalation. Now start by taking a 3-dimensional breath, i.e., expanding the front, back, and sides of the lower rib cage on the inhale and relaxing on the exhale. Note that one does not force the breath during exhalation. When contracting PFM, a deep connection/contraction of the lower and middle fibres of TA should be felt during exhale. One should NOT feel tightening of buttocks, legs rotate out, or movement of spine or pelvis. If the individual feels bulging of the abdomen, butt gripping, or spinal movements, they may not be correctly contracting the pelvic floor muscles. A correct contraction should generate a very gentle tension deep in the abdomen (often very hard to feel initially). The contraction should be held for 3-5 seconds, 3 sets of 10, 3-4 times per week.[34]
EMG studies and ultrasound imaging demonstrates the synergistic relationship between the PFM and diaphragm, TA, and obliques internis (OI)during respiration. The thoracic diaphragm contracts and moves caudally to draw air into the lungs upon inhalation. And at the same time, the anterolateral abdominal wall distends slightly to make room for the displaced abdominal viscera the pelvic floor relaxes caudally. Whereas on exhalation, PFM and anterolateral abdominal muscles (TA and OI) contract as or slightly before the thoracic diaphragm relaxes to transfer IAP from the abdomen to the thorax.[35][36]
Diaphragm:
During pregnancy, the diaphragm is displaced upwards approx. 5 cm to accommodate for the increasing size of the uterus.[37] As a result, the work placed on the diaphragm increases and compensatory strategies such as increased accessory muscle recruitment are adopted. [37]
Given the changes to the diaphragm during pregnancy, it is recommended that during the prenatal, early post-partum and late-postpartum periods, a tension-free diaphragmatic breathing pattern should be adopted.[30] This means that during inhalation, the diaphragm should descend downward and the lateral costal rib cage should expand outward.[30]
To facilitate this breathing pattern, the following breathing exercises can be practiced:
- Diaphragmatic Breathing:
- Position: Supine position with their knees bent. A pillow can be placed under the knees for support.
- Technique: Have the individual place one hand on their chest and one hand over the apex (highest point) of the abdomen. Instruct the individual to breathe into their hand with short, shallow breaths. The individual should only feel their hand rise at their abdomen and not at their chest. Encourage inhalation through the nose and exhalation through the mouth. Alternatively, instructing the individual to “sniff” into their hand on their abdomen is a cue that can be used to encourage diaphragmatic breathing. The individual can practice this technique 5-10 minutes at a time, 1-4 times per day, gradually building up their tolerance.[38]
- Lateral Costal Breathing:
- Position: Supine position with their knees bent. A pillow can be placed under the knees for support.
- Technique: Have the individual place their hands on the sides of their ribcage. Instruct the individual to take a deep breath through their nose and expand their ribcage into their hands. After inhalation, have the individual exhale slowly through their mouth. The individual can practice this technique 5-10 minutes at a time, 1-4x/ day, gradually building up their tolerance.
Throughout postpartum recovery and pregnancy-related DRA management, Physiotherapists should encourage modifications to activities, as well as static and dynamic postures, to reduced repeated increases in IAP.[30] For example, rolling onto one side first prior to getting up out of bed, using a squatty potty to optimize the angle of the rectum and reduce straining.[41] Once isolated, controlled activation of each muscle of the inner unit is achieved, progressions can begin to focus on co-activation of the inner unit as well as more functionally oriented exercises[30] such as isometric contractions and rotational movements. Furthermore, postpartum patients should avoid high-impact exercises until 9-12months,[42] and should avoid all exercises in which the continence mechanism cannot be maintained.[30]
Body Mechanics[edit | edit source]
During the prenatal, intrapartum, early and late postpartum periods, it is important to avoid movements that create repeated increases in intra-abdominal pressure.[30] This recommendation is supported by the findings of Sperstad and colleagues whereby pregnant women who performed heavy lifting more than 20 times per week were at an increased risk of developing DRA.[43]
Education on posture and body mechanics should include aspects such as: lifting/carrying objects, rolling to the side to get up while using the arm to push up, straining on the toilet, maintenance of a neutral spine alignment with both dynamic and static postures and placement of one foot higher than the other when standing for prolonged periods of time.[30][44]
Commonly taught techniques:
- Bed Mobility: To get out of bed, the individual should first roll to their side and then push off the edge of the bed using their top arm.[45]
- Lifting: Whether it involves lifting a light object or heavy object, effective body mechanics should always be applied.[45] To do so, instruct the individual to get as close as possible to the object they are lifting.[45] The individual should inhale as they grasp onto the object while widening their stance with bent knees and a neutral spine.[45] To lift the object, the individual should straighten their knees while exhaling.[45] Lastly, the individual should ensure their spine is kept in neutral as they bend their knees to release the object onto its resting place.[45]
Postural Awareness[edit | edit source]
After pregnancy, some women tend to stand with and an exaggerated anterior pelvic tilt and with their pelvis pushed forward. In order to stand up against gravity, their bodies typically develop areas of rigidity in the upper lumbar and the lower thoracic area along with the buttock muscles. Diane Lee refers to this as “back clenching and buttock griping behaviour.” Manual therapy and relaxation exercises may be indicated before initiating strengthening exercises.
Abdominal Supports[edit | edit source]
Although researchers suggest that external support, such as abdominal binding, should not be recommended as a primary rehabilitation technique for DRA to avoid reliance, there may be benefits to its use, coupled with exercise, in specific cases.[30] For example, abdominal binding can provide additional support and comfort, and can help with cueing and proprioception for women in the early postpartum period and can increase patients’ confidence when attempting to activate or contract the abdominal muscles. A randomized control trial by Cheifetz and colleagues (2010), suggests that abdominal support is effective at managing distress and improving patients’ experience following a major abdominal surgery, which could be relevant for patients with DRA recovering from a caesarean delivery.[50]
Select clinical experts have suggested that non-elastic binders result in a greater likelihood of an increase in intravesical pressure (IVP)[42], or pressure of urine in the bladder.[51] Therefore, it is important to note that if abdominal binders are going to be prescribed or suggested, elastic binders are more likely to promote recovery than non-elastic binders.[42] Additionally, elastic wraps allow for greater movement and are less likely to restrict breathing.[42]
If an abdominal wrap or binding is going to be used, it should be initiated immediately postpartum and worn for support for approximately 8 weeks, or until the patient has the ability to generate tension in the inner unit during activity. External support should always be used in conjunction with inner unit activation and exercises to regain control and co-activation of the inner unit muscles. Additionally, abdominal bindings should always be wrapped from the bottom up to avoid an increase in pressure on the uterus and pelvic organs, which can cause downward descent or prolapse of the pelvic organs. The abdominal wrap should offer light compression or gentle hugging as too much compression can increase IAP.[42]
References[edit | edit source]
- ↑ 1.0 1.1 1.2 Radiopedia Diastasis Recti Available from: https://radiopaedia.org/articles/diastasis-recti (accessed 4.4.2021)
- ↑ Corvino A, De Rosa D, Sbordone C, Nunziata A, Corvino F, Varelli C, Catalano O. Diastasis of rectus abdominis muscles: patterns of anatomical variation as demonstrated by ultrasound. Polish Journal of Radiology. 2019 Dec 15;84:542-8.
- ↑ Healthline DR Available from:https://www.healthline.com/health/diastasis-recti#causes (accessed 4.4.2021)
- ↑ 4.0 4.1 4.2 Boissonnault JS, Blaschak MJ. Incidence of diastasis recti abdominis during the childbearing year. Physical therapy. 1988 Jul 1;68(7):1082-6.
- ↑ 5.0 5.1 5.2 Mota PG, Pascoal AG, Carita AI, Bø K. Prevalence and risk factors of diastasis recti abdominis from late pregnancy to 6 months postpartum, and relationship with lumbo-pelvic pain. Manual therapy. 2015 Feb 1;20(1):200-5.
- ↑ 6.0 6.1 6.2 Gilleard WL, Brown JM. Structure and function of the abdominal muscles in primigravid subjects during pregnancy and the immediate postbirth period. Physical therapy. 1996 Jul 1;76(7):750-62.
- ↑ Hsia M, Jones S. Natural resolution of rectus abdominis diastasis. Two single case studies. Aust J Physiother. 2000 Jan 1;46(4):301-7.
- ↑ Coldron Y, Stokes MJ, Newham DJ, Cook K. Postpartum characteristics of rectus abdominis on ultrasound imaging. Manual therapy. 2008 Apr 1;13(2):112-21.
- ↑ Keshwani N, Hills N, McLean L. Inter-rectus distance measurement using ultrasound imaging: does the rater matter?. Physiotherapy Canada. 2016;68(3):223-9.
- ↑ Qu E, Wu J, Zhang M, Wu L, Zhang T, Xu J, Zhang X. The ultrasound diagnostic criteria for diastasis recti and its correlation with pelvic floor dysfunction in early postpartum women. Quantitative Imaging in Medicine and Surgery. 2021 Feb;11(2):706.
- ↑ Michalska A, Rokita W, Wolder D, Pogorzelska J, Kaczmarczyk K. Diastasis recti abdominis—a review of treatment methods. Ginekologia polska. 2018;89(2):97-101.Available from: https://journals.viamedica.pl/ginekologia_polska/article/view/GP.a2018.0016/43304(accessed 4.4.2021)
- ↑ Learn with Diane Lee. Linea alba screen DRA with Diane Lee. Available from: https://www.youtube.com/watch?v=06o8Z54l-40 [last accessed 22/06/2018]
- ↑ Benjamin DR, Van de Water AT, Peiris CL. Effects of exercise on diastasis of the rectus abdominis muscle in the antenatal and postnatal periods: a systematic review. Physiotherapy. 2014 Mar 1;100(1):1-8.
- ↑ Liaw LJ, Hsu MJ, Liao CF, Liu MF, Hsu AT. The relationships between inter-recti distance measured by ultrasound imaging and abdominal muscle function in postpartum women: a 6-month follow-up study. journal of orthopaedic & sports physical therapy. 2011 Jun;41(6):435-43
- ↑ Hills NF, Graham RB, McLean L. Comparison of trunk muscle function between women with and without diastasis recti abdominis at 1 year postpartum. Physical therapy. 2018 Oct 1;98(10):891-901.
- ↑ Fast AV, Weiss L, Ducommun EJ, Medina EV, Butler JG. Low-back pain in pregnancy. Abdominal muscles, sit-up performance, and back pain. Spine. 1990 Jan;15(1):28-30.
- ↑ 17.0 17.1 Spitznagle TM, Leong FC, Van Dillen LR. Prevalence of diastasis recti abdominis in a urogynecological patient population. International Urogynecology Journal. 2007 Mar 1;18(3):321-8.
- ↑ Parker MA, Millar LA, Dugan SA. Diastasis rectus abdominis and lumbo-pelvic pain and dysfunction-are they related?. Journal of Women’s Health Physical Therapy. 2009 Jul 1;33(2):15-22.
- ↑ Zappile-Lucis M. Quality of life measurements and physical therapy management of a female diagnosed with diastasis recti abdominis. Journal of Women’s Health Physical Therapy. 2009 Apr 1;33(1):22.
- ↑ Chiarello CM, Falzone LA, McCaslin KE, Patel MN, Ulery KR. The effects of an exercise program on diastasis recti abdominis in pregnant women. Journal of Women’s Health Physical Therapy. 2005 Apr 1;29(1):11-6.
- ↑ 21.0 21.1 21.2 Thabet AA, Alshehri MA. Efficacy of deep core stability exercise program in postpartum women with diastasis recti abdominis: a randomised controlled trial. Journal of musculoskeletal & neuronal interactions. 2019;19(1):62.
- ↑ 22.0 22.1 22.2 22.3 22.4 22.5 Lee D, Hodges PW. Behavior of the linea alba during a curl-up task in diastasis rectus abdominis: an observational study. journal of orthopaedic & sports physical therapy. 2016 Jul;46(7):580-9.
- ↑ 23.0 23.1 Gluppe SL, Hilde G, Tennfjord MK, Engh ME, Bø K. Effect of a postpartum training program on the prevalence of diastasis recti abdominis in postpartum primiparous women: a randomized controlled trial. Physical therapy. 2018 Apr 1;98(4):260-8.
- ↑ Glynn LM, Schetter CD, Hobel CJ, Sandman CA. Pattern of perceived stress and anxiety in pregnancy predicts preterm birth. Health Psychology. 2008;27(1):43–51.
- ↑ Benjamin DR, Van de Water AT, Peiris CL. Effects of exercise on diastasis of the rectus abdominis muscle in the antenatal and postnatal periods: a systematic review. Physiotherapy. 2014 Mar 1;100(1):1-8.
- ↑ Oneal RM, Mulka JP, Shapiro P, Hing D, Cavaliere C. Wide Abdominal Rectus Plication Abdominoplasty for the Treatment of Chronic Intractable Low Back Pain. Plastic and Reconstructive Surgery. 2011;127(1):225–31.
- ↑ Phit Physiotherapy. DRA: Being (banana) split up the middle, a fresh (produce) perspective. Available from: https://www.youtube.com/watch?v=rVxAUOkb3M4[last accessed 22/06/2018]
- ↑ Michalska A, Rokita W, Wolder D, Pogorzelska J, Kaczmarczyk K. Diastasis recti abdominis — a review of treatment methods. Ginekologia Polska. 2018;89(2):97–101.
- ↑ Keshwani N, Mathur S, Mclean L. Relationship Between Interrectus Distance and Symptom Severity in Women With Diastasis Recti Abdominis in the Early Postpartum Period. Physical Therapy. 2017 Apr;98(3):182–90.
- ↑ 30.00 30.01 30.02 30.03 30.04 30.05 30.06 30.07 30.08 30.09 30.10 30.11 30.12 30.13 Dufour S, Bernard S, Murray-Davis B, Graham N. Establishing expert-based recommendations for the conservative management of pregnancy-related diastasis rectus abdominis: A Delphi consensus study. Journal of Women’s Health Physical Therapy. 2019 Apr 1;43(2):73-81.
- ↑ Mesquita LA, Machado AV, Andrade AV. Physiotherapy for reduction of diastasis of the recti abdominis muscles in the postpartum period. Revista Brasileira de Ginecologia e Obstetrícia. 1999 Jun 1;21(5):267-72.
- ↑ Tupler Technique [Internet]. YouTube. 2018 [cited 2022Nov25]. Available from: https://youtu.be/8Uo5l85Zuf4?t=168
- ↑ Posterior Pelvic Tilt [Internet]. Orthoindy.com. 2016 [cited 2022Nov25]. Available from: https://youtu.be/-AWtsAzHBp4
- ↑ 34.00 34.01 34.02 34.03 34.04 34.05 34.06 34.07 34.08 34.09 34.10 34.11 34.12 Core training vs. strengthening: Core Training vs. Strengthening [Internet]. Diane Lee & Associates. 2019 [cited 2020Jun8]. Available from: https://dianeleephysio.com/education/core-training-vs-strengthening/
- ↑ Gordon KE, Reed O. The role of the pelvic floor in respiration: a multidisciplinary literature review. Journal of Voice. 2020 Mar 1;34(2):243-9.
- ↑ Talasz H, Kofler M, Kalchschmid E, Pretterklieber M, Lechleitner M. Breathing with the pelvic floor? Correlation of pelvic floor muscle function and expiratory flows in healthy young nulliparous women. International urogynecology journal. 2010 Apr;21(4):475-81.
- ↑ 37.0 37.1 LoMauro A, Aliverti A. Respiratory physiology of pregnancy: physiology masterclass. Breathe. 2015 Dec 1;11(4):297-301.
- ↑ Wong C. How to Do Belly Breathing Technique [Internet]. Verywell Health. Verywell Health; 2020 [cited 2020Jun8]. Available from: https://www.verywellhealth.com/how-to-breathe-with-your-belly-89853
- ↑ jivan sharma. Diaphragmatic Breathing Technique. Available from: http://www.youtube.com/watch?v=0Ua9bOsZTYg [last accessed 11/6/2020]
- ↑ BlueJay Mobile Health. Lateral Costal Breathing | Pelvic Physical Therapy. Available from: http://www.youtube.com/watch?v=SRj425_jark [last accessed 11/6/2020]
- ↑ Modi RM, Hinton A, Pinkhas D, Groce R, Meyer MM, Balasubramanian G, et al. Implementation of a Defecation Posture Modification Device. Journal of Clinical Gastroenterology. 2019;53(3):216–9.
- ↑ 42.0 42.1 42.2 42.3 42.4 Di Paolo J. Diastasis Rectus Abdominis: Moving the evidence to practice-based solutions. PowerPoint Presentation at: American Physical Therapy Association – Combined Sections Meeting; 2019 Jan 24; Washington, DC.
- ↑ Sperstad JB, Tennfjord MK, Hilde G, Ellström-Engh M, Bø K. Diastasis recti abdominis during pregnancy and 12 months after childbirth: prevalence, risk factors and report of lumbopelvic pain. Br J Sports Med. 2016 Jun 20:bjsports-2016.
- ↑ Davis DC. The discomforts of pregnancy. Journal of Obstetric, Gynecologic, & Neonatal Nursing. 1996 Jan;25(1):73-81.
- ↑ 45.0 45.1 45.2 45.3 45.4 45.5 Correct Body Mechanics and Posture for Pregnancy [Internet]. Correct Body Mechanics and Posture for Pregnancy | Lovelace Health System in New Mexico. [cited 2020Jun11]. Available from: https://lovelace.com/news/blog/correct-body-mechanics-and-posture-pregnancy
- ↑ LovelaceHealthSystem. Body Mechanics & Posture for Pregnancy: Bed Mobility. Available from: https://www.youtube.com/watch?v=nibeN8lE6rk&feature=emb_logo [last accessed 11/6/2020]
- ↑ LovelaceHealthSystem. Body Mechanics & Posture for Pregnancy: Lifting. Available from: http://www.youtube.com/watch?v=9hePGxsC6nw&feature=emb_logo [last accessed 11/6/2020]
- ↑ Diane Lee's Integrated Systems Model for Physiotherapy in Womens' Health. Available from:https://www.youtube.com/watch?v=5oslM6Pe9AU&t=1844s [last accessed 22/6/2018]
- ↑ Diane Lee. Conference Presentations Diane Lee and Associates in Physiotherapy. Available from: https://www.youtube.com/watch?v=mHY6CSSosNE&t=10s[last accessed 22/6/2018]
- ↑ Cheifetz O, Lucy SD, Overend TJ, Crowe J. The Effect of Abdominal Support on Functional Outcomes in Patients Following Major Abdominal Surgery: A Randomized Controlled Trial. Physiotherapy Canada. 2010;62(3):242–53.
- ↑ Claridge M. Intravesical Pressure And Outflow Resistance During Micturition. Acta Neurologica Scandinavica. 2009;42(S20):95–104.