Compassion Fatigue
Original Editor - Amanda Ager
Top Contributors - Amanda Ager, Tarina van der Stockt, Naomi O'Reilly, Lucinda hampton, Kim Jackson, WikiSysop, Rucha Gadgil and Nicole Hills
Introduction[edit | edit source]
We become rehabilitation professionals because we have compassion and we are interested in positively influencing a person's quality of life. We give of ourselves so that we may help others obtain optimal health. This can also lead to "clinical burnout" or "compassion fatigue". There are many terms to describe this phenomenon, including:
- Compassion Fatigue
- Secondary Traumatic Stress Syndrome (STSS)
- Clinical Burnout
- Burnout Syndrome
- Moral Distress
- Occupational Burnout.
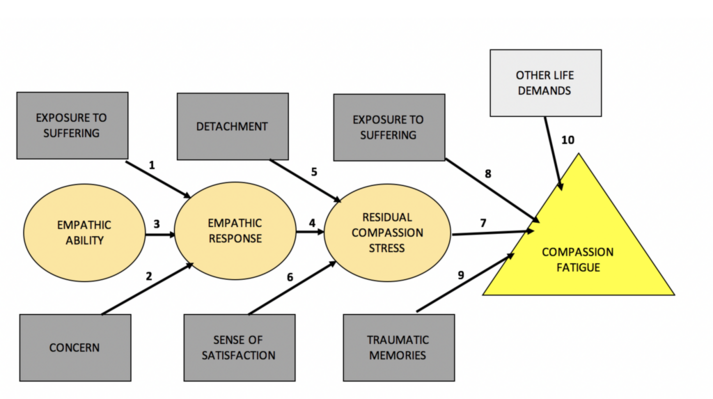
"Burnout" can be best understood as a syndrome that includes emotional exhaustion, depersonalization, and a reduced sense of personal accomplishment. Symptoms of burnout include mental and physical exhaustion, accompanied by psychosomatic disorders and emotional problems. Burnout occurs most often in people employed in occupations requiring work with people (human services and medical services) as a result of coping with stress and experience numerous failures at work. Moreover, compassion fatigue denotes a state of emotional exhaustion that can occur as a result of intensive empathic involvement with people who are in distress.[1]
- Clinical burnout can occur when a rehabilitation professional is exposed to chronic, job-related stressors.
- For clarity sake, the term Compassion Fatigue (CF), will be used hence forth.
Epidemiology[edit | edit source]
Compassion fatigue may start at any stage during a rehabilitation professionals career, irrespective of the work situation.[2] Although controversial at the moment, women seem to have a higher level of professional burnout than men.[3] It has also been noted that more experienced rehabilitation professionals may be at greater risk for the development of Compassion Fatigue.
Clinical Presentation[edit | edit source]
It is important to distinguish the difference between CF, workplace exhaustion and general depression. The main distinguishing factor with workplace exhaustion, is that these problems disappear outside work. Although there are blurred lines between Compassion Fatigue and depression, we can understand depression (major depressive disorder) as; a common and serious medical illness that negatively affects how you feel, the way you think and how you act. Depression causes feelings of sadness and/or a loss of interest in activities once enjoyed, both at work and at home. Whereas, Compassion Fatigue denotes a state of emotional exhaustion that can occur as a result of intensive empathic involvement with people who are in distress.[1] Rehabilitation professionals experiencing Compassion Fatigue reported that they struggle to show compassion to their patients while dealing with job related stressors. [2]
Signs and Symptoms of Burnout[edit | edit source]
- Work Addiction
- Excessive Stress
- Fatigue
- Insomnia
- A negative spillover into personal relationships or home life
- Depression
- Anxiety
- Alcohol or Substance Abuse
- Heart Disease;
- High Cholesterol
- Type 2 Diabetes (especially in women)
- Stroke
- Obesity
- Vulnerability to Illnesses
- Feeling like you are involved in workplace bullying.
It is possible that older and more experienced rehabilitation professionals hold positions of greater responsibility, in which demands are more difficult to meet. In these situations it can become increasingly difficult to maintain feelings of personal accomplishment.[4]
Burnout among health care providers has also been linked to wider organizational factors, such as increased workload, time pressures, safety issues, role ambiguity, lack of supervision, and reduced resources.[5]
Regardless of how you are feeling, you should be aware of the outlined signs and symptoms and consult a professional sooner, rather than later.
Management / Interventions[edit | edit source]
There is no "quick fix" for managing compassion fatigue. The most important action is to identify the key personal stressors. Everyone's situation is different and therefore the "triggers" will most certainly be different. The examination of your work-life balance will certainly be at the core of addressing how you are feeling. The first step is recognizing that there is an issue, followed by seeking the appropriate level of support or change in your life.
How to Reduce Burnout[edit | edit source]
- Identify and manage the source of stress to the best of your ability.
- Manage your expectations about what you can realistically accomplish in a day (it will still be there tomorrow!).
- Evaluate your options
- Adjust your thoughts and your attitudes
- Seek support as needed (speak to your boss, your colleagues, and your social support);
- Take care of yourself (eat well, sleep well and exercise!);
- Speak to a professional who can help you develop a personalized strategy for dealing with your CF.
The early identification of this emotional state is needed in order to prevent the depersonalization of the provider-patient relationship.[6] Prevention and treatment are essentially parallel efforts, which include:
- Greater job control by the individual worker
- Group meetings
- Better communication on all levels (co-workers, subordinates, supervisors)
- Better recognition of individual worth
- Job redesign
- Flexible work hours
- Full orientation to job requirements
- Available employee assistance programmes and adjuvant activities.[6]
Let us also be clear, that Compassion Fatigue is also a leadership concern. The defense against the adverse outcomes of occupational stress begins at the organizational and leadership level. An organization that is committed to protecting people in reasonable and appropriate ways is investing in the future. Organizational protection and prevention is especially important because it addresses the workplace stressors and risk factors, aiming to change the environment. A strong network of leadership is a key defense against clinical burnout.[7]
The bottom line remains that occupational stress can be inevitable, even at times necessary, elements of the work environment, but it does not have to translate into organizational dysfunction nor medical, psychological, or behavioral distress.[7] Compassion fatigue is an avoidable and treatable syndrome among health care providers, which includes physiotherapists. The prevention, management and treatment of such feelings is both a personal and organizational concern. Do note attempt to face this alone, because the sad truth remains, that you are not alone (this affects more people than you may think). Speak to someone about your concerns and make changes to your work environment. Seek help early to avoid an importance disturbance to your quality of life.
Resources[edit | edit source]
For an interesting read, take a look at : Physicians are not burning out, they are simply suffering moral injury.
Check out this great YouTube video on Clinical Resilience: Preventing Burnout, Promoting Compassion, and Improving Quality by The Schwartz Center for Compassionate Healthcare (2014).
References[edit | edit source]
- ↑ 1.0 1.1 Figley, C. R. (2002). Compassion fatigue: Psychotherapists' chronic lack of self care. Journal of Clinical Psychology, 58, 1433–1441.
- ↑ 2.0 2.1 Klappa SG, Fulton LE, Cerier L, Peña A, Sibenaller A, Klappa SP. Compassion fatigue among physiotherapist and physical therapists around the world. Glob. J. Med. Phys. 2015;3(5);124-137
- ↑ Owczarek, K., Wojtowicz, S., Pawłowski, W., & Białoszewski, D. (2017). Burnout syndrome among physiotherapists. Wiad Lek. 70 (3 pt 2): 537-542.
- ↑ Colligan TW, Higgins EM. Workplace stress. J Workplace 948 Behav Health. 2006;21(2):89-97
- ↑ Edwards, D., Burnard, P., Coyle, D., Fothergill, A., & Hannigan, B. (2000). Stress and burnout in community mental health nursing: A review of the literature. Journal of Psychiatric and Mental Health Nursing, 7, 7–14.
- ↑ 6.0 6.1 Felton, J.S. (1998). Burnout as a clinical entity—its importance in health care workers. Occupational Medicine.48 (4): 237–250. https://doi.org/10.1093/occmed/48.4.237
- ↑ 7.0 7.1 Quick, J.C., & Henderson, D.F. (2016). Occupational Stress: Preventing Suffering, Enhancing Wellbeing. Int J Environ Res Public Health. 13(5). pii: E459. doi: 10.3390/ijerph13050459.