Cervical Cancer
Original Editors - Anna Marie Usery & Stephanie Wilton from Bellarmine University's Pathophysiology of Complex Patient Problems project. Rewan Elsayed Elkanafany
Top Contributors - Anna Usery, Stephanie Wilton, Kim Jackson, Nupur Smit Shah, WikiSysop, Rewan Elsayed Elkanafany, Elaine Lonnemann, Wendy Walker, Vidya Acharya, Manisha Shrestha and Lucinda hampton
Definition/Description[edit | edit source]
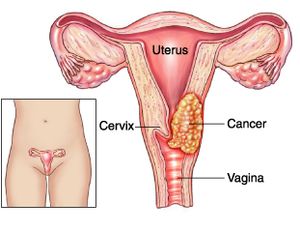
Carcinoma of the cervix is a malignancy arising from the cervix.[1]
- The cervix connects the uterus with the vagina (birth canal).[2], [3]
- The endocervix is the portion of the cervix closest to the uterus whereas the exocervix or ectocervix is closest to the vagina.[3]
The cervix is covered in two main types of cells: squamous cells found on the exocervix, and glandular cells on the endocervix.[3]
- Squamous and glandular cells come together at the area known as the transformation zone. It is here where most cervical cancers originate.[3]
- Gradually, the normal cells lining this area develop pre-cancerous changes that transform into cancer.[3] Cervical cancer typically grows at a slow rate and presents asymptomatically.[2]
Epidemiolgy[edit | edit source]
Cervical cancer continues to be listed among the top gynecologic cancers worldwide.
- According to current data, it is ranked fourteenth among all cancers and fourth-ranked cancer among women worldwide
- Globally, there are more than 500,000 new cases of cervical cancer annually.
- Approximately 250,000 women die of cervical cancer annually.
- In the United States, about 4000 women die from cervical cancer annually with African Americans, Hispanics, and women in low-resource areas having higher disparities in evidenced-based care and a much higher mortality rate. The causative agent is a sexually transmitted viral infection.
- Cervical cancer mortality is higher among women who have not been screened in the last five years and those women without consistent follow-up post identification of a precancerous lesion.
- Trends continue to show that women with the highest risk of mortality may be less likely to receive a vaccination that could potentially prevent cervical cancer.[4]
In the United States, the diagnosis of invasive stage cervical cancer has declined (75% decline since the 1960s) steadily.[5][6]Screening for cervical cancer has become more common due to the introduction of the Pap smear in the 1930s which made early detection possible.[7]
Cervical cancer is the most common cause of gynecological cancer-related death worldwide
- Mortality rates have decreased significantly in the United States (more than 45% since the early 1970s).[6],[7]
- 80% to 85% of cervical cancer-related deaths occur in developing countries.[8]
- Pre-invasive carcinoma in situ (no invasion of surrounding tissues) is more common in women 30-40 years of age.[6] Invasive carcinoma is more frequent in women over 40 years of age.[6] Women ages 65 and over account for 25% of new cases of cervical cancer.[7]
Etiology[edit | edit source]
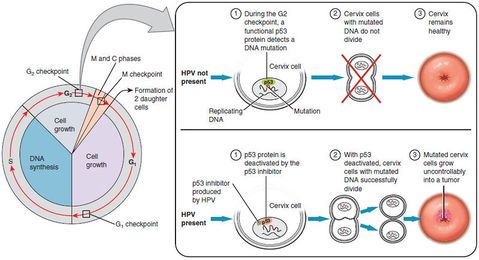
Current literature reports that Human papillomavirus (HPV) is found in the majority of sexually active people at some point during their life. There are more than 130 types of known HPV with 20 HPV types identified as cancer-related.
- HPV-related cervical dysplasia rates are only known in women since men are not screened outside of research protocols.
- HPV 16 and 18 are the most commonly found HPV in invasive cervical cancer.
- Population-based HPV prevalence studies show that the greatest prevalence of high-risk HPV occurs in the young adult period before 25 years of life and cervical cancer death peaks in the middle age period of 40 to 50 years of life[4].
Risk Factors[edit | edit source]
- human papillomavirus (HPV) 16 and 18 infections
- multiple sexual partners or a male partner with multiple previous or current sexual partners
- young age at first intercourse
- high parity
- immunosuppression
- certain HLA subtypes
- oral contraceptives
- nicotine/smoking [1]
Characteristics/Clinical Presentation[edit | edit source]
Presenting symptoms include:
- vaginal bleeding
- vaginal discharge
- subclinical: an abnormal cervical cancer screening test[1]
Clinical Staging for Cervical Cancer[edit | edit source]
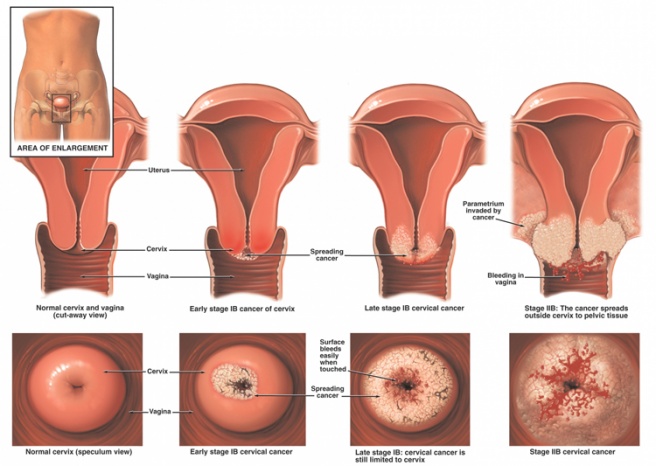
Cervical cancer is staged by the International Federation of Gynecology and Obstetrics (FIGO) staging system, based on clinical examination rather than surgical findings[7]. Revised FIGO staging of cervical carcinoma 2018
FIGO no longer includes Stage 0 (Tis)
I: confined to cervix uteri (extension to the corpus should be disregarded)
II: beyond the uterus, but has not extended onto the lower third of the vagina or to the pelvic wall
III: carcinoma involves the lower third of the vagina and/or extends to the pelvic wall and/or causes hydronephrosis or non‐functioning kidney and/or involves pelvic and/or paraaortic lymph nodes
IV: carcinoma has extended beyond the true pelvis or has involved (biopsy proven) the mucosa of the bladder or rectum[1]
Treatment and prognosis[edit | edit source]
Prognosis is affected by many factors which include:
- tumour stage
- the volume of the primary mass
- histologic grade
Five-year survival rates vary between 92% for stage I disease and 17% for stage IV disease[1]
Screening Tests[edit | edit source]
Cervical cancer screening is one of the best cancer prevention achievements. However, there continue to be women who are not compliant with screening recommendations. Many die from this preventable cancer due to inadequate screening. Public health efforts are available to increase access to screening with appropriate follow-up[9]
- According to the United States Preventative Services Task Force (USPTF), Pap screening is recommended beginning at age 21 years of age.
- HPV testing begins at age 30 in conjunction with Pap smear cytology.
- Screening is recommended every three years for women with continued normal screening and those low risk for cervical cancer.
- For women over 30 years of age, cytology can be every five years with HPV testing.
- Level A recommendation or women with low-risk status and consistent normal screenings can discontinue cervical cancer cytology and HPV testing at age 65.
- Women who have had a total abdominal hysterectomy including removal of the cervix for benign disease do not require further screening[4]
Systemic Involvement[edit | edit source]
- Cervical cancer affects the female reproductive system.
- Pressure from tumor on neighboring structures can affect the urinary system and gastrointestinal system (bowel).[7]
- Metastasis has been known to occur to the central nervous system (CNS), pulmonary system, urinary system (bladder), gastrointestinal system (rectum), retroperitoneal lymph nodes, paracervical lymphatics and parametrial lymphatics.[6]
Medical Management[edit | edit source]
Precancerous lesions are managed conservatively for those women younger than 25 years.
- The majority of abnormal findings in women younger than 25 are low-risk cervical dysplasia and will resolve spontaneously.
Colposcopy evaluates persistent, abnormal cytology or lesions suspected to be greater than low risk. These are managed according to findings.
- Low-risk lesions may be watched and reevaluated more frequently
- High-risk lesions are treated based on size, location, and staging.
- Cryotherapy or excision is done to manage pre-cancerous lesions that are limited in size and depth.
- Conization, laser or Loop Electrosurgical Excision Procedure (LEEP) are used in managing those lesions that include the endocervical canal and are more extensive.
- LEEP may provide better visualization of the squamocolumnar junction and provide the benefit of less bleeding in the outpatient setting.
If cancer is diagnosed, the next step in management is staging (see above) to determine further treatment.
- Treatment of early-stage disease includes a radical hysterectomy.
- For women who desire pregnancy with early-stage disease, conization may be the initial treatment.
- Chemotherapy and radiation are usually the next steps in treatment after hysterectomy to slow the growth of cancer[4]
Physiotherapy Management[edit | edit source]
The primary role of physical therapy associated with cervical cancer is education. Physiotherapists should be an advocate to their patients to stay regular with Pap smears and to practice other preventative measures (physical examinations, vaccines, protected sex). It is important for physiotherapists to gather a thorough patient history, including questions that encompass issues such as vaginal bleeding, GI or genitourinary function, location of pain and discomfort, and pre-existing comorbidities.[7] If issues of concern are found during the evaluation, physiotherapists should refer the patient to their primary care physician for further testing.
The main risk factors of lower limb lymphadema are BMI , FIGO stage, age , radiotherapy, lymphynode dissection and the number of lymph nodes removed. These risk factors should be considered while treating the patients of cervical cancer.[10]Prophylactic complex physiotherapy treatment was associated with lower rates of lymphedema and better patient reported symptom scores based on Gynecologic Cancer Lymphedema Questionnaire.[11]
Compresssion therapy is the gold standard therapy for lymphadema of lowerlimb. It reduces the volume of the limb and it is also considered to be fast acting.[12]Patients can be taught to tighten the compression system if its gets loose with time. For stage two lymphadema, the sub-bandage pressure of 45 mm Hg should be provided. For intolerant patients it should be between 15 to 25 mm Hg.
Physiotherapists should look for signs and symptoms of metastasis in women with a previous history of cervical cancer. Lymph node palpation is an important component of the examination due to the high rate of metastasis to this location.[7] Questions that address possible warning signs of metastasis (ex. rapid weight loss, night pain/sweats, vaginal bleeding, fatigue, frequent infections) should be included in patient history.[6] If issues of concern are found during the evaluation, physiotherapists should refer the patient to their primary care physician for further testing.
Women who have a current diagnosis of cervical cancer can benefit from physical therapy services. Physical therapy provides symptom relief by addressing impairments such as fatigue, muscle weakness, and management of pain.[6]
While treating patients with cancer, it is important for physiotherapists to review hematological values.[6] Aerobic exercise is contraindicated for patients receiving chemotherapy treatments when lab values are as follows:[6]
| Platelet count | <50,000/mm3 |
| Hemoglobin | <10g/dL |
| White blood cell count | <3,000/mm3 |
| Absolute granulocytes | <2,500/mm3 |
In an outpatient setting, it is recommended for physiotherapists to monitor vital signs and rate of perceived exertion (RPE) during exercise when working with patients with cancer.[6]
Research suggest that pelvic floor muscle training prior to radiation therapy for cervical cancer is an important measure to protect the strength of pelvic floor muscles and to prevent incontinence. [13]
Differential Diagnosis[edit | edit source]
- Polyps
- Cervical conditions (infections, polyps, myomas)
- Iatrogenic (birth control pills, HRT, IUD)
- Cervical ectopic pregnancy (consider with women of childbearing age)
- Endometrial cancer with cervical invasion
- Other cervical malignant condition (sarcoma, lymphoma, metastasis)
- Invasion of the cervix from other organs in proximity:
- Bladder cancer
- Rectal cancer
- Vaginal cancer
- Uterine cancer
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 Radiopedia Cervical Cancer Available from:https://radiopaedia.org/articles/carcinoma-of-the-cervix (last accessed 5.9.2020)
- ↑ 2.0 2.1 Available at: http://www.cancer.gov/cancertopics/types/cervical. Accessed March 18, 2014.
- ↑ 3.0 3.1 3.2 3.3 3.4 Available at: http://www.cancer.org/cancer/cervicalcancer/detailedguide/cervical-cancer-what-is-cervical-cancer. Accessed March 18, 2014.
- ↑ 4.0 4.1 4.2 4.3 Fowler JR, Jack BW. Cancer, Cervical.2017 Available from:https://www.ncbi.nlm.nih.gov/books/NBK431093/ (last accessed 5.9.2020)
- ↑ Ph.d. SE, Ph.d. KL. Understanding Pathophysiology. Mosby Incorporated; 2011.
- ↑ 6.0 6.1 6.2 6.3 6.4 6.5 6.6 6.7 6.8 6.9 Goodman CC, Snyder TE. Differential Diagnosis for Physical Therapists, Screening for Referral. W B Saunders Company; 2012.
- ↑ 7.0 7.1 7.2 7.3 7.4 7.5 7.6 Reviews CT. e-Study Guide for: Pathology: Implications for the Physical Therapist by Catherine C. Goodman, ISBN 9781416031185. Cram101 Textbook Reviews; 2012.
- ↑ Available at: http://www.rho.org/about-cervical-cancer.htm. Accessed March 18, 2014.
- ↑ Mansour T, Limaiem F. Cancer, cervical screening. InStatPearls [Internet] 2019 Jan 4. StatPearls Publishing.Available from:https://www.ncbi.nlm.nih.gov/books/NBK537348/ (accessed5.9.2020)
- ↑ Hu H, Fu M, Huang X, Huang J, Gao J. Risk factors for lower extremity lymphedema after cervical cancer treatment: a systematic review and meta-analysis. Translational cancer research. 2022 Jun;11(6):1713.
- ↑ Daggez M, Koyuncu EG, Kocabaş R, Yener C. Prophylactic complex physiotherapy in gynecologic cancer survivors: patient-reported outcomes based on a lymphedema questionnaire. International Journal of Gynecologic Cancer. 2023 Dec 1;33(12).
- ↑ BORDEA MP, EL-BSAT R, PREDESCU C, DANCIU R, VOINEA S, BORDEA C. REHABILITATION AFTER LOWER LIMB LYMPHOEDEMA IN GYNAECOLOGICAL MALIGNANCIES–THE ROLE OF PHYSIOTHERAPY.
- ↑ Sacomori C, Araya-Castro P, Diaz-Guerrero P, Ferrada IA, Martínez-Varas AC, Zomkowski K. Pre-rehabilitation of the pelvic floor before radiation therapy for cervical cancer: a pilot study. International urogynecology journal. 2020 Nov;31:2411-8.
- ↑ 14.0 14.1 Available at: http://oncolex.org/en/Gynecological-cancer/Diagnoses/Cervical-cancer/Background/DifferentialDiagnoses. Accessed March 19, 2014.
- ↑ 15.0 15.1 Available at: http://radiopaedia.org/articles/carcinoma-of-the-cervix. Accessed March 19, 2014.