Total Hip Replacement: Difference between revisions
(replace n+1 occurence of name content) |
No edit summary |
||
| (123 intermediate revisions by 18 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox"> | <div class="editorbox"> | ||
'''Original Editors ''' - [[User:Annelies Beckers|Annelies Beckers]], [[User:Vincent Everaert|Vincent Everaert]] | '''Original Editors ''' - [[User:Annelies Beckers|Annelies Beckers]], [[User:Vincent Everaert|Vincent Everaert]] as part of the [[Vrije Universiteit Brussel Evidence-based Practice Project|Vrije Universiteit Brussel's Evidence-based Practice project]]. | ||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | ||
</div> | </div> | ||
== | == Description == | ||
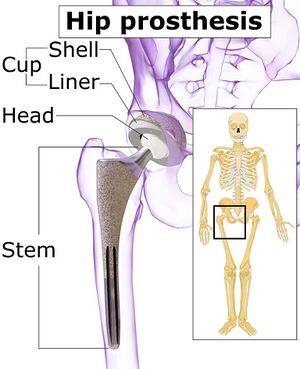
[[File:Hip prosthesis components.jpeg|thumb|Hip prosthesis components|alt=Hip prosthesis components]] | |||
[[ | Total hip replacement (THR), or Total Hip Arthroplasty (THA), is a procedure that removes damaged bone and cartilage and replaces it with prosthetic components. THR is one of the most cost-effective and consistently successful surgeries performed in orthopaedics. | ||
* THR provides good outcomes for patients suffering from advanced degenerative [[Hip Osteoarthritis|hip osteoarthritis]], providing [[Pain Assessment|pain]] relief, functional restoration, and improved [[Quality of Life|quality of life.]]<ref name=":5">Varacallo M, Luo TD, Johanson NA. [https://www.statpearls.com/articlelibrary/viewarticle/22894/ Total Hip Arthroplasty Techniques.] InStatPearls [Internet] 2020 Jul 8. StatPearls Publishing.Available from: https://www.statpearls.com/articlelibrary/viewarticle/22894/ (accessed 14.2.2021)</ref><ref name=":3">Levine BR, Klein GR, Cesare PE. [https://www.researchgate.net/profile/Paul_Dicesare/publication/6296081_Surgical_approaches_in_total_hip_arthroplasty_A_review_of_the_mini-incision_and_MIS_literature/links/0f31752dc21c0f154c000000.pdf Surgical approaches in total hip arthroplasty: A review of the mini-incision and MIS literature.] Bulletin of the NYU Hospital for Joint Diseases 2007;65(1):5-18.</ref> | |||
* During a THR, the head of the [[femur]] is replaced with a [[Prosthetics|prosthetic]] head on a shaft, and the joint surface of the [[Acetabulum fracture|acetabulum]] is lined with a bowl-shaped synthetic joint surface. | |||
* A [[Partial Hip Replacement|partial hip replacement]] can also be done for neck of [[femur]] [[Fracture|fractures]] (mostly displaced)<ref name=":6">Iglesias SL, Gentile L, Mangupli MM, Pioli I, Nomides RE, Allende BL. [http://www.alliedacademies.org/articles/femoral-neck-fractures-in-the-elderly-from-risk-factors-to-pronostic-features-for-survival.pdf Femoral neck fractures in the elderly: from risk factors to pronostic features for survival.] Journal of Trauma and Critical Care. 2017;1(1).</ref> where only the femoral part is replaced. | |||
== Clinically Relevant Anatomy == | == Clinically Relevant Anatomy == | ||
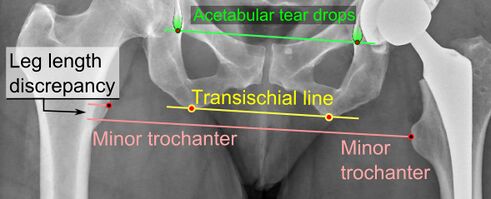
[[File:THR X-ray.jpg|thumb|313x313px|THR X-ray|alt=Total Hip Replacement X-ray]]The hip is a ball and socket joint. This design allows the poly-axial movement seen at the [[Hip Anatomy|hip]]. | |||
The | The head of the femur and the inside of the acetabulum are covered with a layer of hyaline [[cartilage]].<ref name="Fractures of the hip">Meyers HM. Fractures of the hip. Chicago: Year of the book medical publishers Inc., 1985</ref> Once this cartilage is worn away or damaged (usually by [[arthritis]]), the underlying bone is exposed, resulting in pain, stiffness and possibly shortening of the affected leg. By replacing these surfaces the aim is to reduce pain and stiffness to restore an active and pain-free life. | ||
THR is mostly done electively.<ref name="Gremeaux V.">Gremeaux V, Renault J, Pardon L, Deley G, Lepers R, Casillas JM. [https://www.archives-pmr.org/article/S0003-9993(08)01388-9/fulltext Low-frequency electric muscle stimulation combined with physical therapy after total hip arthroplasty for hip osteoarthritis in elderly patients: a randomized controlled trial.] Archives of physical medicine and rehabilitation 2008;89(12):2265-73.</ref><ref name="Jan M.">Jan MH, Hung JY, Lin JC, Wang SF, Liu TK, Tang PF. [https://www.archives-pmr.org/article/S0003-9993(04)00306-5/fulltext Effects of a home program on strength, walking speed, and function after total hip replacement.] Archives of physical medicine and rehabilitation 2004 ;85(12):1943-51.</ref><ref name="Stockton K.">Stockton KA, Mengersen KA. [https://www.archives-pmr.org/article/S0003-9993%2809%2900377-3/fulltext Effect of multiple physiotherapy sessions on functional outcomes in the initial postoperative period after primary total hip replacement: a randomized controlled trial.] Archives of physical medicine and rehabilitation 2009;90(10):1652-7.</ref><ref name="Rahmann A.">Rahmann AE, Brauer SG, Nitz JC. [https://www.archives-pmr.org/article/S0003-9993(09)00144-0/fulltext A specific inpatient aquatic physiotherapy program improves strength after total hip or knee replacement surgery: a randomized controlled trial.] Archives of physical medicine and rehabilitation 2009;90(5):745-55.</ref> | |||
== Indications for Surgery == | |||
The most common indication for THA hip OA. Other indications include:<ref name=":7">Affatato S. [https://books.google.co.za/books?hl=en&lr=&id=igujAgAAQBAJ&oi=fnd&pg=PP1&dq=+Perspectives+in+total+hip+arthroplasty:+Advances+in+biomaterials+and+their+tribological+interactions.+&ots=U9KaS5d_0r&sig=MNHZw0T712KtOThLEZBUZ6OnaSE#v=onepage&q=Perspectives%20i Perspectives in total hip arthroplasty: Advances in biomaterials and their tribological interactions.] London: Woodhead Publishing, 2014. | |||
</ref> | |||
= | * Trauma: can be considered in a case by case basis in [[Femoral Neck Fractures]] (displaced intracapsular) in active and healthy patients | ||
* Osteonecrosis of the hip, commonly known as [[Avascular necrosis of the femoral head|avascular necrosis of the hip]]<ref>Hsu H, Nallamothu SV. Hip Osteonecrosis.Available:https://www.ncbi.nlm.nih.gov/books/NBK499954/ (accessed 9.12.2022)</ref> | |||
* Developmental [[Hip Dysplasia|dysplasia of the hip]] | |||
* Hardware failure after internal fixation of [[Femoral Neck Hip Fracture|hip fractures]]<ref name=":5" /> | |||
== Complications == | |||
[[File:Leg length discrepancy after hip replacement.jpg|thumb|491x491px|Leg length discrepancy after THR|alt=Leg length discrepancy after Total Hip Replacement]] | |||
Complications following THR can be loosely divided into systemic and procedure specific complications. Incidence of complications have improved over time, due to [[Surgery and General Anaesthetic|surgical]] and anaesthetic technique improvements, along with the better diagnosis and management of these complications. | |||
The most common systemic complication is a [[Deep Vein Thrombosis|deep vein thrombosis]]. [[Infection Prevention and Control|Infection]] is the most dreaded complication. [[Leg Length Discrepancy|Leg length discrepancy]] is a common cause of patient dissatisfaction<ref>Park C, Merchant I. Complications of total hip replacement. InTotal Hip Replacement-An Overview 2018 Nov 5. IntechOpen. Available:https://www.intechopen.com/chapters/61241 (accessed 8.12.2022)</ref>. For more see [[Total Hip Replacement Complications]]. | |||
== Contraindications for Surgery == | |||
THA is contraindicated in the following clinical scenarios: | |||
* Local: [[Septic (Infectious) Arthritis]] | |||
* Remote (i.e. extra-articular) active, ongoing infection or bacteraemia. | |||
* Severe cases of [[Peripheral Arterial Disease|Peripheral Vascular Disease]] <ref>Varacallo M, Luo TD, Johanson NA. [https://www.statpearls.com/articlelibrary/viewarticle/22894/ Total Hip Arthroplasty Techniques]. InStatPearls [Internet] 2020 Jul 8. StatPearls Publishing.Available from:https://www.statpearls.com/articlelibrary/viewarticle/22894/ (accessed 14.2.2021)</ref> | |||
== Orthopaedic Assessment == | |||
An assessment by an orthopaedic surgeon consists of several components: | |||
* Medical history: general health and questions about the extent of hip pain and how it affects ability to perform [[Activities of Daily Living|ADLs.]] | |||
* [[Hip Examination]] | |||
* [[X-Rays|X-rays]]. Assess the extent of damage or deformity in the hip. | |||
* Other tests. Occasionally other tests, e.g., [[MRI Scans|MRI]] scan, may be needed to determine the condition of the bone and soft tissues of the hip. | |||
The diagnosis of patients requiring THR is mostly symptom-based. Pain, loss of [[Range of Motion|range of motion]] and functional impairments are mostly considered.<ref name="Crawford A.">Crawford AJ, Hamblen DL. Outline of Orthopaedics , thirteenth edition, London: Churchill Livingstone, 2001</ref> | |||
== Prosthesis == | |||
[[File:Stainless steel and ultra high molecular weight polythene hip replacement (9672239334).jpeg|thumb|Stainless steel and ultra high molecular weight polythene THR|alt=Stainless steel and ultra high molecular weight polythene Total Hip Replacement]] | |||
When performing a THR, the ball is removed, socket reshaped, and the artificial implant is positioned in the bone. The implant may be held in the bone by tightly wedging it in place, or cementing into position. Type of fixation used depends on the patient's bone health and the design of the implant. Contemporary THR techniques have evolved into press-fit femoral and acetabular components, and many variations exist.<ref>Very well health What Type of Hip Replacement Implant Is Best? Available:https://www.verywellhealth.com/what-type-of-hip-replacement-implant-is-best-2549558#citation-2 (accessed 8.12.2022)</ref> The basic components are: | |||
== | # '''Bearing surfaces''' are the surfaces which articulate in the prosthetic joint. The femoral head and the acetabular liner can be used in different combinations. These will give different appearance on radiograph depending on the configuration. Many options are available e.g., Metal-on-polyethylene, Ceramic-on-polyethylene, Ceramic-on-ceramic, Metal-on-metal.<ref name=":5" /> | ||
# '''Femoral component''' or stem: this refers to the prosthesis which is implanted into the femur. They can be described by length, taper, and presence of a collar. Attached to the femoral component is the neck and head which in most prostheses can be altered in size to create a stable joint<ref name=":0">Radiopedia [https://radiopaedia.org/articles/total-hip-arthroplasty THR] Available from:https://radiopaedia.org/articles/total-hip-arthroplasty (accessed 14.2.2021)</ref>. | |||
# '''Prosthesis fixation:''' Femoral stem fixation can be either cemented or non-cemented (biological) fixation<ref name=":0" />. Prevalence of fixation technique: increasing trend towards cementless fixation; 93% of THA in United States in 2012 were cementless<ref name=":2">Ortho bullets [https://www.orthobullets.com/recon/5003/tha-implant-fixation THR] Available from:https://www.orthobullets.com/recon/5003/tha-implant-fixation (accessed 14.2.2021)</ref> | |||
== Surgical Approaches == | |||
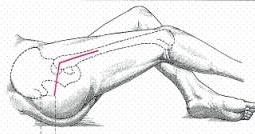
[[File:Posterior hip approach.jpg|thumb|Posterior hip approach|alt=Posterior hip approach illustration]] | |||
Any number of approaches can be used for the THA procedure. The three most common approaches are: | |||
== | # Posterior (PA): Most common surgical approach for THR. Major advantage of this approach is the avoidance of the [[Hip Abductors|hip abductors]]. Performed with a patient lying on their side and a surgical incision made along the outside of the hip.<ref name=":1">Varacallo M, Luo TD, Johanson NA. Total hip arthroplasty techniques. InStatPearls [Internet] 2022 Sep 4. StatPearls Publishing.Available:https://www.ncbi.nlm.nih.gov/books/NBK507864/ (accessed 8.12.2022)</ref> | ||
# Direct Anterior (DA): This surgical procedure has been increasing over the past decade. This approach is performed with a patient lying on their back, and a surgical incision is made coming down the front of the thigh (between the [[Tensor Fascia Lata|tensor fascia lata]] and [[sartorius]] on the superficial end, and the [[Gluteus Medius|gluteus medius]] and [[Rectus Femoris|rectus femoris]] on the deep side). There are several potential advantages of the direct anterior approach. The two most prominent are a low dislocation risk and early postoperative recovery.<ref name=":1" />Perception is that DAA results in less tissue damage, however this lacks support in the literature.<ref>Mead PA, Bugbee WD[https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8735710/ . Direct anterior approach to total hip arthroplasty improves the likelihood of return to previous recreational activities compared with posterior approach]. JAAOS Global Research & Reviews. 2022 Jan;6(1).Available: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8735710/ (accessed 8.1.2024)</ref> | |||
# Direct lateral (Hardinge) or anterolateral: Often considered to be a balance between the AP and PA. Person positioned on their side, and the surgical incision is placed directly down the outside of the hip. The advantage: balance of having a versatile incision that can be used to correct deformities and insert specialised implants with lower dislocation rates following surgery than what is observed with posterior approaches. Disadvantage: superior gluteal nerve dissection may result in nerve injury, leading to postoperative [[Trendelenburg Gait|Trendelenburg gait]], characterized by compensatory movements to address [[Hip Abductors|hip abductor]] weakness. <ref name=":1" /> | |||
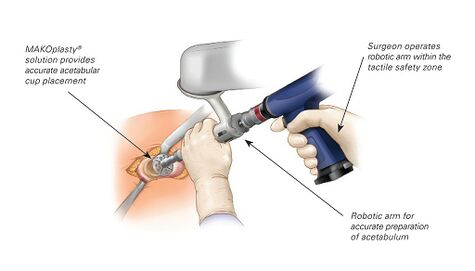
[[File:THR with MAKOplasty procedure.jpeg|thumb|475x475px|MAKOplasty<sup>®</sup> THR is powered by Interactive Robotic Arm]]Additionally | |||
# Robotic Arm Assisted THR: Assists with THR surgery, helping in the accurate positioning of the implants which correlates with improved function and lifespan of the THR. Can be used in all current surgical approaches to the hip (AP, PA and lateral). | |||
# Minimally invasive surgery is becoming popular all around the world, due to the quicker recovery rates and reduced postoperative pain. Long term follow-up and comparison studies are still needed in this field.<ref>Alecci V, Valente M, Crucil M, Minerva M, Pellegrino C, Sabbadini DD. [https://link.springer.com/article/10.1007/s10195-011-0144-0 Comparison of primary total hip replacements performed with a direct anterior approach versus the standard lateral approach: perioperative findings.] J Orthopaed Traumatol 2011;12:123-129.</ref> | |||
View this 3 minute video and learn about the different approaches to hip replacement surgery and the advantages of each method. | |||
{{#ev:youtube|v=1cUu-vMcSkM|300}}<ref>John Hopkins Medical. Approaches to Hip Replacement Surgery | Dr. Savya Thakkar. Available from: https://www.youtube.com/watch?v=1cUu-vMcSkM [last accessed 8.12.2022]</ref> | |||
== Physiotherapy Management == | |||
Plenty of questions remain concerning the most effective rehabilitation management of patients following a THA. This uncertainty exists as a comparison of the effectiveness and harms of interventions is difficult due to the diverse programs, frequently inadequate intervention description, and an extensive variety of outcomes reported across research. What is needed are well-conducted studies that address both effectiveness and harms of interventions using randomised controlled trials.<ref>Konnyu KJ, Pinto D, Cao W, Aaron RK, Panagiotou OA, Bhuma MR, Adam GP, Balk EM, Thoma LM. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9464790/ Rehabilitation for Total Hip Arthroplasty: A Systematic Review.] Am J Phys Med Rehabil. 2023 Jan 1;102(1):11-18. doi: 10.1097/PHM.0000000000002007. Epub 2022 Mar 12. PMID: 35302955; PMCID: PMC9464790.Accessed 8.1.204 Available:https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9464790/</ref> | |||
Discuss '''[[Hip Precautions|Hip precautions]]''' before surgery. | |||
# PA avoid: flexion past 90 degrees; extreme internal rotation; adduction past body's midline | |||
# Anterolateral approach avoid: extension; extreme external rotation; adduction past the body's midline | |||
# AP avoid''':''' bridging; extension; extreme external rotation; adduction past body's midline<ref name=":2" /> | |||
Hip precautions have traditionally been used within the management of total hip arthroplasty to reduce the risk of dislocations <ref>Coole C, Edwards C, Brewin C, Drummond A. [https://journals.sagepub.com/doi/abs/10.4276/030802213X13729279114898 What do clinicians think about hip precautions following total hip replacement?] Br J Occup Ther. 2013;76:7:300-307.</ref>. This is particularly needed to provide safe boundaries for movement when patients are keen to “push” those boundaries soon after surgery or have other risk factors such as abductor deficiency with a history of previous dislocations, loose soft tissues, patients with neuromuscular and cognitive disorders<ref name=":8">Mandel RT, Bruce G, Moss R, Carrington RWJ, Gilbert AW. [https://www.tandfonline.com/doi/full/10.1080/09638288.2020.1845825?scroll=top&needAccess=true&role=tab Hip precautions after primary total hip arthroplasty: a qualitative exploration of clinical reasoning.] Disab Rehab. 2022;44:12:2842–2848</ref>. However, their use is increasingly controversial due to their association with a slower return to activities, an absence in the rise of dislocation rates when precautions are not used, and a lack of evidence to support their use <ref>Barnsley L, Leslie Barnsley L, Page R. [https://journals.sagepub.com/doi/pdf/10.1177/2151458515584640 Are Hip Precautions Necessary Post Total Hip Arthroplasty? A Systematic Review.] Geriatr Orthop Surg Rehabil. 2015;6:3:230-235</ref><ref name=":8" />. | |||
==== Pre-operative ==== | |||
One on one preoperative physical therapy session protocol is effective at reducing the number of postoperative PT visits and time for readiness to discharge from PT. It plays an important role towards improving preoperative quality of life (people can wait many months for surgery and experience further deterioration in health-related quality of life during long waits).<ref>Soeters R, White PB, Murray-Weir M, Koltsov JC, Alexiades MM, Ranawat AS. Preoperative physical therapy education reduces time to meet functional milestones after total joint arthroplasty. Clinical orthopaedics and related research. 2018 Jan;476(1):40.Available: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5919221/ (accessed 89.12.2022)</ref>See also [[Physical Activity Pre and Post Surgery]] | |||
Pre-operative assessment and treatment session | |||
* Helps to develop a patient-specific rehabilitation programme to follow post-operative, taking assessment findings into consideration e.g., Does the patient desires to re uptake golf. | |||
* Benefits: decreased length of stay<ref>Crowe J,Henderson J. [http://journals.sagepub.com/doi/abs/10.1177/000841740307000204 Pre-arthroplasty rehabilitation is effective in reducing length of hospital stay]. Canadian Journal of Occupational Therapy 2003;70:88-96.</ref>; decreased anxiety levels<ref name=":4">Barnes RY, Bodenstein, K, Human N. Raubenheimer J, Dawkins J, Seesink C, Jacobs J, van der Linde J, Venter R. [https://journals.co.za/content/journal/10520/EJC-ee9fbc7e5 Preoperative education in hip and knee arthroplasty patients in Bloemfontein.] South African Journal of Physiotherapy 2018;74(1).</ref>; improved self-confidence<ref name="Sohier">Raymond Sohier, Kinesitherapie de la hanche ; La Hestre : Sohier, 1974</ref>; establish a relationship of trust between the physiotherapist and patient. | |||
* A combination of verbal explanation and written pamphlets is the best method for health education.<ref name=":4" /> Important to incorporate this into the pre-operative physiotherapy management of patients prior to total hip replacements (linked to better post-operative adherence).<ref name=":4" /> | |||
'''Pre op Assessment''' | |||
* Subjective history | |||
* Range of motion | |||
* Muscle power | |||
* Circulation | |||
* Mobility and function<ref name="Sohier" /> | |||
'''Pre op Treatment''' | |||
* Education and advice: Patient information booklet; Precautions and contraindications; Rehabilitation process; Goals & expectations; Functional/ADL adaptions; Safety principles | |||
* Encourage to [[Smoking Cessation and Brief Intervention|stop smoking]] if applicable | |||
* [[Discharge Planning|Discharge planning]] | |||
* Teach: Bed exercises; Transfers in and out of bed (within precautions) | |||
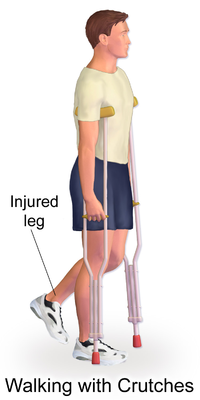
* [[Gait]] re-education with mobility [[Assistive Devices|assistive device]] ([[crutches]] vs [[walkers]]) | |||
* Stair climbing | |||
< | ==== Post-operative ==== | ||
Start the day of surgery as leads to decreased length of stay, reduces pain and improves function. | |||
* Aim of post-operative rehabilitation: address the functional needs of the patient (e.g. start mobilizing) and to improve mobility, strength, flexibility and reduce pain.<ref name="Stockton K." /> . This starts off as an assisted process, but the aim is to get the patient as functional as possible prior to discharge. | |||
* As a result of the underlying pre-operative pathology, patients may present with muscle atrophy and loss of strength, particularly in the gluteus medius and quadriceps muscles. The result of the loss of strength is that the elderly are less independent.<ref name="Gremeaux V." /> | |||
* Surgery will correct the joint problems but associated muscle weakness that was present before the surgery will remain and require post-operative rehabilitation (research has shown hip abductor weakness after surgery is a major risk associated with joint instability and prosthetic loosening).<ref name="Jan M." /> Patients can achieve significant improvements through a targeted strengthening programme following total hip replacement.<ref>Galea MP, Levinger P, Lythgo N, Cimoli C, Weller R, Tully E, McMeeken J, Westh R. [https://www.archives-pmr.org/article/S0003-9993(08)00305-5/fulltext A targeted home-and center-based exercise program for people after total hip replacement: a randomized clinical trial.] Archives of physical medicine and rehabilitation 2008;89(8):1442-7.</ref> Motor Imagery training, has been found to be a useful adjunct therapy tool as it improves both specific and general adaptations that were related to patients’ physical capabilities when added in a corollary to routine physical therapy.<ref>Paravlic AH, Pisot R, Marusic U. Specific and general adaptations following motor imagery practice focused on muscle strength in total knee arthroplasty rehabilitation: A randomized controlled trial. PloS one. 2019;14(8).</ref> | |||
* No specific general hip replacement protocol is currently in use, as small elements of the rehabilitation process are surgeon specific. For example, in some enhanced recovery after surgery protocols, patients are mobilised out of bed within the first 6 hours post-surgery. Other settings may only start mobilizing patients out of bed on day 1 or 2 post-surgery. Accelerated rehabilitation programmes and early mobilization have shown to give patients more confidence in their post-operative mobilization and activities of daily living, as well as being more comfortable with earlier discharge.<ref>Robertson NB, Warganich T, Ghazarossian J, Khatod M. [https://www.hindawi.com/journals/aos/2015/387197/ Implementation of an accelerated rehabilitation protocol for total joint arthroplasty in the managed care setting: the experience of one institution.] Advances in Orthopedic Surgery. 2015;387197.</ref> | |||
*< | ==== Evidence ==== | ||
Physiotherapy: can improve strength and gait speed after total hip replacement and help prevent complications such as subluxation and thromboembolic disease; increases the patient’s mobility and offers education about the exercises and precautions that are necessary during hospitalization and after discharge.<ref>Coulter CL, Scarvell JM, Neeman TM, Smith PN. [https://www.sciencedirect.com/science/article/pii/S183695531370198X Physiotherapist-directed rehabilitation exercises in the outpatient or home setting improve strength, gait speed and cadence after elective total hip replacement: a systematic review.] Journal of physiotherapy. 2013;59(4):219-26.</ref>; maximizes the patient’s function which is associated with a greater probability of earlier discharge, which is in turn associated with a lower total cost of care<ref name="Freburger">Freburger J. [https://academic.oup.com/ptj/article/80/5/448/2842484 An analysis of the relationship between the utilization of physical therapy services and outcomes of care for patients after total hip arthroplasty.] Physical therapy 2000;80(5):448-458.</ref> | |||
* Bed exercise following a total hip replacement important for the effects on oedema, cardiac function and improving range of motion and muscle strength<ref name="Perhonen">Perhonen MA, Franco F, Lane LD, Buckey JC, Blomqvist CG, Zerwekh JE, Peshock RM, Weatherall PT, Levine BD. [https://www.physiology.org/doi/full/10.1152/jappl.2001.91.2.645 Cardiac atrophy after bed rest and spaceflight.] Journal of applied physiology 2001;91(2):645-53.</ref>. | |||
* Early weight bearing and physical activity have benefits for the quality of bone tissue<ref name="Mahendra">Mahendra G, Pandit H, Kliskey K, Murray D, Gill HS, Athanasou N. [https://www.tandfonline.com/doi/full/10.3109/17453670903473016 Necrotic and inflammatory changes in metal-on-metal resurfacing hip arthroplasties: relation to implant failure and pseudotumor formation.] Acta orthopaedica 2009;80(6):653-9.</ref>, improving the fixation of the prosthesis and decreases the incidence of early loosening. The amount of activity is patient-specific, and clinical reasoning should be used to make adaptions where needed. Certain specific sport movements have a higher risk of injury for unskilled individuals, and should be incorporated later in the rehabilitation process under supervision of a physiotherapist. | |||
'''Suggested protocol in the absence of complications:''' Surgeon preference should be taken into account, as well as any other factors that might hinder the following of the protocol. Adaptions should be made to make it more patient specific.<ref name="Sohier" /><ref name="Suetta">Suetta C, Aagaard P, Rosted A, Jakobsen AK, Duus B, Kjaer M, Magnusson SP. [https://www.physiology.org/doi/pdf/10.1152/japplphysiol.01307.2003 Training-induced changes in muscle CSA, muscle strength, EMG, and rate of force development in elderly subjects after long-term unilateral disuse.] Journal of Applied Physiology 2004;97(5):1954-61.</ref> | |||
==== Day 1 Post-Surgery ==== | |||
* Education and advice | |||
* Education of muscular relaxation | |||
* Revision of precautions and contraindications (provided that patient had a pre-operative session with the physiotherapist, otherwise full education will be done as mentioned in pre-operative section). | |||
* Bed exercises: | |||
** Circulation drills | |||
** Upper limb exercises to stimulate the cardiac function | |||
** Maintenance of the non-operated leg: attention should be paid to the range of motion in order to preserve controlled mobilisation on the operated hip | |||
** Isometric quadriceps (progressing to concentric VMO) and gluteal contractions | |||
** Active-assisted (progressing to active) heel slides, hip abduction/adduction | |||
* Bed mobilisation using unilateral bridging on the unaffected leg | |||
* Getting in and out of bed (see [https://www.allinahealth.org/health-conditions-and-treatments/health-library/patient-education/total-hip-replacement/preparing-for-surgery/mobility-and-activity-techniques-for-daily-living here]) | |||
* Getting on and off a chair with arms (see [https://www.allinahealth.org/health-conditions-and-treatments/health-library/patient-education/total-hip-replacement/preparing-for-surgery/mobility-and-activity-techniques-for-daily-living here]) | |||
* Sit to stand with mobility assistive device (preferably a device giving more support like a walking frame or rollator) | |||
* Gait re-education with mobility assistive device as tolerated (weight bearing status as determined by surgeon) | |||
* Sitting out in chair for maximum 1 hour | |||
* Positioning when transferred back to bed | |||
* | ==== Day 2 Post-Surgery ==== | ||
* Bed exercises as described above, progressing repetitions and decreasing assistance given to patient | |||
* Progression of distance mobilised and/or mobility assistive device | |||
* Incorporate balance exercises if needed | |||
* Sitting in chair | |||
==== Day 3 Post-Surgery ==== | |||
[[File:Straight leg raise.png|thumb|single leg bridge|alt=single leg bridge illustration]] | |||
Bed exercises as described above, progressing repetitions and decreasing assistance given to patient | |||
* Progression of distance mobilised and/or mobility assistive device | |||
* Stair climbing (at least 3, or as per home requirements) | |||
* Sitting in chair | |||
* Revision of precautions, contraindications and functional adaptions | |||
* Give 6 week progressive resistive strengthening [[Adherence to Home Exercise Programs|home exercise]] to patient; this can include stationary cycling, as long as the patient stays within the precautions (especially posterior approach surgery) | |||
After 3 days clients are usually discharged home if they meet the discharge criteria. The physiotherapist and nurse help to transfer to a car whilst maintaining hip precautions. As majority of patients lack understanding about the activities they can do following THR surgery, discharge education about pre-discharge pain management, movement, ADL, and support requirements should be provided to the clients. A recent RCT showed that video-assisted discharge program and education booklets given to the patient and their relatives after THR on activities of daily living, functionality, and patient satisfaction found that video-assisted discharge program along with physiotherapy reduced pain perception and kinesiophobia, improve hip function, and increase patient satisfaction. Further research is needed to assess the long-term outcomes of video-assisted discharge education in THR patients.<ref>Cetinkaya Eren O, Buker N, Tonak HA, Urguden M. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8866490/ The effect of video-assisted discharge education after total hip replacement surgery: a randomized controlled study]. Scientific Reports. 2022 Feb 23;12(1):1-9.</ref> | |||
===== '''Discharge Home Criteria:''' ===== | |||
* independent ambulation with assistive device | |||
* independent transfers | |||
* independent ADLs | |||
* stairs with supervision | |||
* appropriate home assistance (spouse, family, visiting nurses)<ref name=":2" /> | |||
< | ==== Home Planning ==== | ||
[[File:Crutches Walking.png|alt=crutch gait swing phase illustration|400x400px|thumb|crutch gait swing phase ]] | |||
Several modifications to make home easier to navigate. The following items help with daily activities: | |||
* Securely fastened safety bars or handrails in shower or bath | |||
* Secure handrails along all stairways | |||
* A stable chair for your early recovery with a firm seat cushion (allows knees to remain lower than hips), a firm back, and two arms | |||
* A raised toilet seat | |||
* A stable shower bench or chair for bathing | |||
* A long-handled sponge and shower hose | |||
* A dressing stick, a sock aid, and a long-handled shoehorn | |||
* A reacher allowing grasping of objects without excessive bending of your hips | |||
* Firm pillows for chairs, sofas, and car enabling client to sit with knees lower than hips | |||
* Removal of all loose carpets and electrical cords from the areas walked in home<ref name=":2" /> | |||
This 7 minute video presents post-operative exercises after a total hip replacement for weeks 1-4.{{#ev:youtube|v=9eU8G038zFo|300}}<ref>HeartlandOrthospecial. Post-Operative Exercises Weeks 1-4 for Total Hip Replacement. Available from: https://www.youtube.com/watch?v=9eU8G038zFo[last accessed 24.3.2023]</ref> | |||
* | ==== 6 Weeks Post Surgery ==== | ||
* Patients are normally followed up by orthopaedic surgeon | |||
* Surgeon determines if the patient is allowed the following: | |||
** Full range of motion at the hip | |||
** Full weight bearing without mobility assistive device | |||
** Driving | |||
==== After 6 Weeks ==== | |||
* Gain of initial ROM, stabilization, and proprioception | |||
* Endurance | |||
* Flexibility | |||
* Balance | |||
* Speed, precision, neurological coordination | |||
* Functional exercises | |||
==== Return to sport ==== | |||
Low-impact exercises are preferred | |||
* golf: handicap shows minimal change after THA; handicap shows increase after TKA | |||
* high-impact exercises increase revision rates in patients less than 55 years-old | |||
== Outcome Measures == | == Outcome Measures == | ||
* [[Harris Hip Score]] | |||
* Oxford Hip Score ([http://www.orthopaedicscore.com/scorepages/oxford_hip_score.html/ OHS]) | |||
* [[Six Minute Walk Test / 6 Minute Walk Test|6 Minute Walking Test]] | |||
* [[Timed Up and Go Test (TUG)|Timed Get Up & Go Test]] | |||
* Western Ontario and McMaster universities osteoarthritis index ([http://www.womac.org/ WOMAC]) | |||
* [http://www.sf-36.org/ SF-36] | |||
* [[Fear Avoidance Belief Questionnaire|Fear Avoidance Belief Score]] | |||
* Hip Disability & Osteoarthritis Outcome Score ([http://www.orthopaedicscore.com/scorepages/hip_disability_osteoarthritis_outcome_score_hoos.html/ HOOS]) | |||
* [[International Hip Outcome Tool (iHOT)|International Hip Outcome Tool]] | |||
* [[Ibadan Knee/Hip Osteoarthritis Outcome Measure (IKHOAM)|Ibadan Knee/Hip Osteoarthritis Outcome Measure]] | |||
== Team Work == | |||
Total hip arthroplasty (THA) is one of the most reliable, reproducible, successful, and cost-effective procedures in all of orthopedics. The procedure requires coordination of care across various healthcare provider groups, including nurses, physical therapists, advanced practitioners and physician extenders, medical physicians, and orthopedic surgeons. | |||
== | |||
Clinicians including the surgeon, nurse practitioner, and physiotherapist should work together to provide the patient and family with education regarding the procedure, expected issues, and guidance for aftercare.<ref name=":5" /> | |||
== Virtual Clinic Visits == | |||
Virtual follow-up for hip and knee arthroplasty patients is an effective substitute to in-person clinic assessment, substantiated in a recent investigation including 1,749 patients seen in a virtual visit between January 2017 and December 2018. | |||
# For the 1-year postoperative visit and routine scheduled follow-up visits, only 7.22% of the patients required a further in-person assessment. | |||
# Is accepted by patients, has high patient satisfaction, and can reduce the cost to both health services and patients.<ref>El Ashmawy AA, Dowson K, El-Bakoury A, Hosny HA, Yarlagadda R, Keenan J. Effectiveness, patient satisfaction, and cost reduction of virtual joint replacement clinic follow-up of hip and knee arthroplasty. The Journal of arthroplasty. 2021 Mar 1;36(3):816-22.Available:https://pubmed.ncbi.nlm.nih.gov/32893060/ (accessed 6.12.2022)</ref> | |||
== References == | == References == | ||
<references /><br> | <references /><br> | ||
[[Category: | [[Category:Orthopaedic Surgical Procedures]] | ||
[[Category:Joints]] | |||
[[Category:Hip]] | |||
[[Category:Musculoskeletal/Orthopaedics]] | |||
[[Category:Vrije Universiteit Brussel Project]] | |||
[[Category:Acute Care]] | |||
[[Category:Older People/Geriatrics]] | |||
[[Category:Older People/Geriatrics - Conditions]] | |||
[[Category:Conditions]] | |||
[[Category:Interventions]] | |||
[[Category:Older People/Geriatrics - Interventions]] | |||
[[Category:Older People/Geriatrics - Interventions]] | |||
[[Category:Hip - Interventions]] | |||
[[Category:Osteoarthritis]] | |||
[[Category:Arthroplasty]] | |||
Latest revision as of 13:42, 11 January 2024
Original Editors - Annelies Beckers, Vincent Everaert as part of the Vrije Universiteit Brussel's Evidence-based Practice project.
Top Contributors - Lucinda hampton, Annelies Beckers, Leana Louw, Jessie Tourwe, Didzis Rozenbergs, Kim Jackson, Vincent Everaert, Admin, Yana Motte, Scott Buxton, Vidya Acharya, Johnathan Fahrner, Rebecca Willis, Liesel Muyelle, Liese Bosman, Blessed Denzel Vhudzijena, George Prudden, Aminat Abolade, WikiSysop, Heleen.Mergan, Karen Wilson, 127.0.0.1, Kenny Bosmans, Laura Mertens, Uchechukwu Chukwuemeka, Shaimaa Eldib, Evan Thomas, Redisha Jakibanjar, Samuel Adedigba, Lauren Lopez and Daniele Barilla
Description[edit | edit source]
Total hip replacement (THR), or Total Hip Arthroplasty (THA), is a procedure that removes damaged bone and cartilage and replaces it with prosthetic components. THR is one of the most cost-effective and consistently successful surgeries performed in orthopaedics.
- THR provides good outcomes for patients suffering from advanced degenerative hip osteoarthritis, providing pain relief, functional restoration, and improved quality of life.[1][2]
- During a THR, the head of the femur is replaced with a prosthetic head on a shaft, and the joint surface of the acetabulum is lined with a bowl-shaped synthetic joint surface.
- A partial hip replacement can also be done for neck of femur fractures (mostly displaced)[3] where only the femoral part is replaced.
Clinically Relevant Anatomy[edit | edit source]
The hip is a ball and socket joint. This design allows the poly-axial movement seen at the hip.
The head of the femur and the inside of the acetabulum are covered with a layer of hyaline cartilage.[4] Once this cartilage is worn away or damaged (usually by arthritis), the underlying bone is exposed, resulting in pain, stiffness and possibly shortening of the affected leg. By replacing these surfaces the aim is to reduce pain and stiffness to restore an active and pain-free life.
THR is mostly done electively.[5][6][7][8]
Indications for Surgery[edit | edit source]
The most common indication for THA hip OA. Other indications include:[9]
- Trauma: can be considered in a case by case basis in Femoral Neck Fractures (displaced intracapsular) in active and healthy patients
- Osteonecrosis of the hip, commonly known as avascular necrosis of the hip[10]
- Developmental dysplasia of the hip
- Hardware failure after internal fixation of hip fractures[1]
Complications[edit | edit source]
Complications following THR can be loosely divided into systemic and procedure specific complications. Incidence of complications have improved over time, due to surgical and anaesthetic technique improvements, along with the better diagnosis and management of these complications.
The most common systemic complication is a deep vein thrombosis. Infection is the most dreaded complication. Leg length discrepancy is a common cause of patient dissatisfaction[11]. For more see Total Hip Replacement Complications.
Contraindications for Surgery[edit | edit source]
THA is contraindicated in the following clinical scenarios:
- Local: Septic (Infectious) Arthritis
- Remote (i.e. extra-articular) active, ongoing infection or bacteraemia.
- Severe cases of Peripheral Vascular Disease [12]
Orthopaedic Assessment[edit | edit source]
An assessment by an orthopaedic surgeon consists of several components:
- Medical history: general health and questions about the extent of hip pain and how it affects ability to perform ADLs.
- Hip Examination
- X-rays. Assess the extent of damage or deformity in the hip.
- Other tests. Occasionally other tests, e.g., MRI scan, may be needed to determine the condition of the bone and soft tissues of the hip.
The diagnosis of patients requiring THR is mostly symptom-based. Pain, loss of range of motion and functional impairments are mostly considered.[13]
Prosthesis[edit | edit source]
When performing a THR, the ball is removed, socket reshaped, and the artificial implant is positioned in the bone. The implant may be held in the bone by tightly wedging it in place, or cementing into position. Type of fixation used depends on the patient's bone health and the design of the implant. Contemporary THR techniques have evolved into press-fit femoral and acetabular components, and many variations exist.[14] The basic components are:
- Bearing surfaces are the surfaces which articulate in the prosthetic joint. The femoral head and the acetabular liner can be used in different combinations. These will give different appearance on radiograph depending on the configuration. Many options are available e.g., Metal-on-polyethylene, Ceramic-on-polyethylene, Ceramic-on-ceramic, Metal-on-metal.[1]
- Femoral component or stem: this refers to the prosthesis which is implanted into the femur. They can be described by length, taper, and presence of a collar. Attached to the femoral component is the neck and head which in most prostheses can be altered in size to create a stable joint[15].
- Prosthesis fixation: Femoral stem fixation can be either cemented or non-cemented (biological) fixation[15]. Prevalence of fixation technique: increasing trend towards cementless fixation; 93% of THA in United States in 2012 were cementless[16]
Surgical Approaches[edit | edit source]
Any number of approaches can be used for the THA procedure. The three most common approaches are:
- Posterior (PA): Most common surgical approach for THR. Major advantage of this approach is the avoidance of the hip abductors. Performed with a patient lying on their side and a surgical incision made along the outside of the hip.[17]
- Direct Anterior (DA): This surgical procedure has been increasing over the past decade. This approach is performed with a patient lying on their back, and a surgical incision is made coming down the front of the thigh (between the tensor fascia lata and sartorius on the superficial end, and the gluteus medius and rectus femoris on the deep side). There are several potential advantages of the direct anterior approach. The two most prominent are a low dislocation risk and early postoperative recovery.[17]Perception is that DAA results in less tissue damage, however this lacks support in the literature.[18]
- Direct lateral (Hardinge) or anterolateral: Often considered to be a balance between the AP and PA. Person positioned on their side, and the surgical incision is placed directly down the outside of the hip. The advantage: balance of having a versatile incision that can be used to correct deformities and insert specialised implants with lower dislocation rates following surgery than what is observed with posterior approaches. Disadvantage: superior gluteal nerve dissection may result in nerve injury, leading to postoperative Trendelenburg gait, characterized by compensatory movements to address hip abductor weakness. [17]
Additionally
- Robotic Arm Assisted THR: Assists with THR surgery, helping in the accurate positioning of the implants which correlates with improved function and lifespan of the THR. Can be used in all current surgical approaches to the hip (AP, PA and lateral).
- Minimally invasive surgery is becoming popular all around the world, due to the quicker recovery rates and reduced postoperative pain. Long term follow-up and comparison studies are still needed in this field.[19]
View this 3 minute video and learn about the different approaches to hip replacement surgery and the advantages of each method.
Physiotherapy Management[edit | edit source]
Plenty of questions remain concerning the most effective rehabilitation management of patients following a THA. This uncertainty exists as a comparison of the effectiveness and harms of interventions is difficult due to the diverse programs, frequently inadequate intervention description, and an extensive variety of outcomes reported across research. What is needed are well-conducted studies that address both effectiveness and harms of interventions using randomised controlled trials.[21]
Discuss Hip precautions before surgery.
- PA avoid: flexion past 90 degrees; extreme internal rotation; adduction past body's midline
- Anterolateral approach avoid: extension; extreme external rotation; adduction past the body's midline
- AP avoid: bridging; extension; extreme external rotation; adduction past body's midline[16]
Hip precautions have traditionally been used within the management of total hip arthroplasty to reduce the risk of dislocations [22]. This is particularly needed to provide safe boundaries for movement when patients are keen to “push” those boundaries soon after surgery or have other risk factors such as abductor deficiency with a history of previous dislocations, loose soft tissues, patients with neuromuscular and cognitive disorders[23]. However, their use is increasingly controversial due to their association with a slower return to activities, an absence in the rise of dislocation rates when precautions are not used, and a lack of evidence to support their use [24][23].
Pre-operative[edit | edit source]
One on one preoperative physical therapy session protocol is effective at reducing the number of postoperative PT visits and time for readiness to discharge from PT. It plays an important role towards improving preoperative quality of life (people can wait many months for surgery and experience further deterioration in health-related quality of life during long waits).[25]See also Physical Activity Pre and Post Surgery
Pre-operative assessment and treatment session
- Helps to develop a patient-specific rehabilitation programme to follow post-operative, taking assessment findings into consideration e.g., Does the patient desires to re uptake golf.
- Benefits: decreased length of stay[26]; decreased anxiety levels[27]; improved self-confidence[28]; establish a relationship of trust between the physiotherapist and patient.
- A combination of verbal explanation and written pamphlets is the best method for health education.[27] Important to incorporate this into the pre-operative physiotherapy management of patients prior to total hip replacements (linked to better post-operative adherence).[27]
Pre op Assessment
- Subjective history
- Range of motion
- Muscle power
- Circulation
- Mobility and function[28]
Pre op Treatment
- Education and advice: Patient information booklet; Precautions and contraindications; Rehabilitation process; Goals & expectations; Functional/ADL adaptions; Safety principles
- Encourage to stop smoking if applicable
- Discharge planning
- Teach: Bed exercises; Transfers in and out of bed (within precautions)
- Gait re-education with mobility assistive device (crutches vs walkers)
- Stair climbing
Post-operative[edit | edit source]
Start the day of surgery as leads to decreased length of stay, reduces pain and improves function.
- Aim of post-operative rehabilitation: address the functional needs of the patient (e.g. start mobilizing) and to improve mobility, strength, flexibility and reduce pain.[7] . This starts off as an assisted process, but the aim is to get the patient as functional as possible prior to discharge.
- As a result of the underlying pre-operative pathology, patients may present with muscle atrophy and loss of strength, particularly in the gluteus medius and quadriceps muscles. The result of the loss of strength is that the elderly are less independent.[5]
- Surgery will correct the joint problems but associated muscle weakness that was present before the surgery will remain and require post-operative rehabilitation (research has shown hip abductor weakness after surgery is a major risk associated with joint instability and prosthetic loosening).[6] Patients can achieve significant improvements through a targeted strengthening programme following total hip replacement.[29] Motor Imagery training, has been found to be a useful adjunct therapy tool as it improves both specific and general adaptations that were related to patients’ physical capabilities when added in a corollary to routine physical therapy.[30]
- No specific general hip replacement protocol is currently in use, as small elements of the rehabilitation process are surgeon specific. For example, in some enhanced recovery after surgery protocols, patients are mobilised out of bed within the first 6 hours post-surgery. Other settings may only start mobilizing patients out of bed on day 1 or 2 post-surgery. Accelerated rehabilitation programmes and early mobilization have shown to give patients more confidence in their post-operative mobilization and activities of daily living, as well as being more comfortable with earlier discharge.[31]
Evidence[edit | edit source]
Physiotherapy: can improve strength and gait speed after total hip replacement and help prevent complications such as subluxation and thromboembolic disease; increases the patient’s mobility and offers education about the exercises and precautions that are necessary during hospitalization and after discharge.[32]; maximizes the patient’s function which is associated with a greater probability of earlier discharge, which is in turn associated with a lower total cost of care[33]
- Bed exercise following a total hip replacement important for the effects on oedema, cardiac function and improving range of motion and muscle strength[34].
- Early weight bearing and physical activity have benefits for the quality of bone tissue[35], improving the fixation of the prosthesis and decreases the incidence of early loosening. The amount of activity is patient-specific, and clinical reasoning should be used to make adaptions where needed. Certain specific sport movements have a higher risk of injury for unskilled individuals, and should be incorporated later in the rehabilitation process under supervision of a physiotherapist.
Suggested protocol in the absence of complications: Surgeon preference should be taken into account, as well as any other factors that might hinder the following of the protocol. Adaptions should be made to make it more patient specific.[28][36]
Day 1 Post-Surgery[edit | edit source]
- Education and advice
- Education of muscular relaxation
- Revision of precautions and contraindications (provided that patient had a pre-operative session with the physiotherapist, otherwise full education will be done as mentioned in pre-operative section).
- Bed exercises:
- Circulation drills
- Upper limb exercises to stimulate the cardiac function
- Maintenance of the non-operated leg: attention should be paid to the range of motion in order to preserve controlled mobilisation on the operated hip
- Isometric quadriceps (progressing to concentric VMO) and gluteal contractions
- Active-assisted (progressing to active) heel slides, hip abduction/adduction
- Bed mobilisation using unilateral bridging on the unaffected leg
- Getting in and out of bed (see here)
- Getting on and off a chair with arms (see here)
- Sit to stand with mobility assistive device (preferably a device giving more support like a walking frame or rollator)
- Gait re-education with mobility assistive device as tolerated (weight bearing status as determined by surgeon)
- Sitting out in chair for maximum 1 hour
- Positioning when transferred back to bed
Day 2 Post-Surgery[edit | edit source]
- Bed exercises as described above, progressing repetitions and decreasing assistance given to patient
- Progression of distance mobilised and/or mobility assistive device
- Incorporate balance exercises if needed
- Sitting in chair
Day 3 Post-Surgery[edit | edit source]
Bed exercises as described above, progressing repetitions and decreasing assistance given to patient
- Progression of distance mobilised and/or mobility assistive device
- Stair climbing (at least 3, or as per home requirements)
- Sitting in chair
- Revision of precautions, contraindications and functional adaptions
- Give 6 week progressive resistive strengthening home exercise to patient; this can include stationary cycling, as long as the patient stays within the precautions (especially posterior approach surgery)
After 3 days clients are usually discharged home if they meet the discharge criteria. The physiotherapist and nurse help to transfer to a car whilst maintaining hip precautions. As majority of patients lack understanding about the activities they can do following THR surgery, discharge education about pre-discharge pain management, movement, ADL, and support requirements should be provided to the clients. A recent RCT showed that video-assisted discharge program and education booklets given to the patient and their relatives after THR on activities of daily living, functionality, and patient satisfaction found that video-assisted discharge program along with physiotherapy reduced pain perception and kinesiophobia, improve hip function, and increase patient satisfaction. Further research is needed to assess the long-term outcomes of video-assisted discharge education in THR patients.[37]
Discharge Home Criteria:[edit | edit source]
- independent ambulation with assistive device
- independent transfers
- independent ADLs
- stairs with supervision
- appropriate home assistance (spouse, family, visiting nurses)[16]
Home Planning[edit | edit source]
Several modifications to make home easier to navigate. The following items help with daily activities:
- Securely fastened safety bars or handrails in shower or bath
- Secure handrails along all stairways
- A stable chair for your early recovery with a firm seat cushion (allows knees to remain lower than hips), a firm back, and two arms
- A raised toilet seat
- A stable shower bench or chair for bathing
- A long-handled sponge and shower hose
- A dressing stick, a sock aid, and a long-handled shoehorn
- A reacher allowing grasping of objects without excessive bending of your hips
- Firm pillows for chairs, sofas, and car enabling client to sit with knees lower than hips
- Removal of all loose carpets and electrical cords from the areas walked in home[16]
This 7 minute video presents post-operative exercises after a total hip replacement for weeks 1-4.
6 Weeks Post Surgery[edit | edit source]
- Patients are normally followed up by orthopaedic surgeon
- Surgeon determines if the patient is allowed the following:
- Full range of motion at the hip
- Full weight bearing without mobility assistive device
- Driving
After 6 Weeks[edit | edit source]
- Gain of initial ROM, stabilization, and proprioception
- Endurance
- Flexibility
- Balance
- Speed, precision, neurological coordination
- Functional exercises
Return to sport[edit | edit source]
Low-impact exercises are preferred
- golf: handicap shows minimal change after THA; handicap shows increase after TKA
- high-impact exercises increase revision rates in patients less than 55 years-old
Outcome Measures[edit | edit source]
- Harris Hip Score
- Oxford Hip Score (OHS)
- 6 Minute Walking Test
- Timed Get Up & Go Test
- Western Ontario and McMaster universities osteoarthritis index (WOMAC)
- SF-36
- Fear Avoidance Belief Score
- Hip Disability & Osteoarthritis Outcome Score (HOOS)
- International Hip Outcome Tool
- Ibadan Knee/Hip Osteoarthritis Outcome Measure
Team Work[edit | edit source]
Total hip arthroplasty (THA) is one of the most reliable, reproducible, successful, and cost-effective procedures in all of orthopedics. The procedure requires coordination of care across various healthcare provider groups, including nurses, physical therapists, advanced practitioners and physician extenders, medical physicians, and orthopedic surgeons.
Clinicians including the surgeon, nurse practitioner, and physiotherapist should work together to provide the patient and family with education regarding the procedure, expected issues, and guidance for aftercare.[1]
Virtual Clinic Visits[edit | edit source]
Virtual follow-up for hip and knee arthroplasty patients is an effective substitute to in-person clinic assessment, substantiated in a recent investigation including 1,749 patients seen in a virtual visit between January 2017 and December 2018.
- For the 1-year postoperative visit and routine scheduled follow-up visits, only 7.22% of the patients required a further in-person assessment.
- Is accepted by patients, has high patient satisfaction, and can reduce the cost to both health services and patients.[39]
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 Varacallo M, Luo TD, Johanson NA. Total Hip Arthroplasty Techniques. InStatPearls [Internet] 2020 Jul 8. StatPearls Publishing.Available from: https://www.statpearls.com/articlelibrary/viewarticle/22894/ (accessed 14.2.2021)
- ↑ Levine BR, Klein GR, Cesare PE. Surgical approaches in total hip arthroplasty: A review of the mini-incision and MIS literature. Bulletin of the NYU Hospital for Joint Diseases 2007;65(1):5-18.
- ↑ Iglesias SL, Gentile L, Mangupli MM, Pioli I, Nomides RE, Allende BL. Femoral neck fractures in the elderly: from risk factors to pronostic features for survival. Journal of Trauma and Critical Care. 2017;1(1).
- ↑ Meyers HM. Fractures of the hip. Chicago: Year of the book medical publishers Inc., 1985
- ↑ 5.0 5.1 Gremeaux V, Renault J, Pardon L, Deley G, Lepers R, Casillas JM. Low-frequency electric muscle stimulation combined with physical therapy after total hip arthroplasty for hip osteoarthritis in elderly patients: a randomized controlled trial. Archives of physical medicine and rehabilitation 2008;89(12):2265-73.
- ↑ 6.0 6.1 Jan MH, Hung JY, Lin JC, Wang SF, Liu TK, Tang PF. Effects of a home program on strength, walking speed, and function after total hip replacement. Archives of physical medicine and rehabilitation 2004 ;85(12):1943-51.
- ↑ 7.0 7.1 Stockton KA, Mengersen KA. Effect of multiple physiotherapy sessions on functional outcomes in the initial postoperative period after primary total hip replacement: a randomized controlled trial. Archives of physical medicine and rehabilitation 2009;90(10):1652-7.
- ↑ Rahmann AE, Brauer SG, Nitz JC. A specific inpatient aquatic physiotherapy program improves strength after total hip or knee replacement surgery: a randomized controlled trial. Archives of physical medicine and rehabilitation 2009;90(5):745-55.
- ↑ Affatato S. Perspectives in total hip arthroplasty: Advances in biomaterials and their tribological interactions. London: Woodhead Publishing, 2014.
- ↑ Hsu H, Nallamothu SV. Hip Osteonecrosis.Available:https://www.ncbi.nlm.nih.gov/books/NBK499954/ (accessed 9.12.2022)
- ↑ Park C, Merchant I. Complications of total hip replacement. InTotal Hip Replacement-An Overview 2018 Nov 5. IntechOpen. Available:https://www.intechopen.com/chapters/61241 (accessed 8.12.2022)
- ↑ Varacallo M, Luo TD, Johanson NA. Total Hip Arthroplasty Techniques. InStatPearls [Internet] 2020 Jul 8. StatPearls Publishing.Available from:https://www.statpearls.com/articlelibrary/viewarticle/22894/ (accessed 14.2.2021)
- ↑ Crawford AJ, Hamblen DL. Outline of Orthopaedics , thirteenth edition, London: Churchill Livingstone, 2001
- ↑ Very well health What Type of Hip Replacement Implant Is Best? Available:https://www.verywellhealth.com/what-type-of-hip-replacement-implant-is-best-2549558#citation-2 (accessed 8.12.2022)
- ↑ 15.0 15.1 Radiopedia THR Available from:https://radiopaedia.org/articles/total-hip-arthroplasty (accessed 14.2.2021)
- ↑ 16.0 16.1 16.2 16.3 Ortho bullets THR Available from:https://www.orthobullets.com/recon/5003/tha-implant-fixation (accessed 14.2.2021)
- ↑ 17.0 17.1 17.2 Varacallo M, Luo TD, Johanson NA. Total hip arthroplasty techniques. InStatPearls [Internet] 2022 Sep 4. StatPearls Publishing.Available:https://www.ncbi.nlm.nih.gov/books/NBK507864/ (accessed 8.12.2022)
- ↑ Mead PA, Bugbee WD. Direct anterior approach to total hip arthroplasty improves the likelihood of return to previous recreational activities compared with posterior approach. JAAOS Global Research & Reviews. 2022 Jan;6(1).Available: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8735710/ (accessed 8.1.2024)
- ↑ Alecci V, Valente M, Crucil M, Minerva M, Pellegrino C, Sabbadini DD. Comparison of primary total hip replacements performed with a direct anterior approach versus the standard lateral approach: perioperative findings. J Orthopaed Traumatol 2011;12:123-129.
- ↑ John Hopkins Medical. Approaches to Hip Replacement Surgery | Dr. Savya Thakkar. Available from: https://www.youtube.com/watch?v=1cUu-vMcSkM [last accessed 8.12.2022]
- ↑ Konnyu KJ, Pinto D, Cao W, Aaron RK, Panagiotou OA, Bhuma MR, Adam GP, Balk EM, Thoma LM. Rehabilitation for Total Hip Arthroplasty: A Systematic Review. Am J Phys Med Rehabil. 2023 Jan 1;102(1):11-18. doi: 10.1097/PHM.0000000000002007. Epub 2022 Mar 12. PMID: 35302955; PMCID: PMC9464790.Accessed 8.1.204 Available:https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9464790/
- ↑ Coole C, Edwards C, Brewin C, Drummond A. What do clinicians think about hip precautions following total hip replacement? Br J Occup Ther. 2013;76:7:300-307.
- ↑ 23.0 23.1 Mandel RT, Bruce G, Moss R, Carrington RWJ, Gilbert AW. Hip precautions after primary total hip arthroplasty: a qualitative exploration of clinical reasoning. Disab Rehab. 2022;44:12:2842–2848
- ↑ Barnsley L, Leslie Barnsley L, Page R. Are Hip Precautions Necessary Post Total Hip Arthroplasty? A Systematic Review. Geriatr Orthop Surg Rehabil. 2015;6:3:230-235
- ↑ Soeters R, White PB, Murray-Weir M, Koltsov JC, Alexiades MM, Ranawat AS. Preoperative physical therapy education reduces time to meet functional milestones after total joint arthroplasty. Clinical orthopaedics and related research. 2018 Jan;476(1):40.Available: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5919221/ (accessed 89.12.2022)
- ↑ Crowe J,Henderson J. Pre-arthroplasty rehabilitation is effective in reducing length of hospital stay. Canadian Journal of Occupational Therapy 2003;70:88-96.
- ↑ 27.0 27.1 27.2 Barnes RY, Bodenstein, K, Human N. Raubenheimer J, Dawkins J, Seesink C, Jacobs J, van der Linde J, Venter R. Preoperative education in hip and knee arthroplasty patients in Bloemfontein. South African Journal of Physiotherapy 2018;74(1).
- ↑ 28.0 28.1 28.2 Raymond Sohier, Kinesitherapie de la hanche ; La Hestre : Sohier, 1974
- ↑ Galea MP, Levinger P, Lythgo N, Cimoli C, Weller R, Tully E, McMeeken J, Westh R. A targeted home-and center-based exercise program for people after total hip replacement: a randomized clinical trial. Archives of physical medicine and rehabilitation 2008;89(8):1442-7.
- ↑ Paravlic AH, Pisot R, Marusic U. Specific and general adaptations following motor imagery practice focused on muscle strength in total knee arthroplasty rehabilitation: A randomized controlled trial. PloS one. 2019;14(8).
- ↑ Robertson NB, Warganich T, Ghazarossian J, Khatod M. Implementation of an accelerated rehabilitation protocol for total joint arthroplasty in the managed care setting: the experience of one institution. Advances in Orthopedic Surgery. 2015;387197.
- ↑ Coulter CL, Scarvell JM, Neeman TM, Smith PN. Physiotherapist-directed rehabilitation exercises in the outpatient or home setting improve strength, gait speed and cadence after elective total hip replacement: a systematic review. Journal of physiotherapy. 2013;59(4):219-26.
- ↑ Freburger J. An analysis of the relationship between the utilization of physical therapy services and outcomes of care for patients after total hip arthroplasty. Physical therapy 2000;80(5):448-458.
- ↑ Perhonen MA, Franco F, Lane LD, Buckey JC, Blomqvist CG, Zerwekh JE, Peshock RM, Weatherall PT, Levine BD. Cardiac atrophy after bed rest and spaceflight. Journal of applied physiology 2001;91(2):645-53.
- ↑ Mahendra G, Pandit H, Kliskey K, Murray D, Gill HS, Athanasou N. Necrotic and inflammatory changes in metal-on-metal resurfacing hip arthroplasties: relation to implant failure and pseudotumor formation. Acta orthopaedica 2009;80(6):653-9.
- ↑ Suetta C, Aagaard P, Rosted A, Jakobsen AK, Duus B, Kjaer M, Magnusson SP. Training-induced changes in muscle CSA, muscle strength, EMG, and rate of force development in elderly subjects after long-term unilateral disuse. Journal of Applied Physiology 2004;97(5):1954-61.
- ↑ Cetinkaya Eren O, Buker N, Tonak HA, Urguden M. The effect of video-assisted discharge education after total hip replacement surgery: a randomized controlled study. Scientific Reports. 2022 Feb 23;12(1):1-9.
- ↑ HeartlandOrthospecial. Post-Operative Exercises Weeks 1-4 for Total Hip Replacement. Available from: https://www.youtube.com/watch?v=9eU8G038zFo[last accessed 24.3.2023]
- ↑ El Ashmawy AA, Dowson K, El-Bakoury A, Hosny HA, Yarlagadda R, Keenan J. Effectiveness, patient satisfaction, and cost reduction of virtual joint replacement clinic follow-up of hip and knee arthroplasty. The Journal of arthroplasty. 2021 Mar 1;36(3):816-22.Available:https://pubmed.ncbi.nlm.nih.gov/32893060/ (accessed 6.12.2022)