Total Hip Replacement: Difference between revisions
No edit summary |
No edit summary |
||
| Line 5: | Line 5: | ||
</div> | </div> | ||
== Description == | == Description == | ||
Total hip arthroplasty (THA) is one of the most cost-effective and consistently successful surgeries performed in orthopaedics. THA provides reliable outcomes for patients’ suffering from end-stage degenerative hip osteoarthritis (OA), specifically pain relief, functional restoration, and overall improved quality of life<ref name=":5">Varacallo M, Luo TD, Johanson NA. [https://www.statpearls.com/articlelibrary/viewarticle/22894/ Total Hip Arthroplasty Techniques.] InStatPearls [Internet] 2020 Jul 8. StatPearls Publishing.Available from: https://www.statpearls.com/articlelibrary/viewarticle/22894/ (accessed 14.2.2021)</ref>.[[File:THR X-ray.jpg|thumb|350x350px|THR X-ray]]A total hip replacement is a surgical procedure in which both damaged surfaces of the [[Hip|hip joint]] are replaced with prosthetic substitutes. It was first performed in the 1960's and is said to be one of the most successful surgeries in the last few decades.<ref>Levine BR, Klein GR, Cesare PE. [https://www.researchgate.net/profile/Paul_Dicesare/publication/6296081_Surgical_approaches_in_total_hip_arthroplasty_A_review_of_the_mini-incision_and_MIS_literature/links/0f31752dc21c0f154c000000.pdf Surgical approaches in total hip arthroplasty: A review of the mini-incision and MIS literature.] Bulletin of the NYU Hospital for Joint Diseases 2007;65(1):5-18.</ref> | Total hip arthroplasty (THA) is one of the most cost-effective and consistently successful surgeries performed in orthopaedics. THA provides reliable outcomes for patients’ suffering from end-stage degenerative hip osteoarthritis (OA), specifically pain relief, functional restoration, and overall improved quality of life<ref name=":5">Varacallo M, Luo TD, Johanson NA. [https://www.statpearls.com/articlelibrary/viewarticle/22894/ Total Hip Arthroplasty Techniques.] InStatPearls [Internet] 2020 Jul 8. StatPearls Publishing.Available from: https://www.statpearls.com/articlelibrary/viewarticle/22894/ (accessed 14.2.2021)</ref>.[[File:THR X-ray.jpg|thumb|350x350px|THR X-ray]]A total hip replacement is a surgical procedure in which both damaged surfaces of the [[Hip|hip joint]] are replaced with prosthetic substitutes. It was first performed in the 1960's and is said to be one of the most successful surgeries in the last few decades.<ref>Levine BR, Klein GR, Cesare PE. [https://www.researchgate.net/profile/Paul_Dicesare/publication/6296081_Surgical_approaches_in_total_hip_arthroplasty_A_review_of_the_mini-incision_and_MIS_literature/links/0f31752dc21c0f154c000000.pdf Surgical approaches in total hip arthroplasty: A review of the mini-incision and MIS literature.] Bulletin of the NYU Hospital for Joint Diseases 2007;65(1):5-18.</ref> | ||
During a hip replacement, the head of the femur is replaced with a [[Prosthetics|prosthetic]] head on a shaft, and the joint surface of the [[Acetabulum fracture|acetabulum]] is lined with a bowl-shaped synthetic joint surface. A partial replacement can also be done for neck of [[femur]] [[Fracture|fractures]] (mostly displaced)<ref>Iglesias SL, Gentile L, Mangupli MM, Pioli I, Nomides RE, Allende BL. [http://www.alliedacademies.org/articles/femoral-neck-fractures-in-the-elderly-from-risk-factors-to-pronostic-features-for-survival.pdf Femoral neck fractures in the elderly: from risk factors to pronostic features for survival.] Journal of Trauma and Critical Care. 2017;1(1).</ref> where only the femoral part is replaced. | During a hip replacement, the head of the femur is replaced with a [[Prosthetics|prosthetic]] head on a shaft, and the joint surface of the [[Acetabulum fracture|acetabulum]] is lined with a bowl-shaped synthetic joint surface. A partial replacement can also be done for neck of [[femur]] [[Fracture|fractures]] (mostly displaced)<ref>Iglesias SL, Gentile L, Mangupli MM, Pioli I, Nomides RE, Allende BL. [http://www.alliedacademies.org/articles/femoral-neck-fractures-in-the-elderly-from-risk-factors-to-pronostic-features-for-survival.pdf Femoral neck fractures in the elderly: from risk factors to pronostic features for survival.] Journal of Trauma and Critical Care. 2017;1(1).</ref> where only the femoral part is replaced. | ||
== Clinically Relevant Anatomy == | == Clinically Relevant Anatomy == | ||
| Line 20: | Line 20: | ||
== Clinical Presentation == | == Clinical Presentation == | ||
[[File:Neck of femur fracture (garden IV).jpeg|Neck of femur fracture|right|frameless]] | |||
=== Preoperative === | === Preoperative === | ||
* [[Hip Fracture|Neck of femur fractures]]: Often unable to walk, complains of vague pain in the knee, thigh, groin, back or buttock and difficulty of weight bearing <ref name="Batra S.">Batra S, Batra M, McMurtrie A, Sinha AK. [https://josr-online.biomedcentral.com/articles/10.1186/1749-799X-3-3 Rapidly destructive osteoarthritis of the hip joint: a case series.] Journal of orthopaedic surgery and research 2008;3(1):3.</ref>. Impacted femur neck on X-ray. | * [[Hip Fracture|Neck of femur fractures]]: Often unable to walk, complains of vague pain in the knee, thigh, groin, back or buttock and difficulty of weight bearing <ref name="Batra S.">Batra S, Batra M, McMurtrie A, Sinha AK. [https://josr-online.biomedcentral.com/articles/10.1186/1749-799X-3-3 Rapidly destructive osteoarthritis of the hip joint: a case series.] Journal of orthopaedic surgery and research 2008;3(1):3.</ref>. Impacted femur neck on X-ray. | ||
* [[Hip Osteoarthritis|Osteoarthritis]]: Sensible or audible crepitations on movement, inability to assume the neutral anatomical position. Often also linked with painful and/or decreased range of motion. X-ray findings commonly include decreased joint space, subchondral sclerosis, cyst formation and osteophytes.<ref>Brandt CD. [https://books.google.co.za/books?hl=en&lr=&id=Ha2gtfP8QkAC&oi=fnd&pg=PR13&dq=Diagnosis+and+non-surgical+management+of+osteoarthritis&ots=7tQ-oJS5VM&sig=HwFI6eIUMVWltPAj84y2yBP3sZg#v=onepage&q=Diagnosis%20and%20non-surgical%20management%20of%20osteoarthrit Diagnosis and non-surgical management of osteoarthritis]. USA: Professional Communications, Inc. 2010</ref>[[File:Hip OA.jpg| | * [[Hip Osteoarthritis|Osteoarthritis]]: Sensible or audible crepitations on movement, inability to assume the neutral anatomical position. Often also linked with painful and/or decreased range of motion. X-ray findings commonly include decreased joint space, subchondral sclerosis, cyst formation and osteophytes.<ref>Brandt CD. [https://books.google.co.za/books?hl=en&lr=&id=Ha2gtfP8QkAC&oi=fnd&pg=PR13&dq=Diagnosis+and+non-surgical+management+of+osteoarthritis&ots=7tQ-oJS5VM&sig=HwFI6eIUMVWltPAj84y2yBP3sZg#v=onepage&q=Diagnosis%20and%20non-surgical%20management%20of%20osteoarthrit Diagnosis and non-surgical management of osteoarthritis]. USA: Professional Communications, Inc. 2010</ref>[[File:Hip OA.jpg|Hip osteoarthritis|right|frameless]] | ||
* [[Rheumatoid Arthritis|Rheumatoid arthritis]]: Range of all hip movements are impaired, movement is painful, pain and stiffness when the activity is resumed after resting. <ref name="Crawford A." /> | * [[Rheumatoid Arthritis|Rheumatoid arthritis]]: Range of all hip movements are impaired, movement is painful, pain and stiffness when the activity is resumed after resting. <ref name="Crawford A." /> | ||
*[[Avascular necrosis of the femoral head|Avascular necrosis]]: Similar signs as with osteoarthritis, often also with referred knee pain.<ref name=":1">Walters J, editor. Orthopaedics - A guide for practitioners. 4th Edition. Cape Town: University of Cape Town, 2010.</ref> | *[[Avascular necrosis of the femoral head|Avascular necrosis]]: Similar signs as with osteoarthritis, often also with referred knee pain.<ref name=":1">Walters J, editor. Orthopaedics - A guide for practitioners. 4th Edition. Cape Town: University of Cape Town, 2010.</ref> | ||
[[File:AVN.JPG| | [[File:AVN.JPG|Avascular necrosis|right|frameless]] | ||
== Indications for Surgery == | == Indications for Surgery == | ||
| Line 70: | Line 70: | ||
* Other: [[CT Scans|CT]], [[MRI Scans|MRI]] | * Other: [[CT Scans|CT]], [[MRI Scans|MRI]] | ||
== | == Prosthesis == | ||
[[File:Hip prosthesis.jpg|thumb|260x260px|Hip prosthesis (titanium), with a ceramic head and polyethylene acetabular cup]]THA prosthetic designs have been evolving since their inception. | |||
Contemporary THA techniques have evolved into press-fit femoral and acetabular components. In general, femoral stems can be categorized into the following general designs: | |||
* Press-fit, proximally coated, distal taper (dual or single tapered in medial-lateral and/or anterior-posterior planes) | |||
* Press-fit, extensively coated, diaphyseal engaging | |||
* Press-fit, Modular stems: Modularity junction options include: (1) head-neck, (2) neck-stem, (3) stem-sleeve, and (4) mid-stem | |||
* Cemented femoral stems: Cobalt-chrome stems are the preferred material to promote cement bonding | |||
Options for bearing surfaces include: | |||
* Metal-on-polyethylene (MoP): MoP has the longest track record of all bearing surfaces at the lowest cost | |||
* Ceramic-on-polyethylene (CoP): becoming an increasingly popular option | |||
* Ceramic-on-ceramic (CoC): CoC has the best wear properties of all THA bearing surfaces | |||
* Metal-on-metal (MoM): Although falling out of favor, MoM has historically demonstrated better wear properties from its MoP counterpart. MoM has lower linear-wear rates and decreased volume of particles generated. However, the potential for pseudotumor development as well as metallosis-based reactions (type-IV delayed hypersensitivity reactions) has resulted in a decline in the use of MoM. MoM is also contraindicated in pregnant women, patients with renal disease, and patients at risk of metal hypersensitivity.<ref name=":5" /> | |||
Important components of prosthesis are friction-coefficient, survival, stability against dislocation and fixation in bone tissue<ref name="Bader">Bader R, Steinhauser E, Zimmermann S, Mittelmeier W, Scholz R, Busch R. [https://link.springer.com/article/10.1023/B:JMSM.0000030214.79180.13 Differences between the wear couples metal-on-polyethylene and ceramic-on-ceramic in the stability against dislocation of total hip replacement.] Journal of materials science: materials in medicine 2004;15(6):711-8.</ref><ref name="Garcia">Garcia-Rey E, Cruz-Pardos A, Garcia-Cimbrelo E. [https://link.springer.com/article/10.1007/s11999-009-0904-9 Alumina-on-alumina total hip arthroplasty in young patients: diagnosis is more important than age.] Clinical Orthopaedics and Related Research 2009;467(9):2281-9.</ref>. In some cases there can be formation of [http://www.physio-pedia.com/index.php5?title=Avascular_Necrosis osteonecrosis] due to erosion of the two components rubbing against each other<ref name="Mahendra">Mahendra G, Pandit H, Kliskey K, Murray D, Gill HS, Athanasou N. [https://www.tandfonline.com/doi/full/10.3109/17453670903473016 Necrotic and inflammatory changes in metal-on-metal resurfacing hip arthroplasties: relation to implant failure and pseudotumor formation.] Acta orthopaedica 2009;80(6):653-9.</ref>. Recent studies have shown that Vitamin E infused polyethylene provides 95% less wear when compared to other liners.<ref>Zimmer Biomet. The E1™ Antioxidant Infused Technology Process. http://www.biomet.fi/viewversion.cfm?contentversionid=36999&sc=1 (accessed 2506/2018).</ref><ref>Lindalen L, Nordsletten L, Høvik Ø, Röhrl SM. [https://www.researchgate.net/profile/Stephan_Rohrl/publication/271594087_E-vitamin_infused_highly_cross-linked_polyethylene_RSA_Results_from_a_Randomised_Controlled_Trial_using_32_mm_and_36_mm_ceramic_heads/links/55d1c26808ae3dc86a4f2e09/E-vitamin-infused-highly-cross-linked-polyethylene-RSA-Results-from-a-Randomised-Controlled-Trial-using-32-mm-and-36-mm-ceramic-heads.pdf E-Vitamin Infused Highly Cross-Linked Polyethylene: RSA Results from a Randomised Controlled Trial Using 32 mm and 36 mm Ceramic Heads]. Hip International 2015;25(1):50 - 55</ref> | |||
== Surgical Approaches == | |||
# Posterior | |||
This is the most common approach for primary and revision THA cases. This dissection does not utilize a true internervous plane. The intermuscular interval involves blunt dissection of the gluteus maximus fibers and sharp incision of the fascia lata distally. The deep dissection involves meticulous dissection of the short external rotators and capsule. A major advantage of this approach is the avoidance of the hip abductors. | |||
2. Direct Anterior (DA) | |||
The DA approach is becoming increasingly popular among THA surgeons. The internervous interval is between the tensor fascia lata (TFL, superior gluteal nerve) and sartorius (femoral nerve) on the superficial end, and the gluteus medius (superficial gluteal nerve) and rectus femoris (RF, femoral nerve) on the deep side. DA THA advocates cite the theoretical decreased hip dislocation rates in the postoperative period and the avoidance of the hip abduction musculature. | |||
3. Anterolateral (Watson-Jones) | |||
Compared to the other approaches, the anterolateral (AL) approach is the least commonly used approach secondary to its violation of the hip abductor mechanism. The interval exploited includes that of the TFL and gluteus medius musculature. This may lead to a postoperative limp at the tradeoff of a theoretically decreased dislocation rate.[[File:Hardinge approach hip.jpg|Hardinge approach|right|frameless]]4. Direct lateral (Hardinge) | |||
This approach, also known as the trangluteal approach, does not use a true internervous plane. Superficial dissection splits the fascia lata to reach the gluteus medius. The superior gluteal nerve enters the gluteal medius muscle belly at approximately 3-5 cm proximal to the greater trochanter. Proximal dissection may result in nerve injury, leading to postoperative Trendelenburg gait, characterized by compensatory movements to address hip abductor weakness. The transgluteal approach has been cited as having the lowest dislocation rate at 0.55%, compared to 3.23% for the posterior approach and 2.18% for the anterolateral approach | |||
{| width="100%" cellspacing="1" cellpadding="1" | {| width="100%" cellspacing="1" cellpadding="1" | ||
|- | |- | ||
| Line 92: | Line 108: | ||
<ref>Kelmanovich D, Parks ML, Sinha R, MD, Macaulay W. [https://www.researchgate.net/profile/William_Macaulay/publication/10643947_Surgical_approaches_to_total_hip_arthroplasty/links/09e415037afd617899000000.pdf Surgical Approaches to total hip arthroplasty.] Journal of the Southern Orthopaedic Association 2003;12:90-94.</ref> | <ref>Kelmanovich D, Parks ML, Sinha R, MD, Macaulay W. [https://www.researchgate.net/profile/William_Macaulay/publication/10643947_Surgical_approaches_to_total_hip_arthroplasty/links/09e415037afd617899000000.pdf Surgical Approaches to total hip arthroplasty.] Journal of the Southern Orthopaedic Association 2003;12:90-94.</ref> | ||
The use of minimally invasive surgery is becoming popular all around the world, due to the quicker recovery rates and reduced postoperative pain.<ref>Alecci V, Valente M, Crucil M, Minerva M, Pellegrino C, Sabbadini DD. [https://link.springer.com/article/10.1007/s10195-011-0144-0 Comparison of primary total hip replacements performed with a direct anterior approach versus the standard lateral approach: perioperative findings.] J Orthopaed Traumatol 2011;12:123-129.</ref> Long term follow-up and comparison studies are still needed in this field. | |||
=== Complications === | === Complications === | ||
2-10% of patients will develop complications during and after a total hip replacement.<ref name=":2">Dargel J, Oppermann J, Brüggemann G, Eysel P. Dislocation Following Total Hip Replacement. Dtsch Arztebl Int 2014;111:51-52.</ref> The following are the most commonly described in literature and observed in the clinical setting: | 2-10% of patients will develop complications during and after a total hip replacement.<ref name=":2">Dargel J, Oppermann J, Brüggemann G, Eysel P. Dislocation Following Total Hip Replacement. Dtsch Arztebl Int 2014;111:51-52.</ref> The following are the most commonly described in literature and observed in the clinical setting: | ||
Revision as of 00:57, 14 February 2021
Original Editors - Annelies Beckers, Vincent Everaert
Top Contributors - Lucinda hampton, Annelies Beckers, Leana Louw, Jessie Tourwe, Didzis Rozenbergs, Vincent Everaert, Kim Jackson, Admin, Yana Motte, Scott Buxton, Vidya Acharya, Johnathan Fahrner, Liese Bosman, Rebecca Willis, Liesel Muyelle, George Prudden, Aminat Abolade, Blessed Denzel Vhudzijena, Shaimaa Eldib, Evan Thomas, Redisha Jakibanjar, Samuel Adedigba, Lauren Lopez, Daniele Barilla, WikiSysop, Heleen.Mergan, Karen Wilson, 127.0.0.1, Kenny Bosmans, Laura Mertens and Uchechukwu Chukwuemeka
Description[edit | edit source]
Total hip arthroplasty (THA) is one of the most cost-effective and consistently successful surgeries performed in orthopaedics. THA provides reliable outcomes for patients’ suffering from end-stage degenerative hip osteoarthritis (OA), specifically pain relief, functional restoration, and overall improved quality of life[1].
A total hip replacement is a surgical procedure in which both damaged surfaces of the hip joint are replaced with prosthetic substitutes. It was first performed in the 1960's and is said to be one of the most successful surgeries in the last few decades.[2]
During a hip replacement, the head of the femur is replaced with a prosthetic head on a shaft, and the joint surface of the acetabulum is lined with a bowl-shaped synthetic joint surface. A partial replacement can also be done for neck of femur fractures (mostly displaced)[3] where only the femoral part is replaced.
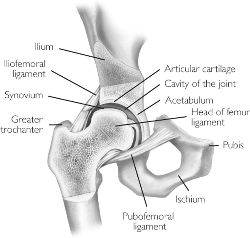
Clinically Relevant Anatomy[edit | edit source]
The hip is a ball and socket joint, meaning that the head of the femur fits into the acetabulum of the pelvis. The ball is the femoral head which fits into the socket, the acetabular part of the pelvis. This ball and socket design allows the poly-axial movement seen at the hip. The acetabulum is cup-shaped, providing the articular surface for the head of the femur to move within. The head of the femur is gripped by the acetabulum beyond its maximum diameter. The head of the femur and the inside of the acetabulum are covered with a layer of hyaline cartilage.[4] Once this cartilage is worn away or damaged (usually by arthritis), the underlying bone is exposed, resulting in pain, stiffness and possibly shortening of the affected leg. By replacing these surfaces the aim is to reduce pain and stiffness to restore an active and pain-free life.
Epidemiology/Etiology[edit | edit source]
Total hip replacement is a frequently done procedure.[5][6][7][8] Although mostly done electively, it is also used to in the management of hip fractures (mostly displaced neck of femur fractures) caused by trauma (e.g. fall) or pathological processes. Osteoporosis and osteomalacia are significant factors responsible for the high incidence of hip fractures within the elderly population. Arthritis is a common degenerative process occurring in joints within this elderly population, with osteoarthritis being the most common of the varieties. Due to the high degree of success at reinstating independence and mobility of osteoarthritis sufferers, total hip replacement procedures have become a well-accepted treatment modality for hip degeneration secondary to osteoarthritis[5][6][7][9][8]. It is also a treatment for juvenile rheumatoid arthritis but only if all the other options have failed[9].
Clinical Presentation[edit | edit source]
Preoperative[edit | edit source]
- Neck of femur fractures: Often unable to walk, complains of vague pain in the knee, thigh, groin, back or buttock and difficulty of weight bearing [10]. Impacted femur neck on X-ray.
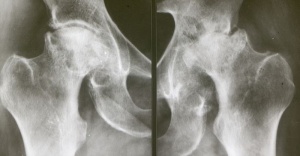
- Osteoarthritis: Sensible or audible crepitations on movement, inability to assume the neutral anatomical position. Often also linked with painful and/or decreased range of motion. X-ray findings commonly include decreased joint space, subchondral sclerosis, cyst formation and osteophytes.[11]
- Rheumatoid arthritis: Range of all hip movements are impaired, movement is painful, pain and stiffness when the activity is resumed after resting. [9]
- Avascular necrosis: Similar signs as with osteoarthritis, often also with referred knee pain.[12]
Indications for Surgery[edit | edit source]
The most common indication for THA includes end-stage, symptomatic hip OA. In addition, hip (osteonecrosis) ON, congenital hip disorders including hip dysplasia, and inflammatory arthritic conditions are not uncommon reasons for performing THA. Hip ON, on average, presents in the younger patient population (35 to 50 years of age) and accounts for approximately 10% of annual THAs. Some common indications include:[13]
- Osteoarthritis
- Post-traumatic arthritis
- Rheumatoid arthritis including juvenile rheumatoid arthritis
- Avascular necrosis
- Hardware failure after internal fixation of hip fractures
- Congenital hip dislocations and dysplasia[1]
Contraindications for Surgery[edit | edit source]
THA is contraindicated in the following clinical scenarios:
- Local: Hip infection or sepsis
- Remote (i.e. extra-articularticular) active, ongoing infection or bacteremia
- Severe cases of vascular dysfunction[14]
</article><article></article>
Diagnostic Procedures[edit | edit source]
The diagnosis of patients requiring total hip replacement surgery is mostly symptom-based. Pain, loss of range of motion and functional impairments are mostly considered here. A comprehensive differential diagnosis should also be made for patients complaining of hip pain, as it can often be referred from the spine or pelvis and have no connection to the hip joint itself.[9] An orthopaedic surgeon will guide the diagnosis and management process.
Consultation with an orthopaedic surgeon would include the following:[12] (Also see the page for hip examination)
- Observation
- Subjective interview:
- Complaints of pain, deformity, stiffness and/or limp
- Previous history linked to hip pain (congenital or childhood problems, previous trauma)
- Physical examination:
- Standing
- Trendelenberg test
- Gait
- Supine (including leg length)
- Objective observation (posture, deformities, muscle atrophy)
- Range of motion
There are specific ways to diagnose osteoarthritis, rheumatoid arthritis and hip fracture but for those subjects see the links above.
Special Investigations[edit | edit source]
- X-rays: AP pelvis for hips
This would be the first and, in a lot of cases, only radiological investigations requested, as a lot of the diagnoses in need of a hip replacement can be diagnosed or confirmed by this. This will guide the need for further investigations if needed.[12]
Prosthesis[edit | edit source]
THA prosthetic designs have been evolving since their inception.
Contemporary THA techniques have evolved into press-fit femoral and acetabular components. In general, femoral stems can be categorized into the following general designs:
- Press-fit, proximally coated, distal taper (dual or single tapered in medial-lateral and/or anterior-posterior planes)
- Press-fit, extensively coated, diaphyseal engaging
- Press-fit, Modular stems: Modularity junction options include: (1) head-neck, (2) neck-stem, (3) stem-sleeve, and (4) mid-stem
- Cemented femoral stems: Cobalt-chrome stems are the preferred material to promote cement bonding
Options for bearing surfaces include:
- Metal-on-polyethylene (MoP): MoP has the longest track record of all bearing surfaces at the lowest cost
- Ceramic-on-polyethylene (CoP): becoming an increasingly popular option
- Ceramic-on-ceramic (CoC): CoC has the best wear properties of all THA bearing surfaces
- Metal-on-metal (MoM): Although falling out of favor, MoM has historically demonstrated better wear properties from its MoP counterpart. MoM has lower linear-wear rates and decreased volume of particles generated. However, the potential for pseudotumor development as well as metallosis-based reactions (type-IV delayed hypersensitivity reactions) has resulted in a decline in the use of MoM. MoM is also contraindicated in pregnant women, patients with renal disease, and patients at risk of metal hypersensitivity.[1]
Important components of prosthesis are friction-coefficient, survival, stability against dislocation and fixation in bone tissue[15][16]. In some cases there can be formation of osteonecrosis due to erosion of the two components rubbing against each other[17]. Recent studies have shown that Vitamin E infused polyethylene provides 95% less wear when compared to other liners.[18][19]
Surgical Approaches[edit | edit source]
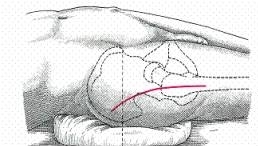
- Posterior
This is the most common approach for primary and revision THA cases. This dissection does not utilize a true internervous plane. The intermuscular interval involves blunt dissection of the gluteus maximus fibers and sharp incision of the fascia lata distally. The deep dissection involves meticulous dissection of the short external rotators and capsule. A major advantage of this approach is the avoidance of the hip abductors.
2. Direct Anterior (DA)
The DA approach is becoming increasingly popular among THA surgeons. The internervous interval is between the tensor fascia lata (TFL, superior gluteal nerve) and sartorius (femoral nerve) on the superficial end, and the gluteus medius (superficial gluteal nerve) and rectus femoris (RF, femoral nerve) on the deep side. DA THA advocates cite the theoretical decreased hip dislocation rates in the postoperative period and the avoidance of the hip abduction musculature.
3. Anterolateral (Watson-Jones)
Compared to the other approaches, the anterolateral (AL) approach is the least commonly used approach secondary to its violation of the hip abductor mechanism. The interval exploited includes that of the TFL and gluteus medius musculature. This may lead to a postoperative limp at the tradeoff of a theoretically decreased dislocation rate.
4. Direct lateral (Hardinge)
This approach, also known as the trangluteal approach, does not use a true internervous plane. Superficial dissection splits the fascia lata to reach the gluteus medius. The superior gluteal nerve enters the gluteal medius muscle belly at approximately 3-5 cm proximal to the greater trochanter. Proximal dissection may result in nerve injury, leading to postoperative Trendelenburg gait, characterized by compensatory movements to address hip abductor weakness. The transgluteal approach has been cited as having the lowest dislocation rate at 0.55%, compared to 3.23% for the posterior approach and 2.18% for the anterolateral approach
- Minimally Invasive Approaches (e.g. direct anterior approach)
The use of minimally invasive surgery is becoming popular all around the world, due to the quicker recovery rates and reduced postoperative pain.[21] Long term follow-up and comparison studies are still needed in this field.
Complications[edit | edit source]
2-10% of patients will develop complications during and after a total hip replacement.[22] The following are the most commonly described in literature and observed in the clinical setting:
- Dislocation: Decreased dislocation rates when comparing anterior approach to direct posterior approach)[22]
- Abductor insufficiency: Mostly after direct lateral approach
- Intra-operative fracture
- Nerve injury (associated to specific surgical approaches):[23]
- Direct lateral approach - superior gluteal nerve, femoral nerve
- Direct anterior approach - femoral cutaneous nerve
- Posterior approach - sciatic nerve
- Wound infection and/or sepsis
- Deep-vein thrombosis or pulmonary emboli
- Melallosis. A complication that arises from metal corrosion and release of debris. This causes a massive local cytokine release with resulting inflammation. Systemically it can manifest in many ways. The only treatment is revision surgery.[24]
- Atelectasis
- Lower respiratory tract infection
- Leg length discrepancy
- Prosthetic loosening and implant wear
Physiotherapy Management[edit | edit source]
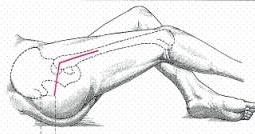
Precautions and Contraindications[edit | edit source]
Patients are at risk of hip dislocation after replacement as a result of the trauma to the hip stabilizers of the hip (capsule, ligaments and muscles) as well as due to the size difference of the prosthesis to the bones. Reduced size of the prosthetic femur head, when compared to the average human femur head, makes it easier to dislocate until the stabilizing tissues have healed and adapted to this smaller size[27]. This generally takes up to 6 weeks to heal.
Posterior Approach[edit | edit source]
- No combination of the following hip movements on the operated side:
- Flexion > 90 degrees
- Internal rotation past neutral
- Adduction past midline
- Weight bearing restrictions as per surgeon (mostly partial to full weight-bearing for 6 weeks after surgery)
Anterior Approach[edit | edit source]
Hip replacements following this surgical approach is generally more stable. No specific ranges are currently linked to the precaution movements, as surgeon preference should also be taken into account.
- Patients are encouraged to avoid a) excessive ranges and b) combination of the following hip movements on the operated side:
- Extension
- Abduction
- External rotation
- Weight bearing restrictions as per surgeon (usually less strict than with posterior approach surgery and patients are able/allowed to mobilize unaided sooner)
Pre-operative[edit | edit source]
Prescribing preoperative exercise as soon as people are approved for hip surgery could play an important role towards improving preoperative quality of life, because people can wait many months for surgery and might experience further deterioration in health-related quality of life during long waits.[28] Level 2b evidence shows that physiotherapy and educational therapy may be useful for end-stage osteoarthritis.[29] A study on a 6 week education and exercise programme has shown significant and sustained improvements in pain and disability on patients wait-listed for joint replacement surgery. Further positive results included improvements in function, knowledge and psycho-social aspects.[30]
A pre-operative assessment and treatment session is very helpful in the planning of the post-operative management of patients following a total hip replacement. Benefits include decreased length of stay[31],decreased anxiety levels[32], improved self-confidence[33] and establishing a relationship of trust between the physiotherapist and patient early on. Further benefits include improved quality of life and psychological health.[32] It also helps to develop a patient-specific rehabilitation programme to follow post-operative, taking assessment findings into consideration. The main factors defining the therapy management are the surgical approach and the general state of the patient. Whether the patient desires to gain physical fitness or wishes to recover for recreational activity should also be taken into account when establishing the rehabilitation programme.
Research has shown that a combination of verbal explanation and written pamphlets is the best method for health education.[32] It is very important to incorporate this into the pre-operative physiotherapy management of patients prior to total hip replacements. Pre-operative education on precautions aislikned to better post-operative adherence.[32]
Assessment[edit | edit source]
- Subjective history
- Range of motion
- Muscle power
- Circulation
- Mobility and function
Treatment[edit | edit source]
- Education and advice:
- Patient information booklet
- Precautions and contraindications
- Rehabilitation process
- Goals & expectations
- Functional/ADL adaptions
- Safety principles
- Encourage to stop smoking if applicable
- Discharge planning
- Teach:
- Bed exercises
- Transfers in and out of bed (within precautions)
- Gait re-education with mobility assestive device (crutches vs walking frame vs rollator)
- Stair climbing
Post-operative[edit | edit source]
The aim of post-operative rehabilitation is to address the functional needs of the patient (e.g. start mobilizing) and to improve strength and range of motion. This starts off as an assisted process, but the aim is to get the patient as functional as possible prior to discharge. As a result of the underlying pre-operative pathology, patients may present with muscle atrophy and loss of strength, particularly in the gluteus medius and quadriceps muscles. The result of the loss of strength is that the elderly are less independent.[5] Although the surgery will correct the joint problems, any associated muscle weakness that was present before the surgery will remain and require post-operative rehabilitation. Research has shown hip abductor weakness after surgery is a major risk associated with joint instability and prosthetic loosening.[6] Early postoperative rehabilitation after a total hip replacement focuses on resorting mobility, strength, flexibility and reducing pain.[7] It is found that patients can achieve significant improvements through a targeted strengthening programme following total hip replacement.[34] Also, Motor Imagery (MI) training, has been found to be a useful adjunct therapy tool as it improves both specific and general adaptations that were related to patients’ physical capabilities when added in a corollary to routine physical therapy.[35]
No specific general hip replacement protocol is currently in use, as small elements of the rehabilitation process are surgeon specific. For example, in some enhanced recovery after surgery protocols, patients are mobilised out of bed within the first 6 hours post-surgery. Other settings may only start mobilizing patients out of bed on day 1 or 2 post-surgery. Accelerated rehabilitation programmes and early mobilization have shown to give patients more confidence in their post-operative mobilization and activities of daily living, as well as being more comfortable with earlier discharge.[36]
Evidence[edit | edit source]
- Physiotherapy can improve strength and gait speed after total hip replacement and help prevent complications such as subluxation and thromboembolic disease. In addition, physiotherapy increases the patient’s mobility and offers education about the exercises and precautions that are necessary during hospitalization and after discharge.[37] (level of evidence 1a)
- Physiotherapy maximizes the patient’s function which is associated with a greater probability of earlier discharge, which is in turn associated with a lower total cost of care[38](level of evidence 2c).
- Physiotherapy provides pain relief, promotes rehabilitation and the reintegration of patients into ADLs. It also provides a better quality of life through the patients’ reintegration into social life [39] (level of evidence 1b).
- Level 1b evidence suggests that bed exercise following a total hip replacement does not seem to have an effect on the quality of life[40], but stays important for the effects on oedema, cardiac function and improving range of motion and muscle strength (level 4 evidence).[41]. It also allows an assessment of the physical and psychological condition of the patient right after surgery.
- Early weight bearing and physical activity have benefits for the quality of bone tissue[17] as it improves the fixation of the prosthesis and decreases the incidence of early loosening. The amount of activity is patient-specific, and clinical reasoning should be used to make adaptions where needed. Certain specific sport movements have a higher risk of injury for unskilled individuals, and should be incorporated later in the rehabilitation process under supervision of a physiotherapist or biokinetisist.
The following is a suggested protocol in the absence of complications. Surgeon preference should be taken into account, as well as any other factors that might hinder the following of the protocol. Adaptions should be made to make it more patient specific.[33][42]
Day 1 Post-Surgery[edit | edit source]
- Education and advice
- Education of muscular relaxation
- Revision of precautions and contraindications (provided that patient had a pre-operative session with the physiotherapist, otherwise full education will be done as mentioned in pre-operative section).
- Bed exercises:
- Circulation drills
- Upper limb exercises to stimulate the cardiac function
- Maintenance of the non-operated leg: attention should be paid to the range of motion in order to preserve controlled mobilisation on the operated hip
- Isometric quadriceps (progressing to consentric VMO) and gluteal contractions
- Active-assisted (progressing to active) heel slides, hip abduction/adduction
- Bed mobilisation using unilateral bridging on the unaffected leg
- Transfer to sit over edge of bed
- Sit to stand with mobility assistive device (preferably a device giving more support like a walking frame or rollator)
- Gait re-education with mobility assistive device as tolerated (weight bearing status as determined by surgeon)
- Sitting out in chair for maximum 1 hour
- Postioning when transferred back to bed
Day 2 Post-Surgery[edit | edit source]
- Bed exercises as described above, progressing repetitions and decreasing assistance given to patient
- Progression of distance mobilised and/or mobility assistive device
- Incorporate balance exercises if needed
- Sitting in chair
Day 3 Post-Surgery[edit | edit source]
- Bed exercises as described above, progressing repetitions and decreasing assistance given to patient
- Progression of distance mobilised and/or mobility assistive device
- Stair climbing (at least 3, or as per home requirements)
- Sitting in chair
- Revision of precautions, contraindications and functional adaptions
- Give 6 week progressive resistive strengthening home exercise to patient; this can include stationary cycling, as long as the patient stays within the precautions (especially posterior approach surgery)
- Discharge from hospital
Accelerated Protocol[edit | edit source]
- Combination of days 2 & 3 to discharge patient day 2 post surgery.
- Only selected patients
6 Weeks Post Surgery[edit | edit source]
- Patients are normally followed up by orthopaedic surgeon
- Surgeon determines if the patient is allowed the following:
- Full range of motion at the hip
- Full weight bearing without mobility assistive device
- Driving
After 6 Weeks[edit | edit source]
- Gain of initial ROM, stabilization, and proprioception
- Endurance
- Flexibility
- Balance
- Speed, precision, neurological coordination
- Functional exercises
Outcome Measures[edit | edit source]
- Harris Hip Score
- Oxford Hip Score (OHS)
- 6 Minute Walking Test
- Timed Get Up & Go Test
- Western Ontario and McMaster universities osteoarthritis index (WOMAC)
- SF-36
- Fear Avoidance Belief Score
- Hip Disability & Osteoarthritis Outcome Score (HOOS)
- International Hip Outcome Tool
- Ibadan Knee/Hip Osteoarthritis Outcome Measure
Take Home Message[edit | edit source]
Proper preoperative examination and early postoperative rehabilitation are crucial for a successful outcome.
Resources[edit | edit source]
- Pre-operative patient workbook on "living with osteoarthritis"
References[edit | edit source]
- ↑ 1.0 1.1 1.2 Varacallo M, Luo TD, Johanson NA. Total Hip Arthroplasty Techniques. InStatPearls [Internet] 2020 Jul 8. StatPearls Publishing.Available from: https://www.statpearls.com/articlelibrary/viewarticle/22894/ (accessed 14.2.2021)
- ↑ Levine BR, Klein GR, Cesare PE. Surgical approaches in total hip arthroplasty: A review of the mini-incision and MIS literature. Bulletin of the NYU Hospital for Joint Diseases 2007;65(1):5-18.
- ↑ Iglesias SL, Gentile L, Mangupli MM, Pioli I, Nomides RE, Allende BL. Femoral neck fractures in the elderly: from risk factors to pronostic features for survival. Journal of Trauma and Critical Care. 2017;1(1).
- ↑ Meyers HM. Fractures of the hip. Chicago: Year of the book medical publishers Inc., 1985
- ↑ 5.0 5.1 5.2 Gremeaux V, Renault J, Pardon L, Deley G, Lepers R, Casillas JM. Low-frequency electric muscle stimulation combined with physical therapy after total hip arthroplasty for hip osteoarthritis in elderly patients: a randomized controlled trial. Archives of physical medicine and rehabilitation 2008;89(12):2265-73.
- ↑ 6.0 6.1 6.2 Jan MH, Hung JY, Lin JC, Wang SF, Liu TK, Tang PF. Effects of a home program on strength, walking speed, and function after total hip replacement. Archives of physical medicine and rehabilitation 2004 ;85(12):1943-51.
- ↑ 7.0 7.1 7.2 Stockton KA, Mengersen KA. Effect of multiple physiotherapy sessions on functional outcomes in the initial postoperative period after primary total hip replacement: a randomized controlled trial. Archives of physical medicine and rehabilitation 2009;90(10):1652-7.
- ↑ 8.0 8.1 Rahmann AE, Brauer SG, Nitz JC. A specific inpatient aquatic physiotherapy program improves strength after total hip or knee replacement surgery: a randomized controlled trial. Archives of physical medicine and rehabilitation 2009;90(5):745-55.
- ↑ 9.0 9.1 9.2 9.3 Crawford AJ, Hamblen DL. Outline of Orthopaedics , thirteenth edition, London: Churchill Livingstone, 2001
- ↑ Batra S, Batra M, McMurtrie A, Sinha AK. Rapidly destructive osteoarthritis of the hip joint: a case series. Journal of orthopaedic surgery and research 2008;3(1):3.
- ↑ Brandt CD. Diagnosis and non-surgical management of osteoarthritis. USA: Professional Communications, Inc. 2010
- ↑ 12.0 12.1 12.2 Walters J, editor. Orthopaedics - A guide for practitioners. 4th Edition. Cape Town: University of Cape Town, 2010.
- ↑ Affatato S. Perspectives in total hip arthroplasty: Advances in biomaterials and their tribological interactions. London: Woodhead Publishing, 2014.
- ↑ Varacallo M, Luo TD, Johanson NA. Total Hip Arthroplasty Techniques. InStatPearls [Internet] 2020 Jul 8. StatPearls Publishing.Available from:https://www.statpearls.com/articlelibrary/viewarticle/22894/ (accessed 14.2.2021)
- ↑ Bader R, Steinhauser E, Zimmermann S, Mittelmeier W, Scholz R, Busch R. Differences between the wear couples metal-on-polyethylene and ceramic-on-ceramic in the stability against dislocation of total hip replacement. Journal of materials science: materials in medicine 2004;15(6):711-8.
- ↑ Garcia-Rey E, Cruz-Pardos A, Garcia-Cimbrelo E. Alumina-on-alumina total hip arthroplasty in young patients: diagnosis is more important than age. Clinical Orthopaedics and Related Research 2009;467(9):2281-9.
- ↑ 17.0 17.1 Mahendra G, Pandit H, Kliskey K, Murray D, Gill HS, Athanasou N. Necrotic and inflammatory changes in metal-on-metal resurfacing hip arthroplasties: relation to implant failure and pseudotumor formation. Acta orthopaedica 2009;80(6):653-9.
- ↑ Zimmer Biomet. The E1™ Antioxidant Infused Technology Process. http://www.biomet.fi/viewversion.cfm?contentversionid=36999&sc=1 (accessed 2506/2018).
- ↑ Lindalen L, Nordsletten L, Høvik Ø, Röhrl SM. E-Vitamin Infused Highly Cross-Linked Polyethylene: RSA Results from a Randomised Controlled Trial Using 32 mm and 36 mm Ceramic Heads. Hip International 2015;25(1):50 - 55
- ↑ Kelmanovich D, Parks ML, Sinha R, MD, Macaulay W. Surgical Approaches to total hip arthroplasty. Journal of the Southern Orthopaedic Association 2003;12:90-94.
- ↑ Alecci V, Valente M, Crucil M, Minerva M, Pellegrino C, Sabbadini DD. Comparison of primary total hip replacements performed with a direct anterior approach versus the standard lateral approach: perioperative findings. J Orthopaed Traumatol 2011;12:123-129.
- ↑ 22.0 22.1 Dargel J, Oppermann J, Brüggemann G, Eysel P. Dislocation Following Total Hip Replacement. Dtsch Arztebl Int 2014;111:51-52.
- ↑ 23.0 23.1 Petis S, Howard JL, Lanting BL, Vasarhelyi EM. Surgical approach in primary total hip arthroplasty: anatomy, technique and clinical outcomes. Can J Surg 2015;58(2):128–139.
- ↑ Oliveira CA, Candelária IS, Oliveira PB, Figueiredo A, Caseiro-Alves F. Metallosis: A diagnosis not only in patients with metal-on-metal prostheses. European journal of radiology open. 2015 Jan 1;2:3-6. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4750564/ (last accessed 24.2.2019)
- ↑ American Association of Orthopaedic Surgeons. Total hip replacement. https://orthoinfo.aaos.org/en/treatment/total-hip-replacement/ (accessed 25/06/2018).
- ↑ Partridge T, Jameson S, Baker P, MBBS, Deehan D, Mason M, Reed MR. Ten-Year Trends in Medical Complications Following 540,623 Primary Total Hip Replacements from a National Database. J Bone Joint Surg Am 2018;100(5):360–367.
- ↑ Mirza S, Dunlop D G, Panesar S, Syed G N, Shafat G, Saif S. Basic Science Considerations in Primary Total Hip Replacement Arthroplasty. The Open Orthopaedics Journal. 2010;4,169-180
- ↑ Gill SD, McBurney H. Does Exercise Reduce Pain and Improve Physical Function Before Hip or Knee Replacement Surgery? A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Archives of physical medicine and rehabilitation. 2013;94(1):164-76.
- ↑ Ferrara PE, Rabini AL, Maggi LO, Piazzini DB, Logroscino G, Magliocchetti G, Amabile E, Tancredi G, Aulisa AG, Padua L, Gnocchi DC. Effect of pre-operative physiotherapy in patients with end-stage osteoarthritis undergoing hip arthroplasty. Clinical rehabilitation 2008;22(10-11):977-86.
- ↑ Saw MM. The effects of a six-week physiotherapist-led exercise and education intervention in patients with osteoarthritis, awaiting an arthroplasty in the South Africa [dissertation]. Cape Town: University of Cape Town. 2015.
- ↑ Crowe J,Henderson J. Pre-arthroplasty rehabilitation is effective in reducing length of hospital stay. Canadian Journal of Occupational Therapy 2003;70:88-96.
- ↑ 32.0 32.1 32.2 32.3 Barnes RY, Bodenstein, K, Human N. Raubenheimer J, Dawkins J, Seesink C, Jacobs J, van der Linde J, Venter R. Preoperative education in hip and knee arthroplasty patients in Bloemfontein. South African Journal of Physiotherapy 2018;74(1).
- ↑ 33.0 33.1 33.2 Raymond Sohier, Kinesitherapie de la hanche ; La Hestre : Sohier, 1974
- ↑ Galea MP, Levinger P, Lythgo N, Cimoli C, Weller R, Tully E, McMeeken J, Westh R. A targeted home-and center-based exercise program for people after total hip replacement: a randomized clinical trial. Archives of physical medicine and rehabilitation 2008;89(8):1442-7.
- ↑ Paravlic AH, Pisot R, Marusic U. Specific and general adaptations following motor imagery practice focused on muscle strength in total knee arthroplasty rehabilitation: A randomized controlled trial. PloS one. 2019;14(8).
- ↑ Robertson NB, Warganich T, Ghazarossian J, Khatod M. Implementation of an accelerated rehabilitation protocol for total joint arthroplasty in the managed care setting: the experience of one institution. Advances in Orthopedic Surgery. 2015;387197.
- ↑ Coulter CL, Scarvell JM, Neeman TM, Smith PN. Physiotherapist-directed rehabilitation exercises in the outpatient or home setting improve strength, gait speed and cadence after elective total hip replacement: a systematic review. Journal of physiotherapy. 2013;59(4):219-26.
- ↑ Freburger J. An analysis of the relationship between the utilization of physical therapy services and outcomes of care for patients after total hip arthroplasty. Physical therapy 2000;80(5):448-458.
- ↑ Umpierres CS, Ribeiro TA, Marchisio ÂE, Galvão L, Borges ÍN, Macedo CA, Galia CR. Rehabilitation following total hip arthroplasty evaluation over short follow-up time: Randomized clinical trial. Journal of rehabilitation research and development. 2014;51(10):1567-78.
- ↑ Smith TO, Mann CJ, Clark A, Donell ST. Bed exercises following total hip replacement: a randomised controlled trial. Physiotherapy 2008;94(4):286-91.
- ↑ Perhonen MA, Franco F, Lane LD, Buckey JC, Blomqvist CG, Zerwekh JE, Peshock RM, Weatherall PT, Levine BD. Cardiac atrophy after bed rest and spaceflight. Journal of applied physiology 2001;91(2):645-53.
- ↑ Suetta C, Aagaard P, Rosted A, Jakobsen AK, Duus B, Kjaer M, Magnusson SP. Training-induced changes in muscle CSA, muscle strength, EMG, and rate of force development in elderly subjects after long-term unilateral disuse. Journal of Applied Physiology 2004;97(5):1954-61.