Lumbar Assessment: Difference between revisions
Evan Thomas (talk | contribs) mNo edit summary |
Evan Thomas (talk | contribs) mNo edit summary |
||
| Line 9: | Line 9: | ||
[[Image:Interactive Spine - Lumbar Vertebral Spine - L7F19.jpg|right|200px]] | [[Image:Interactive Spine - Lumbar Vertebral Spine - L7F19.jpg|right|200px]] | ||
The first aim of the physiotherapy examination for a patient presenting with back pain is to classify the patient according to the diagnostic triage recommended in international back pain guidelines<ref name="Koes">Koes BW, van Tulder M, Lin C-WC, Macedo LG, McAuley J, Maher C. [http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2997201/ An updated overview of clinical guidelines for the management of non-specific low back pain in primary care]. Eur Spine J 2010;19:2075–94</ref>. Serious (such as fracture, cancer, infection and ankylosing spondylitis) and specific causes of back pain with neurological deficits (such as radiculopathy, caudal equina syndrome)are rare<ref>Henschke N, Maher CG, Refshauge KM, et al. Prevalence of and screening for serious spinal pathology in patients presenting to primary care settings with acute low back pain. Arthritis Rheum 2009;60:3072–80.</ref> but it is important to screen for these conditions<ref name="Koes" /><ref name="van Tulder">van Tulder M, Becker A, Bekkering T, et al. Chapter 3. European guidelines for the management of acute nonspecific low back pain in primary care. Eur Spine J 2006;15(Suppl 2):S169–91</ref>. Serious conditions account for 1-2% of people presenting with low back pain and 5-10% present with | The first aim of the physiotherapy examination for a patient presenting with back pain is to classify the patient according to the diagnostic triage recommended in international back pain guidelines<ref name="Koes">Koes BW, van Tulder M, Lin C-WC, Macedo LG, McAuley J, Maher C. [http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2997201/ An updated overview of clinical guidelines for the management of non-specific low back pain in primary care]. Eur Spine J 2010;19:2075–94</ref>. Serious (such as fracture, cancer, infection and ankylosing spondylitis) and specific causes of back pain with neurological deficits (such as radiculopathy, caudal equina syndrome)are rare<ref>Henschke N, Maher CG, Refshauge KM, et al. Prevalence of and screening for serious spinal pathology in patients presenting to primary care settings with acute low back pain. Arthritis Rheum 2009;60:3072–80.</ref> but it is important to screen for these conditions<ref name="Koes" /><ref name="van Tulder">van Tulder M, Becker A, Bekkering T, et al. Chapter 3. European guidelines for the management of acute nonspecific low back pain in primary care. Eur Spine J 2006;15(Suppl 2):S169–91</ref>. Serious conditions account for 1-2% of people presenting with low back pain and 5-10% present with specific causes LBP with neurological deficits<ref>O'Sullivan, P. and Lin, I. Acute low back pain Beyond drug therapies. Pain Management Today, 2014, 1(1):8-14</ref>. When serious and [[Specific Low Back Pain|specific causes of low back pain]] have been ruled out individuals are said to have non-specific (or simple or mechanical) back pain. | ||
[[Non Specific Low Back Pain|Non-specific low back pain]] accounts for over 90% of patients presenting to primary care<ref>Koes BW, van Tulder MW, Thomas S. Diagnosis and treatment of low back pain. BMJ 2006;332:1430–34.</ref> and these are the majority of the individuals with low back pain that present to physiotherapy. | [[Non Specific Low Back Pain|Non-specific low back pain]] accounts for over 90% of patients presenting to primary care<ref>Koes BW, van Tulder MW, Thomas S. Diagnosis and treatment of low back pain. BMJ 2006;332:1430–34.</ref> and these are the majority of the individuals with low back pain that present to physiotherapy. Physiotherapy assessment aims to identify impairments that may have contributed to the onset of the pain, or increase the likelihood of developing persistent pain. These include biological factors (eg. weakness, stiffness), psychological factors (eg. depression, fear of movement and catastrophization) and social factors (eg. work environment)<ref name="Hancock" />. The assessment does not focus on identifying anatomical structures (eg. the intervertebral disc) as the source of pain, as might be the case in peripheral joints such as the knee<ref name="Hancock">M.Hancock. Approach to low back pain. RACGP, 2014, 43(3):117-118</ref>. Previous research and international guidelines suggest it is not possible or necessary to identify the specific tissue source of pain for the effective management of mechanical back pain<ref name="Koes" /><ref name="van Tulder" /><ref>Hancock MJ, Maher CG, Latimer J, et al. Systematic review of tests to identify the disc, SIJ or facet joint as the source of low back pain. Eur Spine J 2007;16:1539–50.</ref>. | ||
The subjective assessment (history taking) is by far the most important part of the assessment with the objective assessment (clinical testing) confirming or refuting hypothesis formed from the subjective. | The subjective assessment (history taking) is by far the most important part of the assessment with the objective assessment (clinical testing) confirming or refuting hypothesis formed from the subjective. | ||
| Line 17: | Line 17: | ||
Assessment of the lumbar spine should allow clinical reasoning to include appropriate data collection tests from those listed below. | Assessment of the lumbar spine should allow clinical reasoning to include appropriate data collection tests from those listed below. | ||
== Subjective | == Subjective == | ||
The subjective examination is one of most powerful tools a clinician can utilize in the examination and treatment of patients with LBP. The questions utilized during this process can improve the clinician’s confidence in identification of sinister pathology warranting outside referral, screening for yellow flags which may interfere with PT interventions, and assist in matching PT interventions with a patient’s symptoms. | The subjective examination is one of most powerful tools a clinician can utilize in the examination and treatment of patients with LBP. The questions utilized during this process can improve the clinician’s confidence in identification of sinister pathology warranting outside referral, screening for yellow flags which may interfere with PT interventions, and assist in matching PT interventions with a patient’s symptoms. | ||
History not only is the record of past and present suffering but also constitutes the basis of future treatment, prevention and prognosis.<br> | History not only is the record of past and present suffering but also constitutes the basis of future treatment, prevention, and prognosis.<br> | ||
=== Patient Intake === | === Patient Intake === | ||
*Self‐report (present complaint (PC), history of present | *Self‐report (present complaint (PC), history of present complaint (HPC), past medical history (PMH), drug history (DH), social history (SH)) | ||
*Region‐specific questions | *Region‐specific questions | ||
**What is the patient’s age? | **What is the patient’s age? | ||
| Line 48: | Line 48: | ||
**Is the patient able to cope during daily activities? | **Is the patient able to cope during daily activities? | ||
=== Special Questions | === Special Questions === | ||
==== Red Flags | ==== Red Flags ==== | ||
Although uncommon [[Serious Spinal Conditions|serious spinal conditions]] (such as those listed below) may present as LBP in approximately 5% of patients presenting to primary care office:<ref name="p2">Deyo, R. et al. What Can the History and Physical Examination Tell Us About Low Back Pain? JAMA. 1992. 268(6):760-766.</ref><ref name="p2"/>. | |||
*[[Cauda Equina Syndrome|Cauda equina syndrome ]] | *[[Cauda Equina Syndrome|Cauda equina syndrome ]] | ||
*[[Cancer pain|Cancer ]] | *[[Cancer pain|Cancer ]] | ||
| Line 63: | Line 62: | ||
*Abdominal aortic aneurysm<br> | *Abdominal aortic aneurysm<br> | ||
During the investigation you must pay attention to any ‘[[Red Flags in Spinal Conditions|red flags]]’ that might be present indicating serious pathology. Koes et al (2006)<ref>Koes B.W. van Tulder M. W., Thomas S.; diagnosis and treatment of low back pain; BMJ volume 332, 17 | During the investigation, you must pay attention to any ‘[[Red Flags in Spinal Conditions|red flags]]’ that might be present indicating serious pathology. Koes et al (2006)<ref>Koes B.W. van Tulder M. W., Thomas S.; diagnosis and treatment of low back pain; BMJ volume 332, 17 June 2006; 1430-1434</ref> mentioned the following ‘red flags’: | ||
*Onset age < 20 or > 55 years | *Onset age < 20 or > 55 years | ||
*Non-mechanical pain (unrelated to time or activity) | *Non-mechanical pain (unrelated to time or activity) | ||
| Line 78: | Line 76: | ||
==== Other Flags ==== | ==== Other Flags ==== | ||
It is also important to screen for [[The Flag System|other (yellow, orange, blue and black) flags]] | It is also important to screen for [[The Flag System|other (yellow, orange, blue and black) flags]] as these may interfere with physiotherapy interventions. | ||
[[The Flag System|Read more about the Flag System]] | [[The Flag System|Read more about the Flag System]] | ||
| Line 87: | Line 85: | ||
*[[STarT Back Screening Tool]] | *[[STarT Back Screening Tool]] | ||
*Acute Low Back Pain Screening Questionnaire | *Acute Low Back Pain Screening Questionnaire | ||
*[[Quebec Back Pain Disability Scale|The Quebec Back Pain Disability Scale]] | *[[Quebec Back Pain Disability Scale|The Quebec Back Pain Disability Scale]] | ||
*[[Oswestry Disability Index|Oswestry Disability Index]] | *[[Oswestry Disability Index|Oswestry Disability Index]] | ||
*Hendler 10-Minute Screening Test for Chronic Back Pain Patients | *Hendler 10-Minute Screening Test for Chronic Back Pain Patients | ||
*[[Roland‐Morris Disability Questionnaire|The Roland-Morris Disability Questionnaire]] | *[[Roland‐Morris Disability Questionnaire|The Roland-Morris Disability Questionnaire]] | ||
=== Investigations | === Investigations === | ||
Has the patient had any other investigations such as radiology (Xray, MRI, CT, ultrasound) or blood tests?<br> | Has the patient had any other investigations such as radiology (Xray, MRI, CT, ultrasound) or blood tests?<br> | ||
| Line 98: | Line 96: | ||
== Objective == | == Objective == | ||
The purpose of the objective examination (clinical testing) is to confirm or refute hypothesis formed from the subjective examination. | The purpose of the objective examination (clinical testing) is to confirm or refute hypothesis formed from the subjective examination. | ||
When assessing the lumbar spine, the examiner must remember that referral of symptoms or the presence of neurological symptoms often makes it necessary to “clear” or rule out lower limb pathology. Many of the symptoms that occur in the lower limb may originate in the lumbar spine. Unless there is a history of definitive trauma to a peripheral joint, a screening or scanning examination must accompany assessment of that joint to rule out problems within the lumbar spine referring symptoms to that joint. | When assessing the lumbar spine, the examiner must remember that referral of symptoms or the presence of neurological symptoms often makes it necessary to “clear” or rule out lower limb pathology. Many of the symptoms that occur in the lower limb may originate in the lumbar spine. Unless there is a history of definitive trauma to a peripheral joint, a screening or scanning examination must accompany assessment of that joint to rule out problems within the lumbar spine referring symptoms to that joint. | ||
| Line 104: | Line 102: | ||
Examination procedures should be performed from standing-sitting-lying and pain provocation movements saved until last. | Examination procedures should be performed from standing-sitting-lying and pain provocation movements saved until last. | ||
=== Observation | === Observation === | ||
==== Movement Patterns | ==== Movement Patterns ==== | ||
*How does the patient enter the room? | *How does the patient enter the room? | ||
| Line 133: | Line 131: | ||
*facial expression | *facial expression | ||
*skin | *skin | ||
*hair | *hair | ||
*leg length discrepancy (functional, structural) | *leg length discrepancy (functional, structural) | ||
=== Functional Tests | === Functional Tests === | ||
#Functional Demonstration of pain provoking movements<br> | #Functional Demonstration of pain provoking movements<br> | ||
| Line 144: | Line 142: | ||
*AROM (flexion 40-60, extension 20-35, side flexion 15-20 - looking for willingness to move, quality of movement, where movement occurs, range, pain, painful arc, deviation) | *AROM (flexion 40-60, extension 20-35, side flexion 15-20 - looking for willingness to move, quality of movement, where movement occurs, range, pain, painful arc, deviation) | ||
*Overpressure (at the end of all AROM if they are pain free, normal end feel should be tissue stretch) | *Overpressure (at the end of all AROM if they are pain-free, normal end-feel should be tissue stretch) | ||
*Sustained positions (if indicated in subjective) | *Sustained positions (if indicated in subjective) | ||
*Combined movements (if indicated in subjective) | *Combined movements (if indicated in subjective) | ||
| Line 160: | Line 158: | ||
|} | |} | ||
*Myotomes | *Myotomes | ||
**L2: Hip flexion | **L2: Hip flexion | ||
**L3: Knee extension | **L3: Knee extension | ||
| Line 167: | Line 165: | ||
**S1: Ankle plantar flexion, ankle eversion, hip extension | **S1: Ankle plantar flexion, ankle eversion, hip extension | ||
**S2: Knee flexion | **S2: Knee flexion | ||
*Dermatomes | *Dermatomes | ||
*Reflexes | *Reflexes | ||
**Patellar (L3–L4) (commonly used in clinical practice) | **Patellar (L3–L4) (commonly used in clinical practice) | ||
| Line 174: | Line 174: | ||
**Posterior tibial (L4–L5)(rarely used in clinical practice) | **Posterior tibial (L4–L5)(rarely used in clinical practice) | ||
**Achilles (S1–S2) (commonly used in clinical practice) | **Achilles (S1–S2) (commonly used in clinical practice) | ||
*[[Neurodynamic Assessment|Neurodynamic testing]] | |||
*[[Neurodynamic Assessment|Neurodynamic testing]] - slump, SLR, PKB and modified versions where appropriate<br> | |||
=== Circulatory Assessment === | === Circulatory Assessment === | ||
| Line 207: | Line 208: | ||
*Thoracic spine - seated rotation with combined movements and overpressure | *Thoracic spine - seated rotation with combined movements and overpressure | ||
*Sacroiliac joints - various tests have been described to clear the SIJ such as Gillet test, sacral clearing test, [[Sacroiliac Joint Special Test Cluster|cluster tests]] | *Sacroiliac joints - various tests have been described to clear the SIJ such as Gillet test, sacral clearing test, [[Sacroiliac Joint Special Test Cluster|cluster tests]] | ||
*Hips - PROM with overpressure | *Hips - PROM with overpressure | ||
*Knees and ankles - should also be cleared for restrictions that may affect movement patterns<br> | *Knees and ankles - should also be cleared for restrictions that may affect movement patterns<br> | ||
| Line 213: | Line 214: | ||
For neurological dysfunction: | For neurological dysfunction: | ||
*Centralization/peripheralization | *Centralization/peripheralization | ||
*Cross straight leg raise test | *Cross straight leg raise test | ||
| Line 222: | Line 222: | ||
For lumbar instability: | For lumbar instability: | ||
{| width="40%" cellspacing="1" cellpadding="1" border="0" align="right" | {| width="40%" cellspacing="1" cellpadding="1" border="0" align="right" | ||
|- | |- | ||
| Line 237: | Line 236: | ||
For joint dysfunction: | For joint dysfunction: | ||
*Bilateral straight leg raise test | *Bilateral straight leg raise test | ||
*One-leg standing (stork standing) lumbar extension test | *One-leg standing (stork standing) lumbar extension test | ||
| Line 243: | Line 241: | ||
For muscle tightness: | For muscle tightness: | ||
*90–90 straight leg raise test | *90–90 straight leg raise test | ||
*[[Ober's Test|Ober test]] | *[[Ober's Test|Ober test]] | ||
| Line 250: | Line 247: | ||
Other tests: | Other tests: | ||
*[[Sign of the Buttock|Sign of the buttock]]<br> | *[[Sign of the Buttock|Sign of the buttock]]<br> | ||
| Line 256: | Line 252: | ||
If you have little time a brief examination of patients with back pain has two basic purposes. | If you have little time a brief examination of patients with back pain has two basic purposes. | ||
#Firstly it will help screen patients for possible serious spinal pathology even though taking a good history is much more important. | #Firstly it will help screen patients for possible serious spinal pathology even though taking a good history is much more important. | ||
#Secondly it will improve patient satisfaction and effectiveness of the consultation. | #Secondly it will improve patient satisfaction and effectiveness of the consultation. | ||
It is suggested that the following be performed as a bare minimum: | It is suggested that the following be performed as a bare minimum: | ||
#Inspect – general appearance, gross structural deformities | #Inspect – general appearance, gross structural deformities | ||
#Active movements – flexion (significant limitation often pathological), extension, side flexion | #Active movements – flexion (significant limitation often pathological), extension, side flexion | ||
Revision as of 20:06, 28 August 2017
Original Editors - Ben Vandoorne
Top Contributors - Admin, Rachael Lowe, Kim Jackson, Laura Ritchie, Jess Bell, Vandoorne Ben, Carin Hunter, Naomi O'Reilly, Kai A. Sigel, Lucinda hampton, Evan Thomas, Simisola Ajeyalemi, Aminat Abolade, WikiSysop, Wanda van Niekerk, 127.0.0.1 and Rishika Babburu
Introduction[edit | edit source]
The first aim of the physiotherapy examination for a patient presenting with back pain is to classify the patient according to the diagnostic triage recommended in international back pain guidelines[1]. Serious (such as fracture, cancer, infection and ankylosing spondylitis) and specific causes of back pain with neurological deficits (such as radiculopathy, caudal equina syndrome)are rare[2] but it is important to screen for these conditions[1][3]. Serious conditions account for 1-2% of people presenting with low back pain and 5-10% present with specific causes LBP with neurological deficits[4]. When serious and specific causes of low back pain have been ruled out individuals are said to have non-specific (or simple or mechanical) back pain.
Non-specific low back pain accounts for over 90% of patients presenting to primary care[5] and these are the majority of the individuals with low back pain that present to physiotherapy. Physiotherapy assessment aims to identify impairments that may have contributed to the onset of the pain, or increase the likelihood of developing persistent pain. These include biological factors (eg. weakness, stiffness), psychological factors (eg. depression, fear of movement and catastrophization) and social factors (eg. work environment)[6]. The assessment does not focus on identifying anatomical structures (eg. the intervertebral disc) as the source of pain, as might be the case in peripheral joints such as the knee[6]. Previous research and international guidelines suggest it is not possible or necessary to identify the specific tissue source of pain for the effective management of mechanical back pain[1][3][7].
The subjective assessment (history taking) is by far the most important part of the assessment with the objective assessment (clinical testing) confirming or refuting hypothesis formed from the subjective.
Assessment of the lumbar spine should allow clinical reasoning to include appropriate data collection tests from those listed below.
Subjective[edit | edit source]
The subjective examination is one of most powerful tools a clinician can utilize in the examination and treatment of patients with LBP. The questions utilized during this process can improve the clinician’s confidence in identification of sinister pathology warranting outside referral, screening for yellow flags which may interfere with PT interventions, and assist in matching PT interventions with a patient’s symptoms.
History not only is the record of past and present suffering but also constitutes the basis of future treatment, prevention, and prognosis.
Patient Intake[edit | edit source]
- Self‐report (present complaint (PC), history of present complaint (HPC), past medical history (PMH), drug history (DH), social history (SH))
- Region‐specific questions
- What is the patient’s age?
- What is the patient’s occupation?
- What was the mechanism of injury?
- How long has the problem bothered the patient?
- Where are the sites and boundaries of pain?
- Is there any radiation of pain? Is the pain centralizing or peripheralizing
- Is the pain deep? Superficial? Shooting? Burning? Aching?
- Is the pain improving? Worsening? Staying the same?
- Is there any increase in pain with coughing? Sneezing? Deep breathing? Laughing?
- Are there any postures or actions that specifically increase or decrease the pain or cause difficulty?Is the pain worse in the morning or evening? Does the pain get better or worse as the day progresses? Does the pain wake you up at night?Which movements hurt? Which movements are stiff?
- Is paresthesia (a “pins and needles” feeling) or anesthesia present?
- Has the patient noticed any weakness or decrease in strength? Has the patient noticed that his/her legs have become weak while walking or climbing stairs?
- What is the patient’s usual activity or pastime? Before the injury, did the patient modify or perform any unusual repetitive or high-stress activity?
- Which activities aggravate the pain? Is there anything in the patient’s lifestyle that increases the pain?
- Which activities ease the pain?
- What is the patient’s sleeping position? Does the patient have any problems sleeping?
- Does the patient have any difficulty with micturition?
- Are there any red flags that the examiner should be aware of, such as a history of cancer, sudden weight loss for no apparent reason, immunosuppressive disorder, infection, fever, or bilateral leg weakness?
- Is the patient receiving any medication?
- Is the patient able to cope during daily activities?
Special Questions[edit | edit source]
Red Flags[edit | edit source]
Although uncommon serious spinal conditions (such as those listed below) may present as LBP in approximately 5% of patients presenting to primary care office:[8][8].
- Cauda equina syndrome
- Cancer
- Ankylosing spondylitis
- Lumbar stenosis
- Lumbar disc herniations
- Vertebral fracture
- Spinal infection
- Abdominal aortic aneurysm
During the investigation, you must pay attention to any ‘red flags’ that might be present indicating serious pathology. Koes et al (2006)[9] mentioned the following ‘red flags’:
- Onset age < 20 or > 55 years
- Non-mechanical pain (unrelated to time or activity)
- Thoracic pain
- Previous history of carcinoma, steroids, HIV
- Feeling unwell
- Weight loss
- Widespread neurological symptoms
- Structural spinal deformity
Read more about red flags in spinal conditions
Other Flags[edit | edit source]
It is also important to screen for other (yellow, orange, blue and black) flags as these may interfere with physiotherapy interventions.
Read more about the Flag System
Outcome Measures[edit | edit source]
- Fear‐Avoidance Belief Questionnaire
- STarT Back Screening Tool
- Acute Low Back Pain Screening Questionnaire
- The Quebec Back Pain Disability Scale
- Oswestry Disability Index
- Hendler 10-Minute Screening Test for Chronic Back Pain Patients
- The Roland-Morris Disability Questionnaire
Investigations[edit | edit source]
Has the patient had any other investigations such as radiology (Xray, MRI, CT, ultrasound) or blood tests?
Objective[edit | edit source]
The purpose of the objective examination (clinical testing) is to confirm or refute hypothesis formed from the subjective examination.
When assessing the lumbar spine, the examiner must remember that referral of symptoms or the presence of neurological symptoms often makes it necessary to “clear” or rule out lower limb pathology. Many of the symptoms that occur in the lower limb may originate in the lumbar spine. Unless there is a history of definitive trauma to a peripheral joint, a screening or scanning examination must accompany assessment of that joint to rule out problems within the lumbar spine referring symptoms to that joint.
Examination procedures should be performed from standing-sitting-lying and pain provocation movements saved until last.
Observation[edit | edit source]
Movement Patterns[edit | edit source]
- How does the patient enter the room?
- A posture deformity in flexion or a deformity with a lateral pelvic tilt, possibly a slight limp, may be seen.
- How does the patient sit down and how comfortably/ uncomfortably does he or she sit?
- How does the patient get up from the chair? A patient with low back pain may splint the spine in order to avoid painful movements.
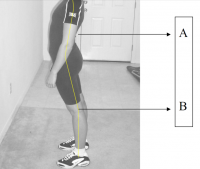
Posture[edit | edit source]
Other observations[edit | edit source]
- body type
- attitude
- facial expression
- skin
- hair
- leg length discrepancy (functional, structural)
Functional Tests[edit | edit source]
- Functional Demonstration of pain provoking movements
- Squat test - to highlight lower limb pathologies. Not be done with patients suspected of having arthritis or pathology in the lower limb joints, pregnant patients, or older patients who exhibit weakness and hypomobility. If this test is negative, there is no need to test the peripheral joints (peripheral joint scan) with the patient in the lying position[10].
Movement Testing[edit | edit source]
- AROM (flexion 40-60, extension 20-35, side flexion 15-20 - looking for willingness to move, quality of movement, where movement occurs, range, pain, painful arc, deviation)
- Overpressure (at the end of all AROM if they are pain-free, normal end-feel should be tissue stretch)
- Sustained positions (if indicated in subjective)
- Combined movements (if indicated in subjective)
- Repeated movements (if indicated in subjective)
- Muscle Strength (resisted isometrics in flex, ext, side flex, rotation; core stabilty, functional strength tests)
Neurologic Assessment[edit | edit source]
Neurologic assessment is indicated where there is suspicion of neurologic deficit.
| [11] |
- Myotomes
- L2: Hip flexion
- L3: Knee extension
- L4: Ankle dorsiflexion
- L5: Great toe extension
- S1: Ankle plantar flexion, ankle eversion, hip extension
- S2: Knee flexion
- Dermatomes
- Reflexes
- Patellar (L3–L4) (commonly used in clinical practice)
- Medial hamstring (L5–S1) (rarely used in clinical practice)
- Lateral hamstring (S1–S2) (rarely used in clinical practice)
- Posterior tibial (L4–L5)(rarely used in clinical practice)
- Achilles (S1–S2) (commonly used in clinical practice)
- Neurodynamic testing - slump, SLR, PKB and modified versions where appropriate
Circulatory Assessment[edit | edit source]
If indicated it may be necessary to perform a haemodynamic assessment.
Palpation[edit | edit source]
| [12] |
It is crucial for a reliable diagnosis and intervention of treatment to adequately palpate the lumbar spinous processes.
Within the scientific world, there has been a debate about the palpation of the spinous processes because scientists assumed that often different persons indicated the processes in a different place (Mckenzie et al)[13]. However, Snider et al (2011)[14] have shown that the indicated points of the different therapists lie that the distance between the indicated points of the different therapists is much smaller than it had always been claimed. Obviously, there were differences because some therapists have more experience and others have more anatomical knowledge. Also, the difference in personality between the therapists led to differences in locating the processes.
Furthermore, this investigation has proven that it is more useful to indicate different points instead of just 1 point. Also it has been proven that a manual examination to detect the lumbar segmental level is highly accurate when accompanied by a verbal subject response (Philips 1996).[15]
There are of course elements that hinder the palpation. For example, a BMI (body mass index) of 30kg/m2 considerably diminishes the accuracy (Ferre et al)[16]. Anatomical abnormalities might also cause problems. The abnormality of the 12th rib leads, for example, to a negative palpatory accuracy in the region L1-L4 for all therapists. [17]
- Passive Intervertebral Motion (PPIVMs, PAIVMs)
- Muscle Tone
Clear Adjacent Joints[edit | edit source]
| [18] |
- Thoracic spine - seated rotation with combined movements and overpressure
- Sacroiliac joints - various tests have been described to clear the SIJ such as Gillet test, sacral clearing test, cluster tests
- Hips - PROM with overpressure
- Knees and ankles - should also be cleared for restrictions that may affect movement patterns
Special Tests[edit | edit source]
For neurological dysfunction:
- Centralization/peripheralization
- Cross straight leg raise test
- Femoral nerve traction test
- Prone knee bending test or variant
- Slump test or variant
- Straight leg raise or variant
For lumbar instability:
| [19] |
- H and I test
- Passive lumbar extension test
- Prone segmental instability test
- Specific lumbar torsion test
- Test for anterior lumbar spine instability
- Test for posterior lumbar spine instability
For joint dysfunction:
- Bilateral straight leg raise test
- One-leg standing (stork standing) lumbar extension test
- Quadrant test
For muscle tightness:
- 90–90 straight leg raise test
- Ober test
- Rectus femoris test
- Thomas test
Other tests:
Brief Examination[edit | edit source]
If you have little time a brief examination of patients with back pain has two basic purposes.
- Firstly it will help screen patients for possible serious spinal pathology even though taking a good history is much more important.
- Secondly it will improve patient satisfaction and effectiveness of the consultation.
It is suggested that the following be performed as a bare minimum:
- Inspect – general appearance, gross structural deformities
- Active movements – flexion (significant limitation often pathological), extension, side flexion
- Myotomes– rise from a knee squat (L3/4), walk on heels (L4/5) and walk on toes (S1/2).
- SLR (if leg pain or if you feel is needed for reassurance) +/- slump test
Obviously, if the history raises concerns that there may be non-spinal pain, structural deformity, widespread neurological disorder or serious spinal pathology it is appropriate to examine the patient more fully as per normal clinical practice.
What Next?[edit | edit source]
Lumbopelvic disorders are not a homogeneous group of conditions, and subgrouping or classification of patients with back pain has been shown to enhance treatment outcomes[20][21]. Classification of lumbopelvic disorders should adequately define the primary signs and symptoms and guide therapeutic interventions. The examination allows us to arrive at a diagnosis and impairment classification for the condition. These classification systems help us to avoid the pitfalls of attempts to identify the pathoanatomic cause of the patient’s symptoms.
References[edit | edit source]
- ↑ 1.0 1.1 1.2 Koes BW, van Tulder M, Lin C-WC, Macedo LG, McAuley J, Maher C. An updated overview of clinical guidelines for the management of non-specific low back pain in primary care. Eur Spine J 2010;19:2075–94
- ↑ Henschke N, Maher CG, Refshauge KM, et al. Prevalence of and screening for serious spinal pathology in patients presenting to primary care settings with acute low back pain. Arthritis Rheum 2009;60:3072–80.
- ↑ 3.0 3.1 van Tulder M, Becker A, Bekkering T, et al. Chapter 3. European guidelines for the management of acute nonspecific low back pain in primary care. Eur Spine J 2006;15(Suppl 2):S169–91
- ↑ O'Sullivan, P. and Lin, I. Acute low back pain Beyond drug therapies. Pain Management Today, 2014, 1(1):8-14
- ↑ Koes BW, van Tulder MW, Thomas S. Diagnosis and treatment of low back pain. BMJ 2006;332:1430–34.
- ↑ 6.0 6.1 M.Hancock. Approach to low back pain. RACGP, 2014, 43(3):117-118
- ↑ Hancock MJ, Maher CG, Latimer J, et al. Systematic review of tests to identify the disc, SIJ or facet joint as the source of low back pain. Eur Spine J 2007;16:1539–50.
- ↑ 8.0 8.1 Deyo, R. et al. What Can the History and Physical Examination Tell Us About Low Back Pain? JAMA. 1992. 268(6):760-766.
- ↑ Koes B.W. van Tulder M. W., Thomas S.; diagnosis and treatment of low back pain; BMJ volume 332, 17 June 2006; 1430-1434
- ↑ Magee, D. Lumbar Spine. Chapter 9 In: Orthopedic Physical Assessment. Elsevier, 2014
- ↑ Scott Bainbridge. Lumbar Spine Examination. Available from: http://www.youtube.com/watch?v=IijlOJPHk1s[last accessed 19/08/15]
- ↑ tsudpt11's channel. Maitland Lumbar PAIVM (skeletal model). Available from: http://www.youtube.com/watch?v=t0OCzavA6SY[last accessed 19/08/15]
- ↑ McKenzie AM, Taylor NF. Can physiotherapists locate lumbar spinal levels by palpation? Physiotherapy 1997;83: 235-9.
- ↑ Karen T. Snider, Eric J. Snider, Brian F. Degenhardt, Jane C. Johnson and James W. Kribs; palpatory accuracy of lumbar spinous processes using multiple bony landmarks. Journal of Manipulative and Physiological Therapeutics; 2011
- ↑ Phillips D. R.; Twomey L. T.; A comparison of manual diagnosis with a diagnosis established by a uni-level lumbar spinal block procedure; manual therapy, March 1996, pages 82-87
- ↑ 3. Ferre RM, Sweeney TW. Emergency physicians can easily obtain ultrasound images of anatomical landmarks relevant to lumbar puncture. Am J Emerg Med 2007;25:291-6.
- ↑ Karen T. Snider, Eric J. Snider, Brian F. Degenhardt, Jane C. Johnson and James W. Kribs; palpatory accuracy of lumbar spinous processes using multiple bony landmarks. Journal of Manipulative and Physiological Therapeutics; 2011
- ↑ Physical Therapy Nation. Lumbar and SIJ Examination. Available from: http://www.youtube.com/watch?v=EL5tXj81Q8M[last accessed 19/08/15]
- ↑ Ed Schrank. Lumbar Stability Tests. Available from: http://www.youtube.com/watch?v=jDoZ4d09M9Q[last accessed 19/08/15]
- ↑ Brennan GP, Fritz JM, Hunter SJ, et al. Identifying subgroups of patients with acute/subacute “nonspecific” low back pain: results of a randomized clinical trial, Spine 31(6):623–631, 2006.
- ↑ Childs J, Fritz J, Flynn T, et al. A clinical prediction rule to identify patients with low back pain most likely to respond to spinal manipulation: a validation study, Ann Intern Med 141(12):922–928, 2004.