Quebec Back Pain Disability Scale
Original Editor - Your name will be added here if you created the original content for this page.
Top Contributors - Laura Vander Goten, Berdien De Koster, Mariam Hashem, Uchechukwu Chukwuemeka, Lucinda hampton, 127.0.0.1, George Prudden, WikiSysop, Kim Jackson, Amrita Patro and Nupur Smit Shah
Objective [edit | edit source]
The Quebec back pain disability scale (QBPDS) is a condition-specific questionnaire developed to measure the level of functional disability for patients with low back pain (LBP) that was designed, developed, and validated by Kopec et al in 1995. [1]
Original versions of the scale were developed in French and English and were reported to meet the most stringent criteria for a health assessment instrument. Investigators and qualified colleagues translated the English version of the QBPDS into Dutch, Iranian, Brazilian Portuguese, Turkish, Chinese, Greek, Polish, Korean, and Arabic. [2] [3]
The original purpose of the questionnaire is to take into account the functional limitations related to pain, to monitor the progress of individual patients and to compare the evolution of LBP subjects incorporated in rehabilitation programs. [4] [2] [5]
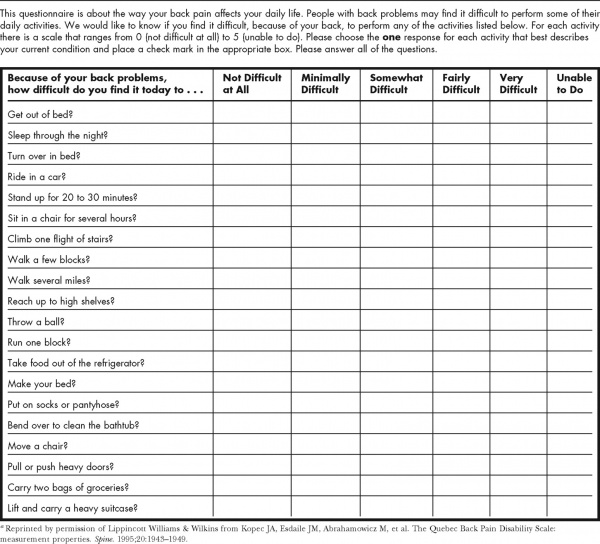
The Quebec back pain disability scale consists of 20 daily activities that can be categorized into 6 types of activities: [1] [2]
- Bed/rest items 1–3
- Sitting/standing items 4–6
- Ambulation items 7–9
- Movement items 10–12
- Bending/stooping items 13–16
- Handling of large/heavy objects items 17–20.
The various components of the questionnaire were selected from a larger pool of items based on test-retest reliability, item-total correlations, and responsiveness of individual items and by using techniques of factor analysis and item response theory. [1]
The scale exists of one central question: “Do you have trouble today with...?” followed by 20 activities of daily life. Some examples of daily activity: taking something out of the fridge, getting out of bed... In every activity, there are 6 answer categories, measured by using a Likert scale from 0-5 (0 = no effort, 5 = not able to). If the patient suffers a lot that day, he scores that activity with a 5, if it gives no problems a 0. [1] [4] [3] The final outcome is obtained by the sum of the scoring of the degree of difficulty in performing the 20 daily activities. These outcomes score within the range of 0 and 100, determents the level of functional disability, with higher numbers representing greater levels of disability. [1][3]
Intended Population[edit | edit source]
The Quebec back pain disability scale has been developed for several populations of patients with various disability levels who suffer diseases such as acute LBP, chronic disabling pain, sacroiliac joint dysfunction, lumbar spinal stenosis, disc surgery, and posterior surgical decompression and settings. (level of evidence: 2 ) [2]
The QBPDS is a useful instrument when someone wants to get an overall impression on the improvement in Pelvic girdle pain. (level of evidence: 2B ) [6]
Method of Use[edit | edit source]
Patients are asked to answer the QBPDS according to the difficulty they have to perform the activities on the current day. The QBPDS examines how lower back pain affects your daily life. It is very important that the patient gives a score for every activity and is not allowed to skip an activity. (level of evidence: 2A) [2]
The scoring is done by counting every digit, circled by the patient. The end score will be between 0 (no limitation) and 100 (totally limited). [4] [2]
It is a very easy questionnaire and takes only five minutes. The QBPDS can be completed by patients by using paper and pen, mail, or telephone. [4]
Evidence[edit | edit source]
The evidence has been extensively examined. (Grade of recommendation: B) [4]
Reliability[edit | edit source]
The ICC is 0,55 (95% CI = 0,20-0,78) in acute occupational low back pain over a period of four weeks. [1]
There is a high internal consistency for the 6-point Likert scale in other languages (Cronbach's a > 0,90). Davidson and Keating examined the test-retest reliability at patients with low back pain who reported no change during six weeks. They found an ICC of 0,85 ([95% CI] 0,73-0,91). This margin of detection is lower in chronic low back pain patients compared with acute low back pain patients. For patients older than 62 years, who suffer acute low back pain, an ICC of 0,94 and a minimal detectable change of 11,04 over a period of 11 days is established. [2] The English, French and Dutch versions have good test-retest reliability. (Grade of recommendation: B) [7]
Validity[edit | edit source]
Construct validity: Construct validity investigates whether the correct variables were measured in relation to the predefined variables. The Quebec back pain disability scale is able to distinguish the difference between patients’ disability levels and self-rated health. (Grade of recommendation: B) [2]
The construct validity of the English, French and Dutch versions is good. (Grade of recommendation: B) [7]
⁃ Internal construct validity: Kopec, the author of the Quebec back pain disability scale, found an inter-item correlation (r) between 0,24 and 0,87 (a relatively high correlation) and an item-total correlation (r) ranged from 0,59 to 0,86 (a relatively very high correlation). The research, after Kopec’s results were published, reported an inter-item correlation lower than 0,80. (Grade of recommendation: B) [2]
⁃ External construct/convergent validity: There is a moderate to strong correlation between the Quebec back pain disability scale (QBPDS) and other disability questionnaires (Grade of recommendation: B):
- QBPDS and Roland-Morris disability questionnaire: r= 0,77-0,81
- QBPDS and Oswestry disability index: r= 0,80- 0,83
- QBPDS and physical function subscale of SF-36: r=0,67- 0,77 [4]
The correlation between the QBPDS and pain (r=0,54- 0,74), psychosocial variables, and direct measures of physical function is weak to moderate. (Grade of recommendation: A) [2][4]
Content and face validity: The questionnaire contains various domains of activities that patients and care providers deem important. Because of this and the good measurement properties, the content and face validity is good. (Grade of recommendation: B) [2]
Responsiveness[edit | edit source]
The responsiveness of the QBPDS is similar to the responsiveness of the Roland-Morris disability questionnaire, modified Oswestry disability questionnaire, Waddell disability index, and the physical function subscale of SF-36. (Grade of recommendation: C) [8]
The QBPDS is highly sensitive to change for the score of the individual domains as for the total score (SRM= 0,80 and effect size= 0,62). [9] In addition, the scale is able to recognize small changes in the level of disability over time. (Grade of recommendation: B) [2] Davidson and Keating found a minimal detectable change of 19 (95% CI 14-24) in patients with low back pain who reported no change during six weeks. For patients with chronic low back pain is minimal detectable change 15.8. (Grade of recommendation: B) [2]
The area under the curve (AUC) can be used as a quantitative method to differentiate patients who improved or deteriorated from the patients who stayed stable. [1] The AUC for the detection of change in patients with chronic low back pain is 0,856. This means that in 85,60 % of the cases the test correctly recognizes a change in chronic low back pain. (Grade of recommendation: B) [2]
Miscellaneous[edit | edit source]
The patients and the clinicians both accept the use of the QBPDS. Researchers (Kopec et al.) declare a low item default (range 0,7-1,8%) [5]. Questionnaires sent by mail had a higher rate of incomplete questionnaires (10.8%). Some patients remarked that a couple of items were not precise enough and the choice between scores 0 and 1 and between 4 and 5 wasn’t always convenient. The researchers didn’t find ceiling or floor effects in the answers. (Grade of recommendation: B) [2]
Resources[edit | edit source]
- The Quebec back pain disability scale website
References[edit | edit source]
References will automatically be added here, see adding references tutorial.
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 Fritz JM, Irrgang JJ. A Comparison of a Modified Oswestry Low Back Pain Disability Questionnaire and the Quebec Back Pain Disability Scale. Physical Therapy 2001; 81: 776-788. (level of evidence: 2B)
- ↑ 2.00 2.01 2.02 2.03 2.04 2.05 2.06 2.07 2.08 2.09 2.10 2.11 2.12 2.13 2.14 Smeets R, Köke A, Lin CW, Ferreira M, Demoulin C. Measures of function in low back pain/disorders: Low Back Pain Rating Scale (LBPRS), Oswestry Disability Index (ODI), Progressive Isoinertial Lifting Evaluation (PILE), Quebec Back Pain Disability Scale (QBPDS), and Roland-Morris Disability Questionnaire (RDQ). Arthritis Care Res (Hoboken). 2011 Nov;63 Suppl 11:S158-73. doi: 10.1002/acr.20542.
- ↑ 3.0 3.1 3.2 Schoppink LE, van Tulder MW, Koes BW, Beurskens SA, de Bie RA. Reliability and validity of the Dutch adaptation of the Quebec Back Pain Disability Scale. Phys Ther. 1996 Mar;76(3):268-75. doi: 10.1093/ptj/76.3.268. (level of evidence: 2B)
- ↑ 4.0 4.1 4.2 4.3 4.4 4.5 4.6 Calmels P, Béthoux F, Condemine A, Fayolle-Minon I. Outils de mesure des paramètres fonctionnels dans la lombalgie [Low back pain disability assessment tools]. Ann Readapt Med Phys. 2005 Jul;48(6):288-97. French. doi: 10.1016/j.annrmp.2005.04.008. Epub 2005 Apr 26. (level of evidence: 2A)
- ↑ 5.0 5.1 Kopec JA, Esdaile JM, Abrahamowicz M, Abenhaim L, Wood-Dauphinee S, Lamping DL, et al. The Quebec Back Pain Disability Scale: conceptualization and development. J Clin Epidemiol. 1996 Feb;49(2):151-61. doi: 10.1016/0895-4356(96)00526-4. (level of evidence: 2B)
- ↑ Vleeming A, Albert HB, Ostgaard HC, Sturesson B, Stuge B. European guidelines for the diagnosis and treatment of pelvic girdle pain. Eur Spine J. 2008 Jun;17(6):794-819. doi: 10.1007/s00586-008-0602-4. (level of evidence: 2B)
- ↑ 7.0 7.1 Peters ML, Vlaeyen JW, Weber WE. The joint contribution of physical pathology, pain-related fear and catastrophizing to chronic back pain disability. Pain. 2005 Jan;113(1-2):45-50. doi: 10.1016/j.pain.2004.09.033. (level of evidence 2B)
- ↑ Davidson M, Keating JL. A comparison of five low back disability questionnaires: reliability and responsiveness. Phys Ther. 2002 Jan;82(1):8-24. doi: 10.1093/ptj/82.1.8. (level of evidence: 2B)
- ↑ Wilhelm F, Fayolle-Minon I, Phaner V, Le-Quang B, Rimaud D, Béthoux F, et al. Sensitivity to change of the Quebec Back Pain Disability Scale and the Dallas Pain Questionnaire. Ann Phys Rehabil Med. 2010 Feb;53(1):15-23. doi: 10.1016/j.rehab.2009.10.004. (level of evidence: 2B)