Treatment‐based classification approach to neck pain: Difference between revisions
No edit summary |
No edit summary |
||
| (85 intermediate revisions by 11 users not shown) | |||
| Line 1: | Line 1: | ||
<div class=" | <div class="editorbox"> | ||
'''Original Editors ''' - [[User:Nora Corbett|Nora Corbett]] and [[User:Jennifer Breithaupt|Jennifer Breithaupt]] from [[Temple University Evidence-Based Practice Project|Temple University's Evidence Based Practice Project]] | |||
''' | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | ||
</div> | </div> | ||
== Introduction == | |||
There are many different ways to [[Classification of Neck Pain|classify individuals with neck pain]] but in recent years the treatment based approach has emerged as a cost-effective way to manage individuals with neck pain. | |||
== | The treatment based classification for individuals with neck pain was first proposed in 2004 by Childs et al<ref name=":0">Childs MJ, Fritz JM, Piva SR, Whitman JM. [http://www.jospt.org/doi/pdf/10.2519/jospt.2004.34.11.686 Proposal of a classification system for patients with neck pain.] Journal of Orthopaedic & Sports Physical Therapy. 2004 Nov;34(11):686-700.</ref>, the system was based on the overall goal of treatment rather than an attempt to classify patients by pathology or symptom distribution. In 2007 Fritz and Brennan<ref name=":1">Fritz JM, Brennan GP. [http://www.ncbi.nlm.nih.gov/pubmed/17374633 Preliminary examination of a proposed treatment-based classification system for patients receiving physical therapy interventions for neck pain]. Phys Ther. 2007;87(5):513-24</ref> validated this classification system by finding that receiving interventions matched to the classification system was associated with better outcomes than receiving non-matched interventions. It was updated in 2008 as part of the APTA Orthopaedic section [[ICF in Relation to Wheelchair Users|ICF]] Guidelines with the four current classification categories including: | ||
* Neck pain with mobility deficits. | |||
* Neck pain with radiating pain ([[Cervical Radiculopathy|radicular]]). | |||
* Neck pain with movement coordination impairments ([[Whiplash Associated Disorders|WAD]]). | |||
* Neck pain with headache ([[Cervicogenic Headache|cervicogenic]]). | |||
It is recognised that additional decision making is necessary within each classification to more specifically guide the application of the selected intervention. However, the first step in the use of a classification system is to direct initial interventions toward the optimal treatment for the individual's presentation. | |||
== Classification == | |||
Proposed causes of neck pain include: | |||
* [[Cervical Spondylosis|Degenerative changes]] | |||
* Disc protrusion | |||
* [[Cervical Radiculopathy|Nerve impingement]] and impaired function of muscle | |||
* Connective tissue | |||
* Nervous tissue<ref name="Cote">Cote P, Cassidy JD, Carroll LJ, Krisman V.[http://www.ncbi.nlm.nih.gov/pubmed/15561381 The Annual Incidence and Course of Neck Pain in the General Population: A Population-Based Cohort Study].Pain.2004;112: 267-273</ref>. | |||
Beyond identifying serious pathology [[Red Flags in Spinal Conditions|( red flags]])such as fractures, diagnostic imaging is not often useful in identifying the tissue source of the patient’s neck pain. Many imaging findings such as spondylosis and herniated discs are found commonly in individuals without pain<ref name="Cote" /> Therefore, this classification is based on the patient’s presenting signs, symptoms, and impairments rather than pathoanatomical sources of pain and is designed to assist the clinician with matching an initial treatment intervention strategy to an individuals presentation. | |||
== | === Is The Individual Appropriate For Treatment? === | ||
Initially, individuals with neck pain should be properly screened for potentially [[Serious Cervical Spine Conditions|serious pathology]] such as fracture, instability, CAD, myelopathy, cancer, infection, and visceral disorders. | |||
=== Is the Individual Ready For Treatment? === | |||
Factors which are associated with [[The Flag System|personal and environmental factors]] that might perpetuate a patient’s neck pain should also be considered including: | |||
* Psychosocial factors such as fear-avoidance beliefs, depression, anxiety, and catastrophizing. | |||
* Environmental factors such as ergonomic considerations, occupation, and recreational activities | |||
Identifying psychosocial or environmental factors during the evaluation can direct the therapist to employ specific education strategies to optimise the outcomes of physical therapy interventions. | |||
== | == Differential Diagnosis == | ||
Once serious pathology has been ruled out and personal and environmental factors considered and the individual considered as suitable for intervention, the therapist can continue with the examination that will direct classification. Differential evaluation of musculoskeletal clinical findings is used to determine the most relevant physical impairments associated with the patient’s reported activity limitations and medical diagnosis. | |||
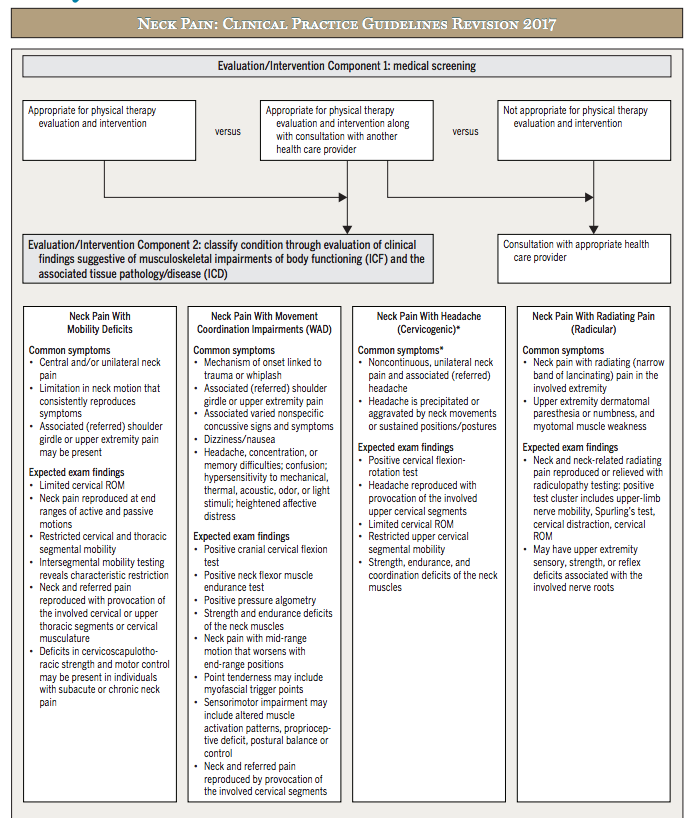
[[File:Neck Pain Revision Decision Tree 2017.png|frameless|818x818px]] | |||
Therapists must recognise that these categories will not be exclusive or exhaustive, the assignation of an individual into the category that “best fits” their current clinical picture relies on clinical reasoning and judgment of the clinician. | |||
== Determine Stage == | |||
Acute, subacute, and chronic stages are time-based stages helpful in classifying patient conditions. Time-based stages are helpful in making treatment decisions only in the sense that: | |||
# In '''the acute phase''', the condition is usually highly irritable (pain experienced at rest or with initial to mid-range spinal movements: before tissue resistance). | |||
# In '''the subacute phase''', the condition often exhibits moderate irritability (pain experienced with mid-range motions that worsen with end-range spinal movements: with tissue resistance). | |||
# '''chronic conditions''' often have a low degree of irritability (pain that worsens with sustained end-range spinal movements or positions: overpressure into tissue resistance). | |||
There are cases where the alignment of irritability and the duration of symptoms does not match accordingly, requiring clinicians to make judgments when applying time-based research results on a patient-by-patient basis. | |||
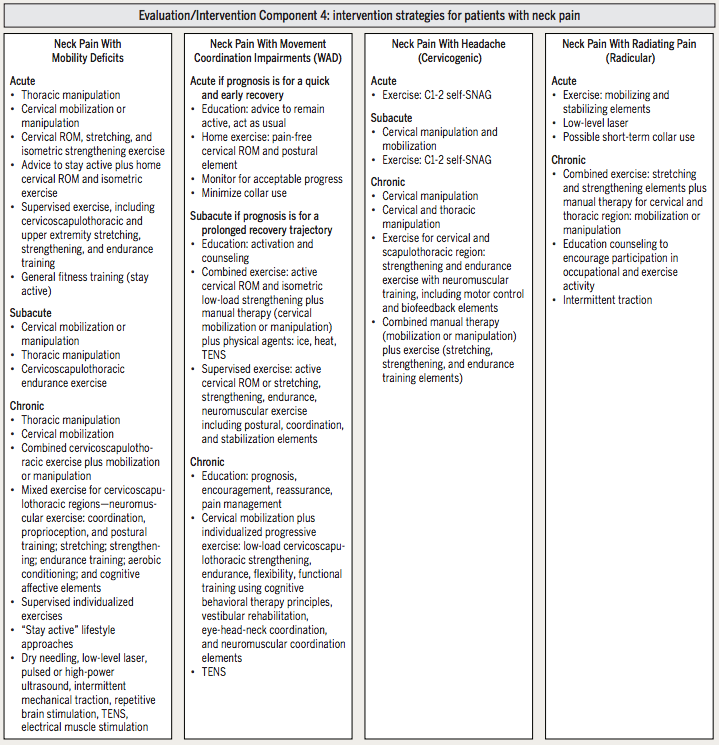
== Intervention Strategies == | |||
[[File:Intervention strategies for patients with neck pain.png|class=mw-ref|frameless|745x745px]] | |||
== Continual Reassessment and Reasoning == | |||
Each individual has a primary goal of treatment at a given period during the course of management, making the classification categories mutually exclusive at a single point in time. However, the process of classification is ongoing and it is anticipated that an individuals presentation will change with time and treatment. Ongoing reassessment is, therefore, necessary to determine the most appropriate intervention at any point in time<ref name=":0" />. | |||
== Resources == | |||
[https://www.google.fr/url?sa=t&rct=j&q=&esrc=s&source=web&cd=1&cad=rja&uact=8&ved=0ahUKEwicif-jrcDWAhVGbBoKHan1DT8QFggoMAA&url=https%3A%2F%2Fwww.orthopt.org%2Fuploads%2Fcontent_files%2Ffiles%2FNeck%2520Pain%2520Revision%2520Decision%2520Tree%25202017%2520 Neck Pain Revision Decision Tree] | |||
== | |||
== | |||
== References == | == References == | ||
<references /> <br> | |||
<references /> | |||
[[Category:Interventions]] | |||
[[Category:Cervical Spine - Interventions]] | |||
[[Category:Cervical Spine]] | |||
[[Category:Pain]] | |||
[[Category:Musculoskeletal/Orthopaedics]] | |||
[[Category:Temple Student Project]] | |||
Latest revision as of 11:49, 15 November 2023
Original Editors - Nora Corbett and Jennifer Breithaupt from Temple University's Evidence Based Practice Project
Top Contributors - Nora Corbett, Admin, Rachael Lowe, Jennifer Breithaupt, Kim Jackson, Evan Thomas, Shaimaa Eldib, Scott A Burns, Simisola Ajeyalemi, Jess Bell and WikiSysop
Introduction[edit | edit source]
There are many different ways to classify individuals with neck pain but in recent years the treatment based approach has emerged as a cost-effective way to manage individuals with neck pain.
The treatment based classification for individuals with neck pain was first proposed in 2004 by Childs et al[1], the system was based on the overall goal of treatment rather than an attempt to classify patients by pathology or symptom distribution. In 2007 Fritz and Brennan[2] validated this classification system by finding that receiving interventions matched to the classification system was associated with better outcomes than receiving non-matched interventions. It was updated in 2008 as part of the APTA Orthopaedic section ICF Guidelines with the four current classification categories including:
- Neck pain with mobility deficits.
- Neck pain with radiating pain (radicular).
- Neck pain with movement coordination impairments (WAD).
- Neck pain with headache (cervicogenic).
It is recognised that additional decision making is necessary within each classification to more specifically guide the application of the selected intervention. However, the first step in the use of a classification system is to direct initial interventions toward the optimal treatment for the individual's presentation.
Classification[edit | edit source]
Proposed causes of neck pain include:
- Degenerative changes
- Disc protrusion
- Nerve impingement and impaired function of muscle
- Connective tissue
- Nervous tissue[3].
Beyond identifying serious pathology ( red flags)such as fractures, diagnostic imaging is not often useful in identifying the tissue source of the patient’s neck pain. Many imaging findings such as spondylosis and herniated discs are found commonly in individuals without pain[3] Therefore, this classification is based on the patient’s presenting signs, symptoms, and impairments rather than pathoanatomical sources of pain and is designed to assist the clinician with matching an initial treatment intervention strategy to an individuals presentation.
Is The Individual Appropriate For Treatment?[edit | edit source]
Initially, individuals with neck pain should be properly screened for potentially serious pathology such as fracture, instability, CAD, myelopathy, cancer, infection, and visceral disorders.
Is the Individual Ready For Treatment?[edit | edit source]
Factors which are associated with personal and environmental factors that might perpetuate a patient’s neck pain should also be considered including:
- Psychosocial factors such as fear-avoidance beliefs, depression, anxiety, and catastrophizing.
- Environmental factors such as ergonomic considerations, occupation, and recreational activities
Identifying psychosocial or environmental factors during the evaluation can direct the therapist to employ specific education strategies to optimise the outcomes of physical therapy interventions.
Differential Diagnosis[edit | edit source]
Once serious pathology has been ruled out and personal and environmental factors considered and the individual considered as suitable for intervention, the therapist can continue with the examination that will direct classification. Differential evaluation of musculoskeletal clinical findings is used to determine the most relevant physical impairments associated with the patient’s reported activity limitations and medical diagnosis.
Therapists must recognise that these categories will not be exclusive or exhaustive, the assignation of an individual into the category that “best fits” their current clinical picture relies on clinical reasoning and judgment of the clinician.
Determine Stage[edit | edit source]
Acute, subacute, and chronic stages are time-based stages helpful in classifying patient conditions. Time-based stages are helpful in making treatment decisions only in the sense that:
- In the acute phase, the condition is usually highly irritable (pain experienced at rest or with initial to mid-range spinal movements: before tissue resistance).
- In the subacute phase, the condition often exhibits moderate irritability (pain experienced with mid-range motions that worsen with end-range spinal movements: with tissue resistance).
- chronic conditions often have a low degree of irritability (pain that worsens with sustained end-range spinal movements or positions: overpressure into tissue resistance).
There are cases where the alignment of irritability and the duration of symptoms does not match accordingly, requiring clinicians to make judgments when applying time-based research results on a patient-by-patient basis.
Intervention Strategies[edit | edit source]
Continual Reassessment and Reasoning[edit | edit source]
Each individual has a primary goal of treatment at a given period during the course of management, making the classification categories mutually exclusive at a single point in time. However, the process of classification is ongoing and it is anticipated that an individuals presentation will change with time and treatment. Ongoing reassessment is, therefore, necessary to determine the most appropriate intervention at any point in time[1].
Resources[edit | edit source]
Neck Pain Revision Decision Tree
References[edit | edit source]
- ↑ 1.0 1.1 Childs MJ, Fritz JM, Piva SR, Whitman JM. Proposal of a classification system for patients with neck pain. Journal of Orthopaedic & Sports Physical Therapy. 2004 Nov;34(11):686-700.
- ↑ Fritz JM, Brennan GP. Preliminary examination of a proposed treatment-based classification system for patients receiving physical therapy interventions for neck pain. Phys Ther. 2007;87(5):513-24
- ↑ 3.0 3.1 Cote P, Cassidy JD, Carroll LJ, Krisman V.The Annual Incidence and Course of Neck Pain in the General Population: A Population-Based Cohort Study.Pain.2004;112: 267-273