Cervical Myelopathy: Difference between revisions
No edit summary |
No edit summary |
||
| (61 intermediate revisions by 16 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox"> | <div class="editorbox"> | ||
'''Original Editors '''- [[User:Bridgit A Finley|Bridgit A Finley | '''Original Editors '''- [[User:Bridgit A Finley|Bridgit A Finley]] | ||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | ||
</div> | </div> | ||
== Introduction == | |||
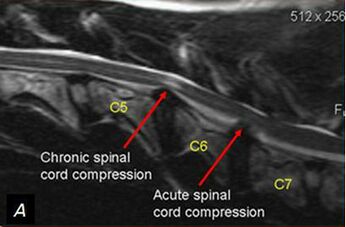
[[File:Compressive myeolopathy C6C7.png|thumb|Cervical myelopathy C6-C7]] | |||
Cervical [[myelopathy]] is a condition involving compression of the [[Spinal cord anatomy|spinal cord]] at the [[Cervical Anatomy|cervical]] level of the spinal column resulting in [[spasticity]], hyperreflexia, pathologic [[reflexes]], digit/hand clumsiness, and/or [[Gait: Antalgic|gait disturbance.]] | |||
The spontaneous course of myelopathy is characterised either by long periods of stable disability followed by episodes of deterioration or a linear progressive course. The presentation of a cervical myelopathy varies in accordance with the severity of the spinal cord compression as well as its location.Without treatment, patients may progress toward significant paralysis and loss of function. .<ref name="Boos">Boos N and Aebi M (Eds). Spinal disorders: Fundamentals of Diagnosis and Treatment. Springer-Verlag Berlin Heidelberg. 2008.</ref> | |||
Any space-occupying lesion within the cervical spine with the potential to compress the spinal cord can cause cervical myelopathy.<ref name="Richard">Richard K. Root Clinical Infectious Diseases: A Practical Approach, 1999</ref><ref name="Kong">Kong LD, Meng LC, Wang LF, Shen Y, Wang P and Shang ZK. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3786935/ Evaluation of conservative treatment and timing of surgical intervention for mild forms of cervical spondylotic myelopathy.] Exp Ther Med. 2013 Sep;6(3):852-856.</ref> Cervical myelopathy is predominantly due to pressure on the anterior spinal cord with ischemia as a result of deformation of the cord by anterior [[Disc Herniation|herniated discs]], spondylitic [[Osteophyte|bone spurs]], an ossified [[posterior longitudinal ligament]] or [[Cervical Stenosis|spinal stenosis]]<ref name="Dai">Dai L, Ni B, Yuan W and Jia L. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3786935/ Radiculopathy after laminectomy for cervical compression myelopathy.] J Bone Joint Surg Br. 1998 Sep;80(5):846-9.</ref> | |||
== Clinically Relevant Anatomy == | |||
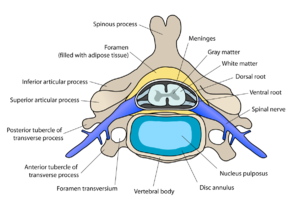
[[File:Cervical vertebra english.png|thumb|Cervical Vertebra]] | |||
There are seven [[Cervical Anatomy|cervical vertebrae]] and eight cervical nerve roots.<ref name="Kong" /><ref name="Cook">Cook C, Brown C, Isaacs R, Roman M, Davis S, Richardson W. [https://www.researchgate.net/publication/51844211_Clustered_clinical_findings_for_diagnosis_of_cervical_spine_myelopathy Clustered clinical findings for diagnosis of cervical spine myelopathy.] Journal of Manual & Manipulative Therapy. 2010 Dec 1;18(4):175-80.</ref> The spinal cord is the extension of the central nervous system outside the cranium. It is encased by the vertebral column and begins at the foramen magnum.<ref name="Cramer">Cramer GD and Darby SA. Basic and Clinical Anatomy of the Spine, Spinal Cord, and ANS. 2nd Edition. Elsevier 2008.</ref> The spinal cord is an extremely vital part of the central nervous system, and even a small injury can lead to severe disability.<ref name="Selzer">Selzer ME and Dobkin BH. Spinal Cord Injury (American Academy of Neurology Quality of Life Series). Demos Medical Publishing (New York). 2008</ref> | |||
A complex system of ligaments serves to stabilise and protect the cervical spine. For example, [[ligamentum flavum]] extends from the anterior surface of the cephalic vertebra to the posterior surface of the caudal vertebra and connects to the ventral aspect of the facet joint capsules. A ligament that is often involved in this condition is the [[posterior longitudinal ligament]]. It is situated within the vertebral canal, originating from the body of the [[axis]], where it is continuous with the [[tectorial membrane]], and extends along the posterior surfaces of the bodies of the vertebrae until inserting into the [[sacrum]].<ref name="Selzer" /> | |||
== Epidemiology == | |||
* [[Cervical Spondylosis|Cervical spondylotic]] myelopathy is the most common disorder of the spinal cord in persons older than 55 years of age.<ref name="Cook" /><ref name="Amenta">Amenta PS, Ghobrial GM, Krespan K, Nguyen P, Ali M, Harrop JS. [https://pubmed.ncbi.nlm.nih.gov/24731579/ Cervical spondylotic myelopathy in the young adult: a review of the literature and clinical diagnostic criteria in an uncommon demographic.] Clinical neurology and neurosurgery. 2014 May 1;120:68-72.</ref><ref name="Kadanka">Kadaňka Z, Bednařík J, Voháňka S, Vlach O, Stejskal L, Chaloupka R, Filipovičová D, Šurelová D, Adamová B, Novotný O, Němec M. [https://pubmed.ncbi.nlm.nih.gov/11189924/ Conservative treatment versus surgery in spondylotic cervical myelopathy: a prospective randomised study.] European Spine Journal. 2000 Dec;9(6):538-44.</ref> | |||
* Radiologic spondylotic changes increase with patient age - 90% of asymptomatic persons older than 70 years have some form of degenerative change in the cervical spine. Cervical spine myelopathy resulting from sagittal narrowing of the spinal canal and compression of the spinal cord is present in 90% of individuals by the seventh decade of life.<ref name="cook">Cook C, Roman M, Stewart KM, Leithe LG, Isaacs R. [https://www.jospt.org/doi/10.2519/jospt.2009.2938 Reliability and diagnostic accuracy of clinical special tests for myelopathy in patients seen for cervical dysfunction.] journal of orthopaedic & sports physical therapy. 2009 Mar;39(3):172-8.</ref> | |||
* Both sexes are affected equally. Cervical spondylosis usually starts earlier in men (50 years) than in women (60 years). | |||
* It causes hospitalisation at a rate of 4.04 per 100,000 person-years.<ref name="Cook" /><ref name="Koakutsu">Koakutsu T, Nakajo J, Morozumi N, Hoshikawa T, Ogawa S, Ishii Y. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3078542/ Cervical myelopathy due to degenerative spondylolisthesis. U]psala journal of medical sciences. 2011 May 1;116(2):129-32.</ref> | |||
== Etiology == | |||
[[File:Muscles of the cervical region multifidus superficial layer Primal.png|thumb|Cervical region: Multifidus Superficial]] | |||
The causes of cervical myelopathy can be divided into different categories: | The causes of cervical myelopathy can be divided into different categories: | ||
# '''Static factors:''' A narrowing of the spinal canal size commonly results from degenerative changes in the [[Cervical Anatomy|cervical spine]] anatomy ([[Cervical Spondylosis|cervical spondylosis]]) such as [[Intervertebral Disc Disease: Lumbar Intervertebral Disc Herniation|disc degeneration]], spondylosis, stenosis, [[osteophyte]] formation at the level of [[Facet Joints|facet joints]], segmental ossification of the posterior longitudinal ligament and yellow ligament hypertrophy, calcification or ossification. Patients with a congenitally narrow spinal canal (<13mm) have a higher risk for the development of symptomatic cervical myelopathy.<ref name="Boos" /><ref name="cook" /><ref name="Koakutsu" /><ref name="Yonenobu">Yonenobu K. [https://pubmed.ncbi.nlm.nih.gov/10766070/ Cervical radiculopathy and myelopathy: when and what can surgery contribute to treatment?.] European Spine Journal. 2000 Feb;9(1):1-7.</ref>[[Cervical Spondylosis|Chronic cervical degeneration]] is the most common cause of progressive spinal cord and nerve root compression. Spondylotic changes can result in stenosis of the spinal canal, lateral recess, and foramina. Spinal canal stenosis can lead to myelopathy, whereas the latter two can lead to [[radiculopathy]]. | |||
# '''Dynamic factors:''' Due to mechanical abnormalities of the cervical spine or instability.<ref name="Boos" /> | |||
# '''Vascular and cellular factors:''' Spinal cord ischemia affects [[Glial Cells|oligodendrocytes]], which results in demyelination exhibiting features of chronic degenerative disorders. Glutamatergic toxicity, cell injury and apoptosis may also occur.<ref name="Boos" /> | |||
Cord compression is thought to be a combination of static compression and intermittent dynamic compression from cervical motion (flexion/extension). | |||
== Characteristics and Clinical Presentation == | |||
Cervical myelopathy can cause a variety of signs and symptoms. | |||
* Cervical spondylotic myelopathy frequently involve compression of the lateral [[Corticospinal Tract|corticospinal]] tracts resulting in (voluntary skeletal muscle control), and the spinocerebellar tracts ([[proprioception]]). It causes classic signs: the wide-based spastic gait with clumsy upper extremity function.<ref name=":1">Donnally III CJ, Hanna A, Odom CK. [https://www.ncbi.nlm.nih.gov/books/NBK482312/ Cervical myelopathy.] StatPearls [Internet]. 2021 Mar 6.</ref> | |||
Cervical spondylotic myelopathy | * Onset is insidious, typically in persons aged 50-60 years. Because of the lack of [[Pain Assessment|pain]], there may be an interval of years between the onset of disease and first treatment. Progression takes place in a stepwise manner with functional decline. | ||
* Early symptoms of this condition: numb, clumsy, painful hands, disturbance of fine motor skills.<ref name="Boos" /> | |||
* Weakness and numbness occur in a non-specific/non-dermatomal pattern. | |||
* Additional clinical findings may include neck pain and stiffness (decreased ROM, especially extension), shoulder and scapular pain, paresthaesia in one or both arms or hands, signs of radiculopathy, [[Babinski Sign|Babinski]] and [[Hoffmann's Sign|Hoffmann's]] sign, [[ataxia]] and dexterity loss.<ref name="Cook" /><ref name="Harrop">Harrop JS, Naroji S, Maltenfort M, Anderson DG, Albert T, Ratliff JK, Ponnappan RK, Rihn JA, Smith HE, Hilibrand A, Sharan AD. [https://pubmed.ncbi.nlm.nih.gov/20150835/ Cervical myelopathy: a clinical and radiographic evaluation and correlation to cervical spondylotic myelopathy.] Spine. 2010 Mar 15;35(6):620-4.</ref><ref name="Park">Park SJ, Kim SB, Kim MK, Lee SH, Oh IH. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3941769/ Clinical features and surgical results of cervical myelopathy caused by soft disc herniation.] Korean Journal of Spine. 2013 Sep;10(3):138.</ref> | |||
* Typical neurological signs of long-tract involvement are exaggerated tendon reflexes (patellar and Achilles), presence of pathological reflexes (e.g. clonus, Babinski and Hoffman's sign), spastic quadriplegia, sensory loss and bladder-bowel disturbance.<ref name="Yonenobu" />Indicators of poor prognosis include bowel or bladder dysfunction, and general weakness.<ref name=":1" /> | |||
Once the disorder is diagnosed, complete remission to normality never occurs and spontaneous temporary remission is uncommon. In 75% of the patients, episodic worsening with neurological deterioration occurs, 20% have slow steady progression, and 5% experience rapid onset and progression.<ref name="Boos" /> | |||
'''Common Symptoms''' | |||
*Distal weakness | *Distal weakness | ||
*Decreased ROM in the cervical spine, especially extension. | *Decreased ROM in the cervical spine, especially extension. | ||
*Clumsy or weak hands | *Clumsy or weak hands with difficulty in fine motor movements. | ||
*Pain in shoulder or arms | *Pain in shoulder or arms | ||
*Unsteady or clumsy gait | *Unsteady or clumsy gait | ||
*Increased reflexes in the lower extremities and in the upper extremities below the level of the lesion. | *Increased reflexes in the lower extremities and in the upper extremities below the level of the lesion. | ||
*Numbness and | *Numbness and paresthesia in one or both hands | ||
* | *Radiculopathy signs | ||
== Diagnostic Procedures == | |||
A detailed and thorough neurological examination plus MRI is the current standard to diagnose the presence of cervical myelopathy. | |||
[[File:Cervical Myelopathy.jpg|thumb|alt=|346x346px|Cervical Myelopathy]] | |||
Plain radiographs alone are of little use as an initial diagnostic procedure. A magnetic resonance image (MRI) is considered the best imaging method for confirming the presence of spinal canal stenosis, cord compression, or myelomalacia, elements germane to cervical spine myelopathy. MRI of the cervical spine can also rule out [[Spinal Malignancy|spinal cord tumours.]] | |||
An MRI is most useful because it expresses the amount of compression placed on the spinal cord and demonstrates relatively high levels of sensitivity and specificity<ref name="Cook" /><ref name="Harrop" />. Anterior-posterior width reduction, cross-sectional evidence of cord compression, obliteration of the subarachnoid space and signal intensity changes to the cord found on MR imaging are considered the most appropriate parameters for confirmation of a spinal cord compression myelopathy<ref name="Cook" />. More than half of patients with cervical spine myelopathy show intramedullary high signal intensity on T2-weighted imaging, mainly in the spinal gray matter<ref name="Sato">Sato T, Horikoshi T, Watanabe A, Uchida M, Ishigame K, Araki T, Kinouchi H. [http://www.ajnr.org/content/33/2/388 Evaluation of cervical myelopathy using apparent diffusion coefficient measured by diffusion-weighted imaging.] American journal of neuroradiology. 2012 Feb 1;33(2):388-92.0</ref>. Radiographic cervical spinal cord compression and hyperintense T2 intraparenchymal signal abnormalities (MRI) correlate well with the presence of myelopathic findings on physical examination.<ref name="Harrop" />{{#ev:youtube|mJVEtq5GsJk|300}}<ref>Stanford Imaging Patients with Myelopathy. Available from https://www.youtube.com/watch?time_continue=5&v=mJVEtq5GsJk</ref> | |||
== Clinical Examination == | |||
The diagnosis of CSM is primarily based on the clinical signs found on physical examination and is supported by imaging findings.<ref name="Amenta" /> According to Cook et al,<ref name="cook 2">Cook C, Brown C, Isaacs R, Roman M, Davis S, Richardson W. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3113267/ Clustered clinical findings for diagnosis of cervical spine myelopathy.] Journal of Manual & Manipulative Therapy. 2010 Dec 1;18(4):175-80.</ref> selected combinations of the following clinical findings are effective in ruling out and ruling in cervical spine myelopathy. Combinations of three of five or four of five of these tests enable post-test probability of the condition to 94–99%: | |||
#Gait deviation | |||
#+ve [[Hoffmann's Sign|Hoffmann’s test]] | |||
#[[Inverted Supinator Test|Inverted supinator sign]] | |||
#+ve [[Babinski Sign|Babinski sign]] | |||
#Age 45 years or older | |||
Other clinical examination tests often used for myelopathy include:<ref name="Cook" /><ref name="Amenta" /> | |||
*[[ | *[[Spurling's Test|Spurling’s test]] | ||
*Brown-Sequard Syndrome | *[[Cervical Distraction Test|Distraction test]] | ||
*+ve Clonus/Babinski/Hoffman's | |||
*Hyper-reflexic biceps | |||
*Hyper-reflexic quadriceps | |||
*Hyper-reflexic Achilles | |||
*Pain constancy | |||
*[[Lhermitte's Sign|Lhermitte’s sign]] | |||
*[[Romberg Test|Romberg test]] | |||
Although these tests exhibit moderate to substantial reliability among skilled clinicians, they demonstrate low sensitivity and are not appropriate for ruling out myelopathy. One method used to improve the diagnostic accuracy of clinical testing is combining tests into clusters. These often overcome the inherent weakness of stand-alone tests.<ref name="Cook" /><ref name="cook 2" /> | |||
==Outcome Measures== | |||
* [[Neck Disability Index|Neck disability index]] | |||
* [[Neck Pain and Disability Scale|Neck pain and disability scale]] | |||
* Nurick-score <ref name="Vitzthum">Vitzthum HE, Dalitz K. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2140133/ Analysis of five specific scores for cervical spondylogenic myelopathy]. European Spine Journal. 2007 Dec;16(12):2096-103.</ref> | |||
* Japanese-orthopaedic-association-score (JOA-Score) <ref name="Vitzthum" /> <ref name="Tanaka">Tanaka N, Konno SI, Takeshita K, Fukui M, Takahashi K, Chiba K, Miyamoto M, Matsumoto M, Kasai Y, Kanamori M, Matsunaga S. [https://pubmed.ncbi.nlm.nih.gov/24317702/ An outcome measure for patients with cervical myelopathy: the Japanese Orthopaedic Association Cervical Myelopathy Evaluation Questionnaire (JOACMEQ): an average score of healthy volunteers.] Journal of Orthopaedic Science. 2014 Jan 1;19(1):33-48.</ref> | |||
* Cooper-myelopathy-scale (CMS) <ref name="Vitzthum" /> | |||
* European-myelopathy-score (EMS) | |||
== Differential Diagnosis == | |||
*[[Frozen Shoulder|Adhesive Capsulitis]] | |||
*[[Brown-Sequard Syndrome]] | |||
*[[Carpal Tunnel Syndrome|Carpal Tunnel Syndrome]] | *[[Carpal Tunnel Syndrome|Carpal Tunnel Syndrome]] | ||
*Central Cord Syndrome | *[[Central Cord Syndrome]] | ||
*Cervical Disc Disease | *Cervical Disc Disease | ||
*Cervical Myofascial Pain | *Cervical [[Myofascial Pain]] | ||
*Cervical Sprain and Strain | *Cervical Sprain and Strain | ||
*Chronic Pain Syndrome | *[[Chronic Pain|Chronic Pain Syndrome]] | ||
*Diabetic Neuropathy | *Diabetic Neuropathy | ||
*[[ | *[[Multiple Sclerosis (MS)|Multiple Sclerosis]] | ||
*Myofascial Pain | *Myofascial Pain | ||
*Neoplastic Brachial Plexopathy | *Neoplastic Brachial Plexopathy | ||
*[[Osteoporosis|Osteoporosis]] | *[[Osteoporosis|Osteoporosis]] | ||
*Spinal Cord Injury | *[[Spinal Cord Injury]] | ||
*Radiation-Induced Brachial Plexopathy | *Radiation-Induced Brachial Plexopathy | ||
*[[Rheumatoid Arthritis|Rheumatoid Arthritis]] | *[[Rheumatoid Arthritis|Rheumatoid Arthritis]] | ||
*Traumatic Brachial Plexopathy | *Traumatic Brachial Plexopathy | ||
*Tumors | *Tumors | ||
*[[Arnold Chiari Malformation|Chiari malformation]] | |||
*[[Guillain-Barre Syndrome|Guillain-Barre syndrome]] | |||
*Syrinx | |||
== Management == | |||
There is no consensus about the treatment of mild and moderate forms of cervical myelopathy. Surgical treatment has no better results than conservative treatment over two years of follow-up.<ref name="Kadanka" /> Patients with cervical myelopathy that are treated with a conservative approach (anti-inflammatory medication and physical therapy) may have some short term benefit in relief of painful symptoms. Because the condition is degenerative and progressive, slow and continued progressive neurologic deterioration will occur. | |||
=== Medical Management === | |||
People who have progressive neurologic changes (such as weakness, numbness or falling) with signs of severe spinal cord compression or spinal cord swelling are candidates for surgery. Patients with severe or disabling pain may also be helped with surgery.<ref name="Almeida">Almeida GP, Carneiro KK, Marques AP. [https://europepmc.org/article/med/24139010 Manual therapy and therapeutic exercise in patient with symptomatic cervical spondylotic myelopathy: A case report.] Journal of bodywork and movement therapies. 2013 Oct 1;17(4):504-9.</ref> When myelopathy is caused by factors of a progressive nature, such as spinal cord tumors, surgical treatment is likewise indicated<ref name="1 Massimo Leonardi, Norbert Boos , Degenerative disorders of the cervical spine">Leonardi M, Boos N. [https://link.springer.com/chapter/10.1007%2F978-3-540-69091-7_17 Degenerative disorders of the cervical spine.] InSpinal Disorders 2008 (pp. 429-479). Springer, Berlin, Heidelberg.</ref><ref>Law Jr MD, Bernhardt M, White 3rd AA. [https://pubmed.ncbi.nlm.nih.gov/8209553/ Cervical spondylotic myelopathy: a review of surgical indications and decision making.] The Yale journal of biology and medicine. 1993 May;66(3):165.</ref>. | |||
People who experience better surgical outcomes often have these characteristics: | |||
* The symptom of an electrical sensation that runs down the back and into the limbs | |||
* Younger age | |||
* Shorter duration of symptoms | |||
* Single rather than multiple areas of involvement | |||
* Larger areas available for the cord | |||
The principal aim of surgery for cervical myelopathy is decompression of the spinal cord. Surgical techniques include multi-level discectomies or corpectomies with or without instrumented fusion, laminectomy with or without instrumented fusion or laminoplasty<ref name="Boos" />. Surgical decompression is generally considered if the symptoms affect daily life, but early surgical intervention is thought to be more effective. Therefore, early detection may be the key to minimise postoperative degeneration<ref name="Sato" />. | |||
Final outcomes from the surgery vary. Typically, one-third of patients improve, one-third stay the same, and one-third continue to worsen over time, with respect to their pre-surgical symptoms<ref name="Kadanka" /><ref name="Almeida" /> | |||
[[ | === Physical Therapy Management === | ||
Patients can be treated conservatively. ''Kadaňka et al.'' found no difference in long term outcomes (2 years after the intervention) between patient who received conservative or surgical treatment. <ref name="Kadanka" />Even after 10 years, there were no differences found between the surgery and conservative group<ref>Kadaňka Z, Bednařík J, Novotný O, Urbánek I, Dušek L. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3175900/ Cervical spondylotic myelopathy: conservative versus surgical treatment after 10 years.] European Spine Journal. 2011 Sep;20(9):1533-8.</ref> . ''Fouyas et al'' also confirmed these findings. <ref name=":0">Fouyas IP, Statham PF, Sandercock PA. [https://pubmed.ncbi.nlm.nih.gov/11923667/ Cochrane review on the role of surgery in cervical spondylotic radiculomyelopathy]. Spine. 2002 Apr 1;27(7):736-47. </ref> The only prognostic factor in which surgery can be generally recommended is with a circumferential spinal cord compression seen on an axial MRI.<ref>Shimomura T, Sumi M, Nishida K, Maeno K, Tadokoro K, Miyamoto H, Kurosaka M, Doita M. [https://pubmed.ncbi.nlm.nih.gov/18090088/ Prognostic factors for deterioration of patients with cervical spondylotic myelopathy after nonsurgical treatment.] Spine. 2007 Oct 15;32(22):2474-9. </ref> | |||
''Rhee JM et al.'' describes myelopathy as a typically progressive disorder and that there is little of evidence that conservative treatment halts or reverses its progression. So they recommend routinely not prescribing non-operative treatment as the primary modality in patients with moderate to severe myelopathy.<ref>Rhee JM, Shamji MF, Erwin WM, Bransford RJ, Yoon ST, Smith JS, Kim HJ, Ely CG, Dettori JR, Patel AA, Kalsi-Ryan S. [https://pubmed.ncbi.nlm.nih.gov/23963006/ Nonoperative management of cervical myelopathy: a systematic review.] Spine. 2013 Oct 15;38(22S):S55-67. </ref> | |||
The goals of physiotherapy treatment are: <ref name="Boos" /> | |||
* pain relief | |||
* to improve function | |||
* to prevent neurological deterioration | |||
* to reverse or improve neurological deficits | |||
Cervical myelopathy can be treated symptomatically. Possible therapies include: | Cervical myelopathy can be treated symptomatically. Possible therapies include: | ||
==== Cervical traction and manipulation of the thoracic spine ==== | |||
This is useful for the reduction of pain scores and level of disability in patients with mild cervical myelopathy. Other signs and symptoms, such as weakness, headache, dizziness, and hypoesthesia, can also be positively affected<ref name="Browder">Browder DA, Erhard RE, Piva SR. [https://www.jospt.org/doi/pdf/10.2519/jospt.2004.34.11.701 Intermittent cervical traction and thoracic manipulation for management of mild cervical compressive myelopathy attributed to cervical herniated disc: a case series.] Journal of Orthopaedic & Sports Physical Therapy. 2004 Nov;34(11):701-12.</ref>. Cervical traction can be combined with other treatments like electrotherapy and exercises. ''Joghataei et al''. reported a significant increase in grip strength after 10 weeks of this combined treatment<ref>Joghataei MT, Arab AM, Khaksar H. [https://journals.sagepub.com/doi/abs/10.1191/0269215504cr828oa The effect of cervical traction combined with conventional therapy on grip strength on patients with cervical radiculopathy.] Clinical rehabilitation. 2004 Dec;18(8):879-87.</ref> | |||
==== Manual therapy techniques ==== | |||
[[Manual Techniques for the Cervicothoracic Spine|Manual therapy techniques]] is used to reduce the neck pain with natural apophyseal glides and sustained natural apophyseal glides for cervical extension and rotation<ref name="Almeida" /> Manipulation and mobilisations can be effective when they are combined with exercise therapy. When you use them without exercises, there is only poor evidence that it could be effective<ref>Binder, Allan I. "[https://pubmed.ncbi.nlm.nih.gov/17347239/ Cervical spondylosis and neck pain.]" ''BMJ: British Medical Journal'' 334.7592 (2007): 527-531. </ref><ref>Kay TM, Gross A, Goldsmith C, Santaguida PL, Hoving J, Brontfort G, et al, Cervical Overview Group. [https://pubmed.ncbi.nlm.nih.gov/16034925/ Exercises for mechanical neck disorders.] Cochrane Database Syst Rev 2005</ref> | |||
==== Exercises ==== | |||
The effects of exercise therapy specifically on cervical myelopathy have not been studied, but there is evidence for exercises for mechanical neck pain. For example: Mobility and proprioception exercises, [[Aerobic Exercise|aerobic exercise,]] [[stretching]], [[Strength Training|strengthening exercises]], active [[Range of Motion|range of motion exercises]], home exercise programmes<ref name=":0" /> <ref name="Almeida" /> | |||
''' | ====='''[[Deep Neck Flexor Stabilisation Protocol|Cervical stabilisation exercises]]'''===== | ||
When there is anteroposterior instability of the vertebral bodies of a degenerative nature, vertebral segment stabilisation of the cervical spine can be performed with a pressure biofeedback unit (PBU),<ref name="Almeida" />. | |||
===== Dynamic upper and lower limb exercises ===== | |||
Exercises like flexion and extension with the use of the PBU on the neck.<ref name="Almeida" /> | |||
==== Proprioceptive neuromuscular facilitation ==== | |||
PNF exercises for the upper and lower limbs.<ref name="Almeida" /> Look into this page [[Neurology Treatment Techniques]] for further details. | |||
==== Improve posture ==== | |||
Practice good [[posture]] — especially if you spend hours sitting at the computer or while talking on the phone or reading a book. Keep your head and neck upright<ref>El Camino Health, Cervical Myelopathy. Available from: https://www.elcaminohealth.org/services/spine-care/conditions-treatments/cervical-myelopathy | |||
Lasted accessed: 6th Sep 2021 | |||
</ref>. | |||
== | ==== Motor training programmes ==== | ||
These may improve arm and hand functioning at function and/or activity level in cervical spinal cord injured patients<ref>Spooren AI, Janssen-Potten YJ, Kerckhofs E, Seelen HA. [https://pubmed.ncbi.nlm.nih.gov/19543659/ Outcome of motor training programmes on arm and hand functioning in patients with cervical spinal cord injury according to different levels of the ICF: a systematic review.] Journal of rehabilitation medicine. 2009 Jun 5;41(7):497-505.</ref> | |||
[ | ==== Balance training ==== | ||
Standing on one leg with eyes open and evolving to eyes closed; standing on a stable platform and evolving to an unstable platform with a rocker board. <ref name="Almeida" /> For more details go into this page [[Balance Training|Balance training.]] | |||
[ | ==== Core stability exercises ==== | ||
In surgical cases, the physiotherapist still has an important role, both before and after the surgery. In the pre-operative phase, the physiotherapist needs to become thoroughly familiar with the patient's history and about their activities of daily living that they are aiming to return to. The physiotherapist will inform the patient about the treatment program and the expectations after the surgery. There are different tests to develop a thorough picture of the patient's baseline pre-operative status such as walking tolerance, [[Neck Pain and Disability Scale]], [[Neck Disability Index]] and lung function. ''Nomura et. al'' found that the maximum voluntary ventilation should significantly increase after surgery<ref>Nomura T, Tani T, Kitaoka K, Enoki H, Ishida K. [https://pubmed.ncbi.nlm.nih.gov/15241776/ A subclinical impairment of ventilatory function in cervical spondylotic myelopathy.] Archives of physical medicine and rehabilitation. 2004 Jul 1;85(7):1210-1.</ref> | |||
Exercises to improve mobility and proprioception are given to the patient. The patient starts with unencumbered stabilisation exercises and then progresses to more active mobilisation exercises. During the day the patient is encouraged to perform their usual [[Activities of Daily Living|ADLs.]] The intensity of the exercises is increased the following day and are progressed to include standing and walking exercises. Assuming typical progress with rehabilitation, the patient can go home after the ninth day. Physiotherapy continues in the home environment with active exercises and the ability of the patient to perform their normal ADLs is monitored, whilst increasing the intensity of the exercises as appropriate.<ref name="Almeida" /> | |||
If there are no completions with rehabilitation, there are no recommended limitations with normal ADLs for the patient. [[Posture]] education is an important aspect<ref>G. Aufdemkampe, J.B. Den Dekker, I. Van Ham, B.C.M. Smits-Engelsman, P. Vaes. Jaarboek fysiotherapie-kinesitherapie 2000. Bohn Stafleu Van Loghum, 275 p</ref><ref>Ogawa Y, Chiba K, Matsumoto M, Nakamura M, Takaishi H, Toyama Y. [https://pubmed.ncbi.nlm.nih.gov/17176010/ Postoperative factors affecting neurological recovery after surgery for cervical spondylotic myelopathy.] Journal of Neurosurgery: Spine. 2006 Dec 1;5(6):483-7. </ref> | |||
== Presentations == | == Presentations == | ||
<div class="coursebox"> | <div class="coursebox"> | ||
{| width="100%" cellspacing="4" cellpadding="4" border="0 | {| class="FCK__ShowTableBorders" width="100%" cellspacing="4" cellpadding="4" border="0" | ||
|- | |- | ||
| align="center" | <imagemap> | | align="center" | <imagemap> | ||
| Line 302: | Line 198: | ||
|} | |} | ||
</div> | </div> | ||
== Case Studies == | |||
* [http://www.spineuniverse.com/professional/case-studies/albert/progressive-cervical-myelopathy-57-year-old 57 Year-old male diagnosed with Cervical Myelopathy] | |||
* [http://www.jospt.org/doi/abs/10.2519/jospt.2008.0412#.UupuZWRDsao Cervical Spondylotic Myelopathy in a Patient Presenting With Low Back Pain] | |||
*[https://www.ncbi.nlm.nih.gov/pubmed/28859596 Cervical Myelopathy Presenting as Bilateral Upper Extremity Weakness] | |||
*[https://www.ncbi.nlm.nih.gov/pubmed/28666403 Cervical Myelopathy in a Patient Referred for Lower Extremity Symptoms] | |||
== Clinical Bottom Line == | |||
Cervical myelopathy is the result of spinal cord compression in the cervical spine and is a common disorder in persons older than 55 years of age. Cervical compression in myelopathy is predominantly due to pressure on the anterior spinal cord with ischaemia and to deformation of the cord by anterior herniated discs, spondylitic spurs or an ossified posterior longitudinal ligament. Early symptoms of this condition are ‘numb, clumsy, painful hands’ and disturbance of fine motor skill. The diagnosis of cervical myelopathy is primarily based on the clinical signs found on physical examination and is supported by imaging findings of cervical spondylosis with cord compression. Once the disorder is diagnosed, complete remission to normal function never occurs and spontaneous remission is uncommon. Exercises and techniques that may help relieve symptoms of cervical myelopathy include cervical traction, manual therapy techniques, proprioceptive neuromuscular facilitation, cervical stabilisation exercises and dynamic upper and lower limb exercises. | |||
== References == | |||
<references /> | |||
[[Category:Cervical Spine - Conditions]] | |||
[[Category:Neurological - Conditions]] | |||
[[Category:Vrije_Universiteit_Brussel_Project]] | |||
[[Category:Acute Care]] | |||
[[Category:Osteoarthritis]] | |||
[[Category:Conditions]] [[Category: | |||
Latest revision as of 11:40, 15 November 2023
Original Editors - Bridgit A Finley
Top Contributors - Laura Ritchie, Rachael Lowe, Bridgit A Finley, Stefanie Van De Vijver, Kim Jackson, Admin, Evan Thomas, Vidya Acharya, Loes Verspecht, Lise Buelens, Dale Boren, Manisha Shrestha, Bram Van Laer, Lucinda hampton, Simisola Ajeyalemi, Naomi O'Reilly, Habibu Salisu Badamasi, Ilke Joukes, Kai A. Sigel, Scott Cornish, WikiSysop, Karen Wilson, Timothy Assi, Jess Bell, Olajumoke Ogunleye and Aminat Abolade
Introduction[edit | edit source]
Cervical myelopathy is a condition involving compression of the spinal cord at the cervical level of the spinal column resulting in spasticity, hyperreflexia, pathologic reflexes, digit/hand clumsiness, and/or gait disturbance.
The spontaneous course of myelopathy is characterised either by long periods of stable disability followed by episodes of deterioration or a linear progressive course. The presentation of a cervical myelopathy varies in accordance with the severity of the spinal cord compression as well as its location.Without treatment, patients may progress toward significant paralysis and loss of function. .[1]
Any space-occupying lesion within the cervical spine with the potential to compress the spinal cord can cause cervical myelopathy.[2][3] Cervical myelopathy is predominantly due to pressure on the anterior spinal cord with ischemia as a result of deformation of the cord by anterior herniated discs, spondylitic bone spurs, an ossified posterior longitudinal ligament or spinal stenosis[4]
Clinically Relevant Anatomy[edit | edit source]
There are seven cervical vertebrae and eight cervical nerve roots.[3][5] The spinal cord is the extension of the central nervous system outside the cranium. It is encased by the vertebral column and begins at the foramen magnum.[6] The spinal cord is an extremely vital part of the central nervous system, and even a small injury can lead to severe disability.[7]
A complex system of ligaments serves to stabilise and protect the cervical spine. For example, ligamentum flavum extends from the anterior surface of the cephalic vertebra to the posterior surface of the caudal vertebra and connects to the ventral aspect of the facet joint capsules. A ligament that is often involved in this condition is the posterior longitudinal ligament. It is situated within the vertebral canal, originating from the body of the axis, where it is continuous with the tectorial membrane, and extends along the posterior surfaces of the bodies of the vertebrae until inserting into the sacrum.[7]
Epidemiology[edit | edit source]
- Cervical spondylotic myelopathy is the most common disorder of the spinal cord in persons older than 55 years of age.[5][8][9]
- Radiologic spondylotic changes increase with patient age - 90% of asymptomatic persons older than 70 years have some form of degenerative change in the cervical spine. Cervical spine myelopathy resulting from sagittal narrowing of the spinal canal and compression of the spinal cord is present in 90% of individuals by the seventh decade of life.[10]
- Both sexes are affected equally. Cervical spondylosis usually starts earlier in men (50 years) than in women (60 years).
- It causes hospitalisation at a rate of 4.04 per 100,000 person-years.[5][11]
Etiology[edit | edit source]
The causes of cervical myelopathy can be divided into different categories:
- Static factors: A narrowing of the spinal canal size commonly results from degenerative changes in the cervical spine anatomy (cervical spondylosis) such as disc degeneration, spondylosis, stenosis, osteophyte formation at the level of facet joints, segmental ossification of the posterior longitudinal ligament and yellow ligament hypertrophy, calcification or ossification. Patients with a congenitally narrow spinal canal (<13mm) have a higher risk for the development of symptomatic cervical myelopathy.[1][10][11][12]Chronic cervical degeneration is the most common cause of progressive spinal cord and nerve root compression. Spondylotic changes can result in stenosis of the spinal canal, lateral recess, and foramina. Spinal canal stenosis can lead to myelopathy, whereas the latter two can lead to radiculopathy.
- Dynamic factors: Due to mechanical abnormalities of the cervical spine or instability.[1]
- Vascular and cellular factors: Spinal cord ischemia affects oligodendrocytes, which results in demyelination exhibiting features of chronic degenerative disorders. Glutamatergic toxicity, cell injury and apoptosis may also occur.[1]
Cord compression is thought to be a combination of static compression and intermittent dynamic compression from cervical motion (flexion/extension).
Characteristics and Clinical Presentation[edit | edit source]
Cervical myelopathy can cause a variety of signs and symptoms.
- Cervical spondylotic myelopathy frequently involve compression of the lateral corticospinal tracts resulting in (voluntary skeletal muscle control), and the spinocerebellar tracts (proprioception). It causes classic signs: the wide-based spastic gait with clumsy upper extremity function.[13]
- Onset is insidious, typically in persons aged 50-60 years. Because of the lack of pain, there may be an interval of years between the onset of disease and first treatment. Progression takes place in a stepwise manner with functional decline.
- Early symptoms of this condition: numb, clumsy, painful hands, disturbance of fine motor skills.[1]
- Weakness and numbness occur in a non-specific/non-dermatomal pattern.
- Additional clinical findings may include neck pain and stiffness (decreased ROM, especially extension), shoulder and scapular pain, paresthaesia in one or both arms or hands, signs of radiculopathy, Babinski and Hoffmann's sign, ataxia and dexterity loss.[5][14][15]
- Typical neurological signs of long-tract involvement are exaggerated tendon reflexes (patellar and Achilles), presence of pathological reflexes (e.g. clonus, Babinski and Hoffman's sign), spastic quadriplegia, sensory loss and bladder-bowel disturbance.[12]Indicators of poor prognosis include bowel or bladder dysfunction, and general weakness.[13]
Once the disorder is diagnosed, complete remission to normality never occurs and spontaneous temporary remission is uncommon. In 75% of the patients, episodic worsening with neurological deterioration occurs, 20% have slow steady progression, and 5% experience rapid onset and progression.[1]
Common Symptoms
- Distal weakness
- Decreased ROM in the cervical spine, especially extension.
- Clumsy or weak hands with difficulty in fine motor movements.
- Pain in shoulder or arms
- Unsteady or clumsy gait
- Increased reflexes in the lower extremities and in the upper extremities below the level of the lesion.
- Numbness and paresthesia in one or both hands
- Radiculopathy signs
Diagnostic Procedures[edit | edit source]
A detailed and thorough neurological examination plus MRI is the current standard to diagnose the presence of cervical myelopathy.
Plain radiographs alone are of little use as an initial diagnostic procedure. A magnetic resonance image (MRI) is considered the best imaging method for confirming the presence of spinal canal stenosis, cord compression, or myelomalacia, elements germane to cervical spine myelopathy. MRI of the cervical spine can also rule out spinal cord tumours.
An MRI is most useful because it expresses the amount of compression placed on the spinal cord and demonstrates relatively high levels of sensitivity and specificity[5][14]. Anterior-posterior width reduction, cross-sectional evidence of cord compression, obliteration of the subarachnoid space and signal intensity changes to the cord found on MR imaging are considered the most appropriate parameters for confirmation of a spinal cord compression myelopathy[5]. More than half of patients with cervical spine myelopathy show intramedullary high signal intensity on T2-weighted imaging, mainly in the spinal gray matter[16]. Radiographic cervical spinal cord compression and hyperintense T2 intraparenchymal signal abnormalities (MRI) correlate well with the presence of myelopathic findings on physical examination.[14]
Clinical Examination[edit | edit source]
The diagnosis of CSM is primarily based on the clinical signs found on physical examination and is supported by imaging findings.[8] According to Cook et al,[18] selected combinations of the following clinical findings are effective in ruling out and ruling in cervical spine myelopathy. Combinations of three of five or four of five of these tests enable post-test probability of the condition to 94–99%:
- Gait deviation
- +ve Hoffmann’s test
- Inverted supinator sign
- +ve Babinski sign
- Age 45 years or older
Other clinical examination tests often used for myelopathy include:[5][8]
- Spurling’s test
- Distraction test
- +ve Clonus/Babinski/Hoffman's
- Hyper-reflexic biceps
- Hyper-reflexic quadriceps
- Hyper-reflexic Achilles
- Pain constancy
- Lhermitte’s sign
- Romberg test
Although these tests exhibit moderate to substantial reliability among skilled clinicians, they demonstrate low sensitivity and are not appropriate for ruling out myelopathy. One method used to improve the diagnostic accuracy of clinical testing is combining tests into clusters. These often overcome the inherent weakness of stand-alone tests.[5][18]
Outcome Measures[edit | edit source]
- Neck disability index
- Neck pain and disability scale
- Nurick-score [19]
- Japanese-orthopaedic-association-score (JOA-Score) [19] [20]
- Cooper-myelopathy-scale (CMS) [19]
- European-myelopathy-score (EMS)
Differential Diagnosis[edit | edit source]
- Adhesive Capsulitis
- Brown-Sequard Syndrome
- Carpal Tunnel Syndrome
- Central Cord Syndrome
- Cervical Disc Disease
- Cervical Myofascial Pain
- Cervical Sprain and Strain
- Chronic Pain Syndrome
- Diabetic Neuropathy
- Multiple Sclerosis
- Myofascial Pain
- Neoplastic Brachial Plexopathy
- Osteoporosis
- Spinal Cord Injury
- Radiation-Induced Brachial Plexopathy
- Rheumatoid Arthritis
- Traumatic Brachial Plexopathy
- Tumors
- Chiari malformation
- Guillain-Barre syndrome
- Syrinx
Management[edit | edit source]
There is no consensus about the treatment of mild and moderate forms of cervical myelopathy. Surgical treatment has no better results than conservative treatment over two years of follow-up.[9] Patients with cervical myelopathy that are treated with a conservative approach (anti-inflammatory medication and physical therapy) may have some short term benefit in relief of painful symptoms. Because the condition is degenerative and progressive, slow and continued progressive neurologic deterioration will occur.
Medical Management[edit | edit source]
People who have progressive neurologic changes (such as weakness, numbness or falling) with signs of severe spinal cord compression or spinal cord swelling are candidates for surgery. Patients with severe or disabling pain may also be helped with surgery.[21] When myelopathy is caused by factors of a progressive nature, such as spinal cord tumors, surgical treatment is likewise indicated[22][23].
People who experience better surgical outcomes often have these characteristics:
- The symptom of an electrical sensation that runs down the back and into the limbs
- Younger age
- Shorter duration of symptoms
- Single rather than multiple areas of involvement
- Larger areas available for the cord
The principal aim of surgery for cervical myelopathy is decompression of the spinal cord. Surgical techniques include multi-level discectomies or corpectomies with or without instrumented fusion, laminectomy with or without instrumented fusion or laminoplasty[1]. Surgical decompression is generally considered if the symptoms affect daily life, but early surgical intervention is thought to be more effective. Therefore, early detection may be the key to minimise postoperative degeneration[16].
Final outcomes from the surgery vary. Typically, one-third of patients improve, one-third stay the same, and one-third continue to worsen over time, with respect to their pre-surgical symptoms[9][21]
Physical Therapy Management[edit | edit source]
Patients can be treated conservatively. Kadaňka et al. found no difference in long term outcomes (2 years after the intervention) between patient who received conservative or surgical treatment. [9]Even after 10 years, there were no differences found between the surgery and conservative group[24] . Fouyas et al also confirmed these findings. [25] The only prognostic factor in which surgery can be generally recommended is with a circumferential spinal cord compression seen on an axial MRI.[26]
Rhee JM et al. describes myelopathy as a typically progressive disorder and that there is little of evidence that conservative treatment halts or reverses its progression. So they recommend routinely not prescribing non-operative treatment as the primary modality in patients with moderate to severe myelopathy.[27]
The goals of physiotherapy treatment are: [1]
- pain relief
- to improve function
- to prevent neurological deterioration
- to reverse or improve neurological deficits
Cervical myelopathy can be treated symptomatically. Possible therapies include:
Cervical traction and manipulation of the thoracic spine[edit | edit source]
This is useful for the reduction of pain scores and level of disability in patients with mild cervical myelopathy. Other signs and symptoms, such as weakness, headache, dizziness, and hypoesthesia, can also be positively affected[28]. Cervical traction can be combined with other treatments like electrotherapy and exercises. Joghataei et al. reported a significant increase in grip strength after 10 weeks of this combined treatment[29]
Manual therapy techniques[edit | edit source]
Manual therapy techniques is used to reduce the neck pain with natural apophyseal glides and sustained natural apophyseal glides for cervical extension and rotation[21] Manipulation and mobilisations can be effective when they are combined with exercise therapy. When you use them without exercises, there is only poor evidence that it could be effective[30][31]
Exercises[edit | edit source]
The effects of exercise therapy specifically on cervical myelopathy have not been studied, but there is evidence for exercises for mechanical neck pain. For example: Mobility and proprioception exercises, aerobic exercise, stretching, strengthening exercises, active range of motion exercises, home exercise programmes[25] [21]
Cervical stabilisation exercises[edit | edit source]
When there is anteroposterior instability of the vertebral bodies of a degenerative nature, vertebral segment stabilisation of the cervical spine can be performed with a pressure biofeedback unit (PBU),[21].
Dynamic upper and lower limb exercises[edit | edit source]
Exercises like flexion and extension with the use of the PBU on the neck.[21]
Proprioceptive neuromuscular facilitation[edit | edit source]
PNF exercises for the upper and lower limbs.[21] Look into this page Neurology Treatment Techniques for further details.
Improve posture[edit | edit source]
Practice good posture — especially if you spend hours sitting at the computer or while talking on the phone or reading a book. Keep your head and neck upright[32].
Motor training programmes[edit | edit source]
These may improve arm and hand functioning at function and/or activity level in cervical spinal cord injured patients[33]
Balance training[edit | edit source]
Standing on one leg with eyes open and evolving to eyes closed; standing on a stable platform and evolving to an unstable platform with a rocker board. [21] For more details go into this page Balance training.
Core stability exercises [edit | edit source]
In surgical cases, the physiotherapist still has an important role, both before and after the surgery. In the pre-operative phase, the physiotherapist needs to become thoroughly familiar with the patient's history and about their activities of daily living that they are aiming to return to. The physiotherapist will inform the patient about the treatment program and the expectations after the surgery. There are different tests to develop a thorough picture of the patient's baseline pre-operative status such as walking tolerance, Neck Pain and Disability Scale, Neck Disability Index and lung function. Nomura et. al found that the maximum voluntary ventilation should significantly increase after surgery[34]
Exercises to improve mobility and proprioception are given to the patient. The patient starts with unencumbered stabilisation exercises and then progresses to more active mobilisation exercises. During the day the patient is encouraged to perform their usual ADLs. The intensity of the exercises is increased the following day and are progressed to include standing and walking exercises. Assuming typical progress with rehabilitation, the patient can go home after the ninth day. Physiotherapy continues in the home environment with active exercises and the ability of the patient to perform their normal ADLs is monitored, whilst increasing the intensity of the exercises as appropriate.[21]
If there are no completions with rehabilitation, there are no recommended limitations with normal ADLs for the patient. Posture education is an important aspect[35][36]
Presentations[edit | edit source]
 |
Cervical Arthritis, Cervical Spondylotic Myelopathy
This presentation was created by Pablo Pazmino MD. Cervical Arthritis, Cervical Spondylotic Myelopathy/ View the presentation |
Case Studies[edit | edit source]
- 57 Year-old male diagnosed with Cervical Myelopathy
- Cervical Spondylotic Myelopathy in a Patient Presenting With Low Back Pain
- Cervical Myelopathy Presenting as Bilateral Upper Extremity Weakness
- Cervical Myelopathy in a Patient Referred for Lower Extremity Symptoms
Clinical Bottom Line[edit | edit source]
Cervical myelopathy is the result of spinal cord compression in the cervical spine and is a common disorder in persons older than 55 years of age. Cervical compression in myelopathy is predominantly due to pressure on the anterior spinal cord with ischaemia and to deformation of the cord by anterior herniated discs, spondylitic spurs or an ossified posterior longitudinal ligament. Early symptoms of this condition are ‘numb, clumsy, painful hands’ and disturbance of fine motor skill. The diagnosis of cervical myelopathy is primarily based on the clinical signs found on physical examination and is supported by imaging findings of cervical spondylosis with cord compression. Once the disorder is diagnosed, complete remission to normal function never occurs and spontaneous remission is uncommon. Exercises and techniques that may help relieve symptoms of cervical myelopathy include cervical traction, manual therapy techniques, proprioceptive neuromuscular facilitation, cervical stabilisation exercises and dynamic upper and lower limb exercises.
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 1.7 Boos N and Aebi M (Eds). Spinal disorders: Fundamentals of Diagnosis and Treatment. Springer-Verlag Berlin Heidelberg. 2008.
- ↑ Richard K. Root Clinical Infectious Diseases: A Practical Approach, 1999
- ↑ 3.0 3.1 Kong LD, Meng LC, Wang LF, Shen Y, Wang P and Shang ZK. Evaluation of conservative treatment and timing of surgical intervention for mild forms of cervical spondylotic myelopathy. Exp Ther Med. 2013 Sep;6(3):852-856.
- ↑ Dai L, Ni B, Yuan W and Jia L. Radiculopathy after laminectomy for cervical compression myelopathy. J Bone Joint Surg Br. 1998 Sep;80(5):846-9.
- ↑ 5.0 5.1 5.2 5.3 5.4 5.5 5.6 5.7 Cook C, Brown C, Isaacs R, Roman M, Davis S, Richardson W. Clustered clinical findings for diagnosis of cervical spine myelopathy. Journal of Manual & Manipulative Therapy. 2010 Dec 1;18(4):175-80.
- ↑ Cramer GD and Darby SA. Basic and Clinical Anatomy of the Spine, Spinal Cord, and ANS. 2nd Edition. Elsevier 2008.
- ↑ 7.0 7.1 Selzer ME and Dobkin BH. Spinal Cord Injury (American Academy of Neurology Quality of Life Series). Demos Medical Publishing (New York). 2008
- ↑ 8.0 8.1 8.2 Amenta PS, Ghobrial GM, Krespan K, Nguyen P, Ali M, Harrop JS. Cervical spondylotic myelopathy in the young adult: a review of the literature and clinical diagnostic criteria in an uncommon demographic. Clinical neurology and neurosurgery. 2014 May 1;120:68-72.
- ↑ 9.0 9.1 9.2 9.3 Kadaňka Z, Bednařík J, Voháňka S, Vlach O, Stejskal L, Chaloupka R, Filipovičová D, Šurelová D, Adamová B, Novotný O, Němec M. Conservative treatment versus surgery in spondylotic cervical myelopathy: a prospective randomised study. European Spine Journal. 2000 Dec;9(6):538-44.
- ↑ 10.0 10.1 Cook C, Roman M, Stewart KM, Leithe LG, Isaacs R. Reliability and diagnostic accuracy of clinical special tests for myelopathy in patients seen for cervical dysfunction. journal of orthopaedic & sports physical therapy. 2009 Mar;39(3):172-8.
- ↑ 11.0 11.1 Koakutsu T, Nakajo J, Morozumi N, Hoshikawa T, Ogawa S, Ishii Y. Cervical myelopathy due to degenerative spondylolisthesis. Upsala journal of medical sciences. 2011 May 1;116(2):129-32.
- ↑ 12.0 12.1 Yonenobu K. Cervical radiculopathy and myelopathy: when and what can surgery contribute to treatment?. European Spine Journal. 2000 Feb;9(1):1-7.
- ↑ 13.0 13.1 Donnally III CJ, Hanna A, Odom CK. Cervical myelopathy. StatPearls [Internet]. 2021 Mar 6.
- ↑ 14.0 14.1 14.2 Harrop JS, Naroji S, Maltenfort M, Anderson DG, Albert T, Ratliff JK, Ponnappan RK, Rihn JA, Smith HE, Hilibrand A, Sharan AD. Cervical myelopathy: a clinical and radiographic evaluation and correlation to cervical spondylotic myelopathy. Spine. 2010 Mar 15;35(6):620-4.
- ↑ Park SJ, Kim SB, Kim MK, Lee SH, Oh IH. Clinical features and surgical results of cervical myelopathy caused by soft disc herniation. Korean Journal of Spine. 2013 Sep;10(3):138.
- ↑ 16.0 16.1 Sato T, Horikoshi T, Watanabe A, Uchida M, Ishigame K, Araki T, Kinouchi H. Evaluation of cervical myelopathy using apparent diffusion coefficient measured by diffusion-weighted imaging. American journal of neuroradiology. 2012 Feb 1;33(2):388-92.0
- ↑ Stanford Imaging Patients with Myelopathy. Available from https://www.youtube.com/watch?time_continue=5&v=mJVEtq5GsJk
- ↑ 18.0 18.1 Cook C, Brown C, Isaacs R, Roman M, Davis S, Richardson W. Clustered clinical findings for diagnosis of cervical spine myelopathy. Journal of Manual & Manipulative Therapy. 2010 Dec 1;18(4):175-80.
- ↑ 19.0 19.1 19.2 Vitzthum HE, Dalitz K. Analysis of five specific scores for cervical spondylogenic myelopathy. European Spine Journal. 2007 Dec;16(12):2096-103.
- ↑ Tanaka N, Konno SI, Takeshita K, Fukui M, Takahashi K, Chiba K, Miyamoto M, Matsumoto M, Kasai Y, Kanamori M, Matsunaga S. An outcome measure for patients with cervical myelopathy: the Japanese Orthopaedic Association Cervical Myelopathy Evaluation Questionnaire (JOACMEQ): an average score of healthy volunteers. Journal of Orthopaedic Science. 2014 Jan 1;19(1):33-48.
- ↑ 21.0 21.1 21.2 21.3 21.4 21.5 21.6 21.7 21.8 Almeida GP, Carneiro KK, Marques AP. Manual therapy and therapeutic exercise in patient with symptomatic cervical spondylotic myelopathy: A case report. Journal of bodywork and movement therapies. 2013 Oct 1;17(4):504-9.
- ↑ Leonardi M, Boos N. Degenerative disorders of the cervical spine. InSpinal Disorders 2008 (pp. 429-479). Springer, Berlin, Heidelberg.
- ↑ Law Jr MD, Bernhardt M, White 3rd AA. Cervical spondylotic myelopathy: a review of surgical indications and decision making. The Yale journal of biology and medicine. 1993 May;66(3):165.
- ↑ Kadaňka Z, Bednařík J, Novotný O, Urbánek I, Dušek L. Cervical spondylotic myelopathy: conservative versus surgical treatment after 10 years. European Spine Journal. 2011 Sep;20(9):1533-8.
- ↑ 25.0 25.1 Fouyas IP, Statham PF, Sandercock PA. Cochrane review on the role of surgery in cervical spondylotic radiculomyelopathy. Spine. 2002 Apr 1;27(7):736-47.
- ↑ Shimomura T, Sumi M, Nishida K, Maeno K, Tadokoro K, Miyamoto H, Kurosaka M, Doita M. Prognostic factors for deterioration of patients with cervical spondylotic myelopathy after nonsurgical treatment. Spine. 2007 Oct 15;32(22):2474-9.
- ↑ Rhee JM, Shamji MF, Erwin WM, Bransford RJ, Yoon ST, Smith JS, Kim HJ, Ely CG, Dettori JR, Patel AA, Kalsi-Ryan S. Nonoperative management of cervical myelopathy: a systematic review. Spine. 2013 Oct 15;38(22S):S55-67.
- ↑ Browder DA, Erhard RE, Piva SR. Intermittent cervical traction and thoracic manipulation for management of mild cervical compressive myelopathy attributed to cervical herniated disc: a case series. Journal of Orthopaedic & Sports Physical Therapy. 2004 Nov;34(11):701-12.
- ↑ Joghataei MT, Arab AM, Khaksar H. The effect of cervical traction combined with conventional therapy on grip strength on patients with cervical radiculopathy. Clinical rehabilitation. 2004 Dec;18(8):879-87.
- ↑ Binder, Allan I. "Cervical spondylosis and neck pain." BMJ: British Medical Journal 334.7592 (2007): 527-531.
- ↑ Kay TM, Gross A, Goldsmith C, Santaguida PL, Hoving J, Brontfort G, et al, Cervical Overview Group. Exercises for mechanical neck disorders. Cochrane Database Syst Rev 2005
- ↑ El Camino Health, Cervical Myelopathy. Available from: https://www.elcaminohealth.org/services/spine-care/conditions-treatments/cervical-myelopathy Lasted accessed: 6th Sep 2021
- ↑ Spooren AI, Janssen-Potten YJ, Kerckhofs E, Seelen HA. Outcome of motor training programmes on arm and hand functioning in patients with cervical spinal cord injury according to different levels of the ICF: a systematic review. Journal of rehabilitation medicine. 2009 Jun 5;41(7):497-505.
- ↑ Nomura T, Tani T, Kitaoka K, Enoki H, Ishida K. A subclinical impairment of ventilatory function in cervical spondylotic myelopathy. Archives of physical medicine and rehabilitation. 2004 Jul 1;85(7):1210-1.
- ↑ G. Aufdemkampe, J.B. Den Dekker, I. Van Ham, B.C.M. Smits-Engelsman, P. Vaes. Jaarboek fysiotherapie-kinesitherapie 2000. Bohn Stafleu Van Loghum, 275 p
- ↑ Ogawa Y, Chiba K, Matsumoto M, Nakamura M, Takaishi H, Toyama Y. Postoperative factors affecting neurological recovery after surgery for cervical spondylotic myelopathy. Journal of Neurosurgery: Spine. 2006 Dec 1;5(6):483-7.