The Calgary-Cambridge Guide to the Medical Interview - Gathering Information on the Biomedical History: Difference between revisions
No edit summary |
No edit summary |
||
| Line 3: | Line 3: | ||
</div> | </div> | ||
The history-taking or information-gathering session form an essential skill of the healthcare practice that assists in the diagnosis of the patient's physical problems. The success of such a process relies on many factors including; preparation, planning, and communication between the healthcare professional and the patient<ref>Gask L, Usherwood T. The consultation. Bmj. 2002 Jun 29;324(7353):1567-9.</ref>. During the consultation, the physiotherapist or other healthcare practitioner aims to gather the information they need to interpret and understand the nature of the symptoms and how patients are coping with them<ref name=":0">Kaufman G. Patient assessment: effective consultation and history taking. Nursing Standard. 2008 Oct 1;23(4).</ref>. | |||
== Hypothesis generation and clinical reasoning == | == Hypothesis generation and clinical reasoning == | ||
Revision as of 21:48, 9 November 2020
The history-taking or information-gathering session form an essential skill of the healthcare practice that assists in the diagnosis of the patient's physical problems. The success of such a process relies on many factors including; preparation, planning, and communication between the healthcare professional and the patient[1]. During the consultation, the physiotherapist or other healthcare practitioner aims to gather the information they need to interpret and understand the nature of the symptoms and how patients are coping with them[2].
Hypothesis generation and clinical reasoning[edit | edit source]
A sound hypothesis depends on good quality clinical reasoning, using as much as possible clinically relevant information gained during the patient interview. Clinical reasoning is defined as a process of analysing acquired clinical data in combination with patient preferences, professional judgement and scientific knowledge, with the goal of structuring meaning, developing objectives and implementing health management strategies in the management of a patient[3]. Physiotherapists often apply clinical reasoning to arrive at a working hypothesis by utilising either a hypothetico-deductive model, or pattern recognition, or a combination of the two. In a hypothetico-deductive model, hypotheses are generated from all observations, after which clinical data gained is tested to arrive at the most likely hypothesis. Pattern recognition, generally used by more experienced therapists, involve the formation of a hypothesis from typical symptom and disease presentation noted, and subsequent data exploration to confirm or negate the hypotheses[4].
The use of a function and disability model can help the therapist to better understand the context of the presenting patient during the process of clinical reasoning and hypothesis generation. It aids to organize information in a practical and logical manner, while also integrating environmental, social and psychological factors in the understanding of the person and condition[3]. Furthermore, the use of a function and disability model as outcome measure allows to standardise patient impairment and provides a concrete, comparable benchmark by which to measure effect of management. The International Classification of Function, Disability and Health (ICF) will be discussed as a function and disability model underpinning clinical reasoning and hypothesis generation.
Information gathering in the context of the International Classification of Function, Disability and Health (ICF)[edit | edit source]
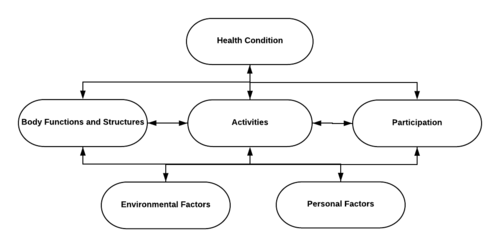
The ICF is a classification system which describes the different components of functioning of a person with any health condition. It was approved by the World Health Organisation (WHO) in 2001 as universally accepted conceptual model and taxonomy of human functioning. The ICF describes human functioning as an interaction between body functions and structures, activities, and participation, together with the effect of psychological and environmental influences (Figure 1). The model is built on biopsychosocial principles which regards the patient as a holistic, psychological being within a specific environment. Disability is described according to impairment of body functions/structure, limitations in activities and restrictions in participation[5].
The term body functioning and structures refers to physiological processes and anatomic structures, and any abnormality to these is referred to as an impairment. Examples of impairments include arterial fibrillation leading to physical weakness and fatigue, or ulnar nerve entrapment leading to forearm pain. Activity refers to execution of tasks or actions and represents the individual’s perception of function. Examples of activities include walking/running, grasping, kicking or carrying. Inability to perform normal activities is referred to as limitations. Participation refers to life situations in which an individual is actively involved. Inability to engage in normal participation is called participation restrictions. Examples are playing soccer, preparing food, looking after children or visiting the shops[5]. Environmental and personal factors are collectively known as contextual factors, and refer to the influence of surroundings, psychology and experience of illness on the patient’s health[6].
From a biopsychosocial point of view, the ICF is a model for standardisation of function and health which allows for comparison across the spectrum of disability. The inclusion of contextual factors provides a patient-specific representation of function which illustrates why different individuals may be differently affected by a seemingly similar pathology. For example, one patient may walk on a fractured metatarsal for days before having it diagnosed, where another patient with similar biomedical factors and who sustained a similar injury may be in much more distress soon after onset of injury. Differences in contextual factors may also influence recovery and behaviour of the individual[6].
Although physiotherapists often successfully treat patients who reach full recovery, we should remember that many conditions are chronic and progressive in nature and that some patients will never be completely asymptomatic (Parkinson’s disease or cystic fibrosis, for example). For this reason, the focus should be on rehabilitation as a process to help patients reach their optimal physical, psychological, social, occupational and educational potential within the anatomical and physiological capacity available[7]. The ICF aids rehabilitation professionals to gauge the functional capacity of a patient, analyse the source of restrictions and limitations and compile a realistic management plan accordingly.
The consideration of the ICF in the medical interview helps rehabilitation professionals to understand the impact of a health condition on the patient’s functionality and well-being. Emphasis is placed on the functional limitation due to presenting symptoms, instead of only focusing on the specific presentation and behaviour of symptoms. Proper comprehension of the bigger context of ill-health will also assist the therapist in realistic goal setting and provide better understanding of the patient as a person, as well as his/her experience of the condition and the potential role this experience can play in symptom presentation and/or recovery. Knowledge of a patient’s functional impairment will furthermore assist the therapist to select assessment techniques based on symptom-eliciting functional movements. For this reason, it is strongly recommended that the process of information gathering should be based on the patient’s current functional capacity and the potential effect of the presenting condition/symptoms.
Gaining biomedical information[edit | edit source]
The specific investigation of biomedical history is highly dependent upon the subspecialty of medicine/allied health involved[8]. A women’s health physiotherapist will have a different investigation approach and special questions to a neuropediatric physiotherapist, for example. The basic principles of most biomedical information to be gathered remains the same across the spectrum, however, and for the purpose of this document, a number of these will be discussed in more detail. These factors include the behaviour of symptoms, red flags, medical history, and a review of relevant systems[2].
Symptom behaviour[edit | edit source]
The mnemonic PQRST can be used to remember five aspects of symptom behaviour to be investigated: Palliation/provocation, quality, region/radiation, severity and timing[2]. Very often, basic information on symptom behaviour is already provided in the initiation of the session and should now be elaborated upon and investigated deeper if necessary.
Palliation/provocation refers to any factors that may aggravate or improve symptoms. As discussed, an investigation into the patient’s functional limitations due to the presenting symptoms, specifically relating to participation restrictions or activity limitations, usually provide valuable information. Ask about specific movements or positions that may aggravate or alleviate symptoms. Patients may also relate their emotional state to their physical symptoms: allostatic overload (cumulative effect of frequent stressful situations in everyday life) can have a significant adverse effect on physical health[9][10].
Quality of symptoms, also called nature of symptoms, involves the patient perception of the presenting symptoms[2]. The therapist should first ask the patient do describe the symptoms ( for example: “what type of a pain is it?” or “can you try to describe the weird sensation in your fingers in more detail?”). The patient should be allowed enough time to think and respond. If the patient seems uncertain, the physiotherapist can prompt for the use of adjectives to try and describe the symptoms, or perhaps offer some options (“Is it a sharp pain, or burning? Or achy, rather?” or “Would you say your cough is dry or wet? Maybe wheezy, or barking?”) Quality of symptoms may provide clues to the possible aetiology of the presenting condition.
Region/Radiation refers to the physical area where symptoms are experienced[2]. The use of a body chart is recommended to indicate the region of symptom presentation. A body chart aids to conceptualise symptoms and assists the therapist to recognise potential patterns that may be specific to certain conditions. It is suggested to ask the patient to indicate the area of symptom experience on his/her body by showing with the hand, after which the physiotherapist plots the area on the body chart, and then confirming with the patient whether the area indicated is correct. All areas where symptoms are experienced should be filled in and the patient should confirm whether any relationship exists between the different areas in terms of any symptom behaviour.
Severity reflects the intensity of symptoms[2]. Severity should be as concrete as possible, using a numeric value or a standardized score. A well-known example is that of the numeric pain scale where a patient indicates the severity of pain on a scale from 0 to 10 (where 0 is no pain and 10 is excruciating and decapacitating). Depending on the presenting condition, different subjective outcome measures can be used to measure severity: the severity of upper limb dysfunction can for instance be determined by the Disability of Arm, Shoulder and Hand (DASH) questionnaire, or the Dizziness Handicap Inventory (DHI) can be used to express severity of experienced dizziness. Patients should be informed that severity is specific and standardised to each patient and is often used as a comparable sign to indicate potential improvement or regression of the condition. In this way, individual variables such as pain threshold is accommodated.
Timing includes three concepts: Firstly, a timeline from onset to current presentation should be established, including further exploration of mechanisms, and any regression/progression of the condition since onset. Secondly, enquire about any 24-hour pattern noted (for example, worse at night, or stiffness and pain first thing in the morning). Thirdly, investigate the frequency of symptoms (i.e. intermittent or constant awareness) and whether this has changed since onset of symptoms[2]. Information on timing assists the therapist to assess aetiology, chronicity and/or phase of recovery.
Red flags[edit | edit source]
Red flags are any signs or symptoms that may indicate a possible serious underlying condition, that warrants further medical assessment and/or intervention[11] before continuing with therapeutic management. Although the concept of red flags covers all areas of medicine, specific subspecialties need to assess specific red flags relevant to their field. For example, musculoskeletal physiotherapists treating a lumber condition should clear any signs of cauda equina syndrome and spinal stenosis, and for upper cervical pain/headache and vertigo, vertebrobasilar insufficiency and cervical spine instability should be excluded.
When screening for red flags, is it suggested for the therapist to inform the patient that the relevant questions are only asked to ensure that no potential underlying pathologies are missed. Also confirm that the prevalence of red flags is mostly low in the general population. This will put potentially catastrophizing patients at ease and prevent unnecessary anxiety regarding questions that may seem irrelevant to the condition. When red flags are indeed identified, share your findings with the patient in a logical manner using easily understandable language, and explain that referral to a specialist is necessary to exclude underlying pathology before continuing with therapy.
Medical history[edit | edit source]
Current medical history[edit | edit source]
The prevalence of chronic conditions and chronic medication use should be assessed. Also check the duration of use of chronic medication and consider any co-incidence in symptom timing and medication use, which may indicate that symptoms can possibly be linked to medication[2]. Remain objective, sensitive, and respectful at all times – patients often feel ashamed or stigmatised for certain conditions or medication uses. Also, check for habitual substance consumption, such as the use of tobacco, alcohol or marijuana or other narcotics. Create a safe, non-judgemental space when assessing these, since patients are often reluctant to share this type of information with health-care professionals. When the patient seems reluctant, explain that prolonged substance use can influence the healing process, which is why it needs to be taken into account. Although it is our task as healthcare professionals to educate patients regarding the use of adverse substances, this should rather be incorporated into the management plan than addressing the issue during the interview. Also ask about regular exercise and note the activity and frequency. Furthermore, enquire about diet, sleep habits, as well as any other preventative medicine used[2].
Previous medical history[edit | edit source]
Enquire about any physical trauma, hospitalisation or injuries throughout the patient’s lifetime, even though the patient may not consider such history as relevant to the presenting condition. Ask about any previous treatment by another medical or rehabilitation professional, and what the patient was treated for[2].
Family history[edit | edit source]
Like with red flags, explain to the patient that an investigation into family history is done routinely and to exclude the possibility of any link to genetic or hereditary diseases. Conditions to look out for include cardiovascular disease, diabetes, chronic respiratory conditions, cancer, and bone diseases. Literature suggests that clinicians should consider family history of the previous two generations[2]. When hereditary diseases are noted, consider providing some counselling in terms of preventative screening to be performed at a relevant health care practitioner.
Review of the systems[edit | edit source]
The idea of performing a complete review of all systems together with your primary assessment is noble and will certainly provide the clinician with a very comprehensive patient image, ensuring nothing has been missed. However, from a practical point of view it would not make sense to do a head-to-toe assessment for every patient. The clinician should apply good judgement and clinical reasoning to decide which system review to include in the assessment. For example, for a patient with neck pain, an investigation into possible eye problems will be sensible, but assessing for sexual health disorders will be inappropriate. Table 1 provides a summary of additional somatic systems to consider in assessment. It is important to explain to the patients why other systems than that of the presenting pathology are investigated to prevent unnecessary anxiety.
| SYSTEM | FACTORS TO CONSIDER |
|---|---|
| Head | Dizziness, headaches, faintness, recent head injury |
| Eyes | Any changes in vision, regular optometric tests |
| Respiratory | Breathing problems, coughing, wheezing, sputum production, allergic rhinitis, chronic sinusitis, ear ache hearing loss |
| Cardiac | Anemia, hypertension, palpitations |
| Gastrointestinal | Heartburn, irritable bowel syndrome, nausea, changes in regular toileting routine |
| Urogenital/gynaecological | Pain with urination, menstruation-related symptoms, changes in regular toileting routine |
| Muskuloskeletal | Stiffness, cramps, weakness, swelling |
| Neurological | Numbness, tingling, tremors, weakness, coordination, balance |
Conclusion[edit | edit source]
The gaining of biomedical information is regarded as the core of the medical assessment process by many. Although information gathered is imperative for the formation of a sound hypothesis, the clinical significance of psychosocial factors should not be overlooked. It is recommended to follow a function-based approach in the investigation of biomedical information in order to ensure patient centred care. Throughout the gaining of information, dynamic clinical reasoning is necessary to develop relevant hypotheses, select the appropriate assessment techniques, formulate a sound diagnosis and ensure a comprehensive and applicable management plan.
References[edit | edit source]
- ↑ Gask L, Usherwood T. The consultation. Bmj. 2002 Jun 29;324(7353):1567-9.
- ↑ 2.00 2.01 2.02 2.03 2.04 2.05 2.06 2.07 2.08 2.09 2.10 Kaufman G. Patient assessment: effective consultation and history taking. Nursing Standard. 2008 Oct 1;23(4).
- ↑ 3.0 3.1 Jones, M., Edwards, I., Gifford, L., 2002. Conceptual models for implementing biopsychosocial theory in clinical practice. Man. Ther. 7, 2–9. https://doi.org/10.1054/math.2001.0426
- ↑ Jones, M.A., 1992. Clinical Reasoning in Manual Therapy. Phys. Ther. 72, 875–884. https://doi.org/10.1093/ptj/72.12.875
- ↑ 5.0 5.1 Stucki, G., Cieza, A., Melvin, J., 2007. The International Classification of Functioning, Disability and Health (ICF): a unifying model for the conceptual description of the rehabilitation strategy. J. Rehabil. Med. 39, 279–285. https://doi.org/10.2340/16501977-0041
- ↑ 6.0 6.1 Johnston, M., Dixon, D., 2014. Developing an integrated biomedical and behavioural theory of functioning and disability: adding models of behaviour to the ICF framework. Health Psychol. Rev. 8, 381–403. https://doi.org/10.1080/17437199.2013.855592
- ↑ Heerkens, Y., Hendriks, E., Oostendorp, R., 2006. Assessment instruments and the ICF in rehabilitation and physiotherapy. Med. Rehabil. 10, 1–14.
- ↑ Johnson, P., Rain, S., Meadows, L., Lynch-Ellerington, M., 2009. Assessment and Clinical Reasoning in the Bobath Concept, in: Bobath Concept: Theory and Clinical Practice in Neurological Rehabilitation. Blackwill Publishing Ltd, pp. 43–63.
- ↑ Butler, R.K., Finn, D.P., 2009. Stress-induced analgesia. Prog. Neurobiol. 88, 184–202. https://doi.org/10.1016/j.pneurobio.2009.04.003
- ↑ Fava, G.A., McEwen, B.S., Guidi, J., Gostoli, S., Offidani, E., Sonino, N., 2019. Clinical characterization of allostatic overload. Psychoneuroendocrinology 108, 94–101. https://doi.org/10.1016/j.psyneuen.2019.05.028
- ↑ Briggs, A.M., Fary, R.E., Slater, H., Ranelli, S., Chan, M., 2013. Physiotherapy co-management of rheumatoid arthritis: Identification of red flags, significance to clinical practice and management pathways. Man. Ther. 18, 583–587. https://doi.org/10.1016/j.math.2013.01.006