Supraspinatus Tendinopathy
Original Editors - Aiko Deckers
Top Contributors - Aiko Deckers, Kim Jackson, Naaike Verhaeghe, Admin, Fasuba Ayobami, Wendy Walker, Ajay Upadhyay, Ina De Maeyer, Shaimaa Eldib, Rachael Lowe, Joao Costa, Tony Lowe, Wanda van Niekerk, Abbey Wright, Naomi O'Reilly, Mathieu Cooreman, Ammar Suhail, Sweta Christian, WikiSysop and Evan Thomas
Search strategy[edit | edit source]
Databases used: Pubmed
Keywords used: supraspinatus tendinopathy, supraspinatus tendonitis, supraspinatus tendinitis, shoulder pain, epidemiology, impingement, upper arm sports
Definition/Description
[edit | edit source]
For information about tendinopathy, see http://www.physio-pedia.com/Tendinopathy
Supraspinatus tendinopathy is a common and disabling condition that becomes more prevalent after middle age (6,7) and is a common cause of pain in the shoulder (26, 27). A predisposing factor is resistive overuse.[1]
The supraspinatus tendon of the rotator cuff is involved and affected tendons[2][3] (28) of the musculoskeletal system and becomes degenerated, most often as a result of repetitive stresses and overloading during sports or occupational activities (29).
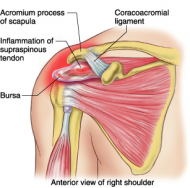
The tendon of the supraspinatus commonly impinges under the acromion as it passes between the acromion and the humeral head. This mechanism is multifactorial (see below).
Epidemiology/Etiology[edit | edit source]
The causes of supraspinatus tendonitis can be primary impingement, which is a result of increased subacromial loading, and secondary impingement, which is a result of rotator cuff overload and muscle imbalanceCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title.
The mean age of onset of this complication is in the sixth decade (age 50 to 59), and it is more frequent in diabetic patientsCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title. It is also a common cause of shoulder pain in athletes whose sports involve throwing and overhead motionsCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title.
Characteristics/Clinical Presentation[edit | edit source]
Patients present with progressive subdeltoid aching that is aggravated by abduction, elevation, or sustained overhead activity. The pain may radiate to the lateral upper arm. Other complaints include nocturnal pain and difficulty with dressing. The patient may have a history of sports or occupational repetitive trauma, however, this is not universalCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive titleCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title.
Supraspinatus tendinitis is usually consistent with anterior instability causing posterior tightness.The problems that patient with Supraspinatus Tendinitis complain off, are pain, inflammation, decreased ROM, strength, and functional activityCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title.
Clinical Relevant Anatomy[edit | edit source]
The supraspinatus muscle is of the greatest practical importance in the rotator cuff (30), derives its innervation from the suprascapular nerve (31) and stabilises the schoulder, exorotates and helps abduct (lift up sideways) the arm, by initiating the abduction of the humerus on the scapula (30). For more information about the function of the musculus supraspinatis in the rotator cuff, see http://www.physio-pedia.com/Rotator_Cuff
Any friction between the tendon and the acromion is normally reduced by the subacromial bursa.
For origo en insertion of the musculus supraspinatus, see also http://www.physio-pedia.com/Rotator_Cuff
The anterior margin of the supraspinatus is defined by the posterior edge of the rotator interval that separates the supraspinatus from the rolled superior border of the subscapularis. The posterior margin of the supraspinatus is marked by the extension of the raphe between supraspinatus and infraspinatus around the scapular spine. The anterior portion of the supraspinatus is composed of a long and thick tendinous component whereas the posterior portion has been shown to be short and thin (31).
An anatomic dissection study of the supraspinatus footprint found that the mean anterior to posterior dimension of the supraspinatus tendon was 25 mm, with a mean medial to lateral thickness of the footprint of 12 mm - the mean distance from the cartilage to the supraspinatus footprint was 1.5 mm at midtendon (32).
The supraspinatus and infraspinatus tendons fuse 1.5 cm proximal to their insertions (33). Collagen is the major matrix protein of supraspinatus tendons, consisting of > 95% type I collagen, with
lesser amounts of other collagens including collagen type III (35, 36).
The anatomy of the supraspinatus’s insertion is of key relevance in terms of its extracellular matrix composition and has been categorised into four transition zones (34). The first zone is proper tendon, made up of largely type I collagen and small amounts of decorin. The second zone is fibrocartilage and consists of largely types II and III collagen, with small amounts of types I, IX and X collagen. The third zone is mineralised fibrocartilage and consists of type II collagen, with significant amounts of type X collagen and aggrecan. The fourth zone is bone and is largely type I collagen with a high mineral content. This effective bone-tendon attachment is achieved through a functional grading in mineral content and collagen fibre orientation. The supraspinatus enthesis is a highly specialised in homogeneous structure that is subjected to both tensile and compressive forces (33).
Epidemiology/Etiology[edit | edit source]
The mean age of onset of this complication is in the sixth decade (age 50 to 59), and it is more frequent in diabetic patients[1]. It is also a common cause of shoulder pain in athletes whose sports involve throwing and overhead motions[2].
The causes of supraspinatus tendinitis can be primary impingement, which is a result of increased subacromial loading, and secondary impingement, which is a result of rotator cuff overload and muscle imbalance[4]. Figure 1 gives a view on the different extrinsic and intrinsic factors
Characteristics/Clinical presentation[edit | edit source]
Patients present with progressive subdeltoid aching that is aggravated by abduction, elevation, or sustained overhead activity. They feel also tenderness and a burning sensation in their shoulder (29). The pain may radiate to the lateral upper arm or may be located in the top and front of the shoulder. It typically becomes worse with overhead activity. Initially, the pain is felt during activities only, but eventually may occur at rest (29).
One has to think of supraspinatus tendinopthy when the patient says:
• Pain increases with reaching (29).
• Pain is felt after frequent repetitive activity at, or above shoulder (37).
• Patient feels weakness of resisted abduction and forward flexion, especially with pushing and overhead movements (29).
• Patient has difficulty sleeping at night due to pain, especially when lying on the affected shoulder, and with an inability to sleep (29).
• Patient has difficulties with simple movements, such as brushing hair, putting on a shirt or jacket, or reaching the arm above shoulder height (29).
• Patient has a limited range of motion in the shoulder (29).
• Patient had a former shoulder trauma (29).
Figure 2: painfull arc test
(39)
The shoulder may be warm and there may be fullness anterolaterally (29). Further, there is a painfull arc between 70° and 120° of abduction (29) (Figure 2).
So supraspinatus tendinitis is usually consistent with anterior instability causing posterior tightness. The problems that patient with Supraspinatus Tendinitis complain off, are pain, inflammation, decreased ROM, strength, and functional activity (1).
Differential DiagnosisCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title[edit | edit source]
- Acromioclavicular Joint Injury
- Bicipital Tendonitis
- Brachial Plexus Injury
- Cervical Disc Injuries
- Cervical Discogenic Pain Syndrome
- Cervical Radiculopathy
- Cervical Spine Sprain/Strain Injuries
- Clavicular Injuries
- Contusions
- Infraspinatus Syndrome
-Myofascial Pain in Athletes
-Rotator Cuff Injury
- Shoulder Dislocation
- Subacromial impingement
- Superior Labrum Lesions
- Swimmer's Shoulder
Outcome Measures[edit | edit source]
Diagnosis is usually clinical, but imaging can be useful. Shoulder x-rays can reveal calcifications in rotator cuff tendons and in the bursaCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive titleCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title. In longstanding cases, there may be degenerative changes, such as cystic/sclerotic changes at the greater tuberosity and decreased humeral head-acromion distance, secondary to upward migration of the humeral headCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title. In acute calcific tendinitis, calcifications may be irregular, fluffy and ill-defined. Dynamic ultrasound can demonstrate thickening of the subacromial bursa and impingement during abduction. Magnetic resonance imaging (MRI), rather than computed tomography (CT), is the preferred modality, since it produces more detailed soft-tissue imagesCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title.
Examination[edit | edit source]
The shoulders are inspected for symmetry, localized swelling and muscle atrophy. There may be tenderness below the acromion and over the greater tuberosity. Internal rotation of the shoulder can facilitate palpation of the supraspinatus insertion on the greater tuberosity. The most important clinical maneuvers are as followsCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title:
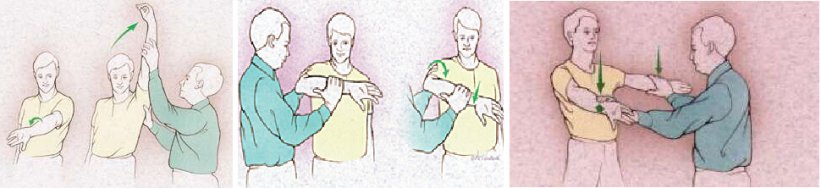
• Painful arcCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title: The patient actively abducts the arm and a painful arc occurs between 70˚ and 120˚. This is due to the compression of the supraspinatus tendon or subacromial bursa between the anterior acromial arch and humeral head. When lowering from full abduction there is often a painful “catch” at midrange. If the patient can achieve adequate muscle relaxation, passive motion tends to be less painful.
• Neer’s sign
• Hawkin’s sign
• Supraspinatus challenge test = “The Empty Beer Can” sign
• Drop arm test
• Impingement test
Neer's test Hawkin's sign Empty Can sign
Medical Management[edit | edit source]
The optimal medical management for these clinical syndromes is unclear, in part because they may be difficult to distinguish from each other or overlap with other shoulder disorders (e.g., small rotator cuff tear or early adhesive capsulitis), and because the natural histories of tendinitis is uncertainCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title.
Nonsteroidal anti-inflammatory drugs (NSAIDs) may be the first choice for mild to moderate symptoms, if there are no contraindications to these agentsCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title.
Moderate to severe symptoms may require a local subacromial corticosteroid injection. Injections are best performed under ultrasound or fluoroscopic guidance. Never inject against resistance since this indicates that the needle may be within the tendon itself, thereby, increasing the risk of tendon degeneration and ruptureCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title.
Surgical approaches include calcium deposit resection, with or without subacromial decompression, bursal resection1 and acromioplasty2, using either arthroscopic or open methods. It’s also possible to split off the coraco-acromial ligament to enlarge the space between acromion and humerus. This can cause instability, but we can compensate it with some training of the rotator cuff. The major indication for surgery is ongoing pain, loss of function and failure to respond to one year of conservative therapyCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title.
1Bursal resection: Removement of the subacromial bursa.
2Acromioplasty: Generally, it implies removal of a small piece of the surface of the acromion that is in contact with a tendon causing, by friction, damage to the latter tissue.
Physical Therapy Management[edit | edit source]
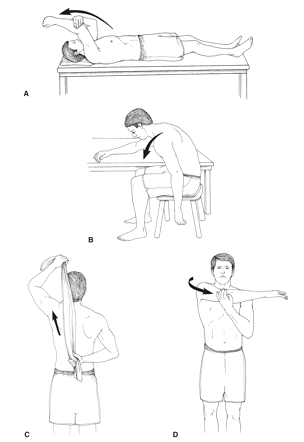
Early management includes avoidance of repetitive movements that aggravate the pain. Gentle range-of-motion exercises, such as Codman’s classic pendulum exercises, maintain range of motion and prevent development of adhesive capsulitisCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive titleCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title. Once pain has been reduced, a strengthening program focusing on the rotator cuff should be instituted. Strengthening exercises should work on the external rotators, internal rotators, biceps, deltoid, and scapular stabilizersCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title.
I.E.:
• Sidelying external rotation with dumbbell against gravity
• Prone horizontal abduction with dumbbell against gravity
• Prone anteflexion in the plane of the scapula
• Prone row with external rotation
• External rotation with Thera-tubing (standing position)
• Horizontal abduction with Thera-tubing (standing position)
• Rows with Thera-tubing (standing position)
• Elevation in the plane of the scapula (standing position)
Joint mobilization may be included with inferior, anterior, and posterior glides in the scapular planeCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title.
Stretching exercises should be done by repeating the exercise 3 times and holding the stretch each time for 30 seconds.
Examples of the stretches for home exercise program are:
Neuromuscular control exercises also may be initiatedCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title. PNF patterns will increase strength in rotator cuff muscles and increase the stability of the shoulder. We can use four different patterns.
Modalities that also may be used as an adjunct include cryotherapy, hyperthermiaCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title, transcutaneous electrical nerve stimulation and ultrasoundCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title. Intensive ultrasound therapy has been shown to increase calcium resorption, but this requires frequent treatment that may not always be practicalCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title.
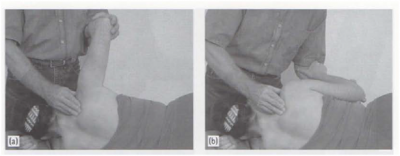
Key component of the treatment program - Friction Massage
Light to deep transverse friction massage is given over the tendon.
The patient sits comfortably on a chair, and the arm is put in a neutral or somewhat extended position with the lower arm supported.
The therapist sits at the patient's side.
A position of neutral or slight humeral extension brings the tendon forward into a position in which the site of the lesion is easily accessible to the fingertips. (see Fig.).
The therapist identifies the site of the supraspinatus tendon lying between the greater tubercle of the humerus and the acromion process. It is essential that the tendon be accurately located by knowledge of anatomy; it cannot be distinguished by palpation.
The pad of the therapist's middle finger, reinforced by the index finger (or vice versa), is placed directly over the site of the lesion, which is always just proximal to the tendon insertion on the greater tubercle. The thumb is used to stabilize the arm.
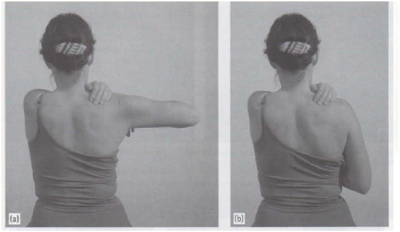
Massage of the supraspinatus muscle combined with joint movement; therapy technique.
a, Starting position. b, End position.
• Patient's starting position: lying on the left side, arm abducted.
• Therapist's starting position: standing, in front of the patient (Fig. Zahnd and Miihlemann 1998).
The therapist applies friction in a direction perpendicular to the normal orientation of the tendon, using the thumb both as fulcrum and to maintain pressure. The thumb and fingers of the opposite hand support and gather the skin over the shoulder to avoid friction between the massaging finger and skin.
This is the most valuable treatment in the management of supraspinatus tendinitis and is a key component of the treatment program. A similar technique is used for the other tendons of the rotator cuff.
Self-exercise
• Patient's starting position: sitting, arm abducted to a position before symptoms appear, contact with three finger tips of the left hand in the supraspinous fossa (a).
• Movement: pressure into the supraspinous fossa, active adduction of the right glenohumeral joint, then releasing the pressure into the supraspinous fossa, and back to the starting position (b).
Patients suffering from non-calicfying supraspinatus tendinopathy may benefit from low energy extracorporeal shock wave therapy, at least in short-termCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title.
At the end of the therapy you should initiate plyometric and sports-specific exercises.
Patient education is again reemphasized, maintaining proper mechanics, strength, and flexibility, and having a good understanding of the pathology. The patient should also show an understanding of a home exercise program with the proper warm-up and strengthening techniquesCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive titleCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title.
Key Research[edit | edit source]
Starr M, Kang H. Recognition and management of common forms tendinitis and bursitis. The Canadian Journal of CME. 2001; 155-163.
Clinical Bottom Line[edit | edit source]
Supraspinatus tendinitis is a common source of shoulder pain in athletes that participate in overhead sports (handball, volleyball, tennis, baseball). This tendinitis is in most cases caused by an impingement of the supraspinatus tendon on the acromion as it passes between the acromion and the humeral head. Pain, and a decrease in range of motion, strength and functionality are the main complaints that accompany this injury and should be addressed in the physical therapy. There is enough evidence to prove that physical applications such as ultrasound , cryotherapy, hyperthermia, transcutaneous electrical nerve stimulation and extracorporeal shock wave therapy have a beneficial effect on the recovery of supraspinatus tendinitis. But we have to remember that it is very important to use these methods as an adjunct to physical therapy (increasing ROM, strength training of the rotator cuff muscles and other shoulder stabilizers).