Subacromial Pain Syndrome: Difference between revisions
Lauren Lopez (talk | contribs) mNo edit summary |
No edit summary |
||
| (21 intermediate revisions by 6 users not shown) | |||
| Line 2: | Line 2: | ||
'''Original Editor '''- [[User:David Drinkard|David Drinkard]], [[User:Dorien De Strijcker|Dorien De Strijcker]] | '''Original Editor '''- [[User:David Drinkard|David Drinkard]], [[User:Dorien De Strijcker|Dorien De Strijcker]] | ||
''' | '''Top Contributors''' {{Special:Contributors/{{FULLPAGENAME}}}} </div> | ||
</div | |||
== Introduction == | == Introduction == | ||
There has been huge debate in relation to the diagnostic labelling of non-traumatic shoulder pain related to the structures of the subacromial space. The diagnostic label Subacromial | This page addresses the condition known as the following: | ||
* '''Subacromial impingement syndrome (SIS)''' | |||
* '''Subacromial pain syndrome (SAPS)''' | |||
* '''Rotator cuff related disorders''' | |||
* '''Biomechanical impingement of the shoulder''' | |||
There has been huge debate in relation to the diagnostic labelling of non-traumatic shoulder pain related to the structures of the subacromial space. The diagnostic label Subacromial Impingement Syndrome (SIS), presenting as anterograde-lateral shoulder pain when the arm is elevated, was first introduced in 1972 by Dr Charles Neer and was based on the mechanism of structural impingement of the structures of the subacromial space.<ref name=":5">de Witte PB Nagels J van Arkel ER, et al. Study protocol subacromial impingement syndrome: the identification of pathophysiologic mechanisms (SISTIM). BMC Musculoskelet Disord. 2011; 12:1-12. </ref><ref name=":6">Cools AM, Michener LA. Shoulder Pain: Can One Label Satisfy Everyone and Everything? Br J Sports Med. 2017 Feb 16;51(5):416–7.</ref><ref name=":7" /> SIS has been viewed as symptomatic irritation of the subacromial structures between the coracoacromial arch and the humeral head during elevation of the arm above the shoulder/head <ref name=":5" /> and as reflected by the literature is considered by many to be one of the most common causes of shoulder pain. | |||
What is important to understand is that "impingement" on its own, is not a diagnosis, but rather simply describes the mechanism: | |||
The compression of the rotator cuff against the anterior inferior aspect of the acromion and the coracoacromial ligament. | |||
Neers Classification of Impingement identified four types of shoulder impingement identified below; | |||
'''Neer Classification of Subacromial Impingement''' | '''Neer Classification of Subacromial Impingement''' | ||
| Line 11: | Line 22: | ||
According to Neer, impingement syndrome is divided into three stages: | According to Neer, impingement syndrome is divided into three stages: | ||
'''Type I''': <25 years old, Reversible, Swelling, Tendonitis, No Tears, Conservative Treatment. | '''<u>Type I</u>'''<u>:</u> <25 years old, Reversible, Swelling, Tendonitis, No Tears, Conservative Treatment. | ||
* Moderate pain during exercise, no loss of strength and no limitation in movement. Edema and/or hemorrhage may be present. This stage generally occurs in patients less than 25 years of age and is frequently associated with an overuse injury. At this stage the syndrome could be possibly reversible. <ref name="khan">KHAN Y, NAGY MT, MALAL J, WASEEM M, The painful shoulder: shoulder impingement syndrome. Open Orthop J Sept 2013, 6(7): 347-51</ref> | * Moderate pain during exercise, no loss of strength and no limitation in movement. Edema and/or hemorrhage may be present. This stage generally occurs in patients less than 25 years of age and is frequently associated with an overuse injury. At this stage, the syndrome could be possibly reversible. <ref name="khan">KHAN Y, NAGY MT, MALAL J, WASEEM M, The painful shoulder: shoulder impingement syndrome. Open Orthop J Sept 2013, 6(7): 347-51</ref> | ||
'''Type II''': 25-40 years old, Permanent Scarring, Tendonitis, No Tears, Subacromial Decompression | '''<u>Type II</u>'''<u>:</u> 25-40 years old, Permanent Scarring, Tendonitis, No Tears, Subacromial Decompression | ||
* Pain is usually reported during ADL and especially during the night. loss of mobility is associated with this stage. Type II is more advanced and tends to occur in patients between 25 to 40 years of age. The pathological changes show fibrosis as well as irreversible tendon changes.<ref name="khan" /> | * Pain is usually reported during ADL and especially during the night. loss of mobility is associated with this stage. Type II is more advanced and tends to occur in patients between 25 to 40 years of age. The pathological changes show fibrosis as well as irreversible tendon changes.<ref name="khan" /> | ||
'''Type III''': >40 years old, Small Rotator Cuff Tear, Subacromial Decompression with Debridement/Repair | '''<u>Type III</u>'''<u>:</u> >40 years old, Small Rotator Cuff Tear, Subacromial Decompression with Debridement/Repair | ||
'''Type IV''': >40 years old, Large Rotator Cuff Tear, Sub Acromial Decompression with Repair | '''<u>Type IV</u>'''<u>:</u> >40 years old, Large Rotator Cuff Tear, Sub Acromial Decompression with Repair | ||
While Neers Classification of SIS was key to understanding shoulder pathology at the time, SIS was further broken down into four subtypes associated with either External Impingement (Primary or Secondary) and Internal Impingement. | While Neers Classification of SIS was key to understanding shoulder pathology at the time, SIS was further broken down into four subtypes associated with either '''External Impingement''' (Primary or Secondary) and '''Internal Impingement'''. | ||
==== | ====External Impingement==== | ||
[[File:Shapes of Acromion.jpg|thumb|463x463px|Figure 1. Acromion Shapes]] | [[File:Shapes of Acromion.jpg|thumb|463x463px|Figure 1. Acromion Shapes]] | ||
* Primary External Impingement related to structural changes, either congenital or acquired, that mechanically narrow the subacromial space such as; bony narrowing or osteophyte formation, bony malposition after a fracture, or an increase in the volume of the subacromial soft tissues.<ref>Neer CS. Anterior acromioplasty for the chronic impingement syndrome in the shoulder: A preliminary report. J Bone Joint Surg Am. 1972;54:41–50.</ref><ref>Leroux J-L, Codine P, Thomas E, Pocholle M, Mailhe D, Blotman F. Isokinetic evaluation of rotational strength in normal shoulders and shoulders with impingement syndrome. Clin Orthop. 1994;304:108–115</ref><ref name="af" /><ref name=":0">Bigliani LU, Levine WN. Current concepts review: Subacromial impingement syndrome. J Bone Joint Surg Am. 1997;79:1854–1868.</ref><ref name=":14">Harryman DT, Sidles JA, Clark JM, McQuade KJ, Gibb TD, Matsen FA. Translation of the humeral head on the glenoid with passive glenohumeral motion. J Bone Joint Surg Am. 1990;72-a:1334–1343.</ref><ref name=":16">Morrison DS, Greenbaum BS, Einhorn A. Shoulder impingement. Orthop Clin North Am. 2000;31:285–293</ref><ref name=":17">Nicholson GP, Goodman DA, Flatow EL, Bigliani LU. The acromion: Morphologic condition and age-related changes. A study of 420 scapulas. J Shoulder Elbow Surg. 1996;5:1–11.</ref><ref>Lewis JS, Wright C, Green A. Subacromial impingement syndrome: The effect of changing posture on shoulder range of movement. J Orthop Sports Phys Ther. 2005;35:72–87.</ref><ref name="debie">DE BIE R.A., BASTIANENEN C.H.G. Effectiveness of individualized physiotherapy on pain and functioning compared to a standard exercise protocol in patients presenting with clinical signs of subacromial impingement syndrome. A randomized controlled trial. BMC Musculoskeletal Disorders. 2010 Jun 9; 11:114.Level of evicence: 1B</ref><ref name="page">Phil Page, PhD, PT, ATC, LAT, CSCS, FACSM, Shoulder Muscle Imbalance and Subacromial Impingement Syndrome in Overhead Athletes, Int J Sport Phys. Ther., 2011</ref><ref name="coaches">http://www.sbcoachescollege.com/articles/UpperCrossSyndromeShPain.html</ref> The shape of the acromion process of the scapula or shoulder blade may play an important role in recovery and treatment from primary impingement. | * '''Primary External Impingement''' related to structural changes, either congenital or acquired, that mechanically narrow the subacromial space such as; bony narrowing or osteophyte formation, bony malposition after a fracture, or an increase in the volume of the subacromial soft tissues.<ref>Neer CS. Anterior acromioplasty for the chronic impingement syndrome in the shoulder: A preliminary report. J Bone Joint Surg Am. 1972;54:41–50.</ref><ref>Leroux J-L, Codine P, Thomas E, Pocholle M, Mailhe D, Blotman F. Isokinetic evaluation of rotational strength in normal shoulders and shoulders with impingement syndrome. Clin Orthop. 1994;304:108–115</ref><ref name="af" /><ref name=":0">Bigliani LU, Levine WN. Current concepts review: Subacromial impingement syndrome. J Bone Joint Surg Am. 1997;79:1854–1868.</ref><ref name=":14">Harryman DT, Sidles JA, Clark JM, McQuade KJ, Gibb TD, Matsen FA. Translation of the humeral head on the glenoid with passive glenohumeral motion. J Bone Joint Surg Am. 1990;72-a:1334–1343.</ref><ref name=":16">Morrison DS, Greenbaum BS, Einhorn A. Shoulder impingement. Orthop Clin North Am. 2000;31:285–293</ref><ref name=":17">Nicholson GP, Goodman DA, Flatow EL, Bigliani LU. The acromion: Morphologic condition and age-related changes. A study of 420 scapulas. J Shoulder Elbow Surg. 1996;5:1–11.</ref><ref>Lewis JS, Wright C, Green A. Subacromial impingement syndrome: The effect of changing posture on shoulder range of movement. J Orthop Sports Phys Ther. 2005;35:72–87.</ref><ref name="debie">DE BIE R.A., BASTIANENEN C.H.G. Effectiveness of individualized physiotherapy on pain and functioning compared to a standard exercise protocol in patients presenting with clinical signs of subacromial impingement syndrome. A randomized controlled trial. BMC Musculoskeletal Disorders. 2010 Jun 9; 11:114.Level of evicence: 1B</ref><ref name="page">Phil Page, PhD, PT, ATC, LAT, CSCS, FACSM, Shoulder Muscle Imbalance and Subacromial Impingement Syndrome in Overhead Athletes, Int J Sport Phys. Ther., 2011</ref><ref name="coaches">http://www.sbcoachescollege.com/articles/UpperCrossSyndromeShPain.html</ref> <ref>Creech JA, Silver S. [https://www.ncbi.nlm.nih.gov/books/NBK554518/ Shoulder impingement syndrome.] InStatPearls [Internet] 2021 Jul 26. StatPearls Publishing.</ref>The shape of the acromion process of the scapula or shoulder blade may play an important role in recovery and treatment from primary impingement. | ||
* Secondary External Impingement related to abnormal scapulothoracic kinematics, strength balance alteration resulting in functional disturbance in the centering of the humeral head, leading to an abnormal displacement of the center of rotation when the arm is elevated. Generally caused by weakness of the Rotator Cuff Muscles (functional instability) combined with a glenohumeral joint capsule and ligaments that are to loose (micro-instability). Impingement generally occurs at the coracoacromial space secondary to anterior translation of the humeral head as opposed to the Subacromial space that is seen in primary impingement. Typically occurs in younger individuals with pain is located in the anterior or anterolateral aspect of the shoulder. The symptoms are usually activity specific and involve overhand activities.<ref name=":0" /><ref name=":14" /><ref name=":16" /><ref name=":17" /><ref name=":1" /><ref name=":10" /><ref name=":11" /><ref name=":0" /><ref name=":12" /><ref name=":13" /> | * '''Secondary External Impingement''' related to abnormal scapulothoracic kinematics, strength balance alteration resulting in functional disturbance in the centering of the humeral head, leading to an abnormal displacement of the center of rotation when the arm is elevated. Generally caused by weakness of the Rotator Cuff Muscles (functional instability) combined with a glenohumeral joint capsule and ligaments that are to loose (micro-instability). Impingement generally occurs at the coracoacromial space secondary to anterior translation of the humeral head as opposed to the Subacromial space that is seen in primary impingement. Typically occurs in younger individuals with pain is located in the anterior or anterolateral aspect of the shoulder. The symptoms are usually activity-specific and involve overhand activities.<ref name=":0" /><ref name=":14" /><ref name=":16" /><ref name=":17" /><ref name=":1" /><ref name=":10" /><ref name=":11" /><ref name=":0" /><ref name=":12" /><ref name=":13" /> | ||
==== | ====Internal Impingement==== | ||
* Internal Glenoid Impingement is probably the most common cause of posterior shoulder | * '''Internal Glenoid Impingement''' is probably the most common cause of posterior shoulder pain in the throwing or overhead athlete. Caused by impingement of the articular surface (intra-articular) of the Rotator Cuff (posterior edge of the supraspinatus and the anterior edge of the infraspinatus) against the posterior-superior-glenoid and glenoid labrum. Mainly seen with repetitive overhead activities, this positioning becomes pathologic during excessive external rotation, anterior capsular instability, scapular muscle imbalances<ref name=":12" />, and/or upon repetitive overload of the rotator cuff musculature <ref name=":13" /><ref name=":1">Urwin M, Symmons D, Allison T, et al.: Estimating the burden of musculoskeletal disorders in the community: the comparative prevalence of symptoms at different anatomical sites, and the relation to social deprivation. Ann Rheum Dis 1998; 57: 649–55.</ref><ref name=":10">McClure PW, Michener LA, Karduna AR. Shoulder function and 3-dimensional scapular kinematics in people with and without shoulder impingement syndrome. Phys Ther. 2006;86:1075–1090.</ref><ref name=":11">Belling Sorensen AK, Jorgensen U. Secondary impingement in the shoulder. Scand J Med Sci Sports. 2000;10:266–278.</ref><ref name=":0" /><ref name=":12">Lukasiewicz AC, McClure P, Michener L, Pratt N, Sennett B. Comparison of 3-dimensional scapular position and orientation between subjects with and without shoulder impingement. J Orthop Sports Phys Ther. 1999;29:574–583.</ref><ref name=":13">Belling Sorensen AK, Jorgensen U. Secondary impingement in the shoulder. Scand J Med Sci Sports. 2000;10:266–278.</ref>. These deficiencies result in poor scapulohumeral control. | ||
These definitions and descriptions of SIS are based on a hypothesis that acromial irritation leads to external abrasion of the bursa, rotator cuff or other structures within the subacromial space.<ref name=":7">Lewis J. Subacromial Impingement Syndrome: A Musculoskeletal Condition or a Clinical Illusion? Physical Therapy Reviews 2011;16:388-298.</ref> Throughout the years, the description progressed from SIS to ‘impingement related shoulder pain’, with the growing opinion that ‘impingement’ represents a cluster of symptoms and a possible mechanism for the pain, rather than a pathoanatomic diagnose itself. This remained the dominant theory for injury to structures within the subacromial space for the past 40 years | These definitions and descriptions of SIS are based on a hypothesis that acromial irritation leads to external abrasion of the bursa, rotator cuff or other structures within the subacromial space.<ref name=":7">Lewis J. Subacromial Impingement Syndrome: A Musculoskeletal Condition or a Clinical Illusion? Physical Therapy Reviews 2011;16:388-298.</ref> Throughout the years, the description progressed from SIS to ‘impingement related shoulder pain’, with the growing opinion that ‘impingement’ represents a cluster of symptoms and a possible mechanism for the pain, rather than a pathoanatomic diagnose itself. This remained the dominant theory for injury to structures within the subacromial space for the past 40 years and has been the rationale to guide clinical tests, conservative treatment, surgical procedures and rehabilitation protocols,<ref name=":6" /> however the validity of this model of acromial impingement has been challenged from both a theoretical and practical perspective throughout the last decade, with suggestions that the use of SIS terminology can potentially contribute to negative expectations of physiotherapy and conservative treatment for patients, which may compromise outcome, often resulting in an increased incidence for surgery.<ref name=":8" /><ref name=":6" /><ref name=":7" /><ref name=":8">Cuff A, Littlewood C. Subacromial Impingement Syndrome - What does this mean to and for the Patient? A Qualitative Study. Musculoskeletal Science and Practice. Elsevier Ltd; 2017 Oct 17;:1–14.</ref> | ||
While controversy surrounding the diagnostic labelling continues to exist, with many different terms in use to describe subacromial pain and it’s pathology in the literature it has been suggested that the label of SIS does not fully explain the mechanism. Many other diagnostic labels have been proposed but it has been suggested that the term Subacromial Pain Syndrome (SAPS) best describes the pain thought to originate from structures lying between the acromion and the humeral head, most often associated with some degree of shoulder dysfunction,<ref name=":9">Diercks R, Bron C, Dorrestijn O, Meskers C, Naber R, de Ruiter T, et al. Guideline for Diagnosis and Treatment of Subacromial Pain Syndrome. Acta Orthopaedica. 2014 May 21;85(3):314–22.</ref> but does not reflect many other causes of shoulder pain located outside the subacromial space. | While controversy surrounding the diagnostic labelling continues to exist, with many different terms in use to describe subacromial pain and it’s pathology in the literature it has been suggested that the label of SIS does not fully explain the mechanism. Many other diagnostic labels have been proposed but it has been suggested that the term '''Subacromial Pain Syndrome (SAPS)''' best describes the pain thought to originate from structures lying between the acromion and the humeral head, most often associated with some degree of shoulder dysfunction,<ref name=":9">Diercks R, Bron C, Dorrestijn O, Meskers C, Naber R, de Ruiter T, et al. Guideline for Diagnosis and Treatment of Subacromial Pain Syndrome. Acta Orthopaedica. 2014 May 21;85(3):314–22.</ref> but does not reflect many other causes of shoulder pain located outside the subacromial space. | ||
== Definition / Description == | '''Bottom line:''' | ||
Subacromial Pain Syndrome is by defined Diercks et al <ref name=":9" /> as all non-traumatic, usually unilateral, shoulder problems that cause pain, localized around the acromion, often worsening during or subsequent to lifting | * Subacromial impingement: Bursal side | ||
* Internal impingement: Articular side | |||
* Intrinsic mechanisms: Within the tendons | |||
* Extrinsic mechanisms: External to the tendons. | |||
== Definition/Description == | |||
Subacromial Pain Syndrome is by defined Diercks et al <ref name=":9" /> as all non-traumatic, usually unilateral, shoulder problems that cause pain, localized around the acromion, often worsening during or subsequent to lifting the arm. It is basically a generic term that encompasses pain associated with any lesion within a structure or structures within the Subacromial Space. As such the SAPS incorporates all conditions related to subacromial structures such as subacromial bursitis, calcific tendonitis, rotator cuff tendinopathy, rotator cuff tears, biceps tendinopathy, or tendon cuff degeneration as a result of the controversy regarding its pathogenesis.<ref name=":9" /> <ref name=":15">Björnsson Hallgren H. Treatment of Subacromial Pain and Rotator Cuff Tears [dissertation]. Linköping University Sweden. 2012.</ref>Subacromial pain syndrome is poorly understood despite being a commonly diagnoses.<ref>Dhillon KS. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6915323/ Subacromial impingement syndrome of the shoulder: a musculoskeletal disorder or a medical myth?.] Malaysian orthopaedic journal. 2019 Nov;13(3):1.</ref> | |||
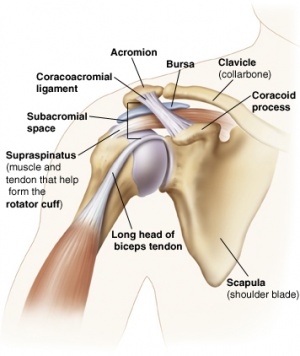
== Clinically Relevant Anatomy == | == Clinically Relevant Anatomy == | ||
The '''Subacromial Space''' is the space beneath the acromion (between the acromion and the top surface of the humeral head). This space is outlined by the acromion and the coracoid process (which are parts of the scapula), and the | The '''Subacromial Space''' is the space beneath the acromion (between the acromion and the top surface of the humeral head). This space is outlined by the acromion and the coracoid process (which are parts of the scapula), and the coracoacromial ligament which connects the two. <ref>http://www.jointsurgery.in/shoulder-arthoscopy/anatomy-of-shoulder/</ref>[[Image:Subacromial structures.jpg|thumb|356x356px|Figure 2. Subacromial Structures ]] | ||
The Subacromial Space measures | The Subacromial Space measures between 2 and 17 millimeters depending on the arm position and contains the following anatomical structures: <ref name=":14" /><ref name=":7" /><ref>Lewis J, McCreesh K, Roy JS, Ginn K. Rotator cuff tendinopathy: navigating the diagnosis-management conundrum. journal of orthopaedic & sports physical therapy. 2015 Nov;45(11):923-37.</ref> | ||
* Coracoacromial Arch, composed of the Acromion, Coracoid Process and Coracoacromial Ligaments<ref name="af">KATCHINGWE AF, Phillips B, Sletten E, Plunkett SW., Comparison of Manual Therapy Techniques with Therapeutic Exercise in the Treatment of Shoulder Impingement: A Randomized Controlled Pilot Clinical Trial. The Journal of Manual Manipulative Therapy 2008;16(4): p238-¬‐247</ref> | * Coracoacromial Arch, composed of the Acromion, Coracoid Process and Coracoacromial Ligaments<ref name="af">KATCHINGWE AF, Phillips B, Sletten E, Plunkett SW., Comparison of Manual Therapy Techniques with Therapeutic Exercise in the Treatment of Shoulder Impingement: A Randomized Controlled Pilot Clinical Trial. The Journal of Manual Manipulative Therapy 2008;16(4): p238-¬‐247</ref> | ||
* Humeral Head | * Humeral Head | ||
| Line 43: | Line 60: | ||
* Tendons of the Rotator Cuff; Supraspinatus, Infraspinatus, Teres Minor and Subscapularis | * Tendons of the Rotator Cuff; Supraspinatus, Infraspinatus, Teres Minor and Subscapularis | ||
* Tendon of the Long Head of Biceps Brachii | * Tendon of the Long Head of Biceps Brachii | ||
* Coracoacromial ligament | |||
* G-H Joint Capsule | * G-H Joint Capsule | ||
== Prevalence / Incidence == | == Shoulder Biomechanics Review == | ||
SAPS is the most common disorder of the shoulder, accounting for anywhere between 44% to 65% of all complaints of shoulder pain, <ref>Bhattacharyya R, Edwards K, Wallace AW. Does arthroscopic sub-acromial decompression really work for sub-acromial impingement syndrome: a cohort study. BMC Musculoskelet Disord. 2014;15:1. </ref> with the incidence increasing with age.<ref>Randelli P, Randelli F, Ragone V, et al. Regenerative medicine in rotator cuff injuries. BioMed Res Int. 2014;2014:129515</ref> Peak incidence occurs during the sixth decade of life.<ref>Ostor AJ, Richards CA, Prevost AT, Speed CA, Hazleman BL: Diagnosis and relation to general health of shoulder disorders presenting to primary care. Rheumatology (Oxford) 2005; 44: 800–5.</ref> | It is important to remember that movements of the shoulder do not occur in isolation of the GH joint. During arm elevation, the following articulations/movements occur within the shoulder complex: | ||
* '''Posterior roll and inferior glide of the humeral head'''. | |||
* '''Posterior rotation of the clavicle:''' which will allow a functioning at the lateral end of the clavicle during elevation and posterior rotation, raising the acromion and help maintain the subacromial space. | |||
* '''External rotation of the scapular''': which means the medial border of the scapula moves towards the thoracic spine and chest wall. As your humerus laterally rotates, the scapular follows that into lateral rotation. | |||
* A '''scapular posterior tilt''' towards the end of elevation (the inferior angle of the scapula will move towards the chest wall). | |||
* Also an '''upward rotation of the scapular''': the movement of the inferior angle of the scapula from the thoracic spine. | |||
It is generally the upward rotation of the scapula which keeps the acromion high; maintaining that acromio-humeral distance and reducing the possibility of impinging of the structures within the subacromial space. The upward rotation movement is generally carried out with the recruitment of the different sections of the trapezius muscle (upper / middle / lower). It is also this movement (upward rotation) which allows the glenoid fossa to follow the humeral head, to maintain a congruency during arm elevation. | |||
'''Scapulohumeral Rhythm:''' Ratio of the GH movement to the scapulothoracic movement during arm elevation. Overall the value is 2:1; meaning for every 1 degree of scapular rotation, we see 2 degrees of humeral elevation - for example, a 180-degree range of motion for elevation, we'll see 60 degrees of scapular upward rotation with 120 degrees of humeral abduction. However, the ratio is not consistent across an entire arc of shoulder elevation. | |||
==== The importance of external rotation of the humerus during elevation: ==== | |||
During arm elevation, normally there is an external (lateral) rotation of the humerus. If the timing of the movement is correct, this external rotation of the humerus during elevation permits the avoidance of the compression of the greater tuberosity against the subacromial structures. If the timing is not right (poor neuromuscular recruitment, internal rotation of the humerus or dysfunctional biomechanics of the shoulder complex), the necessary external rotation will not occur and the greater tuberosity will internally compress the structures and cause an irritation of the tissues. | |||
See the Physiopedia page on [[Biomechanics of the Shoulder|Shoulder Biomechanics]], for further information. | |||
== Prevalence/Incidence == | |||
SAPS is the most common disorder of the shoulder<ref>Park SW, Chen YT, Thompson L, Kjoenoe A, Juul-Kristensen B, Cavalheri V, McKenna L. [https://www.nature.com/articles/s41598-020-76704-z No relationship between the acromiohumeral distance and pain in adults with subacromial pain syndrome: a systematic review and meta-analysis]. Scientific Reports. 2020 Nov 26;10(1):1-4.</ref>, accounting for anywhere between 44% to 65% of all complaints of shoulder pain, <ref>Bhattacharyya R, Edwards K, Wallace AW. Does arthroscopic sub-acromial decompression really work for sub-acromial impingement syndrome: a cohort study. BMC Musculoskelet Disord. 2014;15:1. </ref> with the incidence increasing with age.<ref>Randelli P, Randelli F, Ragone V, et al. Regenerative medicine in rotator cuff injuries. BioMed Res Int. 2014;2014:129515</ref> Peak incidence occurs during the sixth decade of life.<ref>Ostor AJ, Richards CA, Prevost AT, Speed CA, Hazleman BL: Diagnosis and relation to general health of shoulder disorders presenting to primary care. Rheumatology (Oxford) 2005; 44: 800–5.</ref> | |||
== Etiology == | == Etiology == | ||
There remains debate in regards to the | There remains a debate in regards to the etiology of subacromial pain, but it is proposed that the mechanisms include intrinsic, extrinsic and combined factors including muscle imbalance and anatomical factors that may affect the subacromial space; variations in the acromial shape; the anterior slope; the angle of the acromion; and the lateral extension of the acromion over the humeral head. Osseous changes of the inferior acromioclavicular joint or the coracoacromial ligament may also affect the subacromial space. <ref name=":15" /> | ||
While it is accepted that multiple factors are involved in the pathology, several unresolved issues remain such as: which subacromial structure is first engaged by pathology, and what are the pain-generating mechanisms? <ref name=":15" /> | |||
== Contributing Factors == | |||
There are both intrinsic and extrinsic factors which could predispose a person from experiencing a reduction in subacromial space during arm elevation. | |||
'''Intrinsic factors: (generally non-modifiable)''' | |||
* Tendon histology (quality of the tendons) | |||
* Age | |||
* Genetics | |||
'''Extrinsic factors: (potentially modifiable)''' | |||
* Muscle extensibility / performance | |||
* Anatomical/osseous | |||
* GH joint kinematics | |||
* Posture/ergonomics | |||
==== Different types of impingement ==== | |||
'''Subacromial extra-articular impingement: Bursal.''' Compression caused as a result of a decreased in subacromial (AHD) space. Pain is generally located over the anterior aspect of the shoulder with elevation. | |||
'''Internal impingement: Articular.''' Caused by contact between the articular side of the supra/infraspinatus and the posterosuperior rim of the glenoid. Pain is located posteriorly "inside" the joint when in a ABER (throwing) position. | |||
'''Subcoracoid impingement:''' A history of dull pain in the anterior aspect of the shoulder. Exacerbated by the shoulder in forward flexion, ADDuction and internal (medial) rotation (such as the motion of hitting the ball with a racket). | |||
==== Impingement Mechanisms ==== | |||
There are 3 main mechanisms that can affect the distance/space of the subacromial space (acromio-humeral distance) | |||
# Loss of control of the humeral head (GH instabilities) | |||
# Loss of scapular control (scapular instabilities) | |||
# Change to the actual size of structures within the space (tendons of the RC muscles, subacromial bursae, for example). | |||
'''Intrinsic Mechanisms: What can affect the size of the content of the subacromial space?''' | |||
== Clinical Presentation | The load on the tendon (shear or compressive forces). Tendon "overload" due to excessive or repetitive forces on the tendons. This can cause reactive tendinopathy or a tendon dysrepair (causing a painful response to movement). Keep in mind that changes to the tendons are normal depending on activity levels and age. | ||
== Clinical Presentation == | |||
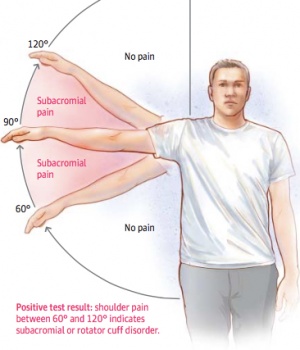
[[File:SIS CP.jpg|thumb|Figure 3. Painful Arc]] | [[File:SIS CP.jpg|thumb|Figure 3. Painful Arc]] | ||
The affected patients are generally over age 40 and suffer from persistent pain without any known preceding trauma.<ref>Garving, C., Jakob, S., Bauer, I., Nadjar, R., & Brunner, U. H. (2017). Impingement Syndrome of the Shoulder, 765–777. | The affected patients are generally over age 40 and suffer from persistent pain without any known preceding trauma.<ref>Garving, C., Jakob, S., Bauer, I., Nadjar, R., & Brunner, U. H. (2017). Impingement Syndrome of the Shoulder, Dtsch Arztebl. 765–777. [https://www.aerzteblatt.de/int/archive/article/194351 https://doi.org/10.3238/arztebl.2017.0765]</ref> Patients report pain on elevating the arm between 70 ° and 120 °, the “Painful Arc” (Figure 3), on forced movement above the head, and when lying on the affected side.<ref name=":1" /> The symptoms may be acute or chronic. Most often it is a gradual, degenerative condition that causes "impingement", rather than due to a strong external force. Therefore, patients often have difficulties with determining the exact onset of symptoms. | ||
In recent studies, there has been a great deal of talk about GIRD (Glenohumeral Internal Rotation Deficit), which can be understood as a loss of internal (medial) rotation range of motion, in the presence of a loss of total rotational motion (evaluation of the total range of motion, of both shoulders). | |||
'''GIRD = (side-to-side difference in ER) + (side-to-side difference in IR)''' | |||
A contributing factor to GIRD has been theorized to be the thickening of the posterior GH capsule, limiting the overall range of internal rotation of the GH joint. | |||
== Differential Diagnosis == | == Differential Diagnosis == | ||
There are a variety of shoulder conditions that can initially be confused with | There are a variety of shoulder conditions that can initially be confused with subacromial pain syndrome <ref name=":2">Fongemie AE, Buss DD, Rolnick SJ. [https://www.aafp.org/afp/1998/0215/p667.html#sec-6 Management of shoulder impingement syndrome and rotator cuff tears]. American family physician. 1998 Feb 15;57(4):667.</ref>. A thorough physical examination should exclude other conditions such as <ref>Lockhart RD. Movements of the Normal Shoulder Joint and of a case with Trapezius Paralysis studied by Radiogram and Experiment in the Living. J Anat 1930; 64: 288-302</ref>: | ||
* [[Rotator Cuff Tears]] (Partial / Full) | * [[Rotator Cuff Tears]] (Partial / Full) | ||
* [[Thoracic Outlet Syndrome (TOS)]] | * [[Thoracic Outlet Syndrome (TOS)]] | ||
* [[Cervical Spondylosis]] | * [[Cervical Spondylosis]] | ||
* Subluxating Shoulder | * Subluxating Shoulder | ||
* SLAP or labral lesions | |||
* [[Acromioclavicular Joint Disorders]] | * [[Acromioclavicular Joint Disorders]] | ||
* [[ | * [[Frozen Shoulder|Adhesive Capsulitis (Frozen Shoulder)]] | ||
* Glenohumeral Arthritis | * Glenohumeral Arthritis | ||
* Paralysis of the Trapezius | * Paralysis of the Trapezius | ||
| Line 71: | Line 139: | ||
* Arthropathy | * Arthropathy | ||
* [[Shoulder Instability|Glenohumeral Instability]] | * [[Shoulder Instability|Glenohumeral Instability]] | ||
* Cervical radicular pain or referred cervical facet pain | |||
* Nerve Palsy | * Nerve Palsy | ||
== Physical Examination == | == Physical Examination == | ||
Detailed History and clinical examination are necessary | Detailed History and clinical examination are necessary for the diagnosis of SAPS. No single test alone is accurate to diagnose SAPS or sufficiently differentiate between various shoulder disorders <ref>Hegedus EJ, Goode A, Campbell S, Morin A, Tamaddoni M, Moorman CT, Cook C. Physical Examination Tests of the Shoulder: A Systematic Review with Meta-analysis of Individual Tests. British Journal of Sports Medicine. 2007 Aug 24.</ref><ref>Hughes PC, Taylor NF, Green RA. Most Clinical Tests Cannot Accurately Diagnose Rotator Cuff Pathology: A Systematic Review . Aust J Physiother. 2008;54(3):159–70.</ref>, but using a combination of specific tests increases the post-test probability of the diagnosis of SAPS. <ref>Murrell GA, Walton JR. Diagnosis of Rotator Cuff Tears. The Lancet. 2001 Mar 10;357(9258):769-70.</ref><ref>Park HB, Yokota A, Gill HS, El Rassi G, McFarland EG. Diagnostic Accuracy of Clinical Tests for the Different Degrees of Subacromial Impingement Syndrome. JBJS. 2005 Jul 1;87(7):1446-55.</ref><ref>Michener LA, Walsworth MK, Doukas WC, Murphy KP. Reliability and Diagnostic Accuracy of 5 Physical Examination Tests and Combination of Tests for Subacromial Impingement. Archives of Physical Medicine and Rehabilitation. 2009 Nov 1;90(11):1898-903.</ref><ref name="michener">MICHENER L.A., WALSWORTH M.K., DOUKAS W.C., MURPHY K.P. Reliability and Diagnostic Accuracy of 5 Physical Examination Tests and Combination of Tests for Subacromial Impingement. Archives of Physical Medicine and Rehabilitation. 2009 Nov; 90(11): 1898-903. Level of evicence: 1C</ref> | ||
The Dutch Orthopaedic Association Guidelines <ref name=":9" /> for diagnosis and treatment of subacromial pain syndrome recommend a combination of the following tests to aid in the diagnosis; | The Dutch Orthopaedic Association Guidelines <ref name=":9" /> for diagnosis and treatment of subacromial pain syndrome recommend a combination of the following tests (pain provocation tests) to aid in the diagnosis; | ||
* [[Hawkins / Kennedy Impingement Test of the Shoulder|Hawkins-Kennedy Test]] | * [[Hawkins / Kennedy Impingement Test of the Shoulder|Hawkins-Kennedy Test]] | ||
* [[Painful Arc|Painful Arc Test]] | * [[Painful Arc|Painful Arc Test]] | ||
| Line 84: | Line 153: | ||
* 3 tests are positive: the probability that the patient has SAPS is (10,56) <ref name=":18" /> | * 3 tests are positive: the probability that the patient has SAPS is (10,56) <ref name=":18" /> | ||
* 2 tests are positive: the probability that the patient has SAPS is (5,03) <ref name=":18" /> | * 2 tests are positive: the probability that the patient has SAPS is (5,03) <ref name=":18" /> | ||
* 1 test is | * 1 test is positive: the probability that the patient has SAPS is (0,90) <ref name=":18" /> | ||
* 0 tests are positive: the probability that the patient has SAPS is (0,17) <ref name=":18" /> | * 0 tests are positive: the probability that the patient has SAPS is (0,17) <ref name=":18" /> | ||
The following additional test should also be used to rule out a Rotator Cuff Tear; | The following additional test should also be used to rule out a Rotator Cuff Tear; | ||
* [https://www.youtube.com/watch?v=JXgRBeqToik Drop Arm Test]: To test the integrity of the [[ | * [https://www.youtube.com/watch?v=JXgRBeqToik Drop Arm Test]: To test the integrity of the [[Supraspinatus|Supraspinatus.]] <ref name=":3">ALGUNAEE M, GALVIN R, FAHEY T, Diagnostic accuracy of clinical tests for subacromial impingement syndrome: a systematic review and meta-analysis. Ach Phys Med Rehabil 2012, 93(2): 229-36</ref> | ||
There is also the Neer Impingement Test, which evaluates a subacromial impingement specifically, while the Hawkins-Kennedy Test evaluates the presence of a coracoacromial impingement. | |||
Considerations for poor neuromuscular control of the scapula (to consider and objectively evaluate, when possible): | |||
* Loss of dynamic stability of the scapula | |||
* Pectoralis minor length and flexibility | |||
* Scapular muscle performance and endurance | |||
* Thoracic spine function/mobility | |||
* Range of motion of GH joint (tightness of joint capsule, or even a GH instability) | |||
* Rotator cuff muscle balance (agonist/antagonist / synergistic muscle activity), performance and muscular endurance. | |||
'''Other considerations:''' | |||
* Capsular tightness: Specific assessment of the posterior capsule, potentially limiting the range of motion in internal rotation (GIRD). | |||
* Lack of extensibility of external rotator muscles (infraspinatus/teres minor). | |||
* Lack of muscular strength, neuromuscular control or endurance of external rotators (infraspinatus/teres minor). | |||
* Lack of extensibility of internal rotators (lattissimus dorsi and pectoralis minor for example). | |||
* Contributions of the serratus anterior muscle to the movement of the scapula (upward rotation, posterior tilt, external rotation and protraction of the scapula) during elevation. | |||
* Thoracic spine and rib cage mobility. A healthy spine and rib cage movement will not impede any movements of the shoulder or scapular complex during upper extremity movements. | |||
== Diagnostic Procedures == | == Diagnostic Procedures == | ||
Radiographs may be used to detect anatomical variants, calcific deposits or acromioclavicular joint arthritis. The three recommended views are<ref>Smith M, Sparkes V, Busse M, Enright S. Upper and Lower trapezius muscle activity in subjects with subacromial impingement symptoms: Is there imbalance and can taping change it? Physical Therapy in Sport. 2009:10, 45-50</ref> | '''Overall considerations''' | ||
* Antero-posterior View with the arm at 30 degrees external rotation which is useful for assessing the glenohumeral joint, subacromial osteophytes and sclerosis of the greater tuberosity. | |||
* Outlet Y View is useful because it shows the subacromial space and can differentiate the acromial processes. | There are anatomical factors which may influence the narrowing of the subacromial space, such as: | ||
* Axillary View is helpful in visualizing the acromion and the | * The presence of a subacromial bone spur (potential thickening or calcification of the coracoacromial ligament) | ||
* The shape of the acromion (type I (flat) / type II (curved)/ type III (hook)/ type IV (upward oriented acromion)) | |||
* AC joint arthrosis (degeneration of surrounding tissues) | |||
* Instability of the humeral head (of the GH joint) | |||
Radiographs may be used to detect anatomical variants, calcific deposits or acromioclavicular joint arthritis. The three recommended views are:<ref>Smith M, Sparkes V, Busse M, Enright S. Upper and Lower trapezius muscle activity in subjects with subacromial impingement symptoms: Is there imbalance and can taping change it? Physical Therapy in Sport. 2009:10, 45-50</ref> | |||
* '''Antero-posterior View''' with the arm at 30 degrees external rotation which is useful for assessing the glenohumeral joint, subacromial osteophytes and sclerosis of the greater tuberosity. | |||
* '''Outlet Y View''' is useful because it shows the subacromial space and can differentiate the acromial processes. | |||
* '''Axillary View''' is helpful in visualizing the acromion and the process coracoid, as well as coracoacromial ligament calcifications. | |||
The size of the subacromial space can also be measured. MRI can show full or partial tears in the tendons of the rotator cuff, and inflammation to weak structures. Ultrasound and arthrography are being used when rotator cuff tears are suspected or in complex cases.<ref name="khan" /> | The size of the subacromial space can also be measured. MRI can show full or partial tears in the tendons of the rotator cuff, and inflammation to weak structures. Ultrasound and arthrography are being used when rotator cuff tears are suspected or in complex cases.<ref name="khan" /> | ||
There is a good clinical-radiological association between subacromial pain syndrome and findings on ultrasound.<ref>Rodríguez-Piñero Durán M, Vidal Vargas V, Castro Agudo M. Hallazgos ecográficos en el síndrome de dolor subacromial crónico [Ultrasound findings in chronic subacromal pain syndrome]. Rehabilitacion (Madr). 2019;53(4):240-6. </ref> The diagnostic accuracy of ultrasound is considered good and comparable to that of conventional MRI for identification and quantification of complete (full-thickness) rotator cuff injuries. The sensitivity and specificity of ultrasound and conventional MRI are not significantly different in the detection of partial- or full-thickness rotator cuff tears with MR Arthrography an accurate method to rule out partial rotator cuff injuries.<ref name=":9" /> | |||
The Dutch Orthopaedic Association Guidelines arise the use of | The Dutch Orthopaedic Association Guidelines arise the use of ultrasounds the most valuable and cost-effective diagnostic imaging if the first period of conservative treatment fails, which they recommend can be combined with conventional radiography of the shoulder to determine osteoarthritis, osseous abnormalities, and presence/absence of calcium deposits. They suggest that where reliable ultrasound is not available or inconclusive, then MRI of the shoulder is indicated and should be used in patients who are eligible for surgical repair of a rotator cuff tear to assess the degree of retraction and atrophied fatty infiltration. An MRI study with intra-articular contrast can be considered if any intra-articular abnormality or a partial rotator cuff injury has to be ruled out. It is preferable for a study in abduction and external rotation (ABER) to be part of an MR arthrography protocol. <ref name=":9" /> | ||
== Treatment/Management == | == Treatment/Management == | ||
The treatment depends on age, activity level and general health of the patient. The goal is to reduce pain and regain function. Conservative treatment is the first line of treatment, and should be considered for up to about a year until improvement and return to function are noticed.<ref>Rhon DI, Boyles RE, Cleland JA, Brown DL, A manual physical therapy approach versus subacromial corticosteroid injection for treatment of shoulder impingement syndrome: a protocol for a randomized clinical trial, BMJ Open 2011</ref> Surgery should only be considered if the patient does not respond to exhaustive non-operative treatment. <ref name=":9" /> | The treatment depends on age, activity level and general health of the patient. The goal is to reduce pain and regain function. Conservative treatment is the first line of treatment, and should be considered for up to about a year until improvement and return to function are noticed.<ref>Rhon DI, Boyles RE, Cleland JA, Brown DL, A manual physical therapy approach versus subacromial corticosteroid injection for treatment of shoulder impingement syndrome: a protocol for a randomized clinical trial, BMJ Open 2011</ref> Surgery should only be considered if the patient does not respond to exhaustive non-operative treatment. <ref name=":9" /> | ||
Conservative treatment consists of; relative rest, reduction of aggravating activities, in particular overhead activities, | Conservative treatment consists of; relative rest, reduction of aggravating activities, in particular overhead activities, NSAIDs to reduce pain and swelling, physical therapy management, and subacromial injection. Cortisone is often used because of its anti-inflammatory and pain-reducing effect, but this is controversial depending on the structure involved and should not be utilised in tendon related pain.<ref>AKGUN K, BIRTANE M., AKARIMAK U., Is local subacromial corticosteroïd injection beneficial in subacromial impingement syndrome?, Clin Rheumatol 2004, 23(6): 496-500</ref> | ||
There is no convincing evidence that surgical treatment is more effective than conservative treatment and surgery should only be considered when the conservative treatments fail to reduce the pain or restore function. Several surgical techniques are available, depending on the character and severity of the injury but no clear preference for surgical technique can be indicated currently.<ref name=":9" /><ref>http://orthoinfo.aaos.org/topic.cfm?topic=a00032</ref> | There is no convincing evidence that surgical treatment is more effective than conservative treatment and surgery should only be considered when the conservative treatments fail to reduce the pain or restore function. Several surgical techniques are available, depending on the character and severity of the injury but no clear preference for the surgical technique can be indicated currently.<ref name=":9" /><ref>http://orthoinfo.aaos.org/topic.cfm?topic=a00032</ref> | ||
* '''Surgical Repair''' of torn tissues, mostly of supraspinatus muscle, long head of biceps tendon or joint capsule. Note: a rotator cuff tear is not an indication for surgery. <ref name=":2" /> | * '''Surgical Repair''' of torn tissues, mostly of the supraspinatus muscle, long head of biceps tendon or joint capsule. Note: a rotator cuff tear is not an indication for surgery. <ref name=":2" /> | ||
* '''Bursectomy''' or removal of the subacromial bursa. | * '''Bursectomy''' or removal of the subacromial bursa. | ||
* '''Subacromial Decompression''' to increase the subacromial space by removing bony spurs or prominences on the underside of the os acromiale or the coracoacromial ligament | * '''Subacromial Decompression''' to increase the subacromial space by removing bony spurs or prominences on the underside of the os acromiale or the coracoacromial ligament | ||
| Line 123: | Line 215: | ||
== Physical Therapy Management == | == Physical Therapy Management == | ||
There is strong evidence that supervised non-operative rehabilitation decreases pain in the shoulder and increases function.<ref name="tate" /> Non-operative treatment should therefore be attempted first, assuming there is no tear that requires surgery. (Level of evidence 4) | There is strong evidence that supervised non-operative rehabilitation decreases pain in the shoulder and increases function.<ref name="tate" /> Non-operative treatment should, therefore, be attempted first, assuming there is no tear that requires surgery. (Level of evidence 4) | ||
Physical therapy management includes: | Physical therapy management includes: | ||
* RICE therapy in the acute phase to reduce pain and swelling | * RICE therapy in the acute phase to reduce pain and swelling | ||
* Stability and postural correction exercises | * Stability and postural correction exercises (forward head posture/kyphosis) | ||
* Mobility Exercises | * Mobility Exercises (cervical spine / thoracic spine / upper extremity in general / GH joint and scapular) | ||
* Strengthening | * Manual therapy of the cervical and / or thoracic spine (also thoracic cage) | ||
* Strengthening and Neuromuscular control exercises | |||
* Stretching exercises, including capsular stretching | * Stretching exercises, including capsular stretching | ||
* Manual therapy techniques of the shoulder | * Manual therapy techniques of the shoulder | ||
* Taping techniques (kinesiology taping or rigid scapular taping for example) | |||
* Acupuncture | * Acupuncture | ||
* Electrical stimulation | * Electrical stimulation | ||
| Line 139: | Line 233: | ||
* High-energy extracorporeal shockwave therapy (ESWT) is more effective than low-energy ESWT, ESWT is not recommended in the acute phase.<ref>Ron Diercks, Carel Bron, Oscar Dorrestijn, Carel Meskers, René Naber, Tjerk de Ruiter; Guideline for diagnosis and treatment of subacromial pain syndrome; Pages 314-322 | Received 23 Jan 2014, Accepted 04 Mar 2014, Published online: 21 May 2014;JournalActaOrthopaedica Volume 85, 2014 | * High-energy extracorporeal shockwave therapy (ESWT) is more effective than low-energy ESWT, ESWT is not recommended in the acute phase.<ref>Ron Diercks, Carel Bron, Oscar Dorrestijn, Carel Meskers, René Naber, Tjerk de Ruiter; Guideline for diagnosis and treatment of subacromial pain syndrome; Pages 314-322 | Received 23 Jan 2014, Accepted 04 Mar 2014, Published online: 21 May 2014;JournalActaOrthopaedica Volume 85, 2014 | ||
</ref>(Level of Evidence 2a) | </ref>(Level of Evidence 2a) | ||
When patient is presented with acute pain, it should be relieved first then | When the patient is presented with acute pain, it should be relieved first then strengthening / neuromuscular re-education exercises are implemented for the prevention of future injuries. Although exercise therapy alone has proved efficient, the addition of manual therapy ensures further increase in muscle strength.<ref>Bang MD, Deyle GD. Comparison of Supervised Exercise With and Without Manual Physical Therapy for Patients with Shoulder Impingement Syndrome. Journal of Orthopaedic and Sports Physical Therapy. 2000;30(3):126-137 (Level of evidence 1b)</ref> Exercise therapy is a vital part of treatment for subacromial impingement but results showed no significant difference between home-based exercises and clinical exercise. (Level of evidence 1b) | ||
Strengthening exercises should include<ref>Kuhn JE. Exercise in the treatment of rotator cuff impingement: A systematic review and synthesized evidence-based rehabilitation protocol. Journal fo Shoulder and Elbow Surgery. 2009;18:138-160 (Level of evidence 1a)</ref>: '''(Level of evidence 1a)''' | |||
* Rotator cuff strengthening such as; external rotation with thera-tubing (therabands). | |||
* Lower and middle trapezius strengthening such as; Press up, Unilateral scapular rotation | |||
* Bilateral shoulder external rotation. | |||
* Unilateral shoulder depression. | |||
* Strengthening of the lower part of the trapezius muscle is an important part of exercise therapy. Individuals with impingement syndrome show greater ratios of upper and lower trapezius activity than asymptomatic individuals.<ref name=":4">Smith M, Sparkes V, Busse M, Enright S. Upper and Lower trapezius muscle activity in subjects with subacromial impingement symptoms: Is there imbalance and can taping change it? Physical Therapy in Sport. 2009:10, 45-50 (Level of evidence 3b)</ref> '''(Level of evidence 3b)''' | |||
Muscles that will require specific attention and neuromuscular re-education generally include (but to be evaluated on an individual basis to have a tailored rehabilitation program): | |||
* Rotator cuff (particularly the external rotators - infraspinatus and teres minor) | |||
* Latissimus dorsi muscle | |||
* Serratus anterior | |||
* All aspects of the trapezius muscle (upper/middle/lower) | |||
* Pectoralis major and minor | |||
* A generalized and global approach for scapular muscles, to encourage proper performance and timing of scapular upward rotation, external rotation and posterior tilting during elevation. A recent study has found that interventions focusing on the scapular can improve short-term shoulder pain and function | |||
* Centralization of the humeral head within the glenoid fossa (primarily the rotator cuff muscles). | |||
* It is also prudent to look at the endurance of the deep neck flexors and thoracic extension muscles. | |||
A specific exercise strategy, focusing on strengthening eccentric exercises for the rotator cuff and concentric/eccentric exercises for the scapula stabilizers, is effective in reducing pain and improving shoulder function. <ref>Theresa Holmgren, Hanna Björnsson Hallgren, Birgitta Öberg, Lars Adolfsson, Kajsa Johansson; Effect of specific exercise strategy on need for surgery in patients with subacromial impingement syndrome: randomised controlled study; BMJ 2012; 344 (Published 20 February 2012)</ref> '''(Level of Evidence 1b)''' | |||
A specific exercise strategy, focusing on strengthening eccentric exercises for the rotator cuff and concentric/eccentric exercises for the scapula | |||
Soft tissue mobilization to normalize muscle spasm and other soft tissue dysfunction | Soft tissue mobilization to normalize muscle spasm and other soft tissue dysfunction have been shown to be effective alongside joint mobilizations to restore motion in the treatment of SAI.<ref name=":4" /> '''(Level of evidence 3b)''' | ||
A combination of physical therapy and surgical treatment | A combination of physical therapy and surgical treatment would give better clinical results than physical therapy alone.<ref>Stefanos Farfaras, Ninni Sernert, Lars Rostgard Christensen; Subacromial Decompression Yields a Better Clinical Outcome Than Therapy Alone: A Prospective Randomized Study of Patients With a Minimum 10-Year Follow-up; First Published March 15, 2018; The American Journal of Sports and Medicine | ||
</ref> (Level of Evidence 2b) | </ref> '''(Level of Evidence 2b)''' | ||
The motions of the rotator cuff that are emphasized for strengthening are internal rotation, external rotation and abduction. It is important to remember that the function of the rotator cuff, in addition to generating torque, is to stabilize the glenohumeral joint. Thus, stronger rotator cuff muscles result in better glenohumeral joint stabilization and less impingement. A typical initial exercise program involves the use of 4 to 8 weights, with 10 to 40 repetitions performed three to five times a week. | The motions of the rotator cuff that are emphasized for strengthening are internal rotation, external rotation and abduction. It is important to remember that the function of the rotator cuff, in addition to generating torque, is to stabilize the glenohumeral joint. Thus, stronger rotator cuff muscles result in better glenohumeral joint stabilization and less impingement. A typical initial exercise program involves the use of 4 to 8 weights, with 10 to 40 repetitions performed three to five times a week. A recent study explored the effectiveness of high intensity aerobic interval training rotator cuff exercise and found that it appears to be a potentially beneficial intervention in SAPS<ref>Berg OK, Paulsberg F, Brabant C, Arabsolghar K, Ronglan S, BjØrnsen N et al. High-Intensity Shoulder Abduction Exercise in Subacromial Pain Syndrome. Med Sci Sports Exerc. 2021;53(1):1-9. </ref> | ||
Patients with Stage II impingement may require a formal physical therapy | Patients with Stage II impingement may require a formal physical therapy programme. Isometric stretches are useful in restoring range of motion. Isotonic (fixed-weight) exercises are preferable to variable weight exercises. Thus, the shoulder exercises should be done with a fixed weight rather than a variable weight such as a rubber band. Repetitions are emphasized, and a relatively lightweight is used. Sometimes, sports-specific techniques are useful, particularly for strengthening the throwing motion, the serving motion or swimming motions. In addition, physical therapy modalities such as electrogalvanic stimulation, ultrasound treatment and transverse friction massages can be helpful.<ref>MORRISON D.S., FROGAMENI AD, WOODWORTH P., Non-operative treatment of subacromial impingement syndrome?, J Bone Joint Surg Am 1997. 79(5): 732 (Level of evidence 2b)</ref> '''(Level of evidence 2b)''' | ||
{{#ev:youtube|FkzYvxhgqQQ|300}} | {{#ev:youtube|FkzYvxhgqQQ|300}} | ||
{{#ev:youtube|9No0i7Wb2Rk|300}} | {{#ev:youtube|9No0i7Wb2Rk|300}} | ||
'''How do you manage GIRD (GH internal rotation deficit):''' | |||
* Sleep stretch (targeting the posterior capsule). | |||
* Cross-body ADDuction at various degrees of elevation (also targeting various portions of the posterior capsule), with or without posterior glides. | |||
* Infraspinatus/teres minor re-education (addressing imbalances, strength, neuromuscular control and muscular recruitment & en | |||
=== Clinical Bottom Line === | |||
* Impingement is not a diagnosis - it is a mechanism. | |||
* Reduction of the subacromial space - reflect on why is this occurring. | |||
** Bony factors (humeral head, acromion)? | |||
** Soft tissue factors (coracoacromial ligament, tight posterior capsule, lack of extensibility of internal rotators)? | |||
** Poor neuromuscular control factors (external rotators of the GH joint, rotator cuff muscles, scapular muscles and their strength, recruitment patterns and overall endurance)? | |||
* Control of the GH joint (instabilities). | |||
* Control of the scapula (overall neuromuscular control). | |||
* Reflect on the role of the entire upper extremity kinetic chain. | |||
* Mobility and contributions of the cervical spine, thoracic spine and thoracic cage mobility. | |||
* Non-surgical management of this shoulder classification is quite good, you only need to prescribe a minimum number of exercises (quality over quantity!) | |||
* To challenge the functional deficit of the patient, a minimum of a 12-week period is recommended. | |||
* Overall imaging is not regarded as useful unless the patient does not respond as expected, or you have the identification of Red Flags. | |||
* Steroid injections should not be considered as a first-line intervention unless pain is severe and preventing the engagement in rehabilitation or exercises. | |||
== Resources == | == Resources == | ||
{{#ev:youtube|Hv5YLrIGdn8|400}} <div class="row"><div class="col-md-6 col-md-offset-3"><div class="text-right"><ref>Sports Congress. Subacromial Pain Syndrome and Scapular Dyskinesia - Sports Medicine Congress 2016. Available from: https://www.youtube.com/watch?v=Hv5YLrIGdn8 [last accessed 30/10/17]</ref></div></div></div> | {{#ev:youtube|Hv5YLrIGdn8|400}} <div class="row"><div class="col-md-6 col-md-offset-3"><div class="text-right"><ref>Sports Congress. Subacromial Pain Syndrome and Scapular Dyskinesia - Sports Medicine Congress 2016. Available from: https://www.youtube.com/watch?v=Hv5YLrIGdn8 [last accessed 30/10/17]</ref></div></div></div> | ||
| Line 174: | Line 300: | ||
[[Category:Shoulder]] | [[Category:Shoulder]] | ||
[[Category:Conditions]] | [[Category:Conditions]] | ||
[[Category:Shoulder - Conditions]] | [[Category:Shoulder - Conditions]] | ||
[[Category:Sports Medicine]] | [[Category:Sports Medicine]] | ||
[[Category:Sports Injuries]] | [[Category:Sports Injuries]] | ||
[[Category:Older People/Geriatrics - Conditions]] | [[Category:Older People/Geriatrics - Conditions]] | ||
[[Category:Course Pages]] | |||
[[Category:Plus Content]] | |||
Latest revision as of 22:17, 7 December 2022
Original Editor - David Drinkard, Dorien De Strijcker
Top Contributors Dorien De Strijcker, Naomi O'Reilly, David Drinkard, Els Van Haver, Mariam Hashem, Admin, Kim Jackson, Rachael Lowe, Florence Brachotte, Amanda Ager, Kai A. Sigel, Tony Lowe, Scott Buxton, Tarina van der Stockt, Yuli Borremans, WikiSysop, Wendy Walker, Jess Bell, Robin Tacchetti, Lisa De Donder, Ewa Jaraczewska, Lucas Villalta, 127.0.0.1, Benjamin Desmedt, Tyler Shultz, Thaisa Van Bellingen, Wanda van Niekerk, Lauren Lopez and Lucinda hamptonIntroduction[edit | edit source]
This page addresses the condition known as the following:
- Subacromial impingement syndrome (SIS)
- Subacromial pain syndrome (SAPS)
- Rotator cuff related disorders
- Biomechanical impingement of the shoulder
There has been huge debate in relation to the diagnostic labelling of non-traumatic shoulder pain related to the structures of the subacromial space. The diagnostic label Subacromial Impingement Syndrome (SIS), presenting as anterograde-lateral shoulder pain when the arm is elevated, was first introduced in 1972 by Dr Charles Neer and was based on the mechanism of structural impingement of the structures of the subacromial space.[1][2][3] SIS has been viewed as symptomatic irritation of the subacromial structures between the coracoacromial arch and the humeral head during elevation of the arm above the shoulder/head [1] and as reflected by the literature is considered by many to be one of the most common causes of shoulder pain.
What is important to understand is that "impingement" on its own, is not a diagnosis, but rather simply describes the mechanism:
The compression of the rotator cuff against the anterior inferior aspect of the acromion and the coracoacromial ligament.
Neers Classification of Impingement identified four types of shoulder impingement identified below;
Neer Classification of Subacromial Impingement
According to Neer, impingement syndrome is divided into three stages:
Type I: <25 years old, Reversible, Swelling, Tendonitis, No Tears, Conservative Treatment.
- Moderate pain during exercise, no loss of strength and no limitation in movement. Edema and/or hemorrhage may be present. This stage generally occurs in patients less than 25 years of age and is frequently associated with an overuse injury. At this stage, the syndrome could be possibly reversible. [4]
Type II: 25-40 years old, Permanent Scarring, Tendonitis, No Tears, Subacromial Decompression
- Pain is usually reported during ADL and especially during the night. loss of mobility is associated with this stage. Type II is more advanced and tends to occur in patients between 25 to 40 years of age. The pathological changes show fibrosis as well as irreversible tendon changes.[4]
Type III: >40 years old, Small Rotator Cuff Tear, Subacromial Decompression with Debridement/Repair
Type IV: >40 years old, Large Rotator Cuff Tear, Sub Acromial Decompression with Repair
While Neers Classification of SIS was key to understanding shoulder pathology at the time, SIS was further broken down into four subtypes associated with either External Impingement (Primary or Secondary) and Internal Impingement.
External Impingement[edit | edit source]
- Primary External Impingement related to structural changes, either congenital or acquired, that mechanically narrow the subacromial space such as; bony narrowing or osteophyte formation, bony malposition after a fracture, or an increase in the volume of the subacromial soft tissues.[5][6][7][8][9][10][11][12][13][14][15] [16]The shape of the acromion process of the scapula or shoulder blade may play an important role in recovery and treatment from primary impingement.
- Secondary External Impingement related to abnormal scapulothoracic kinematics, strength balance alteration resulting in functional disturbance in the centering of the humeral head, leading to an abnormal displacement of the center of rotation when the arm is elevated. Generally caused by weakness of the Rotator Cuff Muscles (functional instability) combined with a glenohumeral joint capsule and ligaments that are to loose (micro-instability). Impingement generally occurs at the coracoacromial space secondary to anterior translation of the humeral head as opposed to the Subacromial space that is seen in primary impingement. Typically occurs in younger individuals with pain is located in the anterior or anterolateral aspect of the shoulder. The symptoms are usually activity-specific and involve overhand activities.[8][9][10][11][17][18][19][8][20][21]
Internal Impingement[edit | edit source]
- Internal Glenoid Impingement is probably the most common cause of posterior shoulder pain in the throwing or overhead athlete. Caused by impingement of the articular surface (intra-articular) of the Rotator Cuff (posterior edge of the supraspinatus and the anterior edge of the infraspinatus) against the posterior-superior-glenoid and glenoid labrum. Mainly seen with repetitive overhead activities, this positioning becomes pathologic during excessive external rotation, anterior capsular instability, scapular muscle imbalances[20], and/or upon repetitive overload of the rotator cuff musculature [21][17][18][19][8][20][21]. These deficiencies result in poor scapulohumeral control.
These definitions and descriptions of SIS are based on a hypothesis that acromial irritation leads to external abrasion of the bursa, rotator cuff or other structures within the subacromial space.[3] Throughout the years, the description progressed from SIS to ‘impingement related shoulder pain’, with the growing opinion that ‘impingement’ represents a cluster of symptoms and a possible mechanism for the pain, rather than a pathoanatomic diagnose itself. This remained the dominant theory for injury to structures within the subacromial space for the past 40 years and has been the rationale to guide clinical tests, conservative treatment, surgical procedures and rehabilitation protocols,[2] however the validity of this model of acromial impingement has been challenged from both a theoretical and practical perspective throughout the last decade, with suggestions that the use of SIS terminology can potentially contribute to negative expectations of physiotherapy and conservative treatment for patients, which may compromise outcome, often resulting in an increased incidence for surgery.[22][2][3][22]
While controversy surrounding the diagnostic labelling continues to exist, with many different terms in use to describe subacromial pain and it’s pathology in the literature it has been suggested that the label of SIS does not fully explain the mechanism. Many other diagnostic labels have been proposed but it has been suggested that the term Subacromial Pain Syndrome (SAPS) best describes the pain thought to originate from structures lying between the acromion and the humeral head, most often associated with some degree of shoulder dysfunction,[23] but does not reflect many other causes of shoulder pain located outside the subacromial space.
Bottom line:
- Subacromial impingement: Bursal side
- Internal impingement: Articular side
- Intrinsic mechanisms: Within the tendons
- Extrinsic mechanisms: External to the tendons.
Definition/Description[edit | edit source]
Subacromial Pain Syndrome is by defined Diercks et al [23] as all non-traumatic, usually unilateral, shoulder problems that cause pain, localized around the acromion, often worsening during or subsequent to lifting the arm. It is basically a generic term that encompasses pain associated with any lesion within a structure or structures within the Subacromial Space. As such the SAPS incorporates all conditions related to subacromial structures such as subacromial bursitis, calcific tendonitis, rotator cuff tendinopathy, rotator cuff tears, biceps tendinopathy, or tendon cuff degeneration as a result of the controversy regarding its pathogenesis.[23] [24]Subacromial pain syndrome is poorly understood despite being a commonly diagnoses.[25]
Clinically Relevant Anatomy[edit | edit source]
The Subacromial Space is the space beneath the acromion (between the acromion and the top surface of the humeral head). This space is outlined by the acromion and the coracoid process (which are parts of the scapula), and the coracoacromial ligament which connects the two. [26]
The Subacromial Space measures between 2 and 17 millimeters depending on the arm position and contains the following anatomical structures: [9][3][27]
- Coracoacromial Arch, composed of the Acromion, Coracoid Process and Coracoacromial Ligaments[7]
- Humeral Head
- Subacromial Bursa[28]
- Tendons of the Rotator Cuff; Supraspinatus, Infraspinatus, Teres Minor and Subscapularis
- Tendon of the Long Head of Biceps Brachii
- Coracoacromial ligament
- G-H Joint Capsule
Shoulder Biomechanics Review[edit | edit source]
It is important to remember that movements of the shoulder do not occur in isolation of the GH joint. During arm elevation, the following articulations/movements occur within the shoulder complex:
- Posterior roll and inferior glide of the humeral head.
- Posterior rotation of the clavicle: which will allow a functioning at the lateral end of the clavicle during elevation and posterior rotation, raising the acromion and help maintain the subacromial space.
- External rotation of the scapular: which means the medial border of the scapula moves towards the thoracic spine and chest wall. As your humerus laterally rotates, the scapular follows that into lateral rotation.
- A scapular posterior tilt towards the end of elevation (the inferior angle of the scapula will move towards the chest wall).
- Also an upward rotation of the scapular: the movement of the inferior angle of the scapula from the thoracic spine.
It is generally the upward rotation of the scapula which keeps the acromion high; maintaining that acromio-humeral distance and reducing the possibility of impinging of the structures within the subacromial space. The upward rotation movement is generally carried out with the recruitment of the different sections of the trapezius muscle (upper / middle / lower). It is also this movement (upward rotation) which allows the glenoid fossa to follow the humeral head, to maintain a congruency during arm elevation.
Scapulohumeral Rhythm: Ratio of the GH movement to the scapulothoracic movement during arm elevation. Overall the value is 2:1; meaning for every 1 degree of scapular rotation, we see 2 degrees of humeral elevation - for example, a 180-degree range of motion for elevation, we'll see 60 degrees of scapular upward rotation with 120 degrees of humeral abduction. However, the ratio is not consistent across an entire arc of shoulder elevation.
The importance of external rotation of the humerus during elevation:[edit | edit source]
During arm elevation, normally there is an external (lateral) rotation of the humerus. If the timing of the movement is correct, this external rotation of the humerus during elevation permits the avoidance of the compression of the greater tuberosity against the subacromial structures. If the timing is not right (poor neuromuscular recruitment, internal rotation of the humerus or dysfunctional biomechanics of the shoulder complex), the necessary external rotation will not occur and the greater tuberosity will internally compress the structures and cause an irritation of the tissues.
See the Physiopedia page on Shoulder Biomechanics, for further information.
Prevalence/Incidence[edit | edit source]
SAPS is the most common disorder of the shoulder[29], accounting for anywhere between 44% to 65% of all complaints of shoulder pain, [30] with the incidence increasing with age.[31] Peak incidence occurs during the sixth decade of life.[32]
Etiology[edit | edit source]
There remains a debate in regards to the etiology of subacromial pain, but it is proposed that the mechanisms include intrinsic, extrinsic and combined factors including muscle imbalance and anatomical factors that may affect the subacromial space; variations in the acromial shape; the anterior slope; the angle of the acromion; and the lateral extension of the acromion over the humeral head. Osseous changes of the inferior acromioclavicular joint or the coracoacromial ligament may also affect the subacromial space. [24]
While it is accepted that multiple factors are involved in the pathology, several unresolved issues remain such as: which subacromial structure is first engaged by pathology, and what are the pain-generating mechanisms? [24]
Contributing Factors[edit | edit source]
There are both intrinsic and extrinsic factors which could predispose a person from experiencing a reduction in subacromial space during arm elevation.
Intrinsic factors: (generally non-modifiable)
- Tendon histology (quality of the tendons)
- Age
- Genetics
Extrinsic factors: (potentially modifiable)
- Muscle extensibility / performance
- Anatomical/osseous
- GH joint kinematics
- Posture/ergonomics
Different types of impingement[edit | edit source]
Subacromial extra-articular impingement: Bursal. Compression caused as a result of a decreased in subacromial (AHD) space. Pain is generally located over the anterior aspect of the shoulder with elevation.
Internal impingement: Articular. Caused by contact between the articular side of the supra/infraspinatus and the posterosuperior rim of the glenoid. Pain is located posteriorly "inside" the joint when in a ABER (throwing) position.
Subcoracoid impingement: A history of dull pain in the anterior aspect of the shoulder. Exacerbated by the shoulder in forward flexion, ADDuction and internal (medial) rotation (such as the motion of hitting the ball with a racket).
Impingement Mechanisms[edit | edit source]
There are 3 main mechanisms that can affect the distance/space of the subacromial space (acromio-humeral distance)
- Loss of control of the humeral head (GH instabilities)
- Loss of scapular control (scapular instabilities)
- Change to the actual size of structures within the space (tendons of the RC muscles, subacromial bursae, for example).
Intrinsic Mechanisms: What can affect the size of the content of the subacromial space?
The load on the tendon (shear or compressive forces). Tendon "overload" due to excessive or repetitive forces on the tendons. This can cause reactive tendinopathy or a tendon dysrepair (causing a painful response to movement). Keep in mind that changes to the tendons are normal depending on activity levels and age.
Clinical Presentation[edit | edit source]
The affected patients are generally over age 40 and suffer from persistent pain without any known preceding trauma.[33] Patients report pain on elevating the arm between 70 ° and 120 °, the “Painful Arc” (Figure 3), on forced movement above the head, and when lying on the affected side.[17] The symptoms may be acute or chronic. Most often it is a gradual, degenerative condition that causes "impingement", rather than due to a strong external force. Therefore, patients often have difficulties with determining the exact onset of symptoms.
In recent studies, there has been a great deal of talk about GIRD (Glenohumeral Internal Rotation Deficit), which can be understood as a loss of internal (medial) rotation range of motion, in the presence of a loss of total rotational motion (evaluation of the total range of motion, of both shoulders).
GIRD = (side-to-side difference in ER) + (side-to-side difference in IR)
A contributing factor to GIRD has been theorized to be the thickening of the posterior GH capsule, limiting the overall range of internal rotation of the GH joint.
Differential Diagnosis[edit | edit source]
There are a variety of shoulder conditions that can initially be confused with subacromial pain syndrome [34]. A thorough physical examination should exclude other conditions such as [35]:
- Rotator Cuff Tears (Partial / Full)
- Thoracic Outlet Syndrome (TOS)
- Cervical Spondylosis
- Subluxating Shoulder
- SLAP or labral lesions
- Acromioclavicular Joint Disorders
- Adhesive Capsulitis (Frozen Shoulder)
- Glenohumeral Arthritis
- Paralysis of the Trapezius
- Calcific Tendinopathy
- Subacromial Bursitis
- Arthropathy
- Glenohumeral Instability
- Cervical radicular pain or referred cervical facet pain
- Nerve Palsy
Physical Examination[edit | edit source]
Detailed History and clinical examination are necessary for the diagnosis of SAPS. No single test alone is accurate to diagnose SAPS or sufficiently differentiate between various shoulder disorders [36][37], but using a combination of specific tests increases the post-test probability of the diagnosis of SAPS. [38][39][40][41]
The Dutch Orthopaedic Association Guidelines [23] for diagnosis and treatment of subacromial pain syndrome recommend a combination of the following tests (pain provocation tests) to aid in the diagnosis;
The combination of the Hawkins-Kennedy Test, the Painful Arc and the Infraspinatus Resistance Test have a considerably higher predictive value;[23][42]
- 3 tests are positive: the probability that the patient has SAPS is (10,56) [42]
- 2 tests are positive: the probability that the patient has SAPS is (5,03) [42]
- 1 test is positive: the probability that the patient has SAPS is (0,90) [42]
- 0 tests are positive: the probability that the patient has SAPS is (0,17) [42]
The following additional test should also be used to rule out a Rotator Cuff Tear;
- Drop Arm Test: To test the integrity of the Supraspinatus. [43]
There is also the Neer Impingement Test, which evaluates a subacromial impingement specifically, while the Hawkins-Kennedy Test evaluates the presence of a coracoacromial impingement.
Considerations for poor neuromuscular control of the scapula (to consider and objectively evaluate, when possible):
- Loss of dynamic stability of the scapula
- Pectoralis minor length and flexibility
- Scapular muscle performance and endurance
- Thoracic spine function/mobility
- Range of motion of GH joint (tightness of joint capsule, or even a GH instability)
- Rotator cuff muscle balance (agonist/antagonist / synergistic muscle activity), performance and muscular endurance.
Other considerations:
- Capsular tightness: Specific assessment of the posterior capsule, potentially limiting the range of motion in internal rotation (GIRD).
- Lack of extensibility of external rotator muscles (infraspinatus/teres minor).
- Lack of muscular strength, neuromuscular control or endurance of external rotators (infraspinatus/teres minor).
- Lack of extensibility of internal rotators (lattissimus dorsi and pectoralis minor for example).
- Contributions of the serratus anterior muscle to the movement of the scapula (upward rotation, posterior tilt, external rotation and protraction of the scapula) during elevation.
- Thoracic spine and rib cage mobility. A healthy spine and rib cage movement will not impede any movements of the shoulder or scapular complex during upper extremity movements.
Diagnostic Procedures[edit | edit source]
Overall considerations
There are anatomical factors which may influence the narrowing of the subacromial space, such as:
- The presence of a subacromial bone spur (potential thickening or calcification of the coracoacromial ligament)
- The shape of the acromion (type I (flat) / type II (curved)/ type III (hook)/ type IV (upward oriented acromion))
- AC joint arthrosis (degeneration of surrounding tissues)
- Instability of the humeral head (of the GH joint)
Radiographs may be used to detect anatomical variants, calcific deposits or acromioclavicular joint arthritis. The three recommended views are:[44]
- Antero-posterior View with the arm at 30 degrees external rotation which is useful for assessing the glenohumeral joint, subacromial osteophytes and sclerosis of the greater tuberosity.
- Outlet Y View is useful because it shows the subacromial space and can differentiate the acromial processes.
- Axillary View is helpful in visualizing the acromion and the process coracoid, as well as coracoacromial ligament calcifications.
The size of the subacromial space can also be measured. MRI can show full or partial tears in the tendons of the rotator cuff, and inflammation to weak structures. Ultrasound and arthrography are being used when rotator cuff tears are suspected or in complex cases.[4]
There is a good clinical-radiological association between subacromial pain syndrome and findings on ultrasound.[45] The diagnostic accuracy of ultrasound is considered good and comparable to that of conventional MRI for identification and quantification of complete (full-thickness) rotator cuff injuries. The sensitivity and specificity of ultrasound and conventional MRI are not significantly different in the detection of partial- or full-thickness rotator cuff tears with MR Arthrography an accurate method to rule out partial rotator cuff injuries.[23]
The Dutch Orthopaedic Association Guidelines arise the use of ultrasounds the most valuable and cost-effective diagnostic imaging if the first period of conservative treatment fails, which they recommend can be combined with conventional radiography of the shoulder to determine osteoarthritis, osseous abnormalities, and presence/absence of calcium deposits. They suggest that where reliable ultrasound is not available or inconclusive, then MRI of the shoulder is indicated and should be used in patients who are eligible for surgical repair of a rotator cuff tear to assess the degree of retraction and atrophied fatty infiltration. An MRI study with intra-articular contrast can be considered if any intra-articular abnormality or a partial rotator cuff injury has to be ruled out. It is preferable for a study in abduction and external rotation (ABER) to be part of an MR arthrography protocol. [23]
Treatment/Management[edit | edit source]
The treatment depends on age, activity level and general health of the patient. The goal is to reduce pain and regain function. Conservative treatment is the first line of treatment, and should be considered for up to about a year until improvement and return to function are noticed.[46] Surgery should only be considered if the patient does not respond to exhaustive non-operative treatment. [23]
Conservative treatment consists of; relative rest, reduction of aggravating activities, in particular overhead activities, NSAIDs to reduce pain and swelling, physical therapy management, and subacromial injection. Cortisone is often used because of its anti-inflammatory and pain-reducing effect, but this is controversial depending on the structure involved and should not be utilised in tendon related pain.[47]
There is no convincing evidence that surgical treatment is more effective than conservative treatment and surgery should only be considered when the conservative treatments fail to reduce the pain or restore function. Several surgical techniques are available, depending on the character and severity of the injury but no clear preference for the surgical technique can be indicated currently.[23][48]
- Surgical Repair of torn tissues, mostly of the supraspinatus muscle, long head of biceps tendon or joint capsule. Note: a rotator cuff tear is not an indication for surgery. [34]
- Bursectomy or removal of the subacromial bursa.
- Subacromial Decompression to increase the subacromial space by removing bony spurs or prominences on the underside of the os acromiale or the coracoacromial ligament
- Acromioplasty to increase the subacromial space by removing a part of the acromion. Arthroscopic acromioplasty is less invasive and requires lesser rehabilitation than the open (Neer) acromioplasty.
No difference in outcome (shoulder function, complications) has currently been shown between an arthroscopic approach and an open approach, with a bursectomy likely to give the same clinical outcome as a bursectomy with acromioplasty.[23]
Physical Therapy Management[edit | edit source]
There is strong evidence that supervised non-operative rehabilitation decreases pain in the shoulder and increases function.[28] Non-operative treatment should, therefore, be attempted first, assuming there is no tear that requires surgery. (Level of evidence 4)
Physical therapy management includes:
- RICE therapy in the acute phase to reduce pain and swelling
- Stability and postural correction exercises (forward head posture/kyphosis)
- Mobility Exercises (cervical spine / thoracic spine / upper extremity in general / GH joint and scapular)
- Manual therapy of the cervical and / or thoracic spine (also thoracic cage)
- Strengthening and Neuromuscular control exercises
- Stretching exercises, including capsular stretching
- Manual therapy techniques of the shoulder
- Taping techniques (kinesiology taping or rigid scapular taping for example)
- Acupuncture
- Electrical stimulation
- Ultrasound and musculoskeletal ultrasound
- Low-level laser therapy has positive effects on all symptoms except on muscle strength[51] (Level of evidence 1b)
- Corticosteroid injections, in the first 8 weeks
- High-energy extracorporeal shockwave therapy (ESWT) is more effective than low-energy ESWT, ESWT is not recommended in the acute phase.[52](Level of Evidence 2a)
When the patient is presented with acute pain, it should be relieved first then strengthening / neuromuscular re-education exercises are implemented for the prevention of future injuries. Although exercise therapy alone has proved efficient, the addition of manual therapy ensures further increase in muscle strength.[53] Exercise therapy is a vital part of treatment for subacromial impingement but results showed no significant difference between home-based exercises and clinical exercise. (Level of evidence 1b)
Strengthening exercises should include[54]: (Level of evidence 1a)
- Rotator cuff strengthening such as; external rotation with thera-tubing (therabands).
- Lower and middle trapezius strengthening such as; Press up, Unilateral scapular rotation
- Bilateral shoulder external rotation.
- Unilateral shoulder depression.
- Strengthening of the lower part of the trapezius muscle is an important part of exercise therapy. Individuals with impingement syndrome show greater ratios of upper and lower trapezius activity than asymptomatic individuals.[55] (Level of evidence 3b)
Muscles that will require specific attention and neuromuscular re-education generally include (but to be evaluated on an individual basis to have a tailored rehabilitation program):
- Rotator cuff (particularly the external rotators - infraspinatus and teres minor)
- Latissimus dorsi muscle
- Serratus anterior
- All aspects of the trapezius muscle (upper/middle/lower)
- Pectoralis major and minor
- A generalized and global approach for scapular muscles, to encourage proper performance and timing of scapular upward rotation, external rotation and posterior tilting during elevation. A recent study has found that interventions focusing on the scapular can improve short-term shoulder pain and function
- Centralization of the humeral head within the glenoid fossa (primarily the rotator cuff muscles).
- It is also prudent to look at the endurance of the deep neck flexors and thoracic extension muscles.
A specific exercise strategy, focusing on strengthening eccentric exercises for the rotator cuff and concentric/eccentric exercises for the scapula stabilizers, is effective in reducing pain and improving shoulder function. [56] (Level of Evidence 1b)
Soft tissue mobilization to normalize muscle spasm and other soft tissue dysfunction have been shown to be effective alongside joint mobilizations to restore motion in the treatment of SAI.[55] (Level of evidence 3b)
A combination of physical therapy and surgical treatment would give better clinical results than physical therapy alone.[57] (Level of Evidence 2b)
The motions of the rotator cuff that are emphasized for strengthening are internal rotation, external rotation and abduction. It is important to remember that the function of the rotator cuff, in addition to generating torque, is to stabilize the glenohumeral joint. Thus, stronger rotator cuff muscles result in better glenohumeral joint stabilization and less impingement. A typical initial exercise program involves the use of 4 to 8 weights, with 10 to 40 repetitions performed three to five times a week. A recent study explored the effectiveness of high intensity aerobic interval training rotator cuff exercise and found that it appears to be a potentially beneficial intervention in SAPS[58]
Patients with Stage II impingement may require a formal physical therapy programme. Isometric stretches are useful in restoring range of motion. Isotonic (fixed-weight) exercises are preferable to variable weight exercises. Thus, the shoulder exercises should be done with a fixed weight rather than a variable weight such as a rubber band. Repetitions are emphasized, and a relatively lightweight is used. Sometimes, sports-specific techniques are useful, particularly for strengthening the throwing motion, the serving motion or swimming motions. In addition, physical therapy modalities such as electrogalvanic stimulation, ultrasound treatment and transverse friction massages can be helpful.[59] (Level of evidence 2b)
How do you manage GIRD (GH internal rotation deficit):
- Sleep stretch (targeting the posterior capsule).
- Cross-body ADDuction at various degrees of elevation (also targeting various portions of the posterior capsule), with or without posterior glides.
- Infraspinatus/teres minor re-education (addressing imbalances, strength, neuromuscular control and muscular recruitment & en
Clinical Bottom Line[edit | edit source]
- Impingement is not a diagnosis - it is a mechanism.
- Reduction of the subacromial space - reflect on why is this occurring.
- Bony factors (humeral head, acromion)?
- Soft tissue factors (coracoacromial ligament, tight posterior capsule, lack of extensibility of internal rotators)?
- Poor neuromuscular control factors (external rotators of the GH joint, rotator cuff muscles, scapular muscles and their strength, recruitment patterns and overall endurance)?
- Control of the GH joint (instabilities).
- Control of the scapula (overall neuromuscular control).
- Reflect on the role of the entire upper extremity kinetic chain.
- Mobility and contributions of the cervical spine, thoracic spine and thoracic cage mobility.
- Non-surgical management of this shoulder classification is quite good, you only need to prescribe a minimum number of exercises (quality over quantity!)
- To challenge the functional deficit of the patient, a minimum of a 12-week period is recommended.
- Overall imaging is not regarded as useful unless the patient does not respond as expected, or you have the identification of Red Flags.
- Steroid injections should not be considered as a first-line intervention unless pain is severe and preventing the engagement in rehabilitation or exercises.
Resources[edit | edit source]
References[edit | edit source]
- ↑ 1.0 1.1 de Witte PB Nagels J van Arkel ER, et al. Study protocol subacromial impingement syndrome: the identification of pathophysiologic mechanisms (SISTIM). BMC Musculoskelet Disord. 2011; 12:1-12.
- ↑ 2.0 2.1 2.2 Cools AM, Michener LA. Shoulder Pain: Can One Label Satisfy Everyone and Everything? Br J Sports Med. 2017 Feb 16;51(5):416–7.
- ↑ 3.0 3.1 3.2 3.3 Lewis J. Subacromial Impingement Syndrome: A Musculoskeletal Condition or a Clinical Illusion? Physical Therapy Reviews 2011;16:388-298.
- ↑ 4.0 4.1 4.2 KHAN Y, NAGY MT, MALAL J, WASEEM M, The painful shoulder: shoulder impingement syndrome. Open Orthop J Sept 2013, 6(7): 347-51
- ↑ Neer CS. Anterior acromioplasty for the chronic impingement syndrome in the shoulder: A preliminary report. J Bone Joint Surg Am. 1972;54:41–50.
- ↑ Leroux J-L, Codine P, Thomas E, Pocholle M, Mailhe D, Blotman F. Isokinetic evaluation of rotational strength in normal shoulders and shoulders with impingement syndrome. Clin Orthop. 1994;304:108–115
- ↑ 7.0 7.1 KATCHINGWE AF, Phillips B, Sletten E, Plunkett SW., Comparison of Manual Therapy Techniques with Therapeutic Exercise in the Treatment of Shoulder Impingement: A Randomized Controlled Pilot Clinical Trial. The Journal of Manual Manipulative Therapy 2008;16(4): p238-¬‐247
- ↑ 8.0 8.1 8.2 8.3 Bigliani LU, Levine WN. Current concepts review: Subacromial impingement syndrome. J Bone Joint Surg Am. 1997;79:1854–1868.
- ↑ 9.0 9.1 9.2 Harryman DT, Sidles JA, Clark JM, McQuade KJ, Gibb TD, Matsen FA. Translation of the humeral head on the glenoid with passive glenohumeral motion. J Bone Joint Surg Am. 1990;72-a:1334–1343.
- ↑ 10.0 10.1 Morrison DS, Greenbaum BS, Einhorn A. Shoulder impingement. Orthop Clin North Am. 2000;31:285–293
- ↑ 11.0 11.1 Nicholson GP, Goodman DA, Flatow EL, Bigliani LU. The acromion: Morphologic condition and age-related changes. A study of 420 scapulas. J Shoulder Elbow Surg. 1996;5:1–11.
- ↑ Lewis JS, Wright C, Green A. Subacromial impingement syndrome: The effect of changing posture on shoulder range of movement. J Orthop Sports Phys Ther. 2005;35:72–87.
- ↑ DE BIE R.A., BASTIANENEN C.H.G. Effectiveness of individualized physiotherapy on pain and functioning compared to a standard exercise protocol in patients presenting with clinical signs of subacromial impingement syndrome. A randomized controlled trial. BMC Musculoskeletal Disorders. 2010 Jun 9; 11:114.Level of evicence: 1B
- ↑ Phil Page, PhD, PT, ATC, LAT, CSCS, FACSM, Shoulder Muscle Imbalance and Subacromial Impingement Syndrome in Overhead Athletes, Int J Sport Phys. Ther., 2011
- ↑ http://www.sbcoachescollege.com/articles/UpperCrossSyndromeShPain.html
- ↑ Creech JA, Silver S. Shoulder impingement syndrome. InStatPearls [Internet] 2021 Jul 26. StatPearls Publishing.
- ↑ 17.0 17.1 17.2 Urwin M, Symmons D, Allison T, et al.: Estimating the burden of musculoskeletal disorders in the community: the comparative prevalence of symptoms at different anatomical sites, and the relation to social deprivation. Ann Rheum Dis 1998; 57: 649–55.
- ↑ 18.0 18.1 McClure PW, Michener LA, Karduna AR. Shoulder function and 3-dimensional scapular kinematics in people with and without shoulder impingement syndrome. Phys Ther. 2006;86:1075–1090.
- ↑ 19.0 19.1 Belling Sorensen AK, Jorgensen U. Secondary impingement in the shoulder. Scand J Med Sci Sports. 2000;10:266–278.
- ↑ 20.0 20.1 20.2 Lukasiewicz AC, McClure P, Michener L, Pratt N, Sennett B. Comparison of 3-dimensional scapular position and orientation between subjects with and without shoulder impingement. J Orthop Sports Phys Ther. 1999;29:574–583.
- ↑ 21.0 21.1 21.2 Belling Sorensen AK, Jorgensen U. Secondary impingement in the shoulder. Scand J Med Sci Sports. 2000;10:266–278.
- ↑ 22.0 22.1 Cuff A, Littlewood C. Subacromial Impingement Syndrome - What does this mean to and for the Patient? A Qualitative Study. Musculoskeletal Science and Practice. Elsevier Ltd; 2017 Oct 17;:1–14.
- ↑ 23.0 23.1 23.2 23.3 23.4 23.5 23.6 23.7 23.8 23.9 Diercks R, Bron C, Dorrestijn O, Meskers C, Naber R, de Ruiter T, et al. Guideline for Diagnosis and Treatment of Subacromial Pain Syndrome. Acta Orthopaedica. 2014 May 21;85(3):314–22.
- ↑ 24.0 24.1 24.2 Björnsson Hallgren H. Treatment of Subacromial Pain and Rotator Cuff Tears [dissertation]. Linköping University Sweden. 2012.
- ↑ Dhillon KS. Subacromial impingement syndrome of the shoulder: a musculoskeletal disorder or a medical myth?. Malaysian orthopaedic journal. 2019 Nov;13(3):1.
- ↑ http://www.jointsurgery.in/shoulder-arthoscopy/anatomy-of-shoulder/
- ↑ Lewis J, McCreesh K, Roy JS, Ginn K. Rotator cuff tendinopathy: navigating the diagnosis-management conundrum. journal of orthopaedic & sports physical therapy. 2015 Nov;45(11):923-37.
- ↑ 28.0 28.1 Tate A.R., McClure P.W., Young I.A., Salvator R., Michener L.A., Comprehensive Impairment-based Exercise and Manual Therapy Intervention for Patients with Subacromial Impingement Syndrome: A Case Series. The Journal of Orthopaedic and Sports Physical Therapy 2010; 40(8): p474-93 (Level of evidence 4)
- ↑ Park SW, Chen YT, Thompson L, Kjoenoe A, Juul-Kristensen B, Cavalheri V, McKenna L. No relationship between the acromiohumeral distance and pain in adults with subacromial pain syndrome: a systematic review and meta-analysis. Scientific Reports. 2020 Nov 26;10(1):1-4.
- ↑ Bhattacharyya R, Edwards K, Wallace AW. Does arthroscopic sub-acromial decompression really work for sub-acromial impingement syndrome: a cohort study. BMC Musculoskelet Disord. 2014;15:1.
- ↑ Randelli P, Randelli F, Ragone V, et al. Regenerative medicine in rotator cuff injuries. BioMed Res Int. 2014;2014:129515
- ↑ Ostor AJ, Richards CA, Prevost AT, Speed CA, Hazleman BL: Diagnosis and relation to general health of shoulder disorders presenting to primary care. Rheumatology (Oxford) 2005; 44: 800–5.
- ↑ Garving, C., Jakob, S., Bauer, I., Nadjar, R., & Brunner, U. H. (2017). Impingement Syndrome of the Shoulder, Dtsch Arztebl. 765–777. https://doi.org/10.3238/arztebl.2017.0765
- ↑ 34.0 34.1 Fongemie AE, Buss DD, Rolnick SJ. Management of shoulder impingement syndrome and rotator cuff tears. American family physician. 1998 Feb 15;57(4):667.
- ↑ Lockhart RD. Movements of the Normal Shoulder Joint and of a case with Trapezius Paralysis studied by Radiogram and Experiment in the Living. J Anat 1930; 64: 288-302
- ↑ Hegedus EJ, Goode A, Campbell S, Morin A, Tamaddoni M, Moorman CT, Cook C. Physical Examination Tests of the Shoulder: A Systematic Review with Meta-analysis of Individual Tests. British Journal of Sports Medicine. 2007 Aug 24.
- ↑ Hughes PC, Taylor NF, Green RA. Most Clinical Tests Cannot Accurately Diagnose Rotator Cuff Pathology: A Systematic Review . Aust J Physiother. 2008;54(3):159–70.
- ↑ Murrell GA, Walton JR. Diagnosis of Rotator Cuff Tears. The Lancet. 2001 Mar 10;357(9258):769-70.
- ↑ Park HB, Yokota A, Gill HS, El Rassi G, McFarland EG. Diagnostic Accuracy of Clinical Tests for the Different Degrees of Subacromial Impingement Syndrome. JBJS. 2005 Jul 1;87(7):1446-55.
- ↑ Michener LA, Walsworth MK, Doukas WC, Murphy KP. Reliability and Diagnostic Accuracy of 5 Physical Examination Tests and Combination of Tests for Subacromial Impingement. Archives of Physical Medicine and Rehabilitation. 2009 Nov 1;90(11):1898-903.
- ↑ MICHENER L.A., WALSWORTH M.K., DOUKAS W.C., MURPHY K.P. Reliability and Diagnostic Accuracy of 5 Physical Examination Tests and Combination of Tests for Subacromial Impingement. Archives of Physical Medicine and Rehabilitation. 2009 Nov; 90(11): 1898-903. Level of evicence: 1C
- ↑ 42.0 42.1 42.2 42.3 42.4 Park HB, Yokota A, Gill HS, El Rassi G, McFarland EG. Diagnostic Accuracy of Clinical Tests for the Different Degrees of Subacromial Impingement Syndrome. JBJS. 2005 Jul 1;87(7):1446-55. Level of Evidence 1
- ↑ ALGUNAEE M, GALVIN R, FAHEY T, Diagnostic accuracy of clinical tests for subacromial impingement syndrome: a systematic review and meta-analysis. Ach Phys Med Rehabil 2012, 93(2): 229-36
- ↑ Smith M, Sparkes V, Busse M, Enright S. Upper and Lower trapezius muscle activity in subjects with subacromial impingement symptoms: Is there imbalance and can taping change it? Physical Therapy in Sport. 2009:10, 45-50
- ↑ Rodríguez-Piñero Durán M, Vidal Vargas V, Castro Agudo M. Hallazgos ecográficos en el síndrome de dolor subacromial crónico [Ultrasound findings in chronic subacromal pain syndrome]. Rehabilitacion (Madr). 2019;53(4):240-6.
- ↑ Rhon DI, Boyles RE, Cleland JA, Brown DL, A manual physical therapy approach versus subacromial corticosteroid injection for treatment of shoulder impingement syndrome: a protocol for a randomized clinical trial, BMJ Open 2011
- ↑ AKGUN K, BIRTANE M., AKARIMAK U., Is local subacromial corticosteroïd injection beneficial in subacromial impingement syndrome?, Clin Rheumatol 2004, 23(6): 496-500
- ↑ http://orthoinfo.aaos.org/topic.cfm?topic=a00032
- ↑ Arthroscopic subacromial decompression - Dr Terry Hammond.dv Available from:https://www.youtube.com/watch?v=YLdjvpxXgnU
- ↑ Shoulder Arthroscopic Subacromial Decompression - Dr. Tony Jabbour Available from:https://www.youtube.com/watch?v=sLd9yBiK3RA
- ↑ YELDAN I., CETIN E., OZDINCLER A.R. The effectiveness of low-level laser therapy on shoulder function in subacromial impingement syndrome. Disability and rehabilitation. 2009; 31(11): 935–940 (Level of evidence 1b)
- ↑ Ron Diercks, Carel Bron, Oscar Dorrestijn, Carel Meskers, René Naber, Tjerk de Ruiter; Guideline for diagnosis and treatment of subacromial pain syndrome; Pages 314-322 | Received 23 Jan 2014, Accepted 04 Mar 2014, Published online: 21 May 2014;JournalActaOrthopaedica Volume 85, 2014
- ↑ Bang MD, Deyle GD. Comparison of Supervised Exercise With and Without Manual Physical Therapy for Patients with Shoulder Impingement Syndrome. Journal of Orthopaedic and Sports Physical Therapy. 2000;30(3):126-137 (Level of evidence 1b)
- ↑ Kuhn JE. Exercise in the treatment of rotator cuff impingement: A systematic review and synthesized evidence-based rehabilitation protocol. Journal fo Shoulder and Elbow Surgery. 2009;18:138-160 (Level of evidence 1a)
- ↑ 55.0 55.1 Smith M, Sparkes V, Busse M, Enright S. Upper and Lower trapezius muscle activity in subjects with subacromial impingement symptoms: Is there imbalance and can taping change it? Physical Therapy in Sport. 2009:10, 45-50 (Level of evidence 3b)
- ↑ Theresa Holmgren, Hanna Björnsson Hallgren, Birgitta Öberg, Lars Adolfsson, Kajsa Johansson; Effect of specific exercise strategy on need for surgery in patients with subacromial impingement syndrome: randomised controlled study; BMJ 2012; 344 (Published 20 February 2012)
- ↑ Stefanos Farfaras, Ninni Sernert, Lars Rostgard Christensen; Subacromial Decompression Yields a Better Clinical Outcome Than Therapy Alone: A Prospective Randomized Study of Patients With a Minimum 10-Year Follow-up; First Published March 15, 2018; The American Journal of Sports and Medicine
- ↑ Berg OK, Paulsberg F, Brabant C, Arabsolghar K, Ronglan S, BjØrnsen N et al. High-Intensity Shoulder Abduction Exercise in Subacromial Pain Syndrome. Med Sci Sports Exerc. 2021;53(1):1-9.
- ↑ MORRISON D.S., FROGAMENI AD, WOODWORTH P., Non-operative treatment of subacromial impingement syndrome?, J Bone Joint Surg Am 1997. 79(5): 732 (Level of evidence 2b)
- ↑ Sports Congress. Subacromial Pain Syndrome and Scapular Dyskinesia - Sports Medicine Congress 2016. Available from: https://www.youtube.com/watch?v=Hv5YLrIGdn8 [last accessed 30/10/17]