Shoulder Dislocation
Top Contributors - Sherin Mathew, Johnathan Fahrner, Haley Stevenson, Lucinda hampton, Admin, Rachael Lowe, Kim Jackson, Scott A Burns, Naomi O'Reilly, Venus Pagare, Wanda van Niekerk, Khloud Shreif, Sai Kripa, Evan Thomas, WikiSysop, Fasuba Ayobami, Candace Goh and Claire Knott
Introduction[edit | edit source]
Shoulder dislocation (correctly termed a glenohumeral joint dislocation) involves separation of the humerus from the glenoid of the scapula at the glenohumeral joint. The shoulder is inherently unstable joint due to the shallow glenoid articulating with a small part of the humeral head. [1]
- This type of dislocation represent 50 percent of all major joint dislocations being the most regularly dislocated joint in the body.
- The shoulder can dislocate in an anterior (95% of shoulder dislocations), posterior, inferior direction and completely or partially.
- Fibrous tissue joining the bones is often stretched or torn, complicating a dislocation.[1][2]
Etiology[edit | edit source]
Extreme rotation can cause the humeral head to come out of the glenoid labrum. Contact sports injuries are a common cause a dislocated shoulder as are motor trauma and falls.[1]
Epidemiology[edit | edit source]
Anterior locations represent 95% of shoulder dislocation.[2]
Risk factors for redislocation;
- Proir dislocation with poor tissue does not healing or soft issue laxity
- Younger patients have a much higher frequency of redislocation as they are more active
- Patients with torn rotator cuffs or fracture of the glenoid have a higher incidence of redislocation.[1]
Mechanism of Injury / Pathological Process[edit | edit source]
Extreme rotation can cause the humeral head to come out of the glenoid labrum. Contact sports injuries are a common cause a dislocated shoulder as are motor trauma and falls.[1]
Anterior Shoulder Dislocation
An anterior dislocation is the most common dislocation and is caused by the arm being positioned in an excessive amount of abduction and external rotation. In this position, the inferior glenohumeral complex serves as the primary restraint to anterior glenohumeral translation.[3] Due to a lack of ligamentous support and dynamic stabilization, the glenohumeral joint is most susceptible to dislocation in the 90° abduction and 90° external rotation.
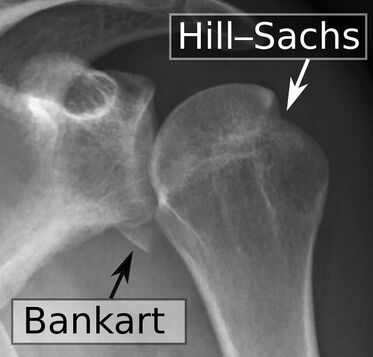
Complications and associated injuries include:
- Shoulder instability from damage to the inferior glenohumeral ligament.
- Hill-Sachs defect
- Bankart lesion or other anterior glenolabral injuries
- Damaged axillary artery, or brachial plexus[4]
Posterior Shoulder Dislocation (PSD)
Posterior dislocation is less common as it accounts for 3% of shoulder dislocations. Typically the humeral head is forced posteriorly in internal rotation while the arm is abducted. Causes include: Convulsive disorders (most common cause in adults, often bilateral); electrocution; road trauma.[5]
Clinical Presentation[edit | edit source]
Anterior Dislocation (humeral head comes to lie anterior, medial and slightly inferior to its normal location and glenoid fossa).
Following an acute anterior glenohumeral dislocation:
- Arm held in an abducted and ER position
- Loss of normal contour of the deltoid and acromion prominent posteriorly and laterally
- Humeral head palpable anteriorly[3]
- All movements limited and painful
- Palpable fullness below the coracoid process and towards the axilla[6]
- Possible damage to rotator cuff musculature and bone.
- Vascular injuries may result from traction of the axillary blood vessels, resulting in a reduced pulse pressure or a transient coolness in the hands.[3]
- Peripheral nerve injuries are common due to traction if the brachial plexus.
Posterior Dislocation
With acute posterior glenohumeral dislocation:
- Arm is abducted and IR
- May or may not lose deltoid contour
- May notice posterior prominence head of humerus
- Tear of subscapularis muscle (weak or cannot internally rotate)
- Neurovascular compromise is rare, but posterior shoulder instability may result from associated glenolabral and capsular injuries.
Posterior dislocations are hard to reduce, attempts at closed reduction need be performed in consultation with a treating orthopaedic surgeon. If the shoulder dislocation was ≥3 weeks ago (common in feeble elderly patients) or if their is reverse Hill-Sachs defect involving >20% of the articular surface, then the closed reduction is contraindicated.[5]
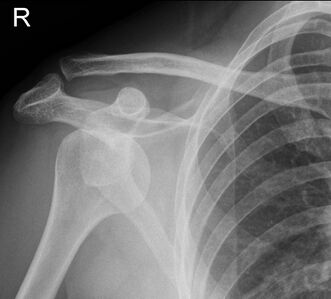
Diagnostic Procedures[edit | edit source]
Refer to rule out a fracture if the dislocation is suspected.
- pre-reduction radiographs are necessary to determine the direction of the dislocation and to assess for any associated fractures. If a glenoid rim fracture is observed on the initial radiograph. a CT scan can be done to determine the size of the fracture. An MRI can be used to rule in or rule out any soft tissue pathologies.[6] As clinicians, it is important for us to know the results of imaging to help guide us in our treatment process. Medical diagnostics will largely depend on local protocol but may include plain radiographs (A/P, stryker notch, or Westpoint views), CT or MRI scans.
Outcome Measures[edit | edit source]
Disabilities of the arm, shoulder and hand (DASH)
QuickDASH
Shoulder Pain and Disability Index (SPADI)
Numeric Pain Rating Scale (NPRS)
Management / Interventions[edit | edit source]
Anterior Dislocation
There is limited evidence or consensus on optimal treatment. Non-surgical management may be preferred initially, but surgical repair may be warranted for those who fail conservative care or require extreme usage of the upper extremity (i.e.-elite level athletes). Post-operative protocols are largely surgeon-dependent and may vary based on several factors including age, tissue quality, repair type, and fixation. For an anterior dislocation, the recommended intervention non surgically would be to have a closed reduction via a physician. An anterior dislocation can be surgically repaired via stabilization procedures. Following either intervention plan, the physician should be contacted for a specific protocol. In addition, after either intervention the management is similar. However, if it is a surgical procedure, knowing what type of surgery was performed as well as the precautions post-surgery. Typical precautions are:
- If subscapularis was cut, no resisted internal rotation for 4-6 weeks
- The external rotation usually limited to 30 degrees initially, then 45 degrees at 6 weeks
Wang and colleagues[6], suggested a three-phase protocol discussing some recommendations for this phasic approach.
Phase 1 (up to 6 weeks)[6]: Goal is to maintain anterior-inferior stability
- Immobilization
It has traditionally been thought to be immobilized with internal rotation, but according to Miller, immobilization has been beneficial in external rotation because there is more contact force between the glenoid labrum and the glenoid.[7] Research by Itoi[8] suggests immobilization at 10 degrees of external rotation has a lower recurrence rate than internal immobilization at 10 degrees.[8] There is currently no consensus on the duration of immobilization in a sling.[9] But, typical time periods in a sling range for 3-6 weeks if under the age of 40 and 1-2 weeks if older than the age of 40.[8] During the immobilization period, the focus is on AROM of the elbow, wrist and hand and reduction of pain. Isometrics can be incorporated for the rotator cuff and biceps musculature.
- Codman Exercises
- AAROM for external rotation (0-30º) and forward elevation (0-90º)
Phase 2 (6-12 weeks)[6]: Goal is to restore adequate motion, specifically in external rotation
- AAROM to achieve a full range of motion when stretching is permitted, passively stretch the posterior joint capsule through the use of joint mobilizations or self-stretching.
- No strengthening or repetitive exercises should start until the achievement of the full range of motion
Phase 3 (12-24 weeks)[6]: Successful return to sports or physical activities of daily living
- Begin strengthening exercise, strengthening exercises should be impairment-based. Typically begin strengthening exercise in a pain-free motion with exercises for stability. A possible progression could begin by focusing on the rotator cuff musculature and scapular stabilizers, which include trapezius, serratus, levator scapulae, and rhomboids. Then, progress to the larger musculature such as the deltoids, latissimus dorsi, and pectorals.
- Start focusing on functional exercises include proprioceptive training, tailor to promote patient's activities and participation in society
Posterior Dislocation
Management for posterior dislocation follows the same progression as anterior protocol, except for the following guidelines:
a. Posterior glide is contraindicated
b. Avoid flexion with adduction and internal rotation
c. Immobilized 3-6 weeks if less than 40 years of age and 2-3 weeks if greater than 40 years of age
d. Strengthening will focus primarily on posterior musculature such as: infraspinatus, teres minor and posterior deltoid
Differential Diagnosis[3][edit | edit source]
- Fracture (clavicle, glenoid, humeral head, greater tuberosity, and proximal humerus)
- Rheumatoid Arthritis
- Rotator Cuff Injury
- Acromioclavicular Joint Dislocation
- Labral Pathology
- Shoulder Subluxation
- Axillary Nerve/Suprascapular Nerve Palsies
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 Abrams R, Akbarnia H. Shoulder dislocations overview. InStatPearls [Internet] 2021 Aug 13. StatPearls Publishing.Available:https://www.ncbi.nlm.nih.gov/books/NBK459125/ (accessed 8.1.2023)
- ↑ 2.0 2.1 Radiopedia Shoulder Dislocation Available:https://radiopaedia.org/articles/shoulder-dislocation (accessed 8.1.2023)
- ↑ 3.0 3.1 3.2 3.3 Boone JL, Arciero RA. First-time anterior shoulder dislocations: has the standard changed? Br J Sports Med. 2010;44:355-360.
- ↑ Radiopedia Anterior Shoulder Dislocation Available:https://radiopaedia.org/articles/anterior-shoulder-dislocation?lang=gb (accessed 8.1.2023)
- ↑ 5.0 5.1 Radiopedia Posterior Shoulder Dislocation Available:https://radiopaedia.org/articles/posterior-shoulder-dislocation?lang=gb (accessed 8.1.2023)
- ↑ 6.0 6.1 6.2 6.3 6.4 6.5 Wang RY, Arciero RA, and Mazzocca AD. The recognition and treatment of first-time shoulder dislocation in active individuals. JOSPT. 2009;39(2):118-123
- ↑ Miller BS, Sonnabend DH, Hatrick C, O'Leary S, Goldberg J, Harper W, et al. Should acute anterior dislocations of the shoulder be immobilized in external rotation? A cadaveric study. J Shoulder Elbow Surg. 2004; 13: 589-592
- ↑ 8.0 8.1 8.2 Itoi E, Hatakeyama Y, Sato T, Kido T, Minagawa H, Yamamoto N, Wakabayashi I, et al. Immobilization in external rotation after shoulder dislocation reduces the risk of recurrence. A randomized controlled trial. J Bone Joint Surg Am. 2007; 89:2124-2131
- ↑ Scheibel M, Kuke A, Nikulka C, Magosch P, Ziesler O, and Schroeder J. How long should acute anterior dislocations of the shoulder be immobilized in external rotation? Am J Sports Med. 2009; 37:1309-1316.