Scheuermann's Kyphosis: Difference between revisions
No edit summary |
No edit summary |
||
| (12 intermediate revisions by 4 users not shown) | |||
| Line 2: | Line 2: | ||
'''Original Editors '''- [[User:Liza De Dobbeleer|Liza De Dobbeleer]] | '''Original Editors '''- [[User:Liza De Dobbeleer|Liza De Dobbeleer]] | ||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} - | ||
</div> | </div> | ||
== Definition/Description == | == Definition/Description == | ||
[[File:Scheuermanns disease.jpg|right|frameless]] | |||
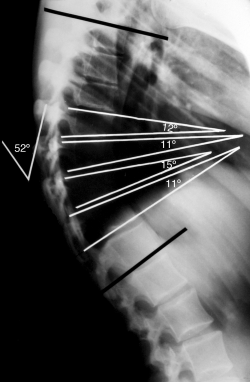
Scheuermann kyphosis, also known as Scheuermann disease, juvenile kyphosis or juvenile discogenic disease, is a condition of hyperkyphosis that involves the vertebral bodies and discs of the spine identified by anterior wedging of greater than or equal to 5 degrees in 3 or more adjacent vertebral bodies. The thoracic spine is most commonly involved, although involvement can include the thoracolumbar/lumbar region as well.<ref name=":0">Mansfield JT, Bennett M[https://www.ncbi.nlm.nih.gov/books/NBK499966/ . Scheuermann Disease.] InStatPearls [Internet] 2019 Jan 17. StatPearls Publishing. Available from:https://www.ncbi.nlm.nih.gov/books/NBK499966/ (last accessed 20.4.2020)</ref> Image R severe case - pre-operative image of a 22 year old male with Scheuermann's Disease | |||
* Most commonly, diagnosis is made in adolescents aged 12 to 17 years who present after their parents notice a postural deformity or “hunchbacked” appearance. | |||
There are two major forms of Scheuermann's kyphosis. The thoracic form is most common and has an apex between T7-T9. Secondly, the thoracolumbar form can occur with an apex between T10-T12 and is more likely to continue into adulthood.<ref name="Savvidou" /><ref name="LoweTG">Lowe TG, Line BG. Evidence based medicine: analysis of Scheuermann kyphosis. Spine 2007;32(19 | * Pain in the affected hyperkyphotic region may also be the cause of initial evaluation | ||
* Scheuermann's disease is the most common cause of kyphotic deformity in adolescents.<ref name="Savvidou">Papagelopoulos PJ, Mavrogenis AF, Savvidou OD, Mitsiokapa EA, Themistocleous GG, Soucacos PN. [https://search.proquest.com/openview/ff361ff1a9fb8c730bcf25b99dc8ffec/1?pq-origsite=gscholar&cbl=40235 Current concepts in Scheuermann's kyphosis]. Orthopedics (Online). 2008;31(1):52.</ref> | |||
There are two major forms of Scheuermann's kyphosis. | |||
* The thoracic form is most common and has an apex between T7-T9. | |||
* Secondly, the thoracolumbar form can occur with an apex between T10-T12 and is more likely to continue into adulthood.<ref name="Savvidou" /><ref name="LoweTG">Lowe TG, Line BG. [https://journals.lww.com/spinejournal/fulltext/2007/09011/Evidence_Based_Medicine__Analysis_of_Scheuermann.9.aspx Evidence based medicine: analysis of Scheuermann kyphosis]. Spine. 2007 Sep 1;32(19):S115-9.</ref> <ref name="Weiss">Weiss H, Turnbull D. Kyphosis (Physical and technical rehabilitation of patients with Scheuermann's disease and kyphosis). International encyclopedia of rehabilitation. 2010.</ref> | |||
| |||
== Clinically Relevant Anatomy == | == Clinically Relevant Anatomy == | ||
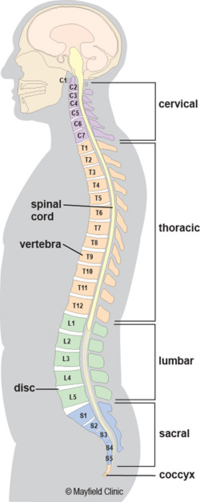
[[File:Spineanatomy.png|right|frameless|502x502px]] | |||
The spine of an adult is naturally shaped in an S-curve. The [[Cervical Anatomy|cervical]] and [[Lumbar Anatomy|lumbar]] regions are concave (lordosis), and the [[Thoracic Anatomy|thoracic]] and sacral regions are convex (kyphosis). According to the Scoliosis Research Society, the thoracic spine has a kyphosis between 20 to 40 degrees. A spinal deformity is considered when the curve is greater (or lesser) as mentioned degrees. <br> | |||
Scheuermann’s disease is a structural deformity of the vertebral bodies and spine. The kyphosis of the thoracic region will be around 45 to 75 degrees. Also there will be vertebral wedging greater than five degrees of 3 or more adjacent vertebrae. <ref name="Sorenson">Soerensen KH. Scheuermann's juvenile kyphosis. Munksgaard; 1964.</ref> The wedge shaped bodies characterize the rigid hyperkyphosis we see in Scheuermann’s disease. The hyperkyphosis can be compensated by a lumbar and cervical hyperlordosis. | |||
Scheuermann’s disease is a structural deformity of the vertebral bodies and spine. The kyphosis of the thoracic region will be around 45 to 75 degrees. Also there will be vertebral wedging greater than five degrees of 3 or more adjacent vertebrae. <ref name="Sorenson"> | |||
== | == Etiology == | ||
Definitive and universally accepted etiology of Scheuermann kyphosis remains undetermined. | |||
* An hereditary component is understood to contribute to this condition's development, although the mode of transmission is still unclear. | |||
* One growing theory, supported by histologic findings, suggests discordant vertebral endplate mineralization and ossification during growth which causes disproportional vertebral body growth and resultant classic wedge-shaped vertebral bodies that lead to kyphosis<ref name=":0" /> | |||
* Other theories proposed include mechanical, metabolic, and endocrinologic causes, but the real cause is still unclear.<br> | |||
== Epidemiology == | |||
* Prevalence: 1% to 8% in the United States | |||
* Sex: Male to female ratio is at least 2:1 | |||
* Age: Most commonly diagnosed in adolescents 12-17 years | |||
* Rarely diagnosed in children less than 10 years. | |||
* Classification: Type I (Classic) - Thoracic spine involvement only, with the apex of curve T7-T9Type II - Thoracic and lumbar involvement, with the apex of curve T10-T12<ref name=":0" /> | |||
== Characteristics/Clinical Presentation == | == Characteristics/Clinical Presentation == | ||
[[File:Scheuerman2.png|right|frameless|382x382px]] | |||
According to Sorenson <ref name="Sorenson" />, Scheuermann’s kyphosis is characterized by following criteria. | |||
* Three or more adjacent vertebrae must be wedged 5° or more | |||
* Must be no evidence of congenital, infectious or traumatic disorders of the spine. | |||
The adolescent will present with | |||
* Cosmetic/postural deformity | |||
* Possible Subacute thoracic pain, usually no identifiable inciting event. The pain is worse with activity and improved with rest. | |||
* Deformity is typically appreciated in the early-mid teenage years by child, parents, or on a school screening exam. | |||
* Physical exam shows rigid hyperkyphotic curve, accentuated with forward bending. | |||
* Hyperkyphosis does not resolve with an extension or lying prone/supine, further supporting the “rigid” nature of this deformity. | |||
* Other associated findings on an exam might include cervical or lumbar hyperlordosis, scoliosis, and tight hamstrings. Although neurologic deficits are uncommon, a thorough neurologic exam must be completed<ref name=":0" /> | |||
* Muscle stiffness and fatigue, especially at the end of the day | |||
* Decreased flexibility of the torso | |||
* In severe cases, heart and lung function can be impaired or severe neurological symptoms can occur. These symptoms are extremely rare. | |||
Patients with Scheuermann's disease may also complain of inability to participate in physical exercise, work and activities of daily living secondary to pain or the presence of their deformity negatively affecting their cosmetic appearance.<ref name="Ristolainen">Ristolainen L, Kettunen JA, Heliövaara M, Kujala UM, Heinonen A, Schlenzka D. [https://link.springer.com/article/10.1007/s00586-011-2075-0 Untreated Scheuermann’s disease: a 37-year follow-up study]. European Spine Journal. 2012 May;21(5):819-24.</ref><br>Possible to see cutaneous skin pigmentation at the area of greatest curvature due to skin friction on chair backs.<ref name="Ristolainen" /><br>The natural history of Scheuermann’s kyphosis is unclear, with conflicting reports as to the severity of pain and physical disability. <ref name="Bezalel">Bezalel T, Carmeli E, Been E, Kalichman L. [https://content.iospress.com/articles/journal-of-back-and-musculoskeletal-rehabilitation/bmr00483 Scheuermann's disease: current diagnosis and treatment approach]. Journal of back and musculoskeletal rehabilitation. 2014 Jan 1;27(4):383-90.</ref><br> | |||
Patients with Scheuermann's disease may also complain of inability to participate in physical exercise, work and activities of daily living secondary to pain or the presence of their deformity negatively affecting their cosmetic appearance.<ref name="Ristolainen">Ristolainen, | |||
== Differential Diagnosis == | == Differential Diagnosis == | ||
* | * Postural [[kyphosis]] (flexible postural deformity) | ||
* [[Thoracic Hyperkyphosis|Hyperkyphosis]] attributable to another known disease state | |||
* [ | * Postsurgical kyphosis | ||
* [[Ankylosing Spondylitis (Axial Spondyloarthritis)|Ankylosing spondylitis]] | |||
* [[Scoliosis]] | |||
* | |||
* | |||
* [ | |||
== Diagnostic Procedures == | == Diagnostic Procedures == | ||
History and physical along with AP/lateral radiographs comprise the essential components for evaluating Scheuermann kyphosis. Lateral radiographs are required for diagnosis, and diagnostic criteria including the following: | |||
* | * Rigid hyperkyphosis, greater than 40 degrees | ||
* | * Anterior wedging, greater than or equal to 5 degrees in three or more adjacent vertebral bodies<ref name=":0" /><ref name="Ali">Ali RM, Green DW, Patel TC. [https://europepmc.org/article/med/10084088 Scheuermann's kyphosis]. Current opinion in pediatrics. 1999 Feb 1;11(1):70-5.</ref> | ||
Other Associated Findings Noted on AP/Lateral Radiographs | |||
* Irregular vertebral endplates | |||
* Schmorl nodes | |||
* Loss of disc space height | |||
* | * Scoliosis | ||
* | * Spondylolysis/spondylolisthesis | ||
* | * Disc herniation | ||
Typically not a necessity, MRI can be helpful to further evaluate anatomic changes or for pre-operative planning. CT imaging is usually not needed. There are also no specific laboratory tests or histologic findings necessary for the diagnosis of Scheuermann kyphosis<ref name=":0" />.<br> | |||
== Outcome Measures == | == Outcome Measures == | ||
[[Occiput to Wall Distance OWD|Occiput to Wall Distance]] | |||
Following self-reported outcome measures can be used after an operative treatment <ref name="Poolman">Poolman | Following self-reported outcome measures can be used after an operative treatment <ref name="Poolman">Poolman R, Been H, Ubags L. [https://link.springer.com/article/10.1007/s00586-002-0418-6 Clinical outcome and radiographic results after operative treatment of Scheuermann's disease]. European Spine Journal. 2002 Dec;11(6):561-9.</ref> or for untreated Scheuermann’s disease as well <ref name="Ristolainen" />: | ||
# | #Scoliosis Research Society Instrument (SRSI): This questionnaire can be used for follow- up of an individual to see if the patient reports improvements in level of activity, pain, personal relationships etc. | ||
#Back pain and disability scores: [http://www.physio-pedia.com/Visual_Analogue_Scale Visual Analogue Scale (VAS)], [http://www.physio-pedia.com/Quebec_Back_Pain_Disability_Scale Quebec Back Pain Disability Scale (QBPDS)], [http://www.physio-pedia.com/Roland‐Morris_Disability_Questionnaire Roland-Morris Disability Questionnaire], [http://www.physio-pedia.com/index.php?title=Oswestry_Disability_Index Oswestry Disability Index (ODI)] and SF-36: measures Quality of Life (QoL) across eight domains, which contain a physical component score (PCS) and a mental component score (MCS) | #Back pain and disability scores: [http://www.physio-pedia.com/Visual_Analogue_Scale Visual Analogue Scale (VAS)], [http://www.physio-pedia.com/Quebec_Back_Pain_Disability_Scale Quebec Back Pain Disability Scale (QBPDS)], [http://www.physio-pedia.com/Roland‐Morris_Disability_Questionnaire Roland-Morris Disability Questionnaire], [http://www.physio-pedia.com/index.php?title=Oswestry_Disability_Index Oswestry Disability Index (ODI)] and SF-36: measures Quality of Life (QoL) across eight domains, which contain a physical component score (PCS) and a mental component score (MCS) | ||
== Examination == | == Examination == | ||
* The most significant feature of patients with Scheuermann’s disease is the thoracic kyphosis. | |||
The most significant feature of patients with Scheuermann’s disease is the thoracic kyphosis. Often the kyphosis is accompanied by a lumbar and/or cervical hyperlordosis. The cervical lordosis can be increased with a protrusion of the head. The shoulders mostly are positioned anteriorly. These abnormalities can be accompanied by a mild to moderate scoliosis. Patients with Scheuermann's disease are well muscled compared to patients with postural kyphosis. <ref name="LoweTG" /><br>The examination consist of: | * Often the kyphosis is accompanied by a lumbar and/or cervical hyperlordosis. | ||
* The cervical lordosis can be increased with a protrusion of the head. The shoulders mostly are positioned anteriorly. | |||
* These abnormalities can be accompanied by a mild to moderate scoliosis. | |||
*[[File:Scheuermann's Kyphosis Example.JPG|right|frameless]]Patients with Scheuermann's disease are well muscled compared to patients with postural kyphosis. <ref name="LoweTG" /><br>The examination consist of: | |||
# Postural assessment: examination of the posture from anterior, posterior and lateral view | # Postural assessment: examination of the posture from anterior, posterior and lateral view | ||
# Neurological screening: <ref name="Weiss" /> rarely the spinal cord can be stretched over the posterior aspect of the vertebral bodies at the apex of the curvature which may cause neurological signs of impending paraplegia with clonus and hyperreflexia.<ref name="Lemire" /> | # Neurological screening: <ref name="Weiss" /> rarely the spinal cord can be stretched over the posterior aspect of the vertebral bodies at the apex of the curvature which may cause neurological signs of impending paraplegia with clonus and hyperreflexia.<ref name="Lemire">Lemire JJ, Mierau DR, Crawford CM, Dzus AK. [https://europepmc.org/article/med/8728463 Scheuermann's juvenile kyphosis]. Journal of manipulative and physiological therapeutics. 1996 Mar 1;19(3):195-201.</ref> | ||
# [http://www.physio-pedia.com/Adam%27s_forward_bend_test Adam’s forward-bend test]: Scheuermann’s kyphosis can be accompanied by a scoliosis | # [http://www.physio-pedia.com/Adam%27s_forward_bend_test Adam’s forward-bend test]: Scheuermann’s kyphosis can be accompanied by a scoliosis. <ref name="Hart">Hart ES, Merlin G, Harisiades J, Grottkau BE. [https://journals.lww.com/orthopaedicnursing/FullText/2010/11000/Scheuermann_s_Thoracic_Kyphosis_in_the_Adolescent.5.aspx Scheuermann's thoracic kyphosis in the adolescent patient]. Orthopaedic Nursing. 2010 Nov 1;29(6):365-71.</ref> | ||
#Muscle length testing: the disease can be accompanied by tightness of the M. Pectoralis, [http://www.physio-pedia.com/Hamstrings M. Hamstrings], M. suboccipitalis and the hip flexors with possible contractures of the anterior shoulder and hip <ref name="Savvidou" /><ref name="LoweTG" /> | #Muscle length testing: the disease can be accompanied by tightness of the [[Pectoralis major|M. Pectoralis]], [http://www.physio-pedia.com/Hamstrings M. Hamstrings], [[Cervical Anatomy|M. suboccipitalis]] and the hip flexors with possible contractures of the anterior shoulder and hip <ref name="Savvidou" /><ref name="LoweTG" /> | ||
#Range of motion: Flexibility of the extremities and spine can identify impairments and track changes over time.<ref name="Hart" /> | #Range of motion: Flexibility of the extremities and spine can identify impairments and track changes over time.<ref name="Hart" /> | ||
#Muscle strength testing: strength of the abdominals, core, trunk extensors and gluteal muscles must be assessed<br> | #[[Muscle Strength Testing|Muscle strength testing:]] strength of the abdominals, core, trunk extensors and gluteal muscles must be assessed<br> | ||
== Medical Management | == Medical Management == | ||
'''Nonoperative Management''' | |||
# Stretching, lifestyle modification, NSAIDs, plus/minus physical therapy | |||
Indication | |||
* Kyphosis less than 60 degrees and asymptomatic | |||
Course | |||
* Majority of patients fall into this category | |||
* Patients typically do well without significant long term sequelae | |||
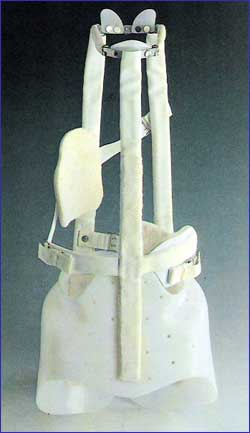
[[File:Milwaukee brace.jpg|right|frameless]] | |||
2. Extension bracing plus above | |||
Indication | |||
* | * Kyphosis 60 to 80 degrees plus/minus symptomatic | ||
Course | |||
* Bracing typically required for 12 to 24 months | |||
* | * [[Milwaukee brace|Milwaukee]] brace (see image R), Kyphologic brace or Thoracolumbosacral orthosis-style Boston brace | ||
* | * Most effective in skeletally immature patients | ||
* Typically, does not improve curve but rather impedes progression | |||
'''Operative Management''' | |||
Spinal fusion, typically combination of anterior release + fusion as well as posterior instrumentation + fusion | |||
= | Indications | ||
* Kyphosis greater than 75 degrees causing unacceptable deformity | |||
* Kyphosis greater than 75 degrees with associated pain | |||
* Neurologic deficit/spinal cord compression | |||
* Severe refractory pain | |||
Course | |||
* Majority of patients experience symptomatic improvement as well as improved curve deformity towards normal | |||
* Operative/postoperative complications must be considered<ref name=":0" /><br> | |||
== Physical Therapy Management == | |||
Non Surgical Treatment | |||
A child or youth with a mild kyphosis may simply need to be observed for changes in the curve, as well as be educated on their posture and activities by the physiotherapist. | |||
* | * Unless the curve or pain becomes worse, no other treatment may be needed. | ||
* Some children eventually improve without having a noticeable abnormal kyphosis and have no long-term problems. | |||
* Others may always have a mildly exaggerated thoracic kyphosis but are able to function normally without subsequent pain or other problems.<ref name=":1">Advantage Physiotherapy [https://www.advantagephysiotherapy.com/Injuries-Conditions/Upper-Back-and-Neck/Upper-Back-Issues/Scheuermann-s-Disease/a~5944/article.html SCHEUERMANN'S DISEASE] Available from:https://www.advantagephysiotherapy.com/Injuries-Conditions/Upper-Back-and-Neck/Upper-Back-Issues/Scheuermann-s-Disease/a~5944/article.html (last accessed 20.4.2020)</ref> | |||
The doctor may suggest bracing along with exercise. | |||
* A brace is most effective when used before the skeleton matures at about age 14. | |||
* Ideally, bracing should begin at the onset of puberty, be worn for approximately 2 years, and removed at the end of skeletal maturity. <ref name="Weiss" /><ref name="Sorenson" /> | |||
* Doctors commonly chose a Milwaukee brace, which is made of molded plastic that conforms to the waist and is designed to hold the shoulders back and gradually straighten the thoracic curve. The brace has two upright, padded bars line up along the sides of the spine. Pressure from the upright bars straightens the spine ( won't reverse the curve a fully developed spine, nor is it helpful for rigid curves that angle more than 75 degrees). | |||
=== | === Bracing === | ||
* Younger patients (under 15) generally wear the brace all the time including at night, although they usually remove the brace to shower. | |||
* The doctor adjusts the brace regularly as the curve improves. | |||
* When the thoracic curve has improved enough, the brace is worn part-time (eight to 12 hours per day) until the skeleton is fully mature, which is typically around age 14 or 15. | |||
* Sometimes adults obtain partial correction of the kyphosis and pain relief with bracing even though they have reached full bone growth. Bracing for pain relief in adults is also considered when surgery is not an option.<ref name=":1" /> | |||
'''Physiotherapy''' is recommended in combination with bracing. | |||
* Exercises appear to maximize the effect of the brace by strengthening muscles that help align the spine | |||
* Advice from a physiotherapist regarding posturing and activity modification can be extremely useful in the treatment of Scheuermann’s kyphosis. | |||
* Even if a brace is not used, physiotherapy is recommended to assist with any pain that may be present, to teach proper posturing for the spine, and to assess and treat any muscular imbalances that may be affecting the mechanical pull on the spine. | |||
Doctors may prescribe anti-inflammatory medication for pain. Younger patients generally use this medicine on a short-term basis, in combination with other treatments. Adults who have ongoing pain sometimes require long-term use of anti-inflammatory medication<ref name=":1" />. | |||
According to Lowe, brace treatment is almost always successful in patients with kyphosis between 55 degrees and 80 degrees if the diagnosis is made before skeletal maturity. | |||
* Bracing therapy has a few shortcomings: as the bracing time increases, the probability to develop low back pain increases | |||
* In adolescents the compliance is usually low | |||
* Other bracing strategies have been attempted such as the use of a soft brace but this however has not shown to be successful. With a soft brace no correction can be achieved in rigid curvatures.<ref name="Sorenson" /><ref name="Weiss" /> | |||
'''Other aspects of Physiotherapy Treatment''' | |||
Scheuermann's disease | Patient education includes | ||
* Extension-based stretching/strengthening program | |||
* Hamstring stretching exercise program | |||
* Proper postural and body mechanic techniques for ADLs | |||
* Appropriate use and handling of braces<ref name=":0" /> | |||
Postural improvement: | |||
* Focuses on hamstring and pectoralis stretching and trunk extensor strengthening as well as improving function.<ref name="Weissetal">Weiss HR, Turnbull D, Bohr S. [https://scoliosisjournal.biomedcentral.com/articles/10.1186/1748-7161-4-22 Brace treatment for patients with Scheuermann's disease-a review of the literature and first experiences with a new brace design]. Scoliosis. 2009 Dec;4(1):1-7.</ref> | |||
* These exercises can be effective when the thoracic spine has not developed a relevant stiffness and when the sagittal curve is not too high: [http://www.physio-pedia.com/Cobb's_angle Cobb angles] from 44° to 55°. <ref name="Goodman">Goodman CC, Fuller KS. Goodman and Fuller’s Pathology E-Book: Implications for the Physical Therapist. 3rd edition Elsevier Health Sciences; 2009.</ref> | |||
* Practice normal posture standing and sitting <ref name="hansrudolf" /><ref name="dieckmann" /><ref name="Ball" /><ref name="montgomery" /><ref name="zaina" /> | |||
Exercises | |||
* Flexibility exercises to relieve lower extremity contractures eg Hamstrings<ref name="Tomer">Bezalel T, Kalichman L. [https://www.sciencedirect.com/science/article/pii/S1360859214000606 Improvement of clinical and radiographical presentation of Scheuermann disease after Schroth therapy treatment]. Journal of bodywork and movement therapies. 2015 Apr 1;19(2):232-7.</ref> | |||
* Strengthen core musculature, back extensors . <ref name="hansrudolf">Weiß HR, Dieckmann J, Gerner HJ. [https://ebooks.iospress.nl/volumearticle/19945 Outcome of in-patient rehabilitation in patients with M. Scheuermann evaluated by surface topography]. Research into Spinal Deformities 3. 2002:246-9.</ref><ref name="dieckmann">Weiß HR, Ddeckmann J, Gerner HJ. [https://ebooks.iospress.nl/doi/10.3233/978-1-60750-932-5-254 Effect of intensive rehabilitation on pain in patients with Scheuermann’s disease]. InResearch into Spinal Deformities 3 2002 (pp. 254-257). IOS Press.</ref><ref name="Ball">Ball JM, Cagle P, Johnson BE, Lucasey C, Lukert BP. [https://link.springer.com/content/pdf/10.1007/s00198-008-0690-3.pdf Spinal extension exercises prevent natural progression of kyphosis]. Osteoporosis International. 2009 Mar 1;20(3):481.</ref><ref name="montgomery">Montgomery SP, Erwin WE. [https://europepmc.org/article/med/6782681 Scheuermann's kyphosis--long-term results of Milwaukee braces treatment]. Spine. 1981 Jan 1;6(1):5-8.</ref><ref name="zaina">Zaina F, Atanasio S, Ferraro C, Fusco C, Negrini A, Romano M, Negrini S. [https://isico.it/images/uploads/pubblicazioni/completo/ID00304.pdf Review of rehabilitation and orthopedic conservative approach to sagittal plane diseases during growth: hyperkyphosis, junctional kyphosis, and Scheuermann disease]. Eur J Phys Rehabil Med. 2009 Dec 1;45(4):595-603.</ref> | |||
Sports | |||
* Extension sports are advised: such as gymnastics, aerobics, swimming, basketball, cycling and hyperextension exercises. | |||
* Some sports should be discouraged: like sports associated with jumping, marked stress and functional overuse of the back. <ref name="engell">Damborg F, Engell V, Andersen M, Kyvik KO, Thomsen K. [https://journals.lww.com/jbjsjournal/Fulltext/2006/10000/Prevalence,_Concordance,_and_Heritability_of.3.aspx Prevalence, concordance, and heritability of Scheuermann kyphosis based on a study of twins.] JBJS. 2006 Oct 1;88(10):2133-6.</ref><ref name="sturm">Sturm PF, Dobson JC, Armstrong GW. [https://europepmc.org/article/med/8516695 The surgical management of Scheuermann's disease]. Spine. 1993 May 1;18(6):685-91.</ref> | |||
Postoperative physical therapy | |||
* Necessary and must contain breathing exercises, mobilizations and strengthening exercises. <ref name="Lowe">Lowe TG. [https://journals.lww.com/jbjsjournal/Citation/1990/72060/Scheuermann_disease_.26.aspx Scheuermann disease]. JBJS. 1990 Jul 1;72(6):940-5.</ref> <br> | |||
'''Scheuermann's disease in adults''' | |||
* Regarded differently from that of the teenager because the major manifestation is pain and not aesthetic quality. | |||
* The functional rehabilitation on an outpatient basis is the favoured treatment and referral for surgery or dorso-lumbar braces is rare. | |||
[[File:Scheuerman3.png|right|frameless|400x400px]] | |||
The kyphotic posture can be treated with the [[Scoliosis|Schroth]] method <ref name="Tomer" /> | |||
Examples of Schroth exercises are shown at R<br> | |||
<br> | |||
[[File:Scheuerman5.jpg|right|frameless|400x400px]] | |||
Another treatment regime is outline her, using a different method <ref name="hagit">Berdishevsky H. [https://scoliosisjournal.biomedcentral.com/articles/10.1186/s13013-016-0094-7 Outcome of intensive outpatient rehabilitation and bracing in an adult patient with Scheuermann’s disease evaluated by radiologic imaging—a case report]. Scoliosis and spinal disorders. 2016 Oct;11(2):47-51.</ref> There are five Principles of Correction:<br> | |||
* Trunk elongation and expansion | * Trunk elongation and expansion | ||
* Symmetrical sagittal straightening: identical exercises must be performed for both sides of the trunk (right and left):<br> Bilateral thoracic expansion in a posterior to anterior (PA) direction to reduce the thoracic hyperkyphosis<br> Bilateral lumbar expansion in an anterior to posterior (AP) direction to reduce the hyperlordotic low back | * Symmetrical sagittal straightening: identical exercises must be performed for both sides of the trunk (right and left):<br> Bilateral thoracic expansion in a posterior to anterior (PA) direction to reduce the thoracic hyperkyphosis<br> Bilateral lumbar expansion in an anterior to posterior (AP) direction to reduce the hyperlordotic low back | ||
| Line 146: | Line 196: | ||
* Correction of breathing: it allows the subject to feel an increased expansion in his/her initially collapsed regions. The goal is to expand the thorax in a back-to-front and a lateral direction. | * Correction of breathing: it allows the subject to feel an increased expansion in his/her initially collapsed regions. The goal is to expand the thorax in a back-to-front and a lateral direction. | ||
* Muscle activation by increasing tension: to achieve the best possible correction, muscle balance, stabilization and to increase the proprioceptive input. It helps to integrate the ‘corrected body schema’ in the brain. | * Muscle activation by increasing tension: to achieve the best possible correction, muscle balance, stabilization and to increase the proprioceptive input. It helps to integrate the ‘corrected body schema’ in the brain. | ||
* This intensive physical therapy combined with bracing (SpinoMed brace) is successful to treat an adult patient with Scheuermann’s kyphosis. <ref name="hagit" /> <br> | |||
More clinical trials are necessary to evaluate the effectiveness of conservative interventions, especially different exercises and manual therapies. These should also be combined/compared with braces. <ref name="Bezalel" /><br> | |||
More clinical trials are necessary to evaluate the effectiveness of conservative interventions, especially different exercises and manual therapies. These should also be combined/compared with braces. <ref name="Bezalel" /> | |||
== Clinical Bottom Line == | == Clinical Bottom Line == | ||
* The majority of patients are successfully treated with conservative measures as discussed above. | |||
* Pain in the affected region typically improves after skeletal maturity is reached, although patients with Scheuermann kyphosis are at increased risk of chronic back pain as compared to the general population. | |||
* Patients with a kyphotic curve less than 60 degrees at skeletal maturity typically have no long-term sequelae<ref name=":0" /><br> | |||
== Key Research == | == Key Research == | ||
#Bezalel, | #Bezalel T, Kalichman L. [https://www.sciencedirect.com/science/article/pii/S1360859214000606 Improvement of clinical and radiographical presentation of Scheuermann disease after Schroth therapy treatment]. Journal of bodywork and movement therapies. 2015 Apr 1;19(2):232-7. | ||
#Berdishevsky | #Berdishevsky H. [https://scoliosisjournal.biomedcentral.com/articles/10.1186/s13013-016-0094-7 Outcome of intensive outpatient rehabilitation and bracing in an adult patient with Scheuermann’s disease evaluated by radiologic imaging—a case report]. Scoliosis and spinal disorders. 2016 Oct;11(2):47-51.<br> | ||
== Resources == | == Resources == | ||
| Line 194: | Line 240: | ||
[[Category:Paediatrics - Conditions]] | [[Category:Paediatrics - Conditions]] | ||
[[Category:Thoracic Spine - Conditions]] | [[Category:Thoracic Spine - Conditions]] | ||
[[Category:Conditions]] | |||
[[Category:Genetic Disorders]] | |||
Latest revision as of 11:35, 12 March 2022
Original Editors - Liza De Dobbeleer
Top Contributors - Nicolas D'Hondt, Leen Meylemans, Liza De Dobbeleer, Lucinda hampton, Rachael Lowe, Kim Jackson, Admin, Fasuba Ayobami, WikiSysop, Aminat Abolade, 127.0.0.1, Elaine Lonnemann, Uchechukwu Chukwuemeka, Claire Knott, Meaghan Rieke and Anna Fuhrmann -
Definition/Description[edit | edit source]
Scheuermann kyphosis, also known as Scheuermann disease, juvenile kyphosis or juvenile discogenic disease, is a condition of hyperkyphosis that involves the vertebral bodies and discs of the spine identified by anterior wedging of greater than or equal to 5 degrees in 3 or more adjacent vertebral bodies. The thoracic spine is most commonly involved, although involvement can include the thoracolumbar/lumbar region as well.[1] Image R severe case - pre-operative image of a 22 year old male with Scheuermann's Disease
- Most commonly, diagnosis is made in adolescents aged 12 to 17 years who present after their parents notice a postural deformity or “hunchbacked” appearance.
- Pain in the affected hyperkyphotic region may also be the cause of initial evaluation
- Scheuermann's disease is the most common cause of kyphotic deformity in adolescents.[2]
There are two major forms of Scheuermann's kyphosis.
- The thoracic form is most common and has an apex between T7-T9.
- Secondly, the thoracolumbar form can occur with an apex between T10-T12 and is more likely to continue into adulthood.[2][3] [4]
Clinically Relevant Anatomy[edit | edit source]
The spine of an adult is naturally shaped in an S-curve. The cervical and lumbar regions are concave (lordosis), and the thoracic and sacral regions are convex (kyphosis). According to the Scoliosis Research Society, the thoracic spine has a kyphosis between 20 to 40 degrees. A spinal deformity is considered when the curve is greater (or lesser) as mentioned degrees.
Scheuermann’s disease is a structural deformity of the vertebral bodies and spine. The kyphosis of the thoracic region will be around 45 to 75 degrees. Also there will be vertebral wedging greater than five degrees of 3 or more adjacent vertebrae. [5] The wedge shaped bodies characterize the rigid hyperkyphosis we see in Scheuermann’s disease. The hyperkyphosis can be compensated by a lumbar and cervical hyperlordosis.
Etiology[edit | edit source]
Definitive and universally accepted etiology of Scheuermann kyphosis remains undetermined.
- An hereditary component is understood to contribute to this condition's development, although the mode of transmission is still unclear.
- One growing theory, supported by histologic findings, suggests discordant vertebral endplate mineralization and ossification during growth which causes disproportional vertebral body growth and resultant classic wedge-shaped vertebral bodies that lead to kyphosis[1]
- Other theories proposed include mechanical, metabolic, and endocrinologic causes, but the real cause is still unclear.
Epidemiology[edit | edit source]
- Prevalence: 1% to 8% in the United States
- Sex: Male to female ratio is at least 2:1
- Age: Most commonly diagnosed in adolescents 12-17 years
- Rarely diagnosed in children less than 10 years.
- Classification: Type I (Classic) - Thoracic spine involvement only, with the apex of curve T7-T9Type II - Thoracic and lumbar involvement, with the apex of curve T10-T12[1]
Characteristics/Clinical Presentation[edit | edit source]
According to Sorenson [5], Scheuermann’s kyphosis is characterized by following criteria.
- Three or more adjacent vertebrae must be wedged 5° or more
- Must be no evidence of congenital, infectious or traumatic disorders of the spine.
The adolescent will present with
- Cosmetic/postural deformity
- Possible Subacute thoracic pain, usually no identifiable inciting event. The pain is worse with activity and improved with rest.
- Deformity is typically appreciated in the early-mid teenage years by child, parents, or on a school screening exam.
- Physical exam shows rigid hyperkyphotic curve, accentuated with forward bending.
- Hyperkyphosis does not resolve with an extension or lying prone/supine, further supporting the “rigid” nature of this deformity.
- Other associated findings on an exam might include cervical or lumbar hyperlordosis, scoliosis, and tight hamstrings. Although neurologic deficits are uncommon, a thorough neurologic exam must be completed[1]
- Muscle stiffness and fatigue, especially at the end of the day
- Decreased flexibility of the torso
- In severe cases, heart and lung function can be impaired or severe neurological symptoms can occur. These symptoms are extremely rare.
Patients with Scheuermann's disease may also complain of inability to participate in physical exercise, work and activities of daily living secondary to pain or the presence of their deformity negatively affecting their cosmetic appearance.[6]
Possible to see cutaneous skin pigmentation at the area of greatest curvature due to skin friction on chair backs.[6]
The natural history of Scheuermann’s kyphosis is unclear, with conflicting reports as to the severity of pain and physical disability. [7]
Differential Diagnosis[edit | edit source]
- Postural kyphosis (flexible postural deformity)
- Hyperkyphosis attributable to another known disease state
- Postsurgical kyphosis
- Ankylosing spondylitis
- Scoliosis
Diagnostic Procedures[edit | edit source]
History and physical along with AP/lateral radiographs comprise the essential components for evaluating Scheuermann kyphosis. Lateral radiographs are required for diagnosis, and diagnostic criteria including the following:
- Rigid hyperkyphosis, greater than 40 degrees
- Anterior wedging, greater than or equal to 5 degrees in three or more adjacent vertebral bodies[1][8]
Other Associated Findings Noted on AP/Lateral Radiographs
- Irregular vertebral endplates
- Schmorl nodes
- Loss of disc space height
- Scoliosis
- Spondylolysis/spondylolisthesis
- Disc herniation
Typically not a necessity, MRI can be helpful to further evaluate anatomic changes or for pre-operative planning. CT imaging is usually not needed. There are also no specific laboratory tests or histologic findings necessary for the diagnosis of Scheuermann kyphosis[1].
Outcome Measures[edit | edit source]
Following self-reported outcome measures can be used after an operative treatment [9] or for untreated Scheuermann’s disease as well [6]:
- Scoliosis Research Society Instrument (SRSI): This questionnaire can be used for follow- up of an individual to see if the patient reports improvements in level of activity, pain, personal relationships etc.
- Back pain and disability scores: Visual Analogue Scale (VAS), Quebec Back Pain Disability Scale (QBPDS), Roland-Morris Disability Questionnaire, Oswestry Disability Index (ODI) and SF-36: measures Quality of Life (QoL) across eight domains, which contain a physical component score (PCS) and a mental component score (MCS)
Examination[edit | edit source]
- The most significant feature of patients with Scheuermann’s disease is the thoracic kyphosis.
- Often the kyphosis is accompanied by a lumbar and/or cervical hyperlordosis.
- The cervical lordosis can be increased with a protrusion of the head. The shoulders mostly are positioned anteriorly.
- These abnormalities can be accompanied by a mild to moderate scoliosis.
- Patients with Scheuermann's disease are well muscled compared to patients with postural kyphosis. [3]
The examination consist of:
- Postural assessment: examination of the posture from anterior, posterior and lateral view
- Neurological screening: [4] rarely the spinal cord can be stretched over the posterior aspect of the vertebral bodies at the apex of the curvature which may cause neurological signs of impending paraplegia with clonus and hyperreflexia.[10]
- Adam’s forward-bend test: Scheuermann’s kyphosis can be accompanied by a scoliosis. [11]
- Muscle length testing: the disease can be accompanied by tightness of the M. Pectoralis, M. Hamstrings, M. suboccipitalis and the hip flexors with possible contractures of the anterior shoulder and hip [2][3]
- Range of motion: Flexibility of the extremities and spine can identify impairments and track changes over time.[11]
- Muscle strength testing: strength of the abdominals, core, trunk extensors and gluteal muscles must be assessed
Medical Management[edit | edit source]
Nonoperative Management
- Stretching, lifestyle modification, NSAIDs, plus/minus physical therapy
Indication
- Kyphosis less than 60 degrees and asymptomatic
Course
- Majority of patients fall into this category
- Patients typically do well without significant long term sequelae
2. Extension bracing plus above
Indication
- Kyphosis 60 to 80 degrees plus/minus symptomatic
Course
- Bracing typically required for 12 to 24 months
- Milwaukee brace (see image R), Kyphologic brace or Thoracolumbosacral orthosis-style Boston brace
- Most effective in skeletally immature patients
- Typically, does not improve curve but rather impedes progression
Operative Management
Spinal fusion, typically combination of anterior release + fusion as well as posterior instrumentation + fusion
Indications
- Kyphosis greater than 75 degrees causing unacceptable deformity
- Kyphosis greater than 75 degrees with associated pain
- Neurologic deficit/spinal cord compression
- Severe refractory pain
Course
- Majority of patients experience symptomatic improvement as well as improved curve deformity towards normal
- Operative/postoperative complications must be considered[1]
Physical Therapy Management[edit | edit source]
Non Surgical Treatment
A child or youth with a mild kyphosis may simply need to be observed for changes in the curve, as well as be educated on their posture and activities by the physiotherapist.
- Unless the curve or pain becomes worse, no other treatment may be needed.
- Some children eventually improve without having a noticeable abnormal kyphosis and have no long-term problems.
- Others may always have a mildly exaggerated thoracic kyphosis but are able to function normally without subsequent pain or other problems.[12]
The doctor may suggest bracing along with exercise.
- A brace is most effective when used before the skeleton matures at about age 14.
- Ideally, bracing should begin at the onset of puberty, be worn for approximately 2 years, and removed at the end of skeletal maturity. [4][5]
- Doctors commonly chose a Milwaukee brace, which is made of molded plastic that conforms to the waist and is designed to hold the shoulders back and gradually straighten the thoracic curve. The brace has two upright, padded bars line up along the sides of the spine. Pressure from the upright bars straightens the spine ( won't reverse the curve a fully developed spine, nor is it helpful for rigid curves that angle more than 75 degrees).
Bracing[edit | edit source]
- Younger patients (under 15) generally wear the brace all the time including at night, although they usually remove the brace to shower.
- The doctor adjusts the brace regularly as the curve improves.
- When the thoracic curve has improved enough, the brace is worn part-time (eight to 12 hours per day) until the skeleton is fully mature, which is typically around age 14 or 15.
- Sometimes adults obtain partial correction of the kyphosis and pain relief with bracing even though they have reached full bone growth. Bracing for pain relief in adults is also considered when surgery is not an option.[12]
Physiotherapy is recommended in combination with bracing.
- Exercises appear to maximize the effect of the brace by strengthening muscles that help align the spine
- Advice from a physiotherapist regarding posturing and activity modification can be extremely useful in the treatment of Scheuermann’s kyphosis.
- Even if a brace is not used, physiotherapy is recommended to assist with any pain that may be present, to teach proper posturing for the spine, and to assess and treat any muscular imbalances that may be affecting the mechanical pull on the spine.
Doctors may prescribe anti-inflammatory medication for pain. Younger patients generally use this medicine on a short-term basis, in combination with other treatments. Adults who have ongoing pain sometimes require long-term use of anti-inflammatory medication[12].
According to Lowe, brace treatment is almost always successful in patients with kyphosis between 55 degrees and 80 degrees if the diagnosis is made before skeletal maturity.
- Bracing therapy has a few shortcomings: as the bracing time increases, the probability to develop low back pain increases
- In adolescents the compliance is usually low
- Other bracing strategies have been attempted such as the use of a soft brace but this however has not shown to be successful. With a soft brace no correction can be achieved in rigid curvatures.[5][4]
Other aspects of Physiotherapy Treatment
Patient education includes
- Extension-based stretching/strengthening program
- Hamstring stretching exercise program
- Proper postural and body mechanic techniques for ADLs
- Appropriate use and handling of braces[1]
Postural improvement:
- Focuses on hamstring and pectoralis stretching and trunk extensor strengthening as well as improving function.[13]
- These exercises can be effective when the thoracic spine has not developed a relevant stiffness and when the sagittal curve is not too high: Cobb angles from 44° to 55°. [14]
- Practice normal posture standing and sitting [15][16][17][18][19]
Exercises
- Flexibility exercises to relieve lower extremity contractures eg Hamstrings[20]
- Strengthen core musculature, back extensors . [15][16][17][18][19]
Sports
- Extension sports are advised: such as gymnastics, aerobics, swimming, basketball, cycling and hyperextension exercises.
- Some sports should be discouraged: like sports associated with jumping, marked stress and functional overuse of the back. [21][22]
Postoperative physical therapy
- Necessary and must contain breathing exercises, mobilizations and strengthening exercises. [23]
Scheuermann's disease in adults
- Regarded differently from that of the teenager because the major manifestation is pain and not aesthetic quality.
- The functional rehabilitation on an outpatient basis is the favoured treatment and referral for surgery or dorso-lumbar braces is rare.
The kyphotic posture can be treated with the Schroth method [20]
Examples of Schroth exercises are shown at R
Another treatment regime is outline her, using a different method [24] There are five Principles of Correction:
- Trunk elongation and expansion
- Symmetrical sagittal straightening: identical exercises must be performed for both sides of the trunk (right and left):
Bilateral thoracic expansion in a posterior to anterior (PA) direction to reduce the thoracic hyperkyphosis
Bilateral lumbar expansion in an anterior to posterior (AP) direction to reduce the hyperlordotic low back - Shoulder traction: the traction enhances the expansion of the thorax and corrects the spine
- Correction of breathing: it allows the subject to feel an increased expansion in his/her initially collapsed regions. The goal is to expand the thorax in a back-to-front and a lateral direction.
- Muscle activation by increasing tension: to achieve the best possible correction, muscle balance, stabilization and to increase the proprioceptive input. It helps to integrate the ‘corrected body schema’ in the brain.
- This intensive physical therapy combined with bracing (SpinoMed brace) is successful to treat an adult patient with Scheuermann’s kyphosis. [24]
More clinical trials are necessary to evaluate the effectiveness of conservative interventions, especially different exercises and manual therapies. These should also be combined/compared with braces. [7]
Clinical Bottom Line[edit | edit source]
- The majority of patients are successfully treated with conservative measures as discussed above.
- Pain in the affected region typically improves after skeletal maturity is reached, although patients with Scheuermann kyphosis are at increased risk of chronic back pain as compared to the general population.
- Patients with a kyphotic curve less than 60 degrees at skeletal maturity typically have no long-term sequelae[1]
Key Research[edit | edit source]
- Bezalel T, Kalichman L. Improvement of clinical and radiographical presentation of Scheuermann disease after Schroth therapy treatment. Journal of bodywork and movement therapies. 2015 Apr 1;19(2):232-7.
- Berdishevsky H. Outcome of intensive outpatient rehabilitation and bracing in an adult patient with Scheuermann’s disease evaluated by radiologic imaging—a case report. Scoliosis and spinal disorders. 2016 Oct;11(2):47-51.
Resources[edit | edit source]
Deutchman: Schroth Method Exercises for Scoliosis:
Strott: The Scheuermann’s Disease Fund:
Spine Universe. Scheuermann's Kyphosis (Scheuermann's disease): abnormal curvature of the spine. Available on: www.spineuniverse.com/conditions/kyphosis/scheuermanns-kyphosis-scheuermanns-disease
Tribus C. Medscape Reference. Scheuermann Kyphosis. Available on: emedicine.medscape.com/article/1266349-overview#showall
http://cirrie.buffalo.edu/encyclopedia/en/article/125/
http://www.spine-health.com/conditions/spine-anatomy/lumbar-spine-anatomy-and-pain
http://emedicine.medscape.com/article/1899031-overview#a2
http://www.innerbody.com/anatomy/skeletal/thoracic-vertebrae-lateral
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 1.7 1.8 Mansfield JT, Bennett M. Scheuermann Disease. InStatPearls [Internet] 2019 Jan 17. StatPearls Publishing. Available from:https://www.ncbi.nlm.nih.gov/books/NBK499966/ (last accessed 20.4.2020)
- ↑ 2.0 2.1 2.2 Papagelopoulos PJ, Mavrogenis AF, Savvidou OD, Mitsiokapa EA, Themistocleous GG, Soucacos PN. Current concepts in Scheuermann's kyphosis. Orthopedics (Online). 2008;31(1):52.
- ↑ 3.0 3.1 3.2 Lowe TG, Line BG. Evidence based medicine: analysis of Scheuermann kyphosis. Spine. 2007 Sep 1;32(19):S115-9.
- ↑ 4.0 4.1 4.2 4.3 Weiss H, Turnbull D. Kyphosis (Physical and technical rehabilitation of patients with Scheuermann's disease and kyphosis). International encyclopedia of rehabilitation. 2010.
- ↑ 5.0 5.1 5.2 5.3 Soerensen KH. Scheuermann's juvenile kyphosis. Munksgaard; 1964.
- ↑ 6.0 6.1 6.2 Ristolainen L, Kettunen JA, Heliövaara M, Kujala UM, Heinonen A, Schlenzka D. Untreated Scheuermann’s disease: a 37-year follow-up study. European Spine Journal. 2012 May;21(5):819-24.
- ↑ 7.0 7.1 Bezalel T, Carmeli E, Been E, Kalichman L. Scheuermann's disease: current diagnosis and treatment approach. Journal of back and musculoskeletal rehabilitation. 2014 Jan 1;27(4):383-90.
- ↑ Ali RM, Green DW, Patel TC. Scheuermann's kyphosis. Current opinion in pediatrics. 1999 Feb 1;11(1):70-5.
- ↑ Poolman R, Been H, Ubags L. Clinical outcome and radiographic results after operative treatment of Scheuermann's disease. European Spine Journal. 2002 Dec;11(6):561-9.
- ↑ Lemire JJ, Mierau DR, Crawford CM, Dzus AK. Scheuermann's juvenile kyphosis. Journal of manipulative and physiological therapeutics. 1996 Mar 1;19(3):195-201.
- ↑ 11.0 11.1 Hart ES, Merlin G, Harisiades J, Grottkau BE. Scheuermann's thoracic kyphosis in the adolescent patient. Orthopaedic Nursing. 2010 Nov 1;29(6):365-71.
- ↑ 12.0 12.1 12.2 Advantage Physiotherapy SCHEUERMANN'S DISEASE Available from:https://www.advantagephysiotherapy.com/Injuries-Conditions/Upper-Back-and-Neck/Upper-Back-Issues/Scheuermann-s-Disease/a~5944/article.html (last accessed 20.4.2020)
- ↑ Weiss HR, Turnbull D, Bohr S. Brace treatment for patients with Scheuermann's disease-a review of the literature and first experiences with a new brace design. Scoliosis. 2009 Dec;4(1):1-7.
- ↑ Goodman CC, Fuller KS. Goodman and Fuller’s Pathology E-Book: Implications for the Physical Therapist. 3rd edition Elsevier Health Sciences; 2009.
- ↑ 15.0 15.1 Weiß HR, Dieckmann J, Gerner HJ. Outcome of in-patient rehabilitation in patients with M. Scheuermann evaluated by surface topography. Research into Spinal Deformities 3. 2002:246-9.
- ↑ 16.0 16.1 Weiß HR, Ddeckmann J, Gerner HJ. Effect of intensive rehabilitation on pain in patients with Scheuermann’s disease. InResearch into Spinal Deformities 3 2002 (pp. 254-257). IOS Press.
- ↑ 17.0 17.1 Ball JM, Cagle P, Johnson BE, Lucasey C, Lukert BP. Spinal extension exercises prevent natural progression of kyphosis. Osteoporosis International. 2009 Mar 1;20(3):481.
- ↑ 18.0 18.1 Montgomery SP, Erwin WE. Scheuermann's kyphosis--long-term results of Milwaukee braces treatment. Spine. 1981 Jan 1;6(1):5-8.
- ↑ 19.0 19.1 Zaina F, Atanasio S, Ferraro C, Fusco C, Negrini A, Romano M, Negrini S. Review of rehabilitation and orthopedic conservative approach to sagittal plane diseases during growth: hyperkyphosis, junctional kyphosis, and Scheuermann disease. Eur J Phys Rehabil Med. 2009 Dec 1;45(4):595-603.
- ↑ 20.0 20.1 Bezalel T, Kalichman L. Improvement of clinical and radiographical presentation of Scheuermann disease after Schroth therapy treatment. Journal of bodywork and movement therapies. 2015 Apr 1;19(2):232-7.
- ↑ Damborg F, Engell V, Andersen M, Kyvik KO, Thomsen K. Prevalence, concordance, and heritability of Scheuermann kyphosis based on a study of twins. JBJS. 2006 Oct 1;88(10):2133-6.
- ↑ Sturm PF, Dobson JC, Armstrong GW. The surgical management of Scheuermann's disease. Spine. 1993 May 1;18(6):685-91.
- ↑ Lowe TG. Scheuermann disease. JBJS. 1990 Jul 1;72(6):940-5.
- ↑ 24.0 24.1 Berdishevsky H. Outcome of intensive outpatient rehabilitation and bracing in an adult patient with Scheuermann’s disease evaluated by radiologic imaging—a case report. Scoliosis and spinal disorders. 2016 Oct;11(2):47-51.