Plantar Heel Pain Summary of Important Questions: Difference between revisions
No edit summary |
No edit summary |
||
| Line 10: | Line 10: | ||
== Why Call it Plantar Heel Pain Syndrome? == | == Why Call it Plantar Heel Pain Syndrome? == | ||
Many terms have been used to describe pain under the plantar aspect of the heel but the majority of these terms are related to specific pathologies, even when the actual underlying pathology of pain under the heel remains largely unknown.<ref name=":2">Riel H, Cotchett M, Delahunt E, Rathleff MS, Vicenzino B, Weir A, Landorf KB. [https://sci-hub.se/https://bjsm.bmj.com/content/51/22/1576 Is ‘plantar heel pain’ a more appropriate term than ‘plantar fasciitis’? Time to move on]. Br J Sports Med. 2017; 15(22):1576-1577. </ref><ref>Cotchett M, Rathleff MS, Dilnot M, Landorf KB, Morrissey D, Barton C. [https://link.springer.com/content/pdf/10.1186/s13047-020-0377-3.pdf Lived experience and attitudes of people with plantar heel pain: a qualitative exploration]. Journal of foot and ankle research. 2020 Dec;13(1):1-9. </ref> Many clinicians have focused on the plantar fascia when presented with complaints of pain under the heel, but sufficient evidence now exists to indicate that the plantar fascia is not the only culprit.<ref name=":2" /> The descriptive term | Many terms have been used to describe pain under the plantar aspect of the heel but the majority of these terms are related to specific pathologies, even when the actual underlying pathology of pain under the heel remains largely unknown.<ref name=":2">Riel H, Cotchett M, Delahunt E, Rathleff MS, Vicenzino B, Weir A, Landorf KB. [https://sci-hub.se/https://bjsm.bmj.com/content/51/22/1576 Is ‘plantar heel pain’ a more appropriate term than ‘plantar fasciitis’? Time to move on]. Br J Sports Med. 2017; 15(22):1576-1577. </ref><ref>Cotchett M, Rathleff MS, Dilnot M, Landorf KB, Morrissey D, Barton C. [https://link.springer.com/content/pdf/10.1186/s13047-020-0377-3.pdf Lived experience and attitudes of people with plantar heel pain: a qualitative exploration]. Journal of foot and ankle research. 2020 Dec;13(1):1-9. </ref> Many clinicians have focused on the [[Plantar Aponeurosis|plantar fascia]] when presented with complaints of pain under the heel, but sufficient evidence now exists to indicate that the plantar fascia is not the only culprit.<ref name=":2" /> The descriptive term “[[Introduction to Plantar Heel Pain|Plantar Heel Pain Syndrome]]” (PHPS) was hence proposed to describe the condition of pain under the heel where no differential diagnosis exists.<ref name=":2" /><ref>Ríos-León M, Ortega-Santiago R, Madeleine P, Fernández-de-Las-Peñas C, Plaza-Manzano G. [https://www.jospt.org/doi/abs/10.2519/jospt.2019.8813 Topographical pressure pain sensitivity maps of the feet reveal bilateral pain sensitivity in patients with unilateral plantar heel pain]. Journal of Orthopaedic & Sports Physical Therapy. 2019 Sep;49(9):640-6. </ref> | ||
== Why are Stretches to the Posterior Calf Muscles Helping Patients with PHPS? == | == Why are Stretches to the Posterior Calf Muscles Helping Patients with PHPS? == | ||
Manual palpation of the plantar flexor muscles in the posterior calf on the affected leg in patients with PHPS revealed stiff, incompliant and painful soft tissue.<ref name=":3">Saban B, Deutscher D, Ziv T. [https://www.sciencedirect.com/science/article/abs/pii/S1356689X13001471?via%3Dihub Deep massage to posterior calf muscles in combination with neural mobilization exercises as a treatment for heel pain: a pilot randomized clinical trial]. Manual therapy. 2014 Apr 1;19(2):102-8. </ref> These myofascial restrictions of the posterior calf muscles have been implicated in the development of PHP as it interferes with the extensibility of the muscles and fascia, impeding optimal muscle functioning.<ref name=":3" /><ref name=":4">Pollack Y, Shashua A, Kalichman L. [https://www.sciencedirect.com/science/article/abs/pii/S0958259217300147 Manual therapy for plantar heel pain]. The Foot. 2018 Mar 1;34:11-6 </ref> Damage to the muscle during injury prevents optimal contraction (widening) and relaxation (lengthening) of the muscle and healing of the muscle tissue is through scar tissue, which is less elastic and more fibrous than muscle tissue. | Manual palpation of the plantar flexor muscles in the posterior calf on the affected leg in patients with PHPS revealed stiff, incompliant and painful soft tissue.<ref name=":3">Saban B, Deutscher D, Ziv T. [https://www.sciencedirect.com/science/article/abs/pii/S1356689X13001471?via%3Dihub Deep massage to posterior calf muscles in combination with neural mobilization exercises as a treatment for heel pain: a pilot randomized clinical trial]. Manual therapy. 2014 Apr 1;19(2):102-8. </ref> These myofascial restrictions of the posterior calf muscles have been implicated in the development of PHP as it interferes with the extensibility of the muscles and fascia, impeding optimal muscle functioning.<ref name=":3" /><ref name=":4">Pollack Y, Shashua A, Kalichman L. [https://www.sciencedirect.com/science/article/abs/pii/S0958259217300147 Manual therapy for plantar heel pain]. The Foot. 2018 Mar 1;34:11-6 </ref> Damage to the muscle during injury prevents optimal contraction (widening) and relaxation (lengthening) of the muscle and healing of the muscle tissue is through scar tissue, which is less elastic and more fibrous than muscle tissue. | ||
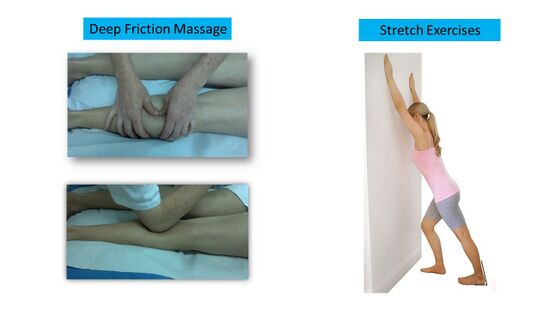
Deep Friction Massage (DFM) supports the muscle to contract and widen effectively as it breaks the adhesions between the muscle fibres limiting the contraction.<ref>Chaves P, Simões D, Paço M, Pinho F, Duarte JA, Ribeiro F. [https://www.mdpi.com/2076-3417/10/8/2705/pdf Pressure Applied during Deep Friction Massage: Characterization and Relationship with Time of Onset of Analgesia]. Applied Sciences. 2020 Jan;10(8):2705. </ref><ref>Farooq N, Aslam S, Bashir N, Awan WA, Shah M, Irshad A. [http://www.imj.com.pk/wp-content/uploads/2020/01/9.-OA-999-09-19-Effectiveness-of-transverse-friction-massage-of-Flexor-digitorum-brevis-and-Calf-muscle.pdf Effectiveness of transverse friction massage of Flexor digitorum brevis and Calf muscle stretching in Plantar fasciitis on foot function index scale: A randomized control trial]. Isra Med J. 2019;11(4):305-9. </ref> It is the stretches, however, that will enable the muscle to recover its full length, improving its ability to relax and narrow.<ref name=":4" /> | [[Deep friction massage|Deep Friction Massage]] (DFM) supports the muscle to contract and widen effectively as it breaks the adhesions between the muscle fibres limiting the contraction.<ref>Chaves P, Simões D, Paço M, Pinho F, Duarte JA, Ribeiro F. [https://www.mdpi.com/2076-3417/10/8/2705/pdf Pressure Applied during Deep Friction Massage: Characterization and Relationship with Time of Onset of Analgesia]. Applied Sciences. 2020 Jan;10(8):2705. </ref><ref>Farooq N, Aslam S, Bashir N, Awan WA, Shah M, Irshad A. [http://www.imj.com.pk/wp-content/uploads/2020/01/9.-OA-999-09-19-Effectiveness-of-transverse-friction-massage-of-Flexor-digitorum-brevis-and-Calf-muscle.pdf Effectiveness of transverse friction massage of Flexor digitorum brevis and Calf muscle stretching in Plantar fasciitis on foot function index scale: A randomized control trial]. Isra Med J. 2019;11(4):305-9. </ref> It is the stretches, however, that will enable the muscle to recover its full length, improving its ability to relax and narrow.<ref name=":4" /> | ||
== Why was the Central Heel Area More Sensitive to Pressure During the Pressure Pain Threshold Studies? == | == Why was the Central Heel Area More Sensitive to Pressure During the Pressure Pain Threshold Studies? == | ||
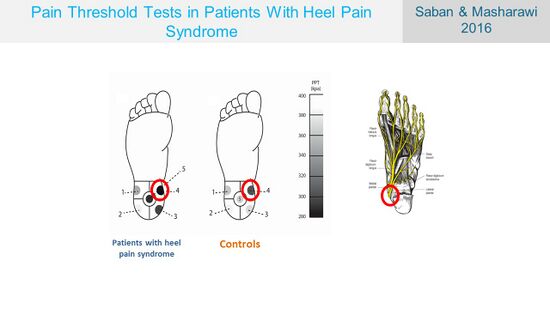
It is not completely clear why the central heel area was so sensitive during the Pressure Pain Threshold (PPT) study performed by Saban & Masharawi <ref name=":5">Saban B, Masharawi Y. [https://sci-hub.se/10.1177/1071100716642038 Pain threshold tests in patients with heel pain syndrome]. Foot & ankle international. 2016 Jul;37(7):730-6. </ref> (Figure 1), especially considering that there are almost no soft tissues in the heel area . No conclusive evidence exists that the fat pad can be a source of pain.<ref name=":6">Bernice Saban. Conclusion of Plantar Heel Pain Syndrome with Practical Demonstrations. PhysioPlus Course. 2021</ref> Anatomically, the medial calcaneal branch of the tibial nerve enters the heel from the medial side and terminates in the skin of the heel, providing sensory innervation to the skin of the heel <ref>Zhang Y, He X, Li J, Ye J, Han W, Zhou S, Zhu J, Wang G, Chen X. [https://link.springer.com/content/pdf/10.1186/s12880-021-00582-8.pdf An MRI study of the tibial nerve in the ankle canal and its branches: a method of multiplanar reformation with 3D-FIESTA-C sequences]. BMC Medical Imaging. 2021 Dec;21(1):1-1. </ref>, which might explain the increased sensitivity to the pressure in this area (Figure 1). | It is not completely clear why the central heel area was so sensitive during the Pressure Pain Threshold (PPT) study performed by Saban & Masharawi <ref name=":5">Saban B, Masharawi Y. [https://sci-hub.se/10.1177/1071100716642038 Pain threshold tests in patients with heel pain syndrome]. Foot & ankle international. 2016 Jul;37(7):730-6. </ref> (Figure 1), especially considering that there are almost no soft tissues in the heel area . No conclusive evidence exists that the fat pad can be a source of pain.<ref name=":6">Bernice Saban. Conclusion of Plantar Heel Pain Syndrome with Practical Demonstrations. PhysioPlus Course. 2021</ref> Anatomically, the medial calcaneal branch of the [[Tibial Nerve|tibial nerve]] enters the heel from the medial side and terminates in the skin of the heel, providing sensory innervation to the skin of the heel <ref>Zhang Y, He X, Li J, Ye J, Han W, Zhou S, Zhu J, Wang G, Chen X. [https://link.springer.com/content/pdf/10.1186/s12880-021-00582-8.pdf An MRI study of the tibial nerve in the ankle canal and its branches: a method of multiplanar reformation with 3D-FIESTA-C sequences]. BMC Medical Imaging. 2021 Dec;21(1):1-1. </ref>, which might explain the increased sensitivity to the pressure in this area (Figure 1). | ||
Figure 1. PPT test sensitivity and the neural anatomy <ref name=":5" /> | [[File:PPT and neural anatomy.jpg|frameless|550x550px]] | ||
'''Figure 1'''. PPT test sensitivity and the neural anatomy <ref name=":5" /> | |||
== Which Risk Factors are Associated with PHPS? == | == Which Risk Factors are Associated with PHPS? == | ||
| Line 33: | Line 35: | ||
== Which Treatment Techniques are Effective for the Management of PHPS? == | == Which Treatment Techniques are Effective for the Management of PHPS? == | ||
Following the literature review on the treatments for PHPS, it is clear that many of the commonly used treatments for PHP are not effective or any better than placebo for the management of PHPS.<ref>Babatunde OO, Legha A, Littlewood C, Chesterton LS, Thomas MJ, Menz HB, van der Windt D, Roddy E. [https://eprints.keele.ac.uk/5014/1/PHP%20NMA%20Manuscript%20updated%20May%202018_Accepted.pdf Comparative effectiveness of treatment options for plantar heel pain: a systematic review with network meta-analysis]. British journal of sports medicine. 2019 Feb 1;53(3):182-94. </ref><ref>Martin RL, Davenport TE, Reischl SF, McPoil TG, Matheson JW, Wukich DK, McDonough CM, Altman RD, Beattie P, Cornwall M, Davis I. [https://www.jospt.org/doi/pdfplus/10.2519/jospt.2014.0303?download=true Heel pain—plantar fasciitis: revision 2014]. Journal of Orthopaedic & Sports Physical Therapy. 2014 Nov;44(11):A1-33. </ref> Saban et al <ref name=":3" />, however, found the use of deep massage therapy combined with stretching exercises and neural mobilisation an effective treatment for PHPS. As other commonly used techniques have not been proven effective for PHPS, they only serve to mislead patients, making them more passive in their treatments.<ref name=":6" /> | Following the literature review on the treatments for PHPS, it is clear that many of the commonly used treatments for PHP are not effective or any better than placebo for the management of PHPS.<ref>Babatunde OO, Legha A, Littlewood C, Chesterton LS, Thomas MJ, Menz HB, van der Windt D, Roddy E. [https://eprints.keele.ac.uk/5014/1/PHP%20NMA%20Manuscript%20updated%20May%202018_Accepted.pdf Comparative effectiveness of treatment options for plantar heel pain: a systematic review with network meta-analysis]. British journal of sports medicine. 2019 Feb 1;53(3):182-94. </ref><ref>Martin RL, Davenport TE, Reischl SF, McPoil TG, Matheson JW, Wukich DK, McDonough CM, Altman RD, Beattie P, Cornwall M, Davis I. [https://www.jospt.org/doi/pdfplus/10.2519/jospt.2014.0303?download=true Heel pain—plantar fasciitis: revision 2014]. Journal of Orthopaedic & Sports Physical Therapy. 2014 Nov;44(11):A1-33. </ref> Saban et al <ref name=":3" />, however, found the use of deep massage therapy combined with stretching exercises and neural mobilisation an effective treatment for PHPS. As other commonly used techniques have not been proven effective for PHPS, they only serve to mislead patients, making them more passive in their treatments.<ref name=":6" /> | ||
The “new protocol” for PHPS:<ref name=":6" /> | |||
The [[A New Protocol for Plantar Heel Pain|“new protocol” for PHPS]]:<ref name=":6" /> | |||
* Relies on our existing physiotherapeutic skills | * Relies on our existing physiotherapeutic skills | ||
| Line 39: | Line 42: | ||
* Is a low tech and low cost intervention | * Is a low tech and low cost intervention | ||
* Is simple, but not easy as it demands a wide scope of knowledge of | * Is simple, but not easy as it demands a wide scope of knowledge of | ||
** what we are doing | ** what we are doing | ||
** why we are doing it (clinical reasoning based on anatomical knowledge) | ** why we are doing it (clinical reasoning based on anatomical knowledge) | ||
** dealing with different patients | ** dealing with different patients | ||
** how to build and manage the treatment sessions | ** how to build and manage the [[Application of the New Protocol for Plantar Heel Pain|treatment sessions]] | ||
== Conclusion == | == Conclusion == | ||
In summary, the key concepts introduced and explored in this course included: | In summary, the key concepts introduced and explored in this course included: | ||
* Basic information about PHPS - the function of the heel in the gait cycle, pain location and behaviour, prevalence of PHPS | * Basic information about PHPS - the function of the heel in the [[Gait Cycle|gait cycle]], pain location and behaviour, prevalence of PHPS | ||
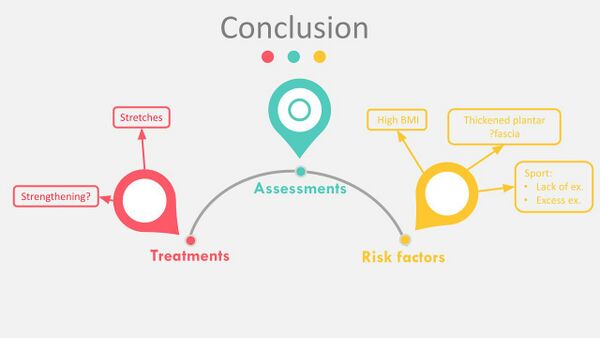
* In-depth literature review on the risk factors for PHPS and the assessment and treatment thereof (Figure 2) | * In-depth literature review on the [[Risk Factors for the Development of Plantar Heel Pain Syndrome - A Literature Review|risk factors]] for PHPS and the [[Assessment of Plantar Heel Pain - A Literature Review|assessment]] and [[Treatment of Plantar Heel Pain - A Literature Review|treatment]] thereof (Figure 2) | ||
* Clear identification of the need for a different approach for the effective management of PHPS | * Clear identification of the need for a different approach for the effective management of PHPS | ||
Figure 2. Known variables from the literature reviews on risk factors, assessment and treatment of PHPS | [[File:Conclusion on literature reviews on PHPS.jpg|frameless|600x600px]] | ||
The | |||
'''Figure 2'''. Known variables from the literature reviews on risk factors, assessment and treatment of PHPS <ref name=":6" /> | |||
The “[[A New Protocol for Plantar Heel Pain|new protocol]]” started with the observation of a poorly understood reaction to two commonly used assessment tests - the heelrise test and the minisquat test. Ultimately, it provided the means for the enhanced management of PHPS, through the use of the: | |||
* Assessment tool (Figure 3)<ref name=":7">Saban B, Masharawi Y. [https://www.physiotherapyjournal.com/article/S0031-9406(16)30032-3/fulltext Three single leg standing tests for clinical assessment of chronic plantar heel pain syndrome: static stance, half-squat and heel rise]. Physiotherapy. 2017 Jun 1;103(2):237-44. </ref> | * [[A New Protocol for Plantar Heel Pain|Assessment tool]] (Figure 3)<ref name=":7">Saban B, Masharawi Y. [https://www.physiotherapyjournal.com/article/S0031-9406(16)30032-3/fulltext Three single leg standing tests for clinical assessment of chronic plantar heel pain syndrome: static stance, half-squat and heel rise]. Physiotherapy. 2017 Jun 1;103(2):237-44. </ref> | ||
* Manual therapy (Figure 4)<ref name=":3" /> | * [[The Theory and Practice of Massage and Exercise for Plantar Heel Pain|Manual therapy]] (Figure 4)<ref name=":3" /> | ||
* Exercises (Figure 4) <ref name=":3" /> | * Exercises (Figure 4) <ref name=":3" /> | ||
[[File:Description of clinical tests used for Ax of PHPS.jpg|frameless|700x700px]]'''Figure 3'''. Clinical tests in the assessment tool <ref name=":7" /> | |||
[[File:New Protocol treatment.jpg|frameless|550x550px]] | |||
Figure 4. Treatment following the New Protocol <ref name=":6" /> | '''Figure 4'''. Treatment following the New Protocol <ref name=":6" /> | ||
== Resources == | == Resources == | ||
| Line 78: | Line 85: | ||
<references /> | <references /> | ||
[[Category:Musculoskeletal/Orthopaedics]] | |||
[[Category:Foot]] | |||
[[Category:Foot - Assessment and Examination]] | |||
[[Category:Foot - Interventions]] | |||
[[Category:Course Pages]] | |||
[[Category:Physioplus Content]] | |||
Revision as of 23:19, 25 October 2021
Original Editor - User Name
Top Contributors - Merinda Rodseth and Kim Jackson
Introduction[edit | edit source]
Plantar heel pain (PHP) is a complex and multifactorial condition with many factors proposed to be associated with it.[1][2] The aetiology of PHP is generally not well understood which causes uncertainty regarding the most effective management thereof, making the condition difficult to effectively treat.[1][2] Following this, many questions arose during this series on PHP, which will can now be answered, based on the literature discussed.
Why Call it Plantar Heel Pain Syndrome?[edit | edit source]
Many terms have been used to describe pain under the plantar aspect of the heel but the majority of these terms are related to specific pathologies, even when the actual underlying pathology of pain under the heel remains largely unknown.[3][4] Many clinicians have focused on the plantar fascia when presented with complaints of pain under the heel, but sufficient evidence now exists to indicate that the plantar fascia is not the only culprit.[3] The descriptive term “Plantar Heel Pain Syndrome” (PHPS) was hence proposed to describe the condition of pain under the heel where no differential diagnosis exists.[3][5]
Why are Stretches to the Posterior Calf Muscles Helping Patients with PHPS?[edit | edit source]
Manual palpation of the plantar flexor muscles in the posterior calf on the affected leg in patients with PHPS revealed stiff, incompliant and painful soft tissue.[6] These myofascial restrictions of the posterior calf muscles have been implicated in the development of PHP as it interferes with the extensibility of the muscles and fascia, impeding optimal muscle functioning.[6][7] Damage to the muscle during injury prevents optimal contraction (widening) and relaxation (lengthening) of the muscle and healing of the muscle tissue is through scar tissue, which is less elastic and more fibrous than muscle tissue.
Deep Friction Massage (DFM) supports the muscle to contract and widen effectively as it breaks the adhesions between the muscle fibres limiting the contraction.[8][9] It is the stretches, however, that will enable the muscle to recover its full length, improving its ability to relax and narrow.[7]
Why was the Central Heel Area More Sensitive to Pressure During the Pressure Pain Threshold Studies?[edit | edit source]
It is not completely clear why the central heel area was so sensitive during the Pressure Pain Threshold (PPT) study performed by Saban & Masharawi [10] (Figure 1), especially considering that there are almost no soft tissues in the heel area . No conclusive evidence exists that the fat pad can be a source of pain.[11] Anatomically, the medial calcaneal branch of the tibial nerve enters the heel from the medial side and terminates in the skin of the heel, providing sensory innervation to the skin of the heel [12], which might explain the increased sensitivity to the pressure in this area (Figure 1).
Figure 1. PPT test sensitivity and the neural anatomy [10]
Which Risk Factors are Associated with PHPS?[edit | edit source]
The literature review on risk factors associated with PHPS found no particular risk factors for the development of PHPS. However, individuals who were:
- Overweight
- Under exercising/sedentary
- Over exercising
could be at a slightly higher risk for developing PHPS.[6][13][14]
Which Treatment Techniques are Effective for the Management of PHPS?[edit | edit source]
Following the literature review on the treatments for PHPS, it is clear that many of the commonly used treatments for PHP are not effective or any better than placebo for the management of PHPS.[15][16] Saban et al [6], however, found the use of deep massage therapy combined with stretching exercises and neural mobilisation an effective treatment for PHPS. As other commonly used techniques have not been proven effective for PHPS, they only serve to mislead patients, making them more passive in their treatments.[11]
The “new protocol” for PHPS:[11]
- Relies on our existing physiotherapeutic skills
- Upgraded our assessment and treatment skills
- Is a low tech and low cost intervention
- Is simple, but not easy as it demands a wide scope of knowledge of
- what we are doing
- why we are doing it (clinical reasoning based on anatomical knowledge)
- dealing with different patients
- how to build and manage the treatment sessions
Conclusion[edit | edit source]
In summary, the key concepts introduced and explored in this course included:
- Basic information about PHPS - the function of the heel in the gait cycle, pain location and behaviour, prevalence of PHPS
- In-depth literature review on the risk factors for PHPS and the assessment and treatment thereof (Figure 2)
- Clear identification of the need for a different approach for the effective management of PHPS
Figure 2. Known variables from the literature reviews on risk factors, assessment and treatment of PHPS [11]
The “new protocol” started with the observation of a poorly understood reaction to two commonly used assessment tests - the heelrise test and the minisquat test. Ultimately, it provided the means for the enhanced management of PHPS, through the use of the:
- Assessment tool (Figure 3)[17]
- Manual therapy (Figure 4)[6]
- Exercises (Figure 4) [6]
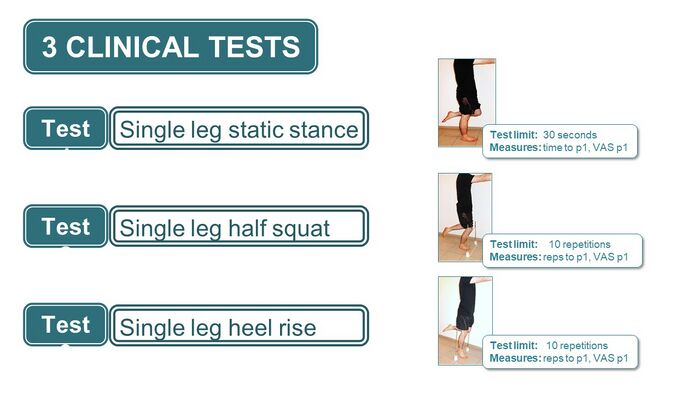 Figure 3. Clinical tests in the assessment tool [17]
Figure 3. Clinical tests in the assessment tool [17]
Figure 4. Treatment following the New Protocol [11]
Resources[edit | edit source]
- bulleted list
- x
or
- numbered list
- x
References[edit | edit source]
- ↑ 1.0 1.1 Sullivan J, Pappas E, Burns J. Role of mechanical factors in the clinical presentation of plantar heel pain: implications for management. The Foot. 2020 Mar 1;42:101636.
- ↑ 2.0 2.1 Thomas MJ, Whittle R, Menz HB, Rathod-Mistry T, Marshall M, Roddy E. Plantar heel pain in middle-aged and older adults: population prevalence, associations with health status and lifestyle factors, and frequency of healthcare use. BMC musculoskeletal disorders. 2019 Dec;20(1):1-8.
- ↑ 3.0 3.1 3.2 Riel H, Cotchett M, Delahunt E, Rathleff MS, Vicenzino B, Weir A, Landorf KB. Is ‘plantar heel pain’ a more appropriate term than ‘plantar fasciitis’? Time to move on. Br J Sports Med. 2017; 15(22):1576-1577.
- ↑ Cotchett M, Rathleff MS, Dilnot M, Landorf KB, Morrissey D, Barton C. Lived experience and attitudes of people with plantar heel pain: a qualitative exploration. Journal of foot and ankle research. 2020 Dec;13(1):1-9.
- ↑ Ríos-León M, Ortega-Santiago R, Madeleine P, Fernández-de-Las-Peñas C, Plaza-Manzano G. Topographical pressure pain sensitivity maps of the feet reveal bilateral pain sensitivity in patients with unilateral plantar heel pain. Journal of Orthopaedic & Sports Physical Therapy. 2019 Sep;49(9):640-6.
- ↑ 6.0 6.1 6.2 6.3 6.4 6.5 Saban B, Deutscher D, Ziv T. Deep massage to posterior calf muscles in combination with neural mobilization exercises as a treatment for heel pain: a pilot randomized clinical trial. Manual therapy. 2014 Apr 1;19(2):102-8.
- ↑ 7.0 7.1 Pollack Y, Shashua A, Kalichman L. Manual therapy for plantar heel pain. The Foot. 2018 Mar 1;34:11-6
- ↑ Chaves P, Simões D, Paço M, Pinho F, Duarte JA, Ribeiro F. Pressure Applied during Deep Friction Massage: Characterization and Relationship with Time of Onset of Analgesia. Applied Sciences. 2020 Jan;10(8):2705.
- ↑ Farooq N, Aslam S, Bashir N, Awan WA, Shah M, Irshad A. Effectiveness of transverse friction massage of Flexor digitorum brevis and Calf muscle stretching in Plantar fasciitis on foot function index scale: A randomized control trial. Isra Med J. 2019;11(4):305-9.
- ↑ 10.0 10.1 Saban B, Masharawi Y. Pain threshold tests in patients with heel pain syndrome. Foot & ankle international. 2016 Jul;37(7):730-6.
- ↑ 11.0 11.1 11.2 11.3 11.4 Bernice Saban. Conclusion of Plantar Heel Pain Syndrome with Practical Demonstrations. PhysioPlus Course. 2021
- ↑ Zhang Y, He X, Li J, Ye J, Han W, Zhou S, Zhu J, Wang G, Chen X. An MRI study of the tibial nerve in the ankle canal and its branches: a method of multiplanar reformation with 3D-FIESTA-C sequences. BMC Medical Imaging. 2021 Dec;21(1):1-1.
- ↑ Van Leeuwen KD, Rogers J, Winzenberg T, van Middelkoop M. Higher body mass index is associated with plantar fasciopathy/‘plantar fasciitis’: systematic review and meta-analysis of various clinical and imaging risk factors. British journal of sports medicine. 2016 Aug 1;50(16):972-81.
- ↑ Menz HB, Thomas MJ, Marshall M, Rathod-Mistry T, Hall A, Chesterton LS, Peat GM, Roddy E. Coexistence of plantar calcaneal spurs and plantar fascial thickening in individuals with plantar heel pain. Rheumatology. 2019 Feb 1;58(2):237-45.
- ↑ Babatunde OO, Legha A, Littlewood C, Chesterton LS, Thomas MJ, Menz HB, van der Windt D, Roddy E. Comparative effectiveness of treatment options for plantar heel pain: a systematic review with network meta-analysis. British journal of sports medicine. 2019 Feb 1;53(3):182-94.
- ↑ Martin RL, Davenport TE, Reischl SF, McPoil TG, Matheson JW, Wukich DK, McDonough CM, Altman RD, Beattie P, Cornwall M, Davis I. Heel pain—plantar fasciitis: revision 2014. Journal of Orthopaedic & Sports Physical Therapy. 2014 Nov;44(11):A1-33.
- ↑ 17.0 17.1 Saban B, Masharawi Y. Three single leg standing tests for clinical assessment of chronic plantar heel pain syndrome: static stance, half-squat and heel rise. Physiotherapy. 2017 Jun 1;103(2):237-44.