Physiotherapy Management for Sexual Dysfunction in Men: Difference between revisions
No edit summary |
(Added links to references) |
||
| (19 intermediate revisions by 5 users not shown) | |||
| Line 2: | Line 2: | ||
== Introduction == | == Introduction == | ||
Sexual dysfunction is defined as a complication occurring in any phase of the sexual response cycle. The phases of the sexual response cycle include; | Sexual dysfunction is defined as a complication occurring in any phase of the sexual response cycle. The phases of the sexual response cycle include; desire, arousal, orgasm, and resolution<ref>deGROAT WC, BOOTH AM. [https://www.acpjournals.org/doi/abs/10.7326/0003-4819-92-2-329 Physiology of male sexual function]. Annals of internal medicine. 1980 Feb 1;92(2_Part_2):329-31.</ref>. Sexual dysfunction is extremely common among women and men, and effective treatment is available. However, few individuals seek help as many, even healthcare professionals, are often embarrassed and hesitant to discuss the topic. | ||
Sexual dysfunction, although less common in men, still affects 31% of men and has a large impact on the quality of life as well as interpersonal relationships<ref>Rosen RC. Prevalence and risk factors of sexual dysfunction in men and women. Current psychiatry reports. 2000 Jun 1;2(3):189-95.</ref>. | Sexual dysfunction, although less common in men, still affects 31% of men and has a large impact on the quality of life as well as interpersonal relationships<ref>Rosen RC. [https://link.springer.com/article/10.1007/s11920-996-0006-2 Prevalence and risk factors of sexual dysfunction in men and women]. Current psychiatry reports. 2000 Jun 1;2(3):189-95.</ref>. | ||
Sexual desire/interest, arousal, orgasm, and sexual pain are the four main categories of sexual dysfunction. | |||
== Risk | Sexual dysfunction may include; | ||
* Psychological | * Sexual desire dysfunctions (Sexual aversion disorder), | ||
* | * Sexual arousal dysfunctions, | ||
* Erectile dysfunction, | |||
* Premature ejaculation, | |||
* Anejaculation (inability to ejaculate), | |||
* Orgasmic dysfunction, | |||
* Priapism (persistent and painful erection of the penis, in the absence of sexual arousal) | |||
* Peyronie’s disease (a bent, rather than straight, erect penis due to scar tissue)<ref>Hatzimouratidis K, Hatzichristou D. [https://www.sciencedirect.com/science/article/pii/S1743609515314892 Sexual dysfunctions: classifications and definitions]. The journal of sexual medicine. 2007 Jan 1;4(1):241-50.</ref>. | |||
Erectile dysfunction ( 5–20% of men) and premature ejaculation (20–30% of men) are the most common male sexual dysfunctions<ref>Hatzimouratidis K, Amar E, Eardley I, Giuliano F, Hatzichristou D, Montorsi F, Vardi Y, Wespes E. [https://www.sciencedirect.com/science/article/pii/S0302283810001338 Guidelines on male sexual dysfunction: erectile dysfunction and premature ejaculation]. European urology. 2010 May 1;57(5):804-14.</ref>. | |||
== Risk Factors == | |||
* Psychological conditions (eg. [[Depression]], anxiety and the medication used to treat these conditions) | |||
* Medical conditions (eg. [[Diabetes]], [[Coronary Artery Disease (CAD)|heart disease]], [[stroke]], [[Urinary Tract Infection|urinary tract disorders]], [[Chronic Disease|chronic illnesses]]) | |||
* [[Substance Use Disorder|Substance abuse]] | |||
* Increase with age | * Increase with age | ||
* Prostate cancer | * [[Sexual Dysfunction After Prostate Cancer|Prostate cancer]] | ||
* Chronic prostatitis/chronic pelvic pain syndrome<ref name=":0">Cohen D, Gonzalez J, Goldstein I. The role of pelvic floor muscles in male sexual dysfunction and pelvic pain. Sexual medicine reviews. 2016 Jan 1;4(1):53-62.</ref> | * Surgical complications in the anatomical region | ||
* Chronic prostatitis/chronic pelvic pain syndrome<ref name=":0">Cohen D, Gonzalez J, Goldstein I. [https://www.sciencedirect.com/science/article/pii/S2050052115000025 The role of pelvic floor muscles in male sexual dysfunction and pelvic pain]. Sexual medicine reviews. 2016 Jan 1;4(1):53-62.</ref><ref>McCabe MP, Sharlip ID, Lewis R, Atalla E, Balon R, Fisher AD, Laumann E, Lee SW, Segraves RT. [https://www.sciencedirect.com/science/article/pii/S1743609515000508 Risk factors for sexual dysfunction among women and men: a consensus statement from the Fourth International Consultation on Sexual Medicine 2015]. The journal of sexual medicine. 2016 Feb 1;13(2):153-67.</ref> | |||
* [[Lumbar Spinal Stenosis|Lumbar spine stenosis]]/ transient [[Cauda Equina Syndrome|cauda equina]] compression<ref>Barbaro K, Midgley J. [https://www.sciencedirect.com/science/article/abs/pii/S2468781221000217#fig1 Priapism, a symptom of claudication of the cauda equina in spinal stenosis.] Musculoskeletal Science and Practice. 2021 Apr 1;52:102337.</ref> | |||
== Anatomy | == Anatomy and Physiology == | ||
Below is a brief overview of the anatomy and physiology of the pelvic region. For detailed information on the anatomy the pelvic floor you can read more [[Pelvic Floor Anatomy|here]] | |||
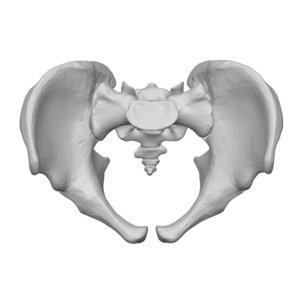
=== Bony | === Bony Structures === | ||
Pelvic cavity; | |||
* Sacrum & coccyx | * Sacrum & coccyx | ||
* Left and Right innominate bones (ilium, ischium & pubis) | * Left and Right innominate bones (ilium, ischium & pubis) | ||
* Pectineal line | * Pectineal line | ||
* Pubic crest<ref name=":0" /> | * Pubic crest<ref name=":0" /> | ||
[[File:Pelvic cavity.png|none|thumb]] | |||
=== Musculature | === Musculature === | ||
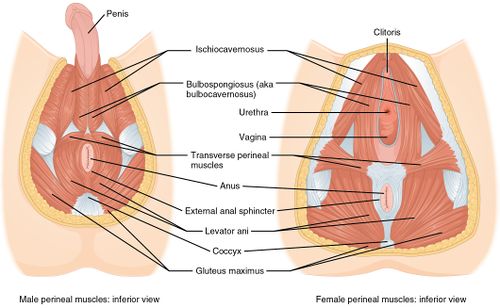
The pelvic floor consists of 3 layers; | The pelvic floor consists of 3 layers<ref name=":0" />; | ||
Most superficial layer | Most superficial layer | ||
* | * Bulbospongiosus m. | ||
* | * Ischiocavernosus m. | ||
* | * Superficial transverse perineal m. | ||
* | * External anal sphincter | ||
The second layer (the urogenital diaphragm) | The second layer (the urogenital diaphragm) | ||
* | * Deep transverse perineal, | ||
* | * Sphincter urethrae, | ||
* | * Compressor urethrae | ||
This layer mainly assists with urethral closure during raised intra-abdominal pressure & plays a role in stabilising the pelvis and lumbar joints. | |||
The third layer (the pelvic diaphragm) | The third layer (the pelvic diaphragm) | ||
| Line 43: | Line 59: | ||
Contraction of the Levator ani muscles maintain anal continence when contracted and allow the evacuation of bowel when relaxed. It also supports the pelvic organs. | Contraction of the Levator ani muscles maintain anal continence when contracted and allow the evacuation of bowel when relaxed. It also supports the pelvic organs. | ||
The obturator internus muscle does not form part of the pelvic floor muscles but still has an effect on the elevation of pelvic organs. | The [[Obturator Internus|obturator internus]] muscle does not form part of the pelvic floor muscles but still has an effect on the elevation of pelvic organs. | ||
[[File:Pelvic floor muscles.jpg|none|thumb| | [[File:Pelvic floor muscles.jpg|none|thumb|500x500px]] | ||
The pelvic floor muscles form a dome-shaped structure that | The pelvic floor muscles form a dome-shaped structure that encloses the pelvic cavity. | ||
The functions of the pelvic floor muscles include; | The functions of the pelvic floor muscles include; | ||
| Line 56: | Line 72: | ||
# Controls continence (urinary & fecal) | # Controls continence (urinary & fecal) | ||
=== Innervation | === Innervation === | ||
The innervation of pelvic floor muscles is from sympathetic, parasympathetic, and somatic nerve fibres. | The innervation of pelvic floor muscles is from sympathetic, parasympathetic, and somatic nerve fibres<ref name=":0" />. | ||
Nerves responsible for pelvic floor functioning; | Nerves that are mainly responsible for pelvic floor functioning; | ||
# Hypogastric nerve | # Hypogastric nerve | ||
# Pudendal nerve | # Pudendal nerve | ||
| Line 65: | Line 81: | ||
== Physiotherapy Management == | == Physiotherapy Management == | ||
=== Assessment === | |||
Individuals with these conditions generally get referred from specialists following screening for possible cancers and/ or urethral complications. | |||
It's important to rule out any other sources that may refer to the pelvic floor area such as; | |||
** Lx spine & Neurodynamics | |||
** Hip | |||
** Breathing pattern | |||
** SIJ provocation tests | |||
** Abdominal palpation (assess Trigger Points in Rectus Abdominis, Internal Obliques, External Obliques, Transverse Abdominis) | |||
Physiotherapists that have specialised in the pelvic floor can complete pelvic floor palpation and feel for trigger points in the puborectalis, obturator, and the coccygeus/ iliococcygeus/ iliococcygeus muscles. | |||
Assessment should also include activation pattern, endurance, speed of contraction and questionnaires<ref name=":2">Hodges, Milios, Jones, Greene, Nwankwo. Focused symposium: MEN´S HEALTH: A GLOBAL PROBLEM AND NEW FRONTIER FOR PHYSIOTHERAPY. 2017, July 4.</ref>. | |||
=== Treatment === | === Treatment === | ||
Studies indicate that pelvic floor muscle training is effective in treating erectile dysfunction, ejaculation complications and chronic pelvic pain. | Studies indicate that [[Kegel's Exercise : Males|pelvic floor muscle training]] is effective in treating erectile dysfunction, ejaculation complications and chronic pelvic pain<ref name=":0" />. | ||
=== Common Complications and Relevance to Physiotherapy<ref name=":0" /><ref name=":1">Rosenbaum TY. REVIEWS: [https://www.sciencedirect.com/science/article/pii/S1743609515314934 Pelvic floor involvement in male and female sexual dysfunction and the role of pelvic floor rehabilitation in treatment: a literature review]. The journal of sexual medicine. 2007 Jan 1;4(1):4-13.</ref> === | |||
==== Erectile Dysfunction (ED) ==== | |||
Literature has indicated that between 9-40% of men struggle with erectile dysfunction by age 40 and raises 10% each decade after 40. Erectile dysfunction is defined as the inability to either obtain and/or maintain a rigid erection sufficient for penetration. | Literature has indicated that between 9-40% of men struggle with erectile dysfunction by age 40 and raises 10% each decade after 40. Erectile dysfunction is defined as the inability to either obtain and/or maintain a rigid erection sufficient for penetration. | ||
The muscles responsible for erection are; the bulbospongiosus and ischiocavernosus muscles. Strengthening voluntary contraction of the ischiocavernosus muscle relaxation techniques in cases of high pelvic floor muscle tone (spasms or increased tone may prevent adequate blood flow necessary for erection) have been proven to be an effective treatment. | The muscles responsible for erection are; the bulbospongiosus and ischiocavernosus muscles. Strengthening the voluntary contraction of the ischiocavernosus muscle and relaxation techniques in cases of high pelvic floor muscle tone (spasms or increased tone may prevent adequate blood flow necessary for erection) have been proven to be an effective treatment<ref name=":0" />. | ||
Emphasis should be placed on isolation and activation of specific trunk and pelvic floor muscles. Home exercise programmes (HEP) should include pelvic floor strengthening exercises with different positioning and intensity. | |||
Studies indicated that 47% of men with ED recovered completely, following a 4-12 month programme including pelvic floor exercise, biofeedback, and electrical stimulation<ref name=":1" />. | |||
==== Ejaculatory Dysfunction ==== | |||
During ejaculation contraction of the smooth muscles of the prostate gland and the bladder neck occur, as well as relaxation of the urethral sphincter. | |||
' | The muscle responsible for ejaculation is the bulbospongiosus muscle. As premature ejaculation (PE) is among the most common sexual dysfunction cases in men, pelvic floor exercises, biofeedback and electrostimulation are proven to improve control and duration. It's important to include isometric pelvic floor contractions in supine and standing<ref name=":0" /><ref name=":1" />. | ||
Behavioural changes are also beneficial and include; pre-intercourse masturbation, frequent sexual activity or stopping intercourse intermittently with sustained contraction/ internal squeeze<ref name=":0" />. | |||
Studies indicate that 61% of men with PE reported improvement in control of ejaculation following 15-20 sessions of the pelvic floor therapy<ref name=":1" />. | |||
==== Chronic Prostatitis/ Chronic Pelvic Pain Syndrome ==== | |||
Chronic Prostatitis/ Chronic Pelvic Pain Syndrome is defined as pelvic -, abdomen - and genital pain without symptoms of urinary tract infection. This most commonly occurs during or after ejaculation. | Chronic Prostatitis/ Chronic Pelvic Pain Syndrome is defined as pelvic -, abdomen - and genital pain without symptoms of urinary tract infection. This most commonly occurs during or after ejaculation. | ||
Motor control exercises emphasising on the relaxation of levator ani muscles (if increased tone is present) and coordinated activation-deactivation exercises with biofeedback methods are an extremely beneficial treatment for men with Chronic Prostatitis/ Chronic Pelvic Pain Syndrome. | Motor control exercises emphasising on the relaxation of levator ani muscles (if the increased tone is present) and coordinated activation-deactivation exercises with biofeedback methods are an extremely beneficial treatment for men with Chronic Prostatitis/ Chronic Pelvic Pain Syndrome. | ||
Soft tissue mobilisation, myofascial release and manipulation are also beneficial if the physiotherapist has undergone adequate and specialised training<ref name=":0" />. | |||
==== Urinary Incontinence ==== | |||
Sexual dysfunction is highly related to urinary dysfunction in men and women. Treatment techniques include voiding rehabilitation and bladder retraining - active pelvic floor muscle contractions to inhibit bladder contraction. This will prevent the detrusor urinae muscle contraction<ref name=":1" />. | |||
=== Other Treatment Techniques === | |||
If increased tone or spasms have been identified as the underlying problem after assessment the following techniques are indicated for the treatment; | |||
* Myofascial release (for specialised pelvic floor therapists) | |||
* Self-release education (for specialised pelvic floor therapists) | |||
* Trigger Point therapy | |||
* Global Therapeutic Massage | |||
Education regarding behavioural changes includes; diet and weight management<ref name=":2" />. | |||
==== Cue's For Pelvic Floor Retraining ==== | |||
* 'Stop the flow' | |||
* 'Shorten the penis' | |||
* 'Lift the pelvic floor or scrotum' | |||
* 'Prevent passing gas' | |||
* 'Tighten around the anus'<ref name=":2" /> | |||
{{#ev:youtube|dSqK4_3YSMI|300}}<ref>Michelle Kenway. How to Kegel for Men - Professional Guide to Effective Kegel Strength Exercises. Available from: https://www.youtube.com/watch?v=dSqK4_3YSMI [last accessed 3/18/2020]</ref> | |||
. | == Conclusion == | ||
Emphasis on pelvic floor rehabilitation is often associated with women, however, pelvic floor dysfunction is also common among men. Literature and studies indicate that pelvic floor rehabilitation and physiotherapy management can be effective in treating many conditions such as; erectile dysfunction, ejaculatory dysfunction, Chronic Prostatitis/ Chronic Pelvic Pain Syndrome and urinary incontinence. | |||
== References == | == References == | ||
<references /> | <references /> | ||
[[Category:Mens Health]] | |||
Latest revision as of 10:05, 7 August 2022
Introduction[edit | edit source]
Sexual dysfunction is defined as a complication occurring in any phase of the sexual response cycle. The phases of the sexual response cycle include; desire, arousal, orgasm, and resolution[1]. Sexual dysfunction is extremely common among women and men, and effective treatment is available. However, few individuals seek help as many, even healthcare professionals, are often embarrassed and hesitant to discuss the topic.
Sexual dysfunction, although less common in men, still affects 31% of men and has a large impact on the quality of life as well as interpersonal relationships[2].
Sexual desire/interest, arousal, orgasm, and sexual pain are the four main categories of sexual dysfunction.
Sexual dysfunction may include;
- Sexual desire dysfunctions (Sexual aversion disorder),
- Sexual arousal dysfunctions,
- Erectile dysfunction,
- Premature ejaculation,
- Anejaculation (inability to ejaculate),
- Orgasmic dysfunction,
- Priapism (persistent and painful erection of the penis, in the absence of sexual arousal)
- Peyronie’s disease (a bent, rather than straight, erect penis due to scar tissue)[3].
Erectile dysfunction ( 5–20% of men) and premature ejaculation (20–30% of men) are the most common male sexual dysfunctions[4].
Risk Factors[edit | edit source]
- Psychological conditions (eg. Depression, anxiety and the medication used to treat these conditions)
- Medical conditions (eg. Diabetes, heart disease, stroke, urinary tract disorders, chronic illnesses)
- Substance abuse
- Increase with age
- Prostate cancer
- Surgical complications in the anatomical region
- Chronic prostatitis/chronic pelvic pain syndrome[5][6]
- Lumbar spine stenosis/ transient cauda equina compression[7]
Anatomy and Physiology[edit | edit source]
Below is a brief overview of the anatomy and physiology of the pelvic region. For detailed information on the anatomy the pelvic floor you can read more here
Bony Structures[edit | edit source]
Pelvic cavity;
- Sacrum & coccyx
- Left and Right innominate bones (ilium, ischium & pubis)
- Pectineal line
- Pubic crest[5]
Musculature[edit | edit source]
The pelvic floor consists of 3 layers[5];
Most superficial layer
- Bulbospongiosus m.
- Ischiocavernosus m.
- Superficial transverse perineal m.
- External anal sphincter
The second layer (the urogenital diaphragm)
- Deep transverse perineal,
- Sphincter urethrae,
- Compressor urethrae
This layer mainly assists with urethral closure during raised intra-abdominal pressure & plays a role in stabilising the pelvis and lumbar joints.
The third layer (the pelvic diaphragm)
- Levator ani (Pubococcygeus & Ischiococcygeus)
- Iliococcygeus,
Contraction of the Levator ani muscles maintain anal continence when contracted and allow the evacuation of bowel when relaxed. It also supports the pelvic organs.
The obturator internus muscle does not form part of the pelvic floor muscles but still has an effect on the elevation of pelvic organs.
The pelvic floor muscles form a dome-shaped structure that encloses the pelvic cavity.
The functions of the pelvic floor muscles include;
- Stabilising pelvic joints
- Support internal pelvic organs
- Voluntary contraction of urethral and anal sphincters
- Regulate erection, emission and ejaculation
- Controls continence (urinary & fecal)
Innervation[edit | edit source]
The innervation of pelvic floor muscles is from sympathetic, parasympathetic, and somatic nerve fibres[5].
Nerves that are mainly responsible for pelvic floor functioning;
- Hypogastric nerve
- Pudendal nerve
- Levator ani nerve
Physiotherapy Management[edit | edit source]
Assessment[edit | edit source]
Individuals with these conditions generally get referred from specialists following screening for possible cancers and/ or urethral complications.
It's important to rule out any other sources that may refer to the pelvic floor area such as;
- Lx spine & Neurodynamics
- Hip
- Breathing pattern
- SIJ provocation tests
- Abdominal palpation (assess Trigger Points in Rectus Abdominis, Internal Obliques, External Obliques, Transverse Abdominis)
Physiotherapists that have specialised in the pelvic floor can complete pelvic floor palpation and feel for trigger points in the puborectalis, obturator, and the coccygeus/ iliococcygeus/ iliococcygeus muscles.
Assessment should also include activation pattern, endurance, speed of contraction and questionnaires[8].
Treatment[edit | edit source]
Studies indicate that pelvic floor muscle training is effective in treating erectile dysfunction, ejaculation complications and chronic pelvic pain[5].
Common Complications and Relevance to Physiotherapy[5][9][edit | edit source]
Erectile Dysfunction (ED)[edit | edit source]
Literature has indicated that between 9-40% of men struggle with erectile dysfunction by age 40 and raises 10% each decade after 40. Erectile dysfunction is defined as the inability to either obtain and/or maintain a rigid erection sufficient for penetration.
The muscles responsible for erection are; the bulbospongiosus and ischiocavernosus muscles. Strengthening the voluntary contraction of the ischiocavernosus muscle and relaxation techniques in cases of high pelvic floor muscle tone (spasms or increased tone may prevent adequate blood flow necessary for erection) have been proven to be an effective treatment[5].
Emphasis should be placed on isolation and activation of specific trunk and pelvic floor muscles. Home exercise programmes (HEP) should include pelvic floor strengthening exercises with different positioning and intensity.
Studies indicated that 47% of men with ED recovered completely, following a 4-12 month programme including pelvic floor exercise, biofeedback, and electrical stimulation[9].
Ejaculatory Dysfunction[edit | edit source]
During ejaculation contraction of the smooth muscles of the prostate gland and the bladder neck occur, as well as relaxation of the urethral sphincter.
The muscle responsible for ejaculation is the bulbospongiosus muscle. As premature ejaculation (PE) is among the most common sexual dysfunction cases in men, pelvic floor exercises, biofeedback and electrostimulation are proven to improve control and duration. It's important to include isometric pelvic floor contractions in supine and standing[5][9].
Behavioural changes are also beneficial and include; pre-intercourse masturbation, frequent sexual activity or stopping intercourse intermittently with sustained contraction/ internal squeeze[5].
Studies indicate that 61% of men with PE reported improvement in control of ejaculation following 15-20 sessions of the pelvic floor therapy[9].
Chronic Prostatitis/ Chronic Pelvic Pain Syndrome[edit | edit source]
Chronic Prostatitis/ Chronic Pelvic Pain Syndrome is defined as pelvic -, abdomen - and genital pain without symptoms of urinary tract infection. This most commonly occurs during or after ejaculation.
Motor control exercises emphasising on the relaxation of levator ani muscles (if the increased tone is present) and coordinated activation-deactivation exercises with biofeedback methods are an extremely beneficial treatment for men with Chronic Prostatitis/ Chronic Pelvic Pain Syndrome.
Soft tissue mobilisation, myofascial release and manipulation are also beneficial if the physiotherapist has undergone adequate and specialised training[5].
Urinary Incontinence[edit | edit source]
Sexual dysfunction is highly related to urinary dysfunction in men and women. Treatment techniques include voiding rehabilitation and bladder retraining - active pelvic floor muscle contractions to inhibit bladder contraction. This will prevent the detrusor urinae muscle contraction[9].
Other Treatment Techniques[edit | edit source]
If increased tone or spasms have been identified as the underlying problem after assessment the following techniques are indicated for the treatment;
- Myofascial release (for specialised pelvic floor therapists)
- Self-release education (for specialised pelvic floor therapists)
- Trigger Point therapy
- Global Therapeutic Massage
Education regarding behavioural changes includes; diet and weight management[8].
Cue's For Pelvic Floor Retraining[edit | edit source]
- 'Stop the flow'
- 'Shorten the penis'
- 'Lift the pelvic floor or scrotum'
- 'Prevent passing gas'
- 'Tighten around the anus'[8]
Conclusion[edit | edit source]
Emphasis on pelvic floor rehabilitation is often associated with women, however, pelvic floor dysfunction is also common among men. Literature and studies indicate that pelvic floor rehabilitation and physiotherapy management can be effective in treating many conditions such as; erectile dysfunction, ejaculatory dysfunction, Chronic Prostatitis/ Chronic Pelvic Pain Syndrome and urinary incontinence.
References[edit | edit source]
- ↑ deGROAT WC, BOOTH AM. Physiology of male sexual function. Annals of internal medicine. 1980 Feb 1;92(2_Part_2):329-31.
- ↑ Rosen RC. Prevalence and risk factors of sexual dysfunction in men and women. Current psychiatry reports. 2000 Jun 1;2(3):189-95.
- ↑ Hatzimouratidis K, Hatzichristou D. Sexual dysfunctions: classifications and definitions. The journal of sexual medicine. 2007 Jan 1;4(1):241-50.
- ↑ Hatzimouratidis K, Amar E, Eardley I, Giuliano F, Hatzichristou D, Montorsi F, Vardi Y, Wespes E. Guidelines on male sexual dysfunction: erectile dysfunction and premature ejaculation. European urology. 2010 May 1;57(5):804-14.
- ↑ 5.0 5.1 5.2 5.3 5.4 5.5 5.6 5.7 5.8 5.9 Cohen D, Gonzalez J, Goldstein I. The role of pelvic floor muscles in male sexual dysfunction and pelvic pain. Sexual medicine reviews. 2016 Jan 1;4(1):53-62.
- ↑ McCabe MP, Sharlip ID, Lewis R, Atalla E, Balon R, Fisher AD, Laumann E, Lee SW, Segraves RT. Risk factors for sexual dysfunction among women and men: a consensus statement from the Fourth International Consultation on Sexual Medicine 2015. The journal of sexual medicine. 2016 Feb 1;13(2):153-67.
- ↑ Barbaro K, Midgley J. Priapism, a symptom of claudication of the cauda equina in spinal stenosis. Musculoskeletal Science and Practice. 2021 Apr 1;52:102337.
- ↑ 8.0 8.1 8.2 Hodges, Milios, Jones, Greene, Nwankwo. Focused symposium: MEN´S HEALTH: A GLOBAL PROBLEM AND NEW FRONTIER FOR PHYSIOTHERAPY. 2017, July 4.
- ↑ 9.0 9.1 9.2 9.3 9.4 Rosenbaum TY. REVIEWS: Pelvic floor involvement in male and female sexual dysfunction and the role of pelvic floor rehabilitation in treatment: a literature review. The journal of sexual medicine. 2007 Jan 1;4(1):4-13.
- ↑ Michelle Kenway. How to Kegel for Men - Professional Guide to Effective Kegel Strength Exercises. Available from: https://www.youtube.com/watch?v=dSqK4_3YSMI [last accessed 3/18/2020]