Persistent Genital Arousal Disorder (PGAD): Difference between revisions
No edit summary |
No edit summary |
||
| Line 1: | Line 1: | ||
<div class="editorbox"> '''Original Editor '''- [[User:User Name|User Name]] <br> | <div class="editorbox"> '''Original Editor '''- [[User:User Name|User Name]] <br> | ||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}}</div> | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}}</div> | ||
== Introduction == | == Introduction == | ||
| Line 16: | Line 15: | ||
</ref>. | </ref>. | ||
'''Nervous system factors,''' nerve roots compression at the level of cauda equina (roots of genetalia) this compression may be because of tarlov cysts that cause cauda equina syndrome. In a study on an online support group for patients with with PGAD(18) their MRI was collected, (12/18) there was Tarlov cysts<ref>Komisaruk BR, Lee HJ. Prevalence of sacral spinal (Tarlov) cysts in persistent genital arousal disorder. The Journal of Sexual Medicine. 2012 Aug;9(8):2047-56.</ref>. Compression of dorsal nerve of clitoris is another possible factor for PGAD<ref>Klifto KM, Dellon AL. Persistent genital arousal disorder: review of pertinent peripheral nerves. Sexual Medicine Reviews. 2020 Apr 1;8(2):265-73. | '''Nervous system factors,''' nerve roots compression at the level of [[Cauda Equina Syndrome|cauda equina]] (roots of genetalia) this compression may be because of tarlov cysts that cause [[Cauda Equina Syndrome|cauda equina syndrome]]. In a study on an online support group for patients with with PGAD(18) their [[MRI Scans|MRI]] was collected, (12/18) there was Tarlov cysts<ref>Komisaruk BR, Lee HJ. Prevalence of sacral spinal (Tarlov) cysts in persistent genital arousal disorder. The Journal of Sexual Medicine. 2012 Aug;9(8):2047-56.</ref>. Compression of dorsal nerve of [[Female Genital Tract|clitoris]] is another possible factor for PGAD<ref>Klifto KM, Dellon AL. Persistent genital arousal disorder: review of pertinent peripheral nerves. Sexual Medicine Reviews. 2020 Apr 1;8(2):265-73. | ||
BibTeXEndNoteRefManRefWorks</ref>. | BibTeXEndNoteRefManRefWorks</ref>. | ||
'''Psychosocial factors,''' assessment of psychological factors of patient sis important for diagnoses of PGAD<ref>· Aswath M, Pandit LV, Kashyap K, Ramnath R. [https://www.ncbi.nlm.nih.gov/ Persistent genital arousal disorder. Indian journal of psychological medicine]. 2016 Jul;38(4):341-3. </ref>, may be it is not the main factor but it may play a role in the development or maintenance of symptoms<ref name=":4" />, history with sexual abuse is another possible cause. | '''[[Psychological approaches to pain management|Psychosocial]] factors,''' assessment of psychological factors of patient sis important for diagnoses of PGAD<ref>· Aswath M, Pandit LV, Kashyap K, Ramnath R. [https://www.ncbi.nlm.nih.gov/ Persistent genital arousal disorder. Indian journal of psychological medicine]. 2016 Jul;38(4):341-3. </ref>, may be it is not the main factor but it may play a role in the development or maintenance of symptoms<ref name=":4" />, history with sexual abuse is another possible cause. | ||
Other factors | '''Other factors;''' childbirth, falling, vehicle accidents, or [[Sacroiliac Joint Syndrome|sacroiliac joint dysfunction]]. In 2022, Zhang reported a case with PGAD symptoms after many visits to neurosurgeons, neurologists, gynecologists, psychologists there was no symptoms reliefe and with physical exam there was SIJ dysfunction and here symptoms was releases after physical therapy sessions to restore joint alignment<ref>Zhang Y, Su L, Ge H, Wang Q. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9537246/ Persistent genital arousal disorder/genito-pelvic dysesthesia caused by sacroiliac joint dysfunction]. Sexual Medicine. 2022 Oct 1;10(5):100544.</ref>. | ||
== Clinical Presentation == | == Clinical Presentation == | ||
* Uncontrollable genital arousal dos not affected by orgasm or masturbation. | * Uncontrollable [[Female Sexual Health|genital arousal]] dos not affected by [[Female Sexual Health|orgasm]] or masturbation. | ||
* | * Symptoms may persist for hours or days in absence of sexual desire or objective stimulus. | ||
* Pain or discomfort in the genetalia | * Pain or discomfort in the genetalia | ||
* Tingling around clitoris. | * Tingling around clitoris. | ||
| Line 36: | Line 35: | ||
== Diagnostic Procedures == | == Diagnostic Procedures == | ||
Pelvic MRI in cases with suspected pudendal nerve entrapment. | Pelvic [[MRI Scans|MRI]] in cases with suspected pudendal nerve entrapment. | ||
Lumbosacral MRI for exclusion of cauda equina syndrome<ref>Oaklander AL, Sharma S, Kessler K, Price BH. Persistent genital arousal disorder: a special sense neuropathy. Pain Reports. 2020 Jan;5(1).</ref>. | [[Lumbosacral Discogenic Pain Syndrome|Lumbosacral]] MRI for exclusion of cauda equina syndrome<ref>Oaklander AL, Sharma S, Kessler K, Price BH. Persistent genital arousal disorder: a special sense neuropathy. Pain Reports. 2020 Jan;5(1).</ref>. | ||
== Management / Interventions == | == Management / Interventions == | ||
There is a guidelines for PGAD/ GD and all we have depend on case studies, the intervention for PGAD treatment need collaboration of multidisciplinary team | There is a guidelines for PGAD/ GD and all we have depend on case studies, the intervention for PGAD treatment need collaboration of multidisciplinary team for diagnosis and treatment<ref>Martín-Vivar M, Villena-Moya A, Mestre-Bach G, Hurtado-Murillo F, Chiclana-Actis C. Treatments for Persistent Genital Arousal Disorder in Women: A Scoping Review. The Journal of Sexual Medicine. 2022 Jun;19(6):961-74.</ref>. | ||
=== Pharmacological intervention === | === Pharmacological intervention === | ||
[[File:Pill Organizer With Vitamins And Medicines.jpeg|thumb|200x200px]] | |||
There was an improvement in PGAD symptoms with the intervention of antidepressant and anticonvulsant<ref name=":0" /> and there was a successful treatment for female patient with leuprolide<ref>Deka K, Dua N, Kakoty M, Ahmed R. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4623662/ Persistent genital arousal disorder: Successful treatment with leuprolide (antiandrogen).] Indian journal of psychiatry. 2015 Jul 1;57(3):326-8.</ref> that were case studies. | There was an improvement in PGAD symptoms with the intervention of antidepressant and anticonvulsant<ref name=":0" /> and there was a successful treatment for female patient with leuprolide<ref>Deka K, Dua N, Kakoty M, Ahmed R. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4623662/ Persistent genital arousal disorder: Successful treatment with leuprolide (antiandrogen).] Indian journal of psychiatry. 2015 Jul 1;57(3):326-8.</ref> that were case studies. | ||
| Line 51: | Line 51: | ||
=== Physical Therapy === | === Physical Therapy === | ||
* Relaxation exercise and diaphragmatic breathing help to relax pelvic floor muscles<ref name=":1">Jackowich RA, Mooney KM, Hecht E, Pukall CF. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7834936/ Online Pelvic Floor Group Education Program for Women With Persistent Genital Arousal Disorder/Genito-Pelvic Dysesthesia]: Descriptive Feasibility Study. JMIR Formative Research. 2021 Jan 11;5(1):e22450.</ref>, manual therapy and soft tissue mobilization<ref name=":2" />. | * Relaxation exercise and [[Diaphragmatic Breathing Exercises|diaphragmatic breathing]] help to relax [[Pelvic Floor|pelvic floor muscles]]<ref name=":1">Jackowich RA, Mooney KM, Hecht E, Pukall CF. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7834936/ Online Pelvic Floor Group Education Program for Women With Persistent Genital Arousal Disorder/Genito-Pelvic Dysesthesia]: Descriptive Feasibility Study. JMIR Formative Research. 2021 Jan 11;5(1):e22450.</ref>, manual therapy and soft tissue mobilization<ref name=":2" />. | ||
* Electrotherapy for pain management ([[Transcutaneous Electrical Nerve Stimulation for Dementia|TENS]], nerve neuromodulation) | * Electrotherapy for pain management ([[Transcutaneous Electrical Nerve Stimulation for Dementia|TENS]], nerve neuromodulation) | ||
* Advice for life style modification, | * Advice for life style modification, to participate on general body conditioning exercise program, [[Yoga and mindfulness for pelvic health|yoga]], advices for bowel and bladder habits, and stress management<ref name=":1" />. | ||
[[File:Yoga Music Festival.jpg|thumb]] | |||
A case report study in 2010 demonstrated a 27 years old female 27 weeks pregnancy, presented with PGAD symptoms she was evaluated and assessed to identify the underling cause, during pelvic floor physical therapy examination there was multiple trigger points in [[Obturator Internus|obtrurator internus]] and hypertonicity of pelvic floor muscles. The patient undregone for [[Obturator Internus|obtrurator internus]] soft tissue mobilization for about 15 minute, there was completely relieve in symptoms 14 weeks later to this session<ref name=":2">Rosenbaum TY. Physical therapy treatment of persistent genital arousal disorder during pregnancy: A case report. The Journal of Sexual Medicine. 2010 Mar 1;7(3):1306-10.</ref>. | A case report study in 2010 demonstrated a 27 years old female 27 weeks pregnancy, presented with PGAD symptoms she was evaluated and assessed to identify the underling cause, during pelvic floor physical therapy examination there was multiple trigger points in [[Obturator Internus|obtrurator internus]] and hypertonicity of pelvic floor muscles. The patient undregone for [[Obturator Internus|obtrurator internus]] soft tissue mobilization for about 15 minute, there was completely relieve in symptoms 14 weeks later to this session<ref name=":2">Rosenbaum TY. Physical therapy treatment of persistent genital arousal disorder during pregnancy: A case report. The Journal of Sexual Medicine. 2010 Mar 1;7(3):1306-10.</ref>. | ||
| Line 60: | Line 60: | ||
'''[https://www.choosingtherapy.com/hypersexuality/ Hypersexuality],''' unlike PGAD it is associated with a desire to have sex and was defined as the desire and urge to engage in sexual activity. | '''[https://www.choosingtherapy.com/hypersexuality/ Hypersexuality],''' unlike PGAD it is associated with a desire to have sex and was defined as the desire and urge to engage in sexual activity. | ||
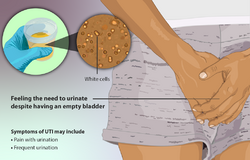
[[File:Urinary Tract Infection (UTI).png|thumb|250x250px|UTI]] | |||
[[Urinary Tract Infection|Urinary tract infection]] if there was symptoms like burning and itching. | [[Urinary Tract Infection|Urinary tract infection]] if there was symptoms like burning and itching. | ||
| Line 66: | Line 66: | ||
[[Male Sexual Dysfunction|Penoscrotodynia]]<ref name=":3" />, related to men and is similar to vulvodynia in women, is a skin burning sensation at genital area. | [[Male Sexual Dysfunction|Penoscrotodynia]]<ref name=":3" />, related to men and is similar to vulvodynia in women, is a skin burning sensation at genital area. | ||
== References == | == References == | ||
Revision as of 00:06, 30 March 2023
Introduction[edit | edit source]
Persistent genital arousal disorder (PGAD), restless genital syndrome (ReGS), or genitopelvic dysesthesia (GD) a rare disorder defined as persistatant, unpleasant , distressing sensation of unwanted, uncontrollable genital arousal, happens in the absence of any arousal or sexual stimulus, dose not resolve by orgasm or masturbation, may last for hours or days, and usually has a negative impact on individual's life. Symptoms may be triggered by sexual cues, non-sexual cues, or it may be idiopathic. Persistent genital arousal disorder (PGAD) was described for the first time in 2001 by Sandra Leiblum and Sharon Nathan[1]. It is relating mainly to women but it was presented in men also[2].
Mechanism of Injury / Pathological Process[edit | edit source]
As it was described for first time 20 years ago and it difficult to know its prevalence there is limited studies about PGAD that are individual case studies till now there is not RCT or SR studies about PGAD how to diagnose, assess, or treat.
There are different hypotheses for causes of PGAD that may be multifacorial; vascular factors, central and peripheral nervous system factors, pharmacological factors, psychosocial factors, dietary, or even idiopathetic factors.
Pharmacological factors, it was reported in a few case report studies that drugs that contain serotonergic such as antidepressant medication (SSRIs /SNRIs) may induce or worsen PGAD symptoms [3]even at initiation or withdrawal of drug, however, there were cases in which there was a fundamental improvement of PGAD symptoms anticonvulsant or SNRI[4].
Nervous system factors, nerve roots compression at the level of cauda equina (roots of genetalia) this compression may be because of tarlov cysts that cause cauda equina syndrome. In a study on an online support group for patients with with PGAD(18) their MRI was collected, (12/18) there was Tarlov cysts[5]. Compression of dorsal nerve of clitoris is another possible factor for PGAD[6].
Psychosocial factors, assessment of psychological factors of patient sis important for diagnoses of PGAD[7], may be it is not the main factor but it may play a role in the development or maintenance of symptoms[1], history with sexual abuse is another possible cause.
Other factors; childbirth, falling, vehicle accidents, or sacroiliac joint dysfunction. In 2022, Zhang reported a case with PGAD symptoms after many visits to neurosurgeons, neurologists, gynecologists, psychologists there was no symptoms reliefe and with physical exam there was SIJ dysfunction and here symptoms was releases after physical therapy sessions to restore joint alignment[8].
Clinical Presentation[edit | edit source]
- Uncontrollable genital arousal dos not affected by orgasm or masturbation.
- Symptoms may persist for hours or days in absence of sexual desire or objective stimulus.
- Pain or discomfort in the genetalia
- Tingling around clitoris.
- Genital engorgement.
- Lubrication or discharges
- Throbbing response[9].
Diagnostic Procedures[edit | edit source]
Pelvic MRI in cases with suspected pudendal nerve entrapment.
Lumbosacral MRI for exclusion of cauda equina syndrome[10].
Management / Interventions[edit | edit source]
There is a guidelines for PGAD/ GD and all we have depend on case studies, the intervention for PGAD treatment need collaboration of multidisciplinary team for diagnosis and treatment[11].
Pharmacological intervention[edit | edit source]
There was an improvement in PGAD symptoms with the intervention of antidepressant and anticonvulsant[4] and there was a successful treatment for female patient with leuprolide[12] that were case studies.
Neurolysis of dorsal nerve to clitoris[edit | edit source]
In cases with nerve compression there was complete relief of symptoms after surgery an bilateral neurolysis had better outcomes than unilateral. The dorsal nerve to clitoris is compressed mainly at the exit of the canal of Alcock and the site of compression can be detected during physical examination it will be tender and painful with palpation[13].
Physical Therapy[edit | edit source]
- Relaxation exercise and diaphragmatic breathing help to relax pelvic floor muscles[14], manual therapy and soft tissue mobilization[15].
- Electrotherapy for pain management (TENS, nerve neuromodulation)
- Advice for life style modification, to participate on general body conditioning exercise program, yoga, advices for bowel and bladder habits, and stress management[14].
A case report study in 2010 demonstrated a 27 years old female 27 weeks pregnancy, presented with PGAD symptoms she was evaluated and assessed to identify the underling cause, during pelvic floor physical therapy examination there was multiple trigger points in obtrurator internus and hypertonicity of pelvic floor muscles. The patient undregone for obtrurator internus soft tissue mobilization for about 15 minute, there was completely relieve in symptoms 14 weeks later to this session[15].
Differential Diagnosis[edit | edit source]
Hypersexuality, unlike PGAD it is associated with a desire to have sex and was defined as the desire and urge to engage in sexual activity.
Urinary tract infection if there was symptoms like burning and itching.
Vulvodynia[16], persistent vulvar pain that is usually unexplained and may be caused by irritation to peripheral nerves around the vulva.
Penoscrotodynia[16], related to men and is similar to vulvodynia in women, is a skin burning sensation at genital area.
References[edit | edit source]
- ↑ 1.0 1.1 Jackowich RA, Pukall CF. Persistent genital arousal disorder: a biopsychosocial framework. Current Sexual Health Reports. 2020 Sep;12:127-35.
- ↑ Stevenson BJ, Köhler TS. First reported case of isolated persistent genital arousal disorder in a male. Case Reports in Urology. 2015 Feb 12;2015.
- ↑ Leiblum SR, Goldmeier D. Persistent genital arousal disorder in women: case reports of association with anti-depressant usage and withdrawal. Journal of Sex & Marital Therapy. 2008 Feb 21;34(2):150-9.
- ↑ 4.0 4.1 Kruger TH, Schippert C, Meyer B. The pharmacotherapy of persistent genital arousal disorder. Current Sexual Health Reports. 2020 Mar;12:34-9.
- ↑ Komisaruk BR, Lee HJ. Prevalence of sacral spinal (Tarlov) cysts in persistent genital arousal disorder. The Journal of Sexual Medicine. 2012 Aug;9(8):2047-56.
- ↑ Klifto KM, Dellon AL. Persistent genital arousal disorder: review of pertinent peripheral nerves. Sexual Medicine Reviews. 2020 Apr 1;8(2):265-73. BibTeXEndNoteRefManRefWorks
- ↑ · Aswath M, Pandit LV, Kashyap K, Ramnath R. Persistent genital arousal disorder. Indian journal of psychological medicine. 2016 Jul;38(4):341-3.
- ↑ Zhang Y, Su L, Ge H, Wang Q. Persistent genital arousal disorder/genito-pelvic dysesthesia caused by sacroiliac joint dysfunction. Sexual Medicine. 2022 Oct 1;10(5):100544.
- ↑ Deka K, Dua N, Kakoty M, Ahmed R. Persistent genital arousal disorder: Successful treatment with leuprolide (antiandrogen). Indian journal of psychiatry. 2015 Jul 1;57(3):326-8.
- ↑ Oaklander AL, Sharma S, Kessler K, Price BH. Persistent genital arousal disorder: a special sense neuropathy. Pain Reports. 2020 Jan;5(1).
- ↑ Martín-Vivar M, Villena-Moya A, Mestre-Bach G, Hurtado-Murillo F, Chiclana-Actis C. Treatments for Persistent Genital Arousal Disorder in Women: A Scoping Review. The Journal of Sexual Medicine. 2022 Jun;19(6):961-74.
- ↑ Deka K, Dua N, Kakoty M, Ahmed R. Persistent genital arousal disorder: Successful treatment with leuprolide (antiandrogen). Indian journal of psychiatry. 2015 Jul 1;57(3):326-8.
- ↑ Klifto K, Dellon AL. Persistent genital arousal disorder: Treatment by neurolysis of dorsal branch of pudendal nerve. Microsurgery. 2020 Feb;40(2):160-6.
- ↑ 14.0 14.1 Jackowich RA, Mooney KM, Hecht E, Pukall CF. Online Pelvic Floor Group Education Program for Women With Persistent Genital Arousal Disorder/Genito-Pelvic Dysesthesia: Descriptive Feasibility Study. JMIR Formative Research. 2021 Jan 11;5(1):e22450.
- ↑ 15.0 15.1 Rosenbaum TY. Physical therapy treatment of persistent genital arousal disorder during pregnancy: A case report. The Journal of Sexual Medicine. 2010 Mar 1;7(3):1306-10.
- ↑ 16.0 16.1 Markos AR, Dinsmore W. Persistent genital arousal and restless genitalia: sexual dysfunction or subtype of vulvodynia?. International Journal of STD & Aids. 2013 Nov;24(11):852-8.