Non Pharmacological Interventions: Difference between revisions
No edit summary |
No edit summary |
||
| (10 intermediate revisions by 2 users not shown) | |||
| Line 1: | Line 1: | ||
= | <div class="editorbox"> '''Original Editor '''- [[User:Debbie Kenny |Debbie Kenny ]] '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}}</div> | ||
== Non-Pharmacological Approaches == | |||
[[File:Brainfood Pyramid.png|thumb|Brainfood pyramid]] | |||
Non-pharmacological interventions (NPI) are any non-chemical intervention (theoretically supported) performed on and benefitting the patient. | |||
* NPI have been employed as medical interventions (predating modern pharmacology), and are intended to improve quality of life, slow down deterioration or relieve pain. NPI also reduce health costs reduced and have minimal environmental impact.. | |||
* Following a healthy lifestyle is possibly the best NPI, contributing to improved health and quality of life.<ref name=":37">Herguedas AJ. [https://www.intechopen.com/chapters/73680 Non-Pharmacological Interventions in Preventive, Rehabilitative and Restorative Medicine.] InAlternative Medicine-Update 2020 Dec 21. IntechOpen. Available:https://www.intechopen.com/chapters/73680 (accessed 30.12.2022)</ref> See [[Lifestyle Medicine for Health and Disease Management]] | |||
== | == Physiotherapy: A Non-Pharmacological Intervention == | ||
A wide range of NPI modalities are used by physiotherapists, including manual therapies, electrophysical agents, thermotherapy, hydrotherapy, therapeutic exercise, meditation, and acupuncture. The physiotherapists' goal is to reduce pain and restore (or maintain) optimal physical functioning via these NPI. Take a look at some of the NPI's used: | |||
== '''Patient education''' == | |||
[[File:Doctor patient.png|thumb|386x386px|Patient Education]] | |||
The importance of increasing a patient’s understanding of their condition and treatment plan is not only of benefit for improving a patient’s adherence to treatment, but can also improve health outcomes <ref>Adams R. Improving health outcomes with better patient understanding and education. Risk Management and Healthcare Policy 2010;3:61-72</ref>. Self-management of chronic conditions as well as preventative health intents rely heavily on provision of contemporary information and communication practice <ref name=":0">Wagner E.H, Austin B.T, Davis C, Hindmarsh M, Schaefer J, Bonomi A. Improving chronic illness care: translating evidence into action. Health Affairs 2001;20:64-78.</ref>. Primary focus for long term conditions commonly involves promotion of informed lifestyle choices, risk-factor modification, and active patient self-management <ref name=":0" />. Education can be provided through a variety of health care professionals, preferably done by providers who have undertaken adequate training for education, and patient communication. Recognized physiotherapy programmes typically include a component of patient education within their training. <ref>Forbes R, Mandrusiak A, Smith M, Russel T. Training physiotherapy students to educate patients: A randomized controlled trial. Patient Education and Counselling 2018;101:295-303.</ref>. See also [[Patient Education in Pain Management]] [[Patient Education for Parkinson's Drugs]] | |||
== Physical Activity == | == '''Physical Activity''' == | ||
Physical activity prescription (a NPI) is an under-utilised tool for improving community health. In the right dose, physical activity can help to prevent, treat, and manage a range of chronic health conditions that increasingly impact the quality of life and physical function of individuals on a global scale.<ref>World Health Organization. [https://www.who.int/publications/i/item/9789241563871 Global health risks: mortality and burden of disease attributable to selected major risks]. Geneva: World Health Organization Press, 2009 Available:https://www.who.int/publications/i/item/9789241563871 (accessed 30.12.2022)</ref> | Physical activity prescription (a NPI) is an under-utilised tool for improving community health. In the right dose, physical activity can help to prevent, treat, and manage a range of chronic health conditions that increasingly impact the quality of life and physical function of individuals on a global scale.<ref>World Health Organization. [https://www.who.int/publications/i/item/9789241563871 Global health risks: mortality and burden of disease attributable to selected major risks]. Geneva: World Health Organization Press, 2009 Available:https://www.who.int/publications/i/item/9789241563871 (accessed 30.12.2022)</ref> | ||
[[File:Health-benefits-of-physical-activity.png|center|frameless|570x570px]] | |||
== | == '''Electrotherapy modalities''' == | ||
*[[Current Concepts in Electrotherapy|E]][[Electrophysical|lectrophysical agents]] is a term describing electrical devices applied by trained professionals to an injury site in effort to enhance, expedite, or improve the treatment plan and recovery process. There are a wide range of electrotherapy modalities used in physical therapy. Conventionally, they are used for pain management, reducing swelling, increasing local blood flow, and breaking down scar tissue and can be applied across various stages of injury recovery <ref name=":5">Watson T. ''Electrotherapy: Modalities''. 2018 [online][viewed 12/04/2018]. Available from: <nowiki>http://www.electrotherapy.org/modalities</nowiki></ref>. | |||
* Common electrotherapy modalities used in pain management include [[Transcutaneous Electrical Nerve Stimulation (TENS)|transcutaneous electrical nerve stimulation (]]TENS), [[Interferential Therapy|interferential current]] (IFC), [[Ultrasound therapy|ultrasound]], and laser therapy. | |||
* [[Current Concepts in Electrotherapy| | |||
* Common electrotherapy modalities used in pain management include [[Transcutaneous Electrical Nerve Stimulation (TENS)|transcutaneous electrical nerve stimulation (]]TENS), [[Interferential Therapy|interferential current]] (IFC), [[Ultrasound therapy|ultrasound]], and laser therapy | |||
== Thermotherapy == | |||
[[Thermotherapy]], involves use of heat or cold | [[Thermotherapy]], involves use of heat or cold | ||
| Line 39: | Line 33: | ||
=== Manual Therapy === | === Manual Therapy === | ||
Manual therapy | Manual therapy has a long history within the profession of physical therapy. There are a wide variety of techniques that can be grouped into four major categories: manipulation, mobilization, static stretching, and muscle energy techniques <ref name=":16">Clar C, Trertsvadze A, Court R, Hundt G.L, Clarke A, Sutcliffe P. Clinical effectiveness of manual therapy for the management of musculoskeletal and non-musculoskeletal conditions: systematic review and update of UK evidence report. Chiropractic & Manual Therapies 2014;22:12.</ref>. Contemporary research reveals intricate neurophysiologic mechanisms are also at play and the beneficial psychological effects of providing hands-on examination and intervention have been substantiated.<ref>Huijbregts PA. [https://www.sciencedirect.com/topics/medicine-and-dentistry/manual-therapy Manual therapy]. InPain Procedures in Clinical Practice 2011 Jan 1 (pp. 573-596). Hanley & Belfus. Available from: https://www.sciencedirect.com/topics/medicine-and-dentistry/manual-therapy (last accessed 30.12.2022)</ref> | ||
=== Therapeutic exercise === | === Therapeutic exercise === | ||
Therapeutic exercise techniques include passive movements, active assisted movements, active movements, resisted movements and assisted resisted movements with aims to correct impairment, improve musculoskeletal function or maintain well-being <ref name=":18">Lieberman J.A, Bockenek W.L. ''Physical Medicine and Rehabilitation: Therapeutic Exercise''. 2016. [online] [viewed 15/04/2018]. Available from: <nowiki>https://emedicine.medscape.com/article/324583-overview#showall</nowiki></ref>. | [[Therapeutic Exercise|Therapeutic exercise]] techniques include passive movements, active assisted movements, active movements, resisted movements and assisted resisted movements with aims to correct impairment, improve musculoskeletal function or maintain well-being <ref name=":18">Lieberman J.A, Bockenek W.L. ''Physical Medicine and Rehabilitation: Therapeutic Exercise''. 2016. [online] [viewed 15/04/2018]. Available from: <nowiki>https://emedicine.medscape.com/article/324583-overview#showall</nowiki></ref>. | ||
See also [[Exercise and Activity in Pain Management]] | See also [[Exercise and Activity in Pain Management]] | ||
== Meditation == | |||
[[Meditation]] | |||
* Benefits include: Removes the accumulated stress and help increase the positive energy; decreases anxiety, depression, and pain (both physical and psychological); increases regional cerebral blood flow in the frontal and anterior cingulate region of the brain; decreases sympathetic overstimulation reduces cholesterol and risk of heart disease and helps in reducing smoking; has been shown to be beneficial in epilepsy, premenstrual symptoms, menopausal symptoms, autoimmune illness, and emotional disturbance in neoplastic disease; improves telomerase activity in the body which slows down the aging process and related diseases.<ref>Sharma H. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4895748/ Meditation: Process and effects.] Ayu. 2015 Jul;36(3):233. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4895748/ (accessed 30.12.2022)</ref> | |||
== | == Mindfulness == | ||
* Mindfulness is a [[Stress and Health|stress]]-reducing strategy where an individual develops an awareness that arises through paying attention, on purpose, in the present moment, non-judgmentally and accepting them as they are. | |||
* [[Mindfulness Meditation in Chronic Pain Management]] | |||
== Virtual Reality == | |||
During physical therapy, virtual reality (VR) can shorten recovery times by e.g. | |||
* Making it easier for patients with pain to do their exercises. VR changes the focus from pain to an absorbing alternative reality that entrances, motivates and encourages them to complete perform the task. | |||
* Helping patients who are recovering from a stroke to be able to practice specific movements without the risk of further injuring themselves by a fall. This boosts confidence when it they are then ready to move in real-life setting.<ref>News Medical Applications of Virtual Reality in Medicine Available:https://www.news-medical.net/health/Applications-of-Virtual-Reality-in-Medicine.aspx (accessed 30.12.2022)</ref> | |||
Findings from a scoping review<ref>Asadzadeh A, Samad-Soltani T, Salahzadeh Z, Rezaei-Hachesu P. [https://www.sciencedirect.com/science/article/pii/S2352914821000526 Effectiveness of virtual reality-based exercise therapy in rehabilitation: A scoping review. Informatics in Medicine] Unlocked. 2021 Jan 1;24:100562.</ref> suggests virtual reality intervention is beneficial for exercise therapy and it can be used for various rehabilitation purposes, such as pain management, improving functional ability, increasing range of motion, promoting muscular strength, increasing motivation, and enhancing quality of life. Many studies state to have use Nintendo Wii for developing VR systems in exercise therapy; more research is needed to confirm and improve the effectiveness of the treatments. | |||
See the below examples of how VR can be used as a NPI | |||
* | * [[Virtual Reality and Parkinson's]], | ||
* [[ | * [[Virtual Reality Treatment for Multiple Sclerosis]], | ||
* [[Virtual Reality for Individuals Affected by Stroke]], | |||
* [[Virtual Reality As a Memory Aid in Cognitive Impaired Older adults]]. | |||
== Other NPIs == | == Other NPIs == | ||
* [[Alternative Therapies for Pain Conditions]] | * [[Alternative Therapies for Pain Conditions]] | ||
* [[Yoga]] | * [[Yoga]] | ||
* [[Cognitive Behavioural Therapy]] | * [[Cognitive Behavioural Therapy]] | ||
| Line 69: | Line 72: | ||
* [[Acupuncture]] | * [[Acupuncture]] | ||
* [[Massage|Massage Therapy]] | * [[Massage|Massage Therapy]] | ||
== References == | |||
<references /> | |||
[[Category:Interventions]] | |||
Latest revision as of 11:12, 31 December 2022
Non-Pharmacological Approaches[edit | edit source]
Non-pharmacological interventions (NPI) are any non-chemical intervention (theoretically supported) performed on and benefitting the patient.
- NPI have been employed as medical interventions (predating modern pharmacology), and are intended to improve quality of life, slow down deterioration or relieve pain. NPI also reduce health costs reduced and have minimal environmental impact..
- Following a healthy lifestyle is possibly the best NPI, contributing to improved health and quality of life.[1] See Lifestyle Medicine for Health and Disease Management
Physiotherapy: A Non-Pharmacological Intervention[edit | edit source]
A wide range of NPI modalities are used by physiotherapists, including manual therapies, electrophysical agents, thermotherapy, hydrotherapy, therapeutic exercise, meditation, and acupuncture. The physiotherapists' goal is to reduce pain and restore (or maintain) optimal physical functioning via these NPI. Take a look at some of the NPI's used:
Patient education[edit | edit source]
The importance of increasing a patient’s understanding of their condition and treatment plan is not only of benefit for improving a patient’s adherence to treatment, but can also improve health outcomes [2]. Self-management of chronic conditions as well as preventative health intents rely heavily on provision of contemporary information and communication practice [3]. Primary focus for long term conditions commonly involves promotion of informed lifestyle choices, risk-factor modification, and active patient self-management [3]. Education can be provided through a variety of health care professionals, preferably done by providers who have undertaken adequate training for education, and patient communication. Recognized physiotherapy programmes typically include a component of patient education within their training. [4]. See also Patient Education in Pain Management Patient Education for Parkinson's Drugs
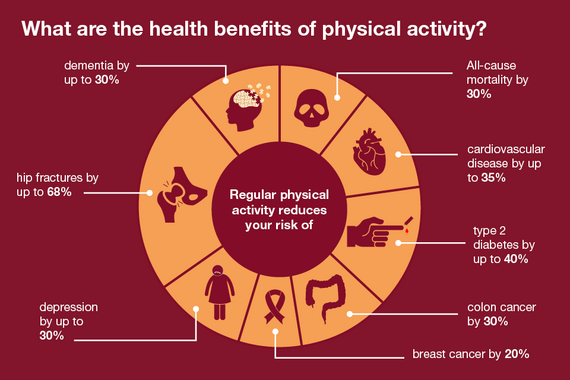
Physical Activity[edit | edit source]
Physical activity prescription (a NPI) is an under-utilised tool for improving community health. In the right dose, physical activity can help to prevent, treat, and manage a range of chronic health conditions that increasingly impact the quality of life and physical function of individuals on a global scale.[5]
Electrotherapy modalities[edit | edit source]
- Electrophysical agents is a term describing electrical devices applied by trained professionals to an injury site in effort to enhance, expedite, or improve the treatment plan and recovery process. There are a wide range of electrotherapy modalities used in physical therapy. Conventionally, they are used for pain management, reducing swelling, increasing local blood flow, and breaking down scar tissue and can be applied across various stages of injury recovery [6].
- Common electrotherapy modalities used in pain management include transcutaneous electrical nerve stimulation (TENS), interferential current (IFC), ultrasound, and laser therapy.
Thermotherapy[edit | edit source]
Thermotherapy, involves use of heat or cold
- Heat can give relief in subacute and chronic inflammatory and traumatic disorders, Heat increases blood flow, helping reduce inflammation, oedema and exudates from connective tissue injuries.
- Cold helps relieve muscle spasms, myofascial or traumatic pain and acute inflammation.
Thermal modalities can also be used as adjuncts to exercise therapy and/or electrophysical modalities, for a variety of therapeutic purposes [7].
Manual Therapy[edit | edit source]
Manual therapy has a long history within the profession of physical therapy. There are a wide variety of techniques that can be grouped into four major categories: manipulation, mobilization, static stretching, and muscle energy techniques [8]. Contemporary research reveals intricate neurophysiologic mechanisms are also at play and the beneficial psychological effects of providing hands-on examination and intervention have been substantiated.[9]
Therapeutic exercise[edit | edit source]
Therapeutic exercise techniques include passive movements, active assisted movements, active movements, resisted movements and assisted resisted movements with aims to correct impairment, improve musculoskeletal function or maintain well-being [10].
See also Exercise and Activity in Pain Management
Meditation[edit | edit source]
- Benefits include: Removes the accumulated stress and help increase the positive energy; decreases anxiety, depression, and pain (both physical and psychological); increases regional cerebral blood flow in the frontal and anterior cingulate region of the brain; decreases sympathetic overstimulation reduces cholesterol and risk of heart disease and helps in reducing smoking; has been shown to be beneficial in epilepsy, premenstrual symptoms, menopausal symptoms, autoimmune illness, and emotional disturbance in neoplastic disease; improves telomerase activity in the body which slows down the aging process and related diseases.[11]
Mindfulness[edit | edit source]
- Mindfulness is a stress-reducing strategy where an individual develops an awareness that arises through paying attention, on purpose, in the present moment, non-judgmentally and accepting them as they are.
- Mindfulness Meditation in Chronic Pain Management
Virtual Reality[edit | edit source]
During physical therapy, virtual reality (VR) can shorten recovery times by e.g.
- Making it easier for patients with pain to do their exercises. VR changes the focus from pain to an absorbing alternative reality that entrances, motivates and encourages them to complete perform the task.
- Helping patients who are recovering from a stroke to be able to practice specific movements without the risk of further injuring themselves by a fall. This boosts confidence when it they are then ready to move in real-life setting.[12]
Findings from a scoping review[13] suggests virtual reality intervention is beneficial for exercise therapy and it can be used for various rehabilitation purposes, such as pain management, improving functional ability, increasing range of motion, promoting muscular strength, increasing motivation, and enhancing quality of life. Many studies state to have use Nintendo Wii for developing VR systems in exercise therapy; more research is needed to confirm and improve the effectiveness of the treatments.
See the below examples of how VR can be used as a NPI
- Virtual Reality and Parkinson's,
- Virtual Reality Treatment for Multiple Sclerosis,
- Virtual Reality for Individuals Affected by Stroke,
- Virtual Reality As a Memory Aid in Cognitive Impaired Older adults.
Other NPIs[edit | edit source]
- Alternative Therapies for Pain Conditions
- Yoga
- Cognitive Behavioural Therapy
- Tai Chi
- Acupuncture
- Massage Therapy
References[edit | edit source]
- ↑ Herguedas AJ. Non-Pharmacological Interventions in Preventive, Rehabilitative and Restorative Medicine. InAlternative Medicine-Update 2020 Dec 21. IntechOpen. Available:https://www.intechopen.com/chapters/73680 (accessed 30.12.2022)
- ↑ Adams R. Improving health outcomes with better patient understanding and education. Risk Management and Healthcare Policy 2010;3:61-72
- ↑ 3.0 3.1 Wagner E.H, Austin B.T, Davis C, Hindmarsh M, Schaefer J, Bonomi A. Improving chronic illness care: translating evidence into action. Health Affairs 2001;20:64-78.
- ↑ Forbes R, Mandrusiak A, Smith M, Russel T. Training physiotherapy students to educate patients: A randomized controlled trial. Patient Education and Counselling 2018;101:295-303.
- ↑ World Health Organization. Global health risks: mortality and burden of disease attributable to selected major risks. Geneva: World Health Organization Press, 2009 Available:https://www.who.int/publications/i/item/9789241563871 (accessed 30.12.2022)
- ↑ Watson T. Electrotherapy: Modalities. 2018 [online][viewed 12/04/2018]. Available from: http://www.electrotherapy.org/modalities
- ↑ Prentice W.E. Therapeutic Modalities in Rehabilitation. 4th ed. New York: McGraw-Hill Medical; 2011.
- ↑ Clar C, Trertsvadze A, Court R, Hundt G.L, Clarke A, Sutcliffe P. Clinical effectiveness of manual therapy for the management of musculoskeletal and non-musculoskeletal conditions: systematic review and update of UK evidence report. Chiropractic & Manual Therapies 2014;22:12.
- ↑ Huijbregts PA. Manual therapy. InPain Procedures in Clinical Practice 2011 Jan 1 (pp. 573-596). Hanley & Belfus. Available from: https://www.sciencedirect.com/topics/medicine-and-dentistry/manual-therapy (last accessed 30.12.2022)
- ↑ Lieberman J.A, Bockenek W.L. Physical Medicine and Rehabilitation: Therapeutic Exercise. 2016. [online] [viewed 15/04/2018]. Available from: https://emedicine.medscape.com/article/324583-overview#showall
- ↑ Sharma H. Meditation: Process and effects. Ayu. 2015 Jul;36(3):233. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4895748/ (accessed 30.12.2022)
- ↑ News Medical Applications of Virtual Reality in Medicine Available:https://www.news-medical.net/health/Applications-of-Virtual-Reality-in-Medicine.aspx (accessed 30.12.2022)
- ↑ Asadzadeh A, Samad-Soltani T, Salahzadeh Z, Rezaei-Hachesu P. Effectiveness of virtual reality-based exercise therapy in rehabilitation: A scoping review. Informatics in Medicine Unlocked. 2021 Jan 1;24:100562.