|
|
| (20 intermediate revisions by 3 users not shown) |
| Line 1: |
Line 1: |
| == Non-Pharmacological Approaches == | | <div class="editorbox"> '''Original Editor '''- [[User:Debbie Kenny |Debbie Kenny ]] '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}}</div> |
| The following is a non-exhaustive list of non-pharmacological options both in and outside the scope of physiotherapy practice. The aim of this resource is to provide physiotherapists and other relevant health professionals with a baseline resource for complementary or alternative treatment options to consider when desiring to remedy clinical scenarios where overprescription is suspected. Clinical professional readers are advised to continually consider relevant and most recent available evidence in relation to their patients’ clinical situation and flagged medication. Additionally, non-prescribing clinical readers are reminded to stay within their scope of practice and always discuss any treatment options preferred as an alternative to drug therapies with the patient’s multidisciplinary team (MDT) or general practitioner (GP). Non-clinical readers are advised to discuss any preferable options with their GP before seeking treatment.
| |
|
| |
|
| == Physiotherapy interventions ==
| |
|
| |
|
| === Patient education === | | == Non-Pharmacological Approaches == |
| The importance of increasing a patient’s understanding of their condition and treatment plan is not only of benefit for improving a patient’s adherence to treatment, but can also improve health outcomes <ref>Adams R. Improving health outcomes with better patient understanding and education. Risk Management and Healthcare Policy 2010;3:61-72</ref>. Self-management of chronic conditions as well as preventative health intents rely heavily on provision of contemporary information and communication practice <ref name=":0">Wagner E.H, Austin B.T, Davis C, Hindmarsh M, Schaefer J, Bonomi A. Improving chronic illness care: translating evidence into action. Health Affairs 2001;20:64-78.</ref>. Primary focus for long term conditions commonly involves promotion of informed lifestyle choices, risk-factor modification, and active patient self-management <ref name=":0" />. Education can be provided through a variety of health care professionals, preferably done by providers who have undertaken adequate training for education, and patient communication. Recognized physiotherapy programmes typically include a component of patient education within their training, however, training interventions for physiotherapy students has shown to improve their self-efficacy and performance in the delivery of patient education <ref>Forbes R, Mandrusiak A, Smith M, Russel T. Training physiotherapy students to educate patients: A randomized controlled trial. Patient Education and Counselling 2018;101:295-303.</ref>. Core competencies for health professional educators according to <ref>Bastable S.B, Gramet P, Jacobs K, Sopczyk D. ''Health Professionals as Educator: Principles of Teaching and Learning.'' Sudbury: Jones and Bartlett Learning; 2012.</ref> include the following:
| | [[File:Brainfood Pyramid.png|thumb|Brainfood pyramid]] |
| | | Non-pharmacological interventions (NPI) are any non-chemical intervention (theoretically supported) performed on and benefitting the patient. |
| · Feature a personal ethic, for social responsibilities and services towards others
| |
| | |
| · Deliver accurate, proficient and evidence based care
| |
| | |
| · Exercise preventative health care
| |
| | |
| · Emphasize relationship-centred care with patients and their families
| |
| | |
| · Consider the multiple determinants of health during provision of care
| |
| | |
| · Remain culturally sensitive and open to diverse society
| |
| | |
| · Utilize technology competently and effectively
| |
| | |
| · Remain current in your field and continue professional development to advance education
| |
| | |
| In the United States, opportunity for health professionals to become certified health educators is provided by the [https://www.nchec.org/ National Commission for Health Education Credentialing]. Information on credentialing can be found below:
| |
| | |
| {{#ev:youtube|emJlL07WRXU}}
| |
| | |
| Evidence for patient education’s effect on health outcomes vary across populations and pathologies, but has shown improvement in many. For patients with inflammatory arthritis, a 2015 systematic literature review investigated patient education delivered through face to face meetings with allied health professionals (including physiotherapists), patient groups, and online support programmes <ref name=":1">Zang H.A, Ndosi M, Adams J, Andersen L, Bode C, Bostrom C, van Eijk-Hustings Y, Gossec L, Korandova J, Mendes G, Niedermann K, Primdahl J, Stoffer M, Voshaar M, van Tubergen A. EULAR recommendations for patient education for people with inflammatory arthritis. Annals of Rheumatic Diseases 2015;74:954-962.</ref>. The best evidence emerging from the review resulted from face to face meetings as an interactive learning process. Beneficial effects were found in terms of adherence to treatment regimens, behavioural change, use of self-management strategies and well-being <ref name=":1" />. In rheumatoid arthritic patients, another systematic review reports patient education is either strongly recommended or recommended as an effective non-pharmacological option by 10 of the 13 selected clinical practice guidelines <ref>Brosseau L, Rahman P, Poitras S, Toupin-April K, Paterson G, Smith C, King J, Casimiro L, De Angelis G, Loew L, Cavallo S, McEwan J. A Systematic Critical Appraisal of Non-Pharmacological Management of Rheumatoid Arthritis with Appraisal of Guidelines for Research and Evaluation II. PLOS ONE 2014;9</ref>. In the amputee population, patient education is recommended as a MDT approach aimed at changing the patient’s lifestyle in regards to physical activity and pain management, as long as it maintains a patient-cantered approach <ref name=":2">Pantera E, Pourtier-Piotte C, Bensoussan L, Coudeyre E. Patient education after amputation: Systematic review and experts’ opinions. Annals of Physical and Rehabilitation Medicine 2014;57:143-158.</ref>. Improvements can be seen in depression, mood, self-management, and functional status, as well as pain and quality of life in certain populations <ref name=":2" />. In palliative care settings, patient education regarding cancer pain management has been systematically reviewed as well <ref name=":3">Bennett M.I, Bagnall A.M, Jose Closs S. How effective are patient-based educational interventions in the management of cancer pain: systematic review and meta-analysis. Pain 2009;143:192-199.</ref>. Authors reported modest but clinically significant reduction in cancer pain after patient-based educational interventions, and although these interventions are underutilized, they are recommended to be routinely used in practice. Additionally, for patients using opioids, an educational session may be more effective than the addition of co-analgesics <ref name=":3" />. Unfortunately, in regards to reducing falls in the elderly, patient knowledge and educational interventions were found to be ineffective <ref name=":4">Rimland J.M, Abraha I, Dell’Aquilla G, Cruz-Jentoft A, Soiza R, Gudmusson A, Petrovic M, O’Mahony D, Todd C, Cherubini A. Effectiveness of Non-Pharmacological Interventions to Prevent Falls in Older People: A Systematic Overview. The SENATOR Project ONTOP Series. PLOS ONE 2016;11. </ref>.
| |
| | |
| === Electrotherapy modalities ===
| |
| Electrotherapy modalities, also referred to as electrophysical agents, are terms to describe electrical devices that are safely applied by trained professionals to an injury site in effort to enhance, expedite, or improve the treatment plan and recovery process. There are a wide range of electrotherapy modalities used in physical therapy. Conventionally, they are used for pain management, reducing swelling, increasing local blood flow, and breaking down scar tissue and can be applied across various stages of injury recovery <ref name=":5">Watson T. ''Electrotherapy: Modalities''. 2018 [online][viewed 12/04/2018]. Available from: <nowiki>http://www.electrotherapy.org/modalities</nowiki></ref>. Common electrotherapy modalities used in pain management include transcutaneous electrical nerve stimulation (TENS), interferential current (IFC), ultrasound, and laser therapy. More information on a wider variety of electrotherapy modalities and their multitude of uses can be found [http://www.electrotherapy.org/modalities here].
| |
| | |
| TENS and IFC are similar modalities as they use electrodes around the desired site to apply electrical impulses in effort to provide symptomatic pain relief through the excitement of local sensory nerves, thereby stimulating the pain gate mechanism and/or opioid system to mask pain symptoms <ref name=":5" />.
| |
| | |
| Evidence for IFC has been published through meta-analysis in knee osteoarthritic patients to reduce pain and likewise decreasing analgesic medication such as paracetamol intake <ref name=":6">Buenavente M.L.D, Gonzalez-Suarez C.B, Lee-Ledesma M.A.B, Liao L.A.S. Evidence on the effectiveness of interferential current therapy in the treatment of knee osteoarthritis: A meta-analysis. OA Arthritis 2014;2:7</ref>. Another meta-analysis for IFC states its potential use in musculoskeletal pain management when used as a supplement to other interventions <ref name=":7">Fuentes J.P, Armijo Olivo S, Magee D.J, Gross D.P. Effectiveness of interferential current therapy in the management of musculoskeletal pain: a systematic review and meta-analysis. Physical Therapy 2010;90:1219-1238.</ref>. The authors caution that no conclusive statements can be made due to heterogeneity and methodological limitations in this case. However, there appears to be a consensus that IFC should be used with exercise or as supplement to other interventions, and less effective for use on its own <ref name=":6" /><ref name=":7" />.
| |
| | |
| Evidence for use of TENS in pain management was demonstrated in a 2014 critical review, in which both high frequency and low frequency TENS can provide an analgesic effect when applied at a strong, non-noxious intensity <ref name=":8">Vance C.G.T, Dailey D.L, Rakel B.A, Sluka K.A. Using TENS for pain control: the state of the evidence. Pain Management 2014;4:197-209.</ref>. High frequency TENS may be more appropriate for patients on opioid medication, as high frequency and low frequency parameters target different opioid receptors <ref name=":8" />. Varying these parameters has been a suggested strategy to avoid a development of tolerance in chronic pain conditions and prolong the analgesic effect if used daily. Populations which may benefit most from TENS include patients with post-operative pain, osteoarthritis, painful diabetic neuropathy, fibromyalgia, spinal cord injuries, and some acute pain conditions <ref name=":8" />.
| |
| | |
| Ultrasound is one of the most widely used electrotherapy modality <ref name=":5" />. Although it is commonly referred to as an electrotherapy modality, it uses mechanical energy as opposed to electrical energy. Mechanical energy is created through the vibration of emitting sound waves from the head of the ultrasound and transmits through to the targeted tissues, providing thermal or non-thermal effects dependent on the parameters <ref name=":5" />. Clinical application includes use for tissue repair, fracture healing, and wound healing among others which can result in a secondary effect of pain relief <ref name=":5" />. A 2010 meta-analysis suggests that ultrasound may be effective for improving physical function and reducing pain in osteoarthritic knee joints, however, the evidence is low quality and there is demand for more definitive clinical trials <ref name=":9">Loyola-Sanchez A, Richardson J, MacIntyre N.J. Efficacy of ultrasound therapy for the management of knee osteoarthritis: a systematic review with meta-analysis. Osteoarthritis and Cartilage 2010;18:1117-1126.</ref>. Low quality evidence has also been reported for ultrasound by a Cochrane review in its use for short-term benefits (6-weeks) in pain and function in individuals with calcific tendinitis <ref name=":10">Page M.J, Green S, Mrocki M.A, Surace S.J, Deitch J, McBain B, Lyttle N, Buchbinder R. Electrotherapy modalities for rotator cuff disease. Cochrane Database of Systematic Reviews 2016;6.</ref>. Further low quality evidence for ultrasound use has been shown in patients with non-specific chronic low back pain, for short-term improvement in function, although authors suggest this may not be clinically significant <ref name=":11">Ebadi S, Henschke N, Nakhostin Ansari N, Fallah E, van Tulder M.W. Therapeutic ultrasound for chronic low-back pain. Cochrane Database of Systematic Reviews 2014;14.</ref>. Unfortunately, no high-quality evidence exists for ultrasound’s reduction in pain for a number of conditions when compared to placebos <ref name=":9" /><ref name=":10" /><ref name=":11" />. This may be due to a lack of high quality randomized control trials and small sample sizes, creating a requirement for large trials with valid and robust methodology.
| |
| | |
| Laser therapy in clinical and research settings is typically referred to as low intensity laser therapy, or low level laser therapy. It is used as a form of light amplifier to provide an enhancement of certain properties of light energy which when delivered to the targeted tissues, result in a generation of heat, chemical change, disorder of molecular bonds and creation of free radicals <ref name=":5" />. Clinically, it can be used for wound healing, inflammatory arthropathies, soft tissue injuries, and pain relief <ref name=":5" />. Its use for pain relief was assumed to be a secondary effect of reducing an inflammatory state, however, it may also be attributed to a direct effect with characteristics of nerve conduction <ref>Vinck E, Coorevits P, Cagnie B, De Muynck M, Vangerstraeten G, Cambier D. Evidence of changes in sural nerve conduction mediated by light emitting diode irradiation. Lasers in medical science 2005;20:35-40.</ref>.
| |
| | |
| Evidence for low level laser therapy have been found through meta-analysis which suggest a strong inclination for its use in the reduction of chronic pain across various aetiologies <ref>Fulup A.M, Dhimmer S, Deluca J.R, Johanson D.D, Lenz R.V, Patel K.B, Douris P.C, Enwemeka C.S. A meta-analysis of the efficacy of laser phototherapy on pain relief. The Clinical Journal of Pain 2010;26:729-736.</ref>. Another systematic review with meta-analysis investigated the modality’s effect on neck pain, which found that low level laser therapy can be used to immediately reduce acute neck pain as well as reduce pain intensity in chronic neck pain patients <ref>Chow R.T, Johnson M.I, Lopes-Martins R.A.B, Bjordal J.M. Efficacy of low-level laser therapy in the management of neck pain: a systematic review and meta-analysis of randomized placebo or active-treatment controlled trials. The Lancet 2009;374:1897-1908.</ref>. A more recent double blinded placebo control study found that low level laser therapy can improve pain and function in patient with knee pain as well <ref>Leal-Junior E.C, Johnson D.S, Saltmarche A, Demchak T. Adjunctive use of combination of super-pulsed laser and light-emitting diodes phototherapy on nonspecific knee pain: double blinded randomized placebo-controlled trial. Lasers in medical science 2014;29:1839-1847.</ref>. Conversely, a meta-analysis performed in 1993 by Gam et al. when the clinical use of the modality was emerging, found no effect on pain in musculoskeletal conditions <ref>Gam A.N, Thorsen H, Lonnberg F. The effect of low-level laser therapy on musculoskeletal pain: a meta-analysis. Pain 1993;52:63-66.</ref>.
| |
| | |
| === Thermal modalities ===
| |
| Thermal modalities include thermotherapy and cryotherapy and can also be referred to as conductive modalities. Thermotherapy includes superficial heating agents such as hydrocollator packs, paraffin wax baths, warm whirlpool, and fluidotherapy <ref name=":12">Prentice W.E. ''Therapeutic Modalities in Rehabilitation''. 4<sup>th</sup> ed. New York: McGraw-Hill Medical; 2011.</ref>. While cryotherapy produce a tissue temperature decrease which include application methods such as ice massage, cold hydrocollator packs, contrast baths, cold whirlpool, cold spray, ice immersion, cryo-cuff, and cryokinetics <ref name=":12" />. Thermal modalities can also be used as adjuncts to exercise therapy and/or electrophysical modalities, for a variety of therapeutic purposes. Physiological Effects of cold and heat can be found listed below adapted from <ref name=":12" />.
| |
| | |
| ====Effects of Heat:''' ====
| |
| · Increased local temperature superficially
| |
| | |
| · Increased local metabolism
| |
| | |
| · Vasodilation of arterioles and capillaries
| |
| | |
| · Increased blood flow to targeted area
| |
| | |
| · Increased leukocytes and phagocytosis
| |
| | |
| · Increased capillary permeability
| |
| | |
| · Increased lymphatic and venous drainage
| |
| | |
| · Increased metabolic wastes
| |
| | |
| · Increased axon reflex activity
| |
| | |
| · Increased elasticity of muscles, ligaments, and capsule fibres
| |
| | |
| · Analgesia
| |
| | |
| · Increased formation of oedema
| |
| | |
| · Decreased muscle tone
| |
| | |
| · Decreased muscle spasm
| |
| | |
| ====Effects of Cold:''' ====
| |
| · Decreased local temperature, in some cases to a considerable depth
| |
| | |
| · Decreased metabolism
| |
|
| |
|
| · Vasoconstriction of arterioles and capillaries (initially)
| | * NPI have been employed as medical interventions (predating modern pharmacology), and are intended to improve quality of life, slow down deterioration or relieve pain. NPI also reduce health costs reduced and have minimal environmental impact.. |
| | * Following a healthy lifestyle is possibly the best NPI, contributing to improved health and quality of life.<ref name=":37">Herguedas AJ. [https://www.intechopen.com/chapters/73680 Non-Pharmacological Interventions in Preventive, Rehabilitative and Restorative Medicine.] InAlternative Medicine-Update 2020 Dec 21. IntechOpen. Available:https://www.intechopen.com/chapters/73680 (accessed 30.12.2022)</ref> See [[Lifestyle Medicine for Health and Disease Management]] |
|
| |
|
| · Decreased blood flow (initially)
| | == Physiotherapy: A Non-Pharmacological Intervention == |
| | A wide range of NPI modalities are used by physiotherapists, including manual therapies, electrophysical agents, thermotherapy, hydrotherapy, therapeutic exercise, meditation, and acupuncture. The physiotherapists' goal is to reduce pain and restore (or maintain) optimal physical functioning via these NPI. Take a look at some of the NPI's used: |
|
| |
|
| · Decreased nerve conduction velocity
| | == '''Patient education''' == |
| | [[File:Doctor patient.png|thumb|386x386px|Patient Education]] |
| | The importance of increasing a patient’s understanding of their condition and treatment plan is not only of benefit for improving a patient’s adherence to treatment, but can also improve health outcomes <ref>Adams R. Improving health outcomes with better patient understanding and education. Risk Management and Healthcare Policy 2010;3:61-72</ref>. Self-management of chronic conditions as well as preventative health intents rely heavily on provision of contemporary information and communication practice <ref name=":0">Wagner E.H, Austin B.T, Davis C, Hindmarsh M, Schaefer J, Bonomi A. Improving chronic illness care: translating evidence into action. Health Affairs 2001;20:64-78.</ref>. Primary focus for long term conditions commonly involves promotion of informed lifestyle choices, risk-factor modification, and active patient self-management <ref name=":0" />. Education can be provided through a variety of health care professionals, preferably done by providers who have undertaken adequate training for education, and patient communication. Recognized physiotherapy programmes typically include a component of patient education within their training. <ref>Forbes R, Mandrusiak A, Smith M, Russel T. Training physiotherapy students to educate patients: A randomized controlled trial. Patient Education and Counselling 2018;101:295-303.</ref>. See also [[Patient Education in Pain Management]] [[Patient Education for Parkinson's Drugs]] |
|
| |
|
| · Decreased delivery of leukocytes and phagocytes
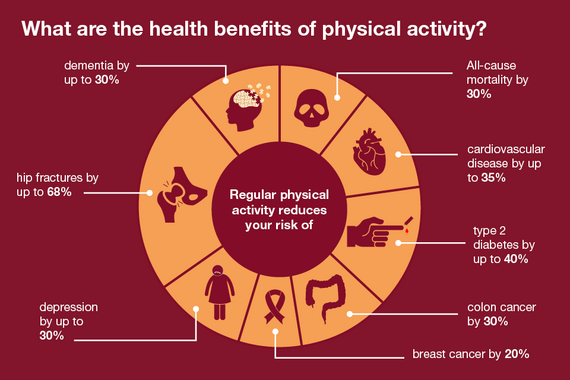
| | == '''Physical Activity''' == |
| | Physical activity prescription (a NPI) is an under-utilised tool for improving community health. In the right dose, physical activity can help to prevent, treat, and manage a range of chronic health conditions that increasingly impact the quality of life and physical function of individuals on a global scale.<ref>World Health Organization. [https://www.who.int/publications/i/item/9789241563871 Global health risks: mortality and burden of disease attributable to selected major risks]. Geneva: World Health Organization Press, 2009 Available:https://www.who.int/publications/i/item/9789241563871 (accessed 30.12.2022)</ref> |
| | [[File:Health-benefits-of-physical-activity.png|center|frameless|570x570px]] |
|
| |
|
| · Decreased lymphatic and venous drainage
| | == '''Electrotherapy modalities''' == |
| | *[[Current Concepts in Electrotherapy|E]][[Electrophysical|lectrophysical agents]] is a term describing electrical devices applied by trained professionals to an injury site in effort to enhance, expedite, or improve the treatment plan and recovery process. There are a wide range of electrotherapy modalities used in physical therapy. Conventionally, they are used for pain management, reducing swelling, increasing local blood flow, and breaking down scar tissue and can be applied across various stages of injury recovery <ref name=":5">Watson T. ''Electrotherapy: Modalities''. 2018 [online][viewed 12/04/2018]. Available from: <nowiki>http://www.electrotherapy.org/modalities</nowiki></ref>. |
| | * Common electrotherapy modalities used in pain management include [[Transcutaneous Electrical Nerve Stimulation (TENS)|transcutaneous electrical nerve stimulation (]]TENS), [[Interferential Therapy|interferential current]] (IFC), [[Ultrasound therapy|ultrasound]], and laser therapy. |
|
| |
|
| · Decreased muscle excitability
| | == Thermotherapy == |
| | [[Thermotherapy]], involves use of heat or cold |
|
| |
|
| · Decreased muscle spindle depolarization
| | # Heat can give relief in subacute and chronic inflammatory and traumatic disorders, Heat increases blood flow, helping reduce inflammation, oedema and exudates from connective tissue injuries. |
| | # Cold helps relieve muscle spasms, myofascial or traumatic pain and acute inflammation. |
|
| |
|
| · Decreased formation and accumulation of oedema
| | Thermal modalities can also be used as adjuncts to exercise therapy and/or electrophysical modalities, for a variety of therapeutic purposes <ref name=":12">Prentice W.E. ''Therapeutic Modalities in Rehabilitation''. 4<sup>th</sup> ed. New York: McGraw-Hill Medical; 2011.</ref>. |
| | |
| · Extreme aesthetic effects
| |
| | |
| Looking at the evidence for these thermal modalities, a Cochrane review was performed in 2006 by French et al. investigating the effects of superficial cold and heat for nonspecific low back pain <ref name=":13">French S.D, Cameron M, Walker B.F, Reggars J.W, Esterman A.J. A Cochrane review of superficial heat or cold for low back pain. Spine 2006;31:998-1006.</ref>. While heat and cold application is commonly recommended by clinicians for low back pain, the authors concluded that the evidence is not strong to support this common practice <ref name=":13" />. More specifically, they only found moderate evidence for continuous heat wraps to provide short term pain relief and improved function in acute and sub-acute back pain (≤ 3 months), with greater improvements with the addition of exercise to the thermotherapy. For cryotherapy, the evidence in this review for its treatment in non-specific low back pain was even more limited, and no conclusions could be drawn at the time of the review <ref name=":13" />. However, the results of this review was limited by many studies with poor methodologic quality. Since then, Dehghan and Farahbod conducted a randomized clinical trial in 2014 investigating both thermotherapy and cryotherapy’s effect on 87 patients with acute low back pain when compared to a routine pharmacologic control (naproxen) <ref name=":14">Dehghan M, Farahbod F. The efficacy of thermotherapy and cryotherapy on pain relief in patients with acute low back pain, a clinical trial study. Journal of Clinical & Diagnostic Research 2014;8:LC01-LC04.</ref>. This study found that both cryotherapy and thermotherapy relieved the acute low back pain, and due to their few side-effects, low economical cost and ease of accessibility, they were suggested to be used alongside pharmacological treatments such as naproxen, as supplementary modalities to reduce acute low back pain <ref name=":14" />. All together, these findings corroborate with a more recent literature review for musculoskeletal injuries. The authors agreed that evidence for use of thermotherapy is limited, with the greatest effects seen with heat wrap therapy for short-term relief of acute low back pain and disability, and additionally provides significantly greater pain relief than cryotherapy when used for delayed onset muscle soreness <ref name=":15">Malanga G.A, Yan N, Stark J. Mechanisms and efficacy of heat and cold therapies for musculoskeletal injury. Postgraduate Medicine 2014;127:57-65.</ref>. The requirement for more sufficiently powered and high-quality randomized control trials exploring the efficacy of cold and heat therapy for pain in various musculoskeletal conditions is ongoing <ref name=":13" /><ref name=":15" />.
| |
|
| |
|
| === Manual Therapy === | | === Manual Therapy === |
| Manual therapy can be defined differently across health professionals but can be described as another non-pharmacological, non-surgical, conservative option for management of a range of musculoskeletal conditions. These skilled, hands on techniques can be applied to patients’ spine and extremities for purpose of assessment and treatment. There are a wide variety of techniques that can be grouped into four major categories: manipulation, mobilization, static stretching, and muscle energy techniques <ref name=":16">Clar C, Trertsvadze A, Court R, Hundt G.L, Clarke A, Sutcliffe P. Clinical effectiveness of manual therapy for the management of musculoskeletal and non-musculoskeletal conditions: systematic review and update of UK evidence report. Chiropractic & Manual Therapies 2014;22:12.</ref>. Commonly, manipulation and mobilization of the spine are used for treatment of low back pain by physiotherapists and other health professionals such as osteopaths and chiropractors <ref name=":16" />. Although the effectiveness of these techniques is dependent on the skills of the handling clinician, it is important to look at the available evidence when deciding to implement this option into a treatment plan. | | Manual therapy has a long history within the profession of physical therapy. There are a wide variety of techniques that can be grouped into four major categories: manipulation, mobilization, static stretching, and muscle energy techniques <ref name=":16">Clar C, Trertsvadze A, Court R, Hundt G.L, Clarke A, Sutcliffe P. Clinical effectiveness of manual therapy for the management of musculoskeletal and non-musculoskeletal conditions: systematic review and update of UK evidence report. Chiropractic & Manual Therapies 2014;22:12.</ref>. Contemporary research reveals intricate neurophysiologic mechanisms are also at play and the beneficial psychological effects of providing hands-on examination and intervention have been substantiated.<ref>Huijbregts PA. [https://www.sciencedirect.com/topics/medicine-and-dentistry/manual-therapy Manual therapy]. InPain Procedures in Clinical Practice 2011 Jan 1 (pp. 573-596). Hanley & Belfus. Available from: https://www.sciencedirect.com/topics/medicine-and-dentistry/manual-therapy (last accessed 30.12.2022)</ref> |
| | |
| A UK evidence report of manual therapies published in 2010 reviewed its effectiveness for the management of a variety of musculoskeletal and non-musculoskeletal conditions <ref name=":17">Bronfort G, Haas M, Evans R, Leininger B, Triano J. Effectiveness of manual therapies: the UK evidence report. Chiropratic & Osteopathy 2010;18:3.</ref>. The report included 49 systematic reviews, 16 evidence based clinical guidelines, and 46 randomized controlled trials not included in the former reviews and guidelines. The report found some evidence that spinal manipulation and mobilization is effective for adults with low back pain of all durations, as well as migraines, cervicogenic headaches and cervicogenic dizziness <ref name=":17" />. Authors suggested manipulation and mobilization is effective for a variety of joint conditions in the extremities. Thoracic mobilization and manipulation is effective for acute and sub-acute neck pain. However, the report found inconclusive evidence for cervical manipulation and mobilization for neck pain at any duration, as well as manipulation and mobilization for mid back pain, sciatica, tension headaches, coccydyina, fibromyalgia, premenstrual syndrome, temporomandibular joint conditions, and pneumonia in older adults <ref name=":17" />.
| |
| | |
| An update to this UK evidence report was published in 2014 to address the inconclusive and negative ratings in the previous report <ref name=":16" />. The updated report concluded that all together, there was limited high quality evidence to support the effectiveness of manual therapy. Reasons for these ratings and unreliable estimations are due to paucity, poor quality methodologies, and heterogeneity of studies, in addition to differences in experience, training and approaches of the clinical providers <ref name=":16" />. Further research in this area will need to include: qualitative methods to involve patient attitudes and opinions; greater consistency across research groups; more non-musculoskeletal disorders; and high quality, long-term, randomized clinical trials investigating clinical and cost-effectiveness <ref name=":16" />.
| |
| | |
| Clinical readers interested in specific patient groups will find more information in these reports found [https://chiromt.biomedcentral.com/articles/10.1186/1746-1340-18-3 here] (2010) and [https://chiromt.biomedcentral.com/articles/10.1186/2045-709X-22-12 here] (2014)
| |
|
| |
|
| === Therapeutic exercise === | | === Therapeutic exercise === |
| Therapeutic exercise techniques include passive movements, active assisted movements, active movements, resisted movements and assisted resisted movements with aims to correct impairment, improve musculoskeletal function or maintain well-being <ref name=":18">Lieberman J.A, Bockenek W.L. ''Physical Medicine and Rehabilitation: Therapeutic Exercise''. 2016. [online] [viewed 15/04/2018]. Available from: <nowiki>https://emedicine.medscape.com/article/324583-overview#showall</nowiki></ref>. To further a pain management approach, the option to perform these movements on land or in water can be explored. Therapeutic exercise can be prescribed to accomplish the following aims <ref name=":18" />: | | [[Therapeutic Exercise|Therapeutic exercise]] techniques include passive movements, active assisted movements, active movements, resisted movements and assisted resisted movements with aims to correct impairment, improve musculoskeletal function or maintain well-being <ref name=":18">Lieberman J.A, Bockenek W.L. ''Physical Medicine and Rehabilitation: Therapeutic Exercise''. 2016. [online] [viewed 15/04/2018]. Available from: <nowiki>https://emedicine.medscape.com/article/324583-overview#showall</nowiki></ref>. |
| | |
| · Improve and enable ambulation
| |
| | |
| · Release contracted muscles, tendons, and fascia
| |
| | |
| · Mobilize joints
| |
| | |
| · Improve circulation and respiratory capacity
| |
| | |
| · Improve coordination
| |
| | |
| · Reduce rigidity
| |
| | |
| · Improve balance
| |
| | |
| · Promote relaxation
| |
| | |
| · Improve and maintain muscular strength and endurance
| |
| | |
| · Improve exercise performance and functional capacity
| |
| | |
| Evidence supporting the use of therapeutic exercise is vast and dependent upon specific patient populations. The following is a summary of evidence for therapeutic exercise in patient populations for: stroke; multiple sclerosis; balance impairment; osteoarthritis; and mental health.
| |
| | |
| There have been several published studies showing the benefits of therapeutic exercise in post-stroke patients. In subacute stroke patients, prescribed exercises increased endurance, balance and mobility resulting in improved function and quality of life <ref>Duncan P.W, Studenski S, Richards L, Gollub S, Lai S.M, Reker D, Perera S, Yates J, Koch V, Rigler S, Johnson D. Randomised clinical trial of therapeutic exercise in subacute stroke. Stroke 2003;34:2173-2180.</ref>. The same patient population also experienced improvement in depressive symptoms <ref>Lai S.M, Studenski S, Richards L, Perera S, Reker D, Rigler S, Duncan P.W. Therapeutic exercise and depressive symptoms after stroke 2006;54:240-247.</ref>. In other randomized control trials within this population, improvements in activities of daily living were found in subacute stroke patients, as well aquatic therapy improved gait in stroke patients with hemiplegia <ref>Koc A. Exercise in patients with subacute stroke: a randomized controlled pilot study of home-based exercise in subacute stroke. Work 2015;52:541-547.</ref><ref>Park B.S, Noh J.W, Kim M.Y, Lee L.K, Yang S.M, Lee W.D, Shin Y.S, Kim J.H, Lee J.U, Kwak T.Y, Lee T.H, Kim J.Y, Park J, Kim J. The effects of aquatic trunk exercise on gait and muscle activity in stroke patients: a randomized controlled pilot study. Journal of Physical Therapy Science 2015;27:3549-3553.</ref>. Furthermore, a systematic review found that progressive resistance exercise for acute and chronic stroke patients improves strength and activity without increasing spasticity <ref>Ada L, Dorsch S, Canning C.G. Strengthening interventions increase strength and improve activity after stroke: a systematic review. The Australian journal of physiotherapy 2006;52:241-248.</ref>.
| |
| | |
| Many types of therapeutic exercise have found to be beneficial for patients with multiple sclerosis as well, although for safe application, certain precautions are required including close supervision of a health professional <ref name=":18" />. Symptoms in this population are generally exacerbated in higher ambient temperatures, and therefore interval training and/or precooling before therapeutic exercise is recommended <ref name=":18" />. A Cochrane review published in 2005 revealed strong evidence for improvements in strength, mobility-related activities, and exercise tolerance, with possible benefits in mood and upper extremity function <ref>Rietberg M.B, Brooks D, Uitdehaag B.M, Kwakkel G. Exercise therapy for multiple sclerosis. Cochrane Database for Systematic Reviews 2005;1.</ref>. However, a 2013 systematic review could not conclude as many of these findings, but suggested exercise was safe and may be beneficial for this population <ref>Sa M.J, Exercise therapy and multiple sclerosis: a systematic review. Journal of Neurology 2014;261:1651-1661.</ref>. As multiple sclerosis is a progressive condition, maintaining function with therapeutic exercise rather than improving it may be a more realistic goal for this population <ref>Sandoval A.E. Exercise in multiple sclerosis. Physical Medicine and Rehabilitation Clinics of North America 2013;24:605-618.</ref>. However, a smaller study investigating use of pilates for wheelchair-bound patients with moderate-to-severe multiple sclerosis did find improvements in back and shoulder pain and sitting balance <ref>Van der Linden M.L, Bulley C, Geneen L.J, Hooper J.E, Cowan P, Mercer T.H. Pilates for people with multiple sclerosis who use a wheelchair: feasibility, efficacy and participant experiences. Disability and Rehabilitation 2014;36:932-939.</ref>.
| |
| | |
| Balance impairment is a major factor in the older population which can lead to falls and injury, and exercise has been a common recommendation in fall prevention <ref>Rubenstein L.Z. Falls in older people: epidemiology, risk factors and strategies for prevention. Age and Ageing 2006;35:ii37-ii41.</ref>. A Cochrane review published in 2011 exploring exercise to improve balance in older people concluded at the time of publishing there was weak evidence that some types of exercise were moderately effective <ref>Howe T.E, Rochester L, Neil F, Skelton D.A, Ballinger C. Exercise for improving balance in older people. Cochrane Database for Systematic Reviews 2011;11.</ref>. It was unclear which types of exercise were optimal for improving balance in the older population (≥60 years of age) living at home and residential care. However, in general, the more effective programmes ran three times weekly for three months and incorporated dynamic exercise in standing. The authors suggested the missing data and poor methods of many included studies highlighted a requirement for high-quality research in the area. A comprehensively tested and effective fall prevention exercise programme used by physiotherapists for older people is the Otago Exercise Programme <ref>Gillespie W.J, Robertson M.C, Lamb S.E, Cumming R.G, Rowe B.H. Interventions for preventing falls in elderly people. Cochrane Database of Systematic Reviews 2003;3.</ref><ref name=":19">ACC. ''Otago Exercise Programme to prevent falls in older adults''. New Zealand: Accident Compensation Corporation; 2007.</ref>. The programme is an individualized, home-based strength and balance retraining programme for older adults which is delivered or supervised by a physiotherapist <ref name=":19" />. More information on the delivery of the Otago Exercise Programme can be found [https://www.acc.co.nz/assets/injury-prevention/acc1162-otago-exercise-manual.pdf here].
| |
| | |
| Apart from therapeutic exercise, there are a number of non-pharmacological interventions that are of use to address falls in the elderly population which have been recently and robustly systematically reviewed, of which, exercise and multifactorial interventions emerged as optimal options in reduction of falls <ref name=":4" />. Further information regarding evidence of several non-pharmacological interventions for fall prevention in elderly populations across a variety of settings can be found [http://journals.plos.org/plosone/article?id=10.1371/journal.pone.0161579 here].
| |
| | |
| Osteoarthritic joints can also benefit from therapeutic exercise. Physiotherapists generally use therapeutic exercise in this population for purposes of improving strength, range of motion, and pain management. Systematic reviews published on this topic have shown that therapeutic exercises such as resistance and endurance training can reduce pain and improve balance in osteoarthritic knee patients <ref>Fransen M, McConnell S. Land-based exercise for osteoarthritis of the knee: a meta-analysis of randomized controlled trials. Journal of rheumatology 2009;36:1109-1117.</ref><ref>Tanaka R, Ozawa J, Kito N, Moriyama H. Efficacy of strengthening of aerobic exercise on pain relief in people with knee osteoarthritis: a systematic review and meta-analysis of randomized controlled trials. Clinical Rehabilitation 2013;27:1059-1071.</ref><ref>Silva A, Serrao P.R, Driusso P, Mattiello S.M. The effects of therapeutic exercise on the balance of women with knee osteoarthritis: a systematic review. Brazilian journal of physical therapy 2012;16:1-9.</ref>. Similar results are found when looking at individuals with osteoarthritis of the hip, where a systematic review revealed that physical function can improve as well as reduce falls risk when using a combination of functional and aquatic exercises <ref>Romeo A, Parazza S, Boschi M, Nava T, Vanti C. Manual therapy and therapeutic exercise in the treatment of osteoarthritis of the hip: a systematic review. Reumatismo 2013;65:63-74.</ref>.
| |
| | |
| Therapeutic exercise can also be of very strong benefit as a non-drug alternative for mental health issues <ref name=":20">Rimes R.R, de Souza Moura A.M, Lamego M.K, de Sa Filho A.S, Manochio J, Paes F, Carta M.G, Mura G, Wegner M, Budde H, Ferreira Rocha N.B, Rocha J, Tavares J.M, Arias-Carrion O, Nadi A.E, Yuan T.F, Machado S. Effects of exercise on physical and mental health, and cognitive and brain functions in schizophrenia: clinical and experimental evidence. CNS & neurological disorders drug targets 2015;14:1244-1254.</ref><ref name=":21">Oertel-Knochel V, Mehler P, Thiel C, Steinbrecher K, Malchow B, Tesky V, Ademmer K, Prvulovic D, Banzer W, Zopf Y, Scmitt A, Hansel F. Effects of aerobic exercise on cognitive performance and individual psychopathology in depressive and schizophrenia patients. European archives of psychiatry and clinical neuroscience 2014;264:589-604.</ref><ref name=":22">Hess N.C.L, Dieberg G, McFarlane J.R, Smart N.A. The effect of exercise intervention on cognitive performance in persons at risk of, or with, dementia: a systematic review and meta-analysis. Healthy Aging Research 2014;3.</ref>. Overall, positive effects have been shown for mental health, cognition and brain activity as a result of a variety of therapeutic exercise programmes <ref name=":20" />. Aerobic exercise has shown to significantly reduce depressive symptoms and state anxiety values in major depressive disorders, reduce negative symptoms severity of schizophrenic patients, and has been suggested to help reduce psychopathological symptoms and improve cognitive skills <ref name=":21" />. Furthermore, a recent meta-analysis found further support for exercise to improve neurocognitive function in people at risk of, or with, dementia <ref name=":22" />.
| |
| | |
| == Non-pharmacological options for referral and signposting ==
| |
|
| |
|
| === Therapeutic communities ===
| | See also [[Exercise and Activity in Pain Management]] |
| Therapeutic communities come in many forms and each are tailored to address a variety of long term issues including personality disorders, mental health, learning disabilities, and substance abuse <ref>TCTC. ''Types of Therapeutic Communities.'' 2013. [online] [viewed 16/04/2018] Available from: <nowiki>https://www.therapeuticcommunities.org/what-is-a-tc/types-of-tcs/</nowiki></ref>. These communities are group-based with a participative approach in a residential or day unit setting. Since the target population for each therapeutic community varies, gaining access to one is best done by directly contacting the programme for a self-referral, however, in most cases you will require a referral from a doctor or social worker. In these cases, physiotherapists and other relevant health professionals would be wise to be aware of local therapeutic communities and their respective access procedures, in order to efficiently sign post patients that express long-term substance abuse concerns from overprescribed medications. Signposting these patients will likely require a discussion with the MDT or referring physician in order to determine if overprescription is an issue in the suspected addiction. A 2010 meta-analysis reviewing therapeutic communities’ effect for individuals with co-occurring substance abuse and mental disorders, found supporting evidence for significant treatment effects for substance use, mental health, crime, employment and housing <ref>Sacks S, McKendrick K, Sacks J.Y, Cleland C.M. Modified Therapeutic Community for Co-Occurring Disorders: Single investigator meta analysis. Substance Abuse 2010;31:146-161.</ref>. More information about therapeutic communities can be found at [https://www.therapeuticcommunities.org/ The Consortium for Therapeutic Communities.]
| |
|
| |
|
| === Mind-body therapies === | | == Meditation == |
| While acute pain can resolve quickly with appropriate use of analgesics, medications and treatment of underlying causes, chronic pain can cause clinicians and patients significant concern. Human perception of pain is not purely somatic, it involves regions of the brain that register and modify pain signals including brain centres engaged with stress, emotion, attention, beliefs, conditioning, mood, and cognition <ref>Zeidan F, Grant J.A, Brown C.A, McHaffie J.G, Coghill R.C. Mindfulness meditation-related pain relief: evidence for unique brain mechanisms in the regulation of pain. Neuroscience letters 2012;520:165-173.</ref>. Mind-body therapies can be described as interventions that change an individual’s mental and/or emotional state which aim to generate corresponding changes in the body, including pain perception. A variety of mind-body therapies can be used in the management of chronic pain as a sole treatment, however they may be better used as a complementary approach to other therapies <ref>Astin J.A. Mind-body therapies for the management of pain. Clinical journal of pain 2004;20:27-32.</ref>. When seeking a mind-body therapist for chronic pain, it is advisable to first consult a GP for a formal diagnosis, as many of these clinical practices are unregulated in the UK. The following is a summary of evidence on a few commonly used mind-body approaches for chronic pain management including: guided imagery; cognitive hypnotherapy; and cognitive behavioural therapy.
| | [[Meditation]] |
|
| |
|
| Guided imagery’s use in the management of chronic pain stems from relaxation, and distracting the individual’s mind from mental elaboration of pain, through use of therapeutic images. A systematic review revealed eight of nine randomized clinical trials found guided imagery results in significant reduction of musculoskeletal pain, however, the methodologies of included studies were graded medium to low and therefor the encouraging results were inconclusive <ref>Posadzki P, Ernst E. Guided imagery for musculoskeletal pain: a systematic review. Clinical journal of pain 2011;27:648-653.</ref>. Guided imagery is often paired with music therapy, and administered by Music Therapists who are required to be registered with the [http://www.hcpc-uk.org/aboutregistration/professions/index.asp?id=1#profDetails Health & Care Professions Council] in the UK.
| | * Benefits include: Removes the accumulated stress and help increase the positive energy; decreases anxiety, depression, and pain (both physical and psychological); increases regional cerebral blood flow in the frontal and anterior cingulate region of the brain; decreases sympathetic overstimulation reduces cholesterol and risk of heart disease and helps in reducing smoking; has been shown to be beneficial in epilepsy, premenstrual symptoms, menopausal symptoms, autoimmune illness, and emotional disturbance in neoplastic disease; improves telomerase activity in the body which slows down the aging process and related diseases.<ref>Sharma H. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4895748/ Meditation: Process and effects.] Ayu. 2015 Jul;36(3):233. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4895748/ (accessed 30.12.2022)</ref> |
|
| |
|
| Cognitive hypnotherapy, also referred to as hypnosis, was one of the first mind-body therapies used for managing chronic pain. Exact definition of hypnosis can vary but it is considered a natural state of mind by those who practice it <ref>NCH. ''What is hypnosis?'' 2018. [online] [viewed 16/04/2018] Available from: <nowiki>https://www.hypnotherapists.org.uk/hypnotherapy/hypnotherapy-faq/</nowiki></ref>. Using progressive relaxation techniques, service users can learn self-hypnosis for self-management as well. A 2012 review suggests there is evidence identified for chronic pain management in subjects with cancer, osteoarthritis, sickle cell disease, fibromyalgia, temporomandibular joint disorders, non-cardiac chest pain, and disability related chronic pain <ref>Elkins G, Johnson A, Fisher W. Cognitive hypnotherapy for pain management. American journal of clinical hypnosis 2012;54:294-310.</ref>. An earlier study found hypnotherapy may provide pain relief in irritable bowel syndrome with beneficial effects measured after 5 years <ref>Gonsalkorale W.M, Miller V, Afzal A, Whorwell P.J. Long term benefits of hypnotherapy for irritable bowel syndrome. Gut 2003;52:1623-1629.</ref>. Currently, hypnotherapy is not a regulated profession in the UK, however, the [https://www.hypnotherapists.org.uk/ National Council for Hypnotherapy] is one of the UK’s largest not-for-profit professional association, with fully insured members.
| | == Mindfulness == |
| | * Mindfulness is a [[Stress and Health|stress]]-reducing strategy where an individual develops an awareness that arises through paying attention, on purpose, in the present moment, non-judgmentally and accepting them as they are. |
| | * [[Mindfulness Meditation in Chronic Pain Management]] |
|
| |
|
| Cognitive behavioural therapy (CBT) is a talking therapy that can help manage issues beyond chronic pain by changing individuals’ perceptions and behaviours. Differing from other talking therapies, CBT focuses on individuals’ current problems rather than past problems, then uses practical ways to improve a daily state of mind <ref>NHS. ''Cognitive Behavioural Therapy''. 2016 [online] [viewed 16/04/2018] Available from: <nowiki>https://www.hypnotherapists.org.uk/hypnotherapy/hypnotherapy-faq/</nowiki> </ref>. There is a strong evidence base for CBT’s use in management of a variety of chronic pain conditions <ref>Roland D, Prince J, Koppe H. Patient centred CBT for chronic pain. Australian family physician 2004;33:339-344.</ref>. A 2012 narrative review also suggests that CBT is beneficial for treatment of nonspecific chronic low back pain and should be incorporated into MDT interventions for a more patient-centred approach <ref>Sveinsdottir V, Eriksen H.R, Reme S.E. Assessing the role of cognitive behavioral therapy in the management of chronic nonspecific back pain. Journal of pain research 2012;5:371-380.</ref>. Finally, a 2011 article published in Best Practice & Research Clinical Rheumatology, suggests CBT coupled with exercise should be integrated into a multi-component approach for chronic widespread pain conditions like fibromyalgia <ref>Hassett A.L, Williams D.A. Non-pharmacological treatment of chronic widespread musculoskeletal pain. Best practice and research: Clinical rheumatology 2011;25:299-309.</ref>. The article includes methods for how exercise and CBT can be combined using evidence-based guidelines. In the UK, CBT is free under the National Health Service (NHS) when referred from a GP. Although psychological therapies are unregulated at the moment in the UK, the [http://www.cbtregisteruk.com/Default.aspx British Association for Behavioural & Cognitive Psychotherapies] keeps a register of accredited therapists.
| | == Virtual Reality == |
| | During physical therapy, virtual reality (VR) can shorten recovery times by e.g. |
|
| |
|
| === Biofield Therapies ===
| | * Making it easier for patients with pain to do their exercises. VR changes the focus from pain to an absorbing alternative reality that entrances, motivates and encourages them to complete perform the task. |
| Biofield therapies is a term coined in 1992 in a United States National Institutes of Health Conference <ref>Rubik B, Pavek R, Greene E, Laurence D, Ward, R, Al E. ''Alternative medicine: expanding medical horizons: a report to the National Institutes of Health on alternative medical systems and practices in the United States.'' Washington, DC: US Government Printing Office; 1995.</ref>. They can be described as non-invasive, non-pharmacological, practitioner-mediated therapies which utilize the biofield of the practitioner and service user to stimulate a response in the service user, sometimes referred to as a “healing response”. Common biofield therapies include Reiki, therapeutic touch, and healing touch, among many others. These therapies are not generally integrated into conventional clinical care, likely due to limited understanding of mechanisms and gaps in research base. While there may be pressure for these therapies to demonstrate plausible physiological mechanisms, an argument can be made that these mechanisms are important, however, not essential for conducting and analysing robust clinical trials. A systematic review on best evidence synthesis for biofield therapies published in 2010 found most studies were of medium quality and typically did not meet minimum standards for validity of inferences <ref name=":23">Jain S, Mills P.J. Biofield therapies: helpful or full of hype? A best evidence synthesis. International journal of behavioral medicine 2010;17:1-16.</ref>. The review did report that there is strong evidence for reducing self-reported pain intensity in a variety of populations, including elderly patients with chronic pain. Another systematic review in 2009 explored the therapeutic effects of Reiki <ref name=":24">vanderVaart S, Jijsen V.M, de Wildt S.N, Koren G. A systematic review of the therapeutic effects of Reiki. Journal of alternative and complementary medicine 2009;15:1157-1169.</ref>. This review was unable to derive any definitive conclusions due to significant methodological and reporting limitations of existing studies investigating effectiveness of Reiki. While nine of the twelve included clinical trials found significant therapeutic effects using Reiki, the Jadad Quality score used in the review found eleven of the twelve studies were ranked as “poor”. It appears the consensus among relevant reviews in the area of various biofield therapies conclude that while the strongest evidence is found in symptom management of pain, there is a demand for high-quality studies for further investigation and recommendations <ref name=":23" /><ref name=":24" /><ref>Jain S, Hammerschlag R, Mills P, Cohen L, Krieger R, Vieten C, Lutgendorf S. Clinical studies of biofield therapies: summary, methodological challenges, and recommendations. Global advances in health and medicine 2015;4:58-66.</ref>.
| | * Helping patients who are recovering from a stroke to be able to practice specific movements without the risk of further injuring themselves by a fall. This boosts confidence when it they are then ready to move in real-life setting.<ref>News Medical Applications of Virtual Reality in Medicine Available:https://www.news-medical.net/health/Applications-of-Virtual-Reality-in-Medicine.aspx (accessed 30.12.2022)</ref> |
|
| |
|
| === Acupuncture ===
| | Findings from a scoping review<ref>Asadzadeh A, Samad-Soltani T, Salahzadeh Z, Rezaei-Hachesu P. [https://www.sciencedirect.com/science/article/pii/S2352914821000526 Effectiveness of virtual reality-based exercise therapy in rehabilitation: A scoping review. Informatics in Medicine] Unlocked. 2021 Jan 1;24:100562.</ref> suggests virtual reality intervention is beneficial for exercise therapy and it can be used for various rehabilitation purposes, such as pain management, improving functional ability, increasing range of motion, promoting muscular strength, increasing motivation, and enhancing quality of life. Many studies state to have use Nintendo Wii for developing VR systems in exercise therapy; more research is needed to confirm and improve the effectiveness of the treatments. |
| Acupuncture is a well-known and most prominent part of Chinese medicine in western medicine <ref name=":25">CAMDOC Alliance, ECH, ECPM, ICMART, IVAA. ''The regulatory status of complementary and alternative medicine for medical doctors in Europe.'' Brussels: 2010.</ref>. The aim of the practice is to affect body functions, as well as stimulate and restore the body’s own regulatory system through use of needles, pressure and/or heat on distinctive locations on the human body <ref name=":25" />. This non-pharmacological option is often incorporated in several clinical settings of conventional medicine, including qualified clinicians in physiotherapy <ref name=":25" />. There is extensive research exploring the use of acupuncture in the management of a variety of chronic pain conditions including low back pain, neck pain, and osteoarthritis, as well as tension-type and migraine headaches <ref name=":26">Liu L, Skinner M, McDonough S, Mabire L, Baxter G.D. Acupuncture for low back pain: an overview of systematic reviews. Evidence-Based Complementary and Alternative Medicine: eCAM 2015;2015 [online] [viewed 17/04/2018] Available from: <nowiki>http://doi.org/10.1155/2015/328196</nowiki></ref><ref name=":27">Seo S.Y, Lee K.B, Shin J.S, Lee J, Kim M.R, Ha I.H, Ko Y, Lee Y.J. Effectiveness of Acupuncture and electroacupuncture for chronic neck pain: a systematic review and meta-analysis. American journal of Chinese medicine 2017;45:1573-1595.</ref><ref name=":28">Ezzo J, Hadhazy V, Birch S, Berman B. Acupuncture for osteoarthritis of the knee: a systematic review. Arthritis & Rheumatology 2001;44:819-825.</ref><ref name=":29">Linde K, Allais G, Brinkhaus B, Fei Y, Mehring M, Shin B.C, Vickers A, White A.R. Acupuncture for the prevention of tension-type headache. Cochrane Database for Systematic Reviews 2016;4.</ref><ref name=":30">Linde K, Allais G, Brinkhaus B, Fei Y, Mehring M, Vertosick E.A, Vickers A, White A.R. Acupuncture for the prevention of episodic migraine. Cochrane Database for Systematic Reviews 2016;6.</ref>. In 2015, an overview of systematic reviews for use of acupuncture on low back pain was published <ref name=":26" />. While overall methodological quality of reviews was low and external validity was weak, a number of conclusions were drawn. For acute low back pain, there was inconsistent evidence that acupuncture has a larger effect on pain relief and improved function compared to sham acupuncture. Conversely, for chronic low back pain, there was consistent evidence that acupuncture either used in isolation or with a conventional therapy, can provide short-term and clinically relevant improvements in pain and function. A recent systematic review with meta-analysis considering the effects of acupuncture on neck pain was published in 2017 <ref name=":27" />. Authors concluded that acupuncture for chronic neck pain has similar effects to conventional medicine for pain reduction and disability, when compared to each other, but is more effective for pain relief when both were used in combination. However, the review added that definitive conclusions were difficult to make due to high risk of bias and imprecision of the included studies. Research for use of acupuncture for osteoarthritis tends to focus around the knee joint. A systematic review regarding its effectiveness on knee joints suggest that acupuncture may play a role for treatment of this population, but currently there is insufficient evidence to determine its efficacy in comparison to conventional treatments <ref name=":28" />. Cochrane reviews have been published in 2016 for effects of acupuncture on both migraine attacks, and tension-type headaches <ref name=":29" /><ref name=":30" />. The review for tension-type headaches found that acupuncture is an effective treatment for frequent episodic or chronic tension-type headaches, however due to the moderate quality of evidence, further trials are needed in comparing with conventional treatment options <ref name=":29" />. In regards to preventing migraine attacks, available evidence shows that acupuncture in combination with symptomatic treatment of migraine attacks, can reduce the frequency of migraine headaches, and may produce similar effects to pharmacological prophylactic treatment <ref name=":30" />.
| |
|
| |
|
| Overall, acupuncture is a valid and reasonable option to consider for individuals to manage certain chronic pain conditions, although, clinical guidelines are inconsistent regarding recommendations <ref name=":26" /><ref name=":27" /><ref name=":28" /><ref name=":29" /><ref name=":30" />. Acupuncture treatments for pain are mainly covered through private insurance companies in the UK, however, some treatments are also provided by the NHS <ref name=":25" />. A large professional and self-regulatory body for the practice of acupuncture is the British Acupuncture Council who are members of the Accredited Resister scheme run by the Professional Standards Authority. Clinical readers looking to ensure patients find a qualified professional in this area, can be directed to the [https://www.acupuncture.org.uk/ British Acupuncture Council website]. There are very few side effects from acupuncture when practiced by qualified practitioners, any minor side effects occurring are mild and self-correcting according to the British Acupuncture Council.
| | See the below examples of how VR can be used as a NPI |
|
| |
|
| === Massage Therapy ===
| | * [[Virtual Reality and Parkinson's]], |
| The terms massage and massage therapy have been defined and differentiated at a 2010 best practice symposium for the profession involving thirty-two experts in the field of massage therapy <ref name=":31">Kennedy A.B, Cambron J.A, Sharpe P.A, Travillian R.S, Saunders R.P. Clarifying definitions for the massage therapy profession: the results of the best practices symposium. International journal of therapeutic massage & bodywork 2016;9:15-26.</ref>. In general, massage is a patterned and purposeful soft tissue manipulation with or without emollients, liniments, thermal modalities or other external apparatus with aims of therapeutic change. Massage therapy includes the addition of non-hands-on components such as health promotion, and client education for self-care and maintenance <ref name=":31" />. Massage therapy is another non-pharmacological approach that has been extensively researched, although has been burdened by poor methodological studies. A 2006 systematic review of twenty studies evaluated the clinical effectiveness of therapeutic massage for symptomatic relief of musculoskeletal pain <ref name=":32">Lewis M, Johnson M.I. The clinical effectiveness of therapeutic massage for musculoskeletal pain: a systematic review. Physiotherapy 2006;92:146-158.</ref>. With positive results for massage compared to no treatment or sham treatment in many studies, the available evidence at the time was inconclusive due to small sample sizes, low methodological quality, and insufficient dosing <ref name=":32" />. Due to the large number of systematic reviews published on massage therapy’s effect on non-specific low back pain, a systematic review of nine systematic reviews was completed in 2013 <ref name=":33">Kumar S, Beaton K, Hughes T. The effectiveness of massage therapy for the treatment of nonspecific low back pain: a systematic review of systematic reviews. International journal of general medicine 2013;4:733-741.</ref>. The methodological quality of the reviews varied from poor to excellent, but the primary research informing the individual reviews was generally weak quality. Overall, the 2013 systematic review found that a small body of evidence emerged to support the use of massage therapy for short-term treatment of non-specific low back pain, although authors cautioned the interpretation of this conclusion due to the methodological limitations of the primary research <ref name=":33" />. Finally, a recent systematic review with meta-analysis was published in 2017, with fifteen studies exploring the efficacy of massage therapy for shoulder pain <ref>Yeun Y.R. Effectiveness of massage therapy for shoulder pain: a systematic review and meta-analysis. Journal of physical therapy science 2017;29:936-940.</ref>. The author of the review suggested that massage therapy is effective for improving shoulder pain in the short-term, although, further research using randomized controlled trials with large sample sizes is required in order to make conclusive evidence-based recommendations. Massage therapy is another unregulated profession in the UK, however, the [https://www.cnhc.org.uk/ Complementary & Natural Healthcare Council] is a UK voluntary regulator for various health practitioners including massage therapists. Their registered practitioners comply with the council’s standards of conduct, ethics and performance so service users can be confident the therapists are properly trained, qualified and insured.
| | * [[Virtual Reality Treatment for Multiple Sclerosis]], |
| | * [[Virtual Reality for Individuals Affected by Stroke]], |
| | * [[Virtual Reality As a Memory Aid in Cognitive Impaired Older adults]]. |
|
| |
|
| === Chiropractic === | | == Other NPIs == |
| Chiropractic is also a non-pharmacological type of complementary and alternative treatment, as it is not considered conventional medical treatment. In these treatments, a chiropractor uses a hands-on approach to help relieve problems with bones, muscles and joints <ref name=":34">GCC. ''About Chiropractic''. 2013. [online] [viewed 17/04/2018]. Available from: <nowiki>http://www.gcc-uk.org/about-us/about-chiropractic/</nowiki> </ref>. Similar to physiotherapists, the first visit entails an assessment to determine if the profession is suitable and which techniques may help. Techniques used by chiropractors include spinal manipulation, short and sharp thrusting movements, gradual joint movements and muscle stretches <ref name=":34" />. A variety of uses for chiropractic include pain for backs, necks, joint pains, tension-type headaches, migraine prevention and sports injury conditions <ref name=":34" />. A 2013 systematic review with meta-analysis explored the efficacy of manipulative therapy in adults with complaints of pain compared to sham manipulation, involving 19 studies <ref name=":35">Scholten-Peeters G.G, Thoomes E, Konings S, Beijer M, Verkerk K, Koes B.W, Verhagen A.P. Is manipulative therapy more effective than sham manipulation in adults?: a systematic review and meta-analysis. Chiropractic & manual therapies 2013;21 [online] [viewed 17/04/2018] Available from: <nowiki>http://doi.org/10.1186/2045-709X-21-34</nowiki></ref>. Results included moderate level of evidence for manipulative therapy’s immediate effect on pain relief, but lower evidence at short-term follow up. Similar results were found in patients with musculoskeletal conditions <ref name=":35" />. Concluding statements were that manipulative therapy has a clinically relevant effect to reduce pain, but not disability. In regards to non-specific low back pain, a 2016 systematic review of six pragmatic studies found moderate evidence to support chiropractic care in producing similar results to other types of care, including physical therapy <ref name=":36">Blanchette M.A, Stochkendahl M.J, Borges Da Silva R, Boruff J, Harrison P, Bussieres A. Effectiveness and economic evaluation of chiropractic care for the treatment of low back pain: a systematic review of pragmatic studies. PLOS ONE 2016;11 [online] [viewed 17/04/2018] Available from: <nowiki>https://doi.org/10.1371/journal.pone.0160037</nowiki></ref>. However, similar conclusions could not be made when compared to medical care and exercise therapy <ref name=":36" />.
| |
|
| |
|
| Chiropractic is generally very safe when receiving treatment from trained and registered clinicians. Besides minor adverse effects from the treatment such as aches and pains, stiffness or tiredness, a more serious risk is of stroke. Case reports and studies have suggested an association between chiropractic neck manipulation and cervical artery dissection, leading to stroke. However, a 2016 systematic review with meta-analysis performed on the subject has since concluded that the association of the two events is small and there is no evidence of direct causation <ref>Church E.W, Sieg E.P, Zalatimo O, Hussain N.S, Glantz M, Harbaugh R.E. Systematic review and meta-analysis of chiropractic care and cervical artery dissection: no evidence for causation. Cureus 2016;8 [online] [viewed 17/04/2018] Available from: <nowiki>http://doi.org/10.7759/cureus.498</nowiki></ref>.
| | * [[Alternative Therapies for Pain Conditions]] |
| | * [[Yoga]] |
| | * [[Cognitive Behavioural Therapy]] |
| | * [[Tai Chi and the Older Person|Tai Chi]] |
| | * [[Acupuncture]] |
| | * [[Massage|Massage Therapy]] |
|
| |
|
| All chiropractors in the UK are required by law to be registered with their regulatory body - The [http://www.gcc-uk.org/ General Chiropractic Council]. The council checks that registered chiropractors have current professional indemnity insurance, have met mandatory continuing professional development, and remain in good health and good character. Chiropractic is not widely available in the NHS, but is provided in some areas. Discussion with a patient’s GP can provide this information, or by contacting a [https://www.nhs.uk/service-search/Clinical-Commissioning-Group/LocationSearch/1 local clinical commissioning group].
| | == References == |
| | <references /> |
| | [[Category:Interventions]] |