Nerve Injury Rehabilitation
Original Editor - Your name will be added here if you created the original content for this page.
Lead Editors
Clinically Relevant Anatomy 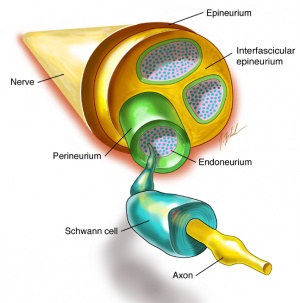 [edit | edit source]
[edit | edit source]
Nerve regrowth in the peripheral nervous system is dependant on type of injury. Functional disability due to nerve lesions is intertwined with severity of lesion. Before reading this article it would be advised to have a good knowledge of the type of lesion and the denervation consequences[1] . Please read Classification of Peripheral Nerve Injury as an introduction to this page.
Mechanism of Injury / Pathological Process[edit | edit source]
Peripheral nerve injuries have numerous causes including: traumatic injuries; infections; metabolic problems ( one of the most common causes is diabetes mellitus); inherited causes; exposure to toxins; tumours; iatrogenic causes.[2]
Watch the below to grasp the concepts of nerve damage and repair
Clinical Presentation[edit | edit source]
Clinical presentation varies according to the nerve affected ie sensory, motor, or combined).
Signs and symptoms may include[2]
- Gradual onset of numbness, prickling or tingling in your feet or hands, which can spread upward into your legs and arms
- Sharp, jabbing, throbbing, freezing or burning pain
- Extreme sensitivity to touch
- Lack of coordination and falling
- Muscle weakness or paralysis if motor nerves are affected
- Neuromatous or causalgia pain.[4]
Assessment[edit | edit source]
After a diagnosis of a peripheral nerve injury a full subjective and objective examination is required to get a clear picture of the way the lesion is affecting the client. The examination should focus on
- Pain assessment
- Sensation deficit and skin condition
- Muscle strength/loss
- Functional deficits
- Balance deficits
- Joint stiffness
- Emotional stress
Outcome Measures[edit | edit source]
Depends on various criteria ( eg upper or lower limb) but could include
Short form McGill pain questionnaire
(see Outcome Measures Database)
Physiotherapy Management / Interventions[edit | edit source]
Management is directed towards
Pain management. Neuropathic pain affects quality of life and is a common consequence of nerve damage. Complete relief is rarely obtained and 40-60 % find means to obtain partial relief. A multidisiplinary approach is taken, with most input from the pharmocologist(s). Anticonvulsants and tri-cyclic anti depressants are the most used drugs for neuropathic pain. Physiotherapist can employ other modalities that show in various studies to be of benefit as a complementary medicine for pain relief[1]. These include
- massage eg aromotherapy massage in studies has shown to help manage neuropathic pain and increase QOL.[5] However many differing massage techniques have been employed showing benefits for pain management and QOL.[6]
- TENS.Application of TENS has been found to be of benefit in pain reduction in neuropathic pain. It was found to be of benefit if used at 100hz in constant mode.[7]
- Relaxation techniques
- Acupuncture
Muscle weakness. A consequence of denervation is muscle atrophy and functional deficits. The healthy neuromuscular junction (NMJ) is critical for nervous control of muscles and to prevent its loss of function TENS has been seen in numerous studies to have a positive effect on nerve regrowth.[1]A 2018 study found the use of TENS was most beneficial if delayed to one week post trauma, the use of 100hz being most beneficial.[8]
Muscle care is of utmost importance to prevent damage to muscle units, in particular prevent: heat or cold trauma; over stretching by gravity or incorrect lifting/transfer techniques; contractures of muscles.
Techniques employed by physiotherapist to achieve the above goals are massage, US, hydrotherapy, splints, passive ROM stretches and correct transfer skill education. When muscle strengthening exercises can commence it is important not to aggravate the regeneration, if pins and needles, numbness or increased pain occurs the exercise is too forceful. Muscle strengthening exercises are employed as appropriate eg isometric, graded weight progression, open close chain. Aerobic activity when possible is also encouraged ( aiming for 30 minutes 4 times a week).
Functional deficits.
Joint Stiffness
Differential Diagnosis[edit | edit source]
Resources[edit | edit source]
add appropriate resources here
References[edit | edit source]
- ↑ 1.0 1.1 1.2 Reza Salman Roghani and Seyed Mansoor Rayegani (2012). Basics of Peripheral Nerve Injury Rehabilitation, Basic Principles of Peripheral Nerve Disorders, Dr. Seyed Mansoor Rayegani (Ed.), ISBN: 978-953-51-0407-0, InTech, Available from: http://www.intechopen.com/books/basic-principles-of-peripheral-nervedisorders/basics-of-peripheral-nerve-injury-rehabilitation (last accessed 24.3.2019)
- ↑ 2.0 2.1 Mayo clinic. Peripheral neuropathy. Available from: https://www.mayoclinic.org/diseases-conditions/peripheral-neuropathy/symptoms-causes/syc-20352061 (last accessed 24.3.2019)
- ↑ Dr. Simon Freilich. Nerve damage and repair. Available from: https://www.youtube.com/watch?v=OlNyp0RfiBg&feature=youtu.be (last accessed 24.3.2019)
- ↑ Medscape. Peripheral nerve injuries clinical presentation. Available from: https://emedicine.medscape.com/article/1270360-clinical (last accessed 24.3.2019)
- ↑ Gok Metin, Zehra & Arikan Dönmez, Ayşe & Izgu, Nur & Ozdemir, Leyla & Emre Arslan, Ismail. (2017). Aromatherapy Massage for Neuropathic Pain and Quality of Life in Diabetic Patients. Journal of nursing scholarship : an official publication of Sigma Theta Tau International Honor Society of Nursing. 49. 10.1111/jnu.12300. (last accessed 25.3.2019)
- ↑ The foundation for peripheral neuropathy. Massage for neuropathy. Available from: https://www.foundationforpn.org/living-well/integrative-therapies/massage/ (last accessed 25.3.2019)
- ↑ Yameen F, Shahbaz NN, Hasan Y, Fauz R, Abdullah M. Efficacy of transcutaneous electrical nerve stimulation and its different modes in patients with trigeminal neuralgia. JPMA-Journal of the Pakistan Medical Association. 2011 May 1;61(5):437. (last accessed 25.3.2019)
- ↑ Su HL, Chiang CY, Lu ZH, Cheng FC, Chen CJ, Sheu ML, Sheehan J, Pan HC. Late administration of high-frequency electrical stimulation increases nerve regeneration without aggravating neuropathic pain in a nerve crush injury. BMC neuroscience. 2018 Dec;19(1):37.(last accessed 25.3.2019)






