Myalgic Encephalomyelitis or Chronic Fatigue Syndrome
Original Editors - Sarah Carlisle & Jill Thompson from Bellarmine University's Pathophysiology of Complex Patient Problems project.
Top Contributors - Sallie Rediske, Patrick Yoder, Sarah Carlisle, Vidya Acharya, Jill Thompson, Niha Mulla, Kim Jackson, Redisha Jakibanjar, Brock Ford, Admin, Tony Lowe, Elaine Lonnemann, WikiSysop, Rucha Gadgil, 127.0.0.1, Rishika Babburu, Wendy Walker and George Prudden
Definition/Description[edit | edit source]
Chronic Fatigue Syndrome (CFS) is a debilitating and complex disorder that is not a single disease but the result of a combination of factors and is a subset of chronic fatigue. This is characterized by intense fatigue that is not improved by bed rest and that may be worsened by physical activity or mental exertion. This unexplained fatigue must last at least 6 consecutive months, must significantly interfere with daily activities/work, and the individual must concurrently demonstrate 4 or more of 8 specific symptoms.[1] There has been some difficulty in exactly defining CFS due to its very nature, and there have been multiple studies attempt to develop and finalize diagnostic criteria for CFS. [2] A Cochrane Review done in 2016 described CFS as an illness characterized by persistent, medically unexplained fatigue [with] symptoms that include severe, disabling fatigue, as well as musculoskeletal pain, sleep disturbance, headaches, and impaired concentration and short-term memory.[1][4]
CFS over the years has been known by various names such as chronic fatigue and immune dysfunction syndrome, chronic Epstein-Barr virus, myalgic encephalomyelitis, neuromyasthenia, as well as the, “yuppie flu”.[1]
CFS is characterized with overlapping symptoms (about 70%) with Fibromyalgia that have some biologic denominator.[3]
Prevalence[edit | edit source]
Reported prevalence is dependent on which definition/diagnostic criteria used, the type of population that was surveyed, and the study methods of the research being referenced. The Cochrane Review of 2016 reported estimates that between 2 in 1000 and 2 in 100 adults in the USA are affected by CFS.[4] Whereas other Goodman et all report studies finding prevalence among adults to be between 0.23% and 0.42% with higher incidence in women, minority groups, and people with lower educational attainment and occupational status.
1. More common in women [1]
2. Members of minority groups [1]
3. Lower educational attainment and occupational status [1]
4. Age range 29-35 years although all age groups can be affected [1]
5. Illness duration ranges from 3-9 years. [1]
6. Children developed CFS typically in the teen years although it was much less common [1]
7. Research conducted by the CDC suggest that less than 20% of people with CFS have been diagnosed in the US. [1]
Characteristics/Clinical Presentation[edit | edit source]
Common reported symptoms:
• Fatigue [2] prolonged (lasting more than 6 months), overwhelming fatigue commonly exacerbated by minimal physical activity. [1]
• Exertional Malaise [2]
• Sleep Disturbance [2]
• Cognitive Impairment
• Decreased Concentration
• Impaired short term memory [2]
• Myalgia [2]
• Frequent or recurring sore throat [1][5]
• Fever (common at onset) [1]
• Muscle Pain [1][5] (common at onset)
• Muscle Weakness (common at onset)
• Multiple Joint Pain [5] without swelling or redness [1]
• Neurally mediated hypotension (NMH) (May experience lightheadedness, lower blood pressure and pulse, visual dimming, slow response to verbal stimuli) [1]
• Tender lymph nodes in neck or armpit [1][5]
Prognosis
• CFS will vary from person to person but will often follow a course, alternating between periods of illness and relative well-being. Some people may experience partial or complete remission of symptoms; however, they often reoccur. [1]
• Recovery rates can be unclear, depending on the study, improvement rates vary from 8% to 63% with a median of 40% of people improving during follow up. [1]
• Full recovery may be rare, with an average of only 5-10% sustaining total remission. [1]
Associated Co-morbidities[edit | edit source]
• Neurally mediated hypotension (NMH) is a common finding in individuals with CFS. Individuals with NMH have a low blood pressure and heart rate; thus, they can experience syncope, visual dimming, or a slow response to verbal stimuli. [1]
• Anxiety [6][7]
• Depression [6][7][8] Connection between immuno-inflammatory and TRYCAT pathways and physio-somatic symptoms. [7]
• Fibromyalgia [1][7][9]
• Irritable Bowel Syndrome [7][8]
• Myofascial pain syndrome [7]
• Temporomandibular joint syndrome [7]
• Interstitial cystitis [7]
• Raynaud's phenomenon [7]
• Prolapsed mitral valve [7]
• Migraine [7]
• Allergies [7]
• Multiple chemical sensitivities [7]
• Sicca syndrome [7]
• Obstructive or central sleep apnea [7]
Medications[edit | edit source]
While studies have investigated the use of various medications, none have been found to have consistent results. However, the following drugs are used to address and manage symptoms[1]:
- Medications to reduce pain, discomfort, and fever
- Medications to treat anxiety
- Medications to treat sleep disturbance (amitryptyline, nefazodone[2])
- Modafinil[3]
- Medications to treat joint pain (amytryptyline[2])
- Medications to treat depression (sertralin, paroxetine, nefazodone[2])
- Anti-inflammatory drugs (aspirin, acetaminophen[2])
- NSAIDS to address headache relief[2]
- Deydroepiandrosterone (DHEA) was found in a pilot study to significantly reduce the pain, helplessness, anxiety, thinking, memory, and activities of daily living difficulties associated with CFS; however, further research is necessary[2].
- Based on current evidence corticosteroids cannot be recommended for CFS due to complications of long-term use, Mineralcorticoids and Intravenous Immunoglobulin are not recommended either and need further research[2][4]
Diagnostic Tests/Lab Tests/Lab Values[edit | edit source]
No specific tests that identify CFS have been found. One study reports that patients with CFS have demonstrated abnormal white blood cell count and brain MRI results.[1] Goodman suggests that physicians rule out other diagnoses (from list below: Differential Diagnosis) and make use of the CDC’s criteria to determine if an individual has CFS.[5] The CDC’s criteria are:[5][6]
1. Clinically evaluated, unexplained persistent or relapsing chronic fatigue that is any of the following:
a. New or definite onset
b. Not the result of ongoing exertion
c. Not substantially alleviated by rest
d. Results in substantial reduction in previous levels of occupational, educational, social, or personal activities
2. The concurrent occurrence of 4 or more of the following symptoms:
a. Substantial impairment in short-term memory or concentration
b. Sore throat
c. Tender lymph nodes
d. Muscle pain
e. Multiple arthralgias (joint pain) without swelling or redness
f. Headaches of a new type, pattern, or severity
g. Unrefreshing sleep
h. Postexertional malaise lasting more than 24 hours
The symptoms must have persisted or recurred during 6 or more consecutive months of illness and must not have predated the fatigue.[5]
Sixteen gene abnormalities have been found in individuals with CFS, some related to immunity and defense; however, further research is needed to determine just how gene expression might effect those with CFS.[6]
Etiology/Causes[edit | edit source]
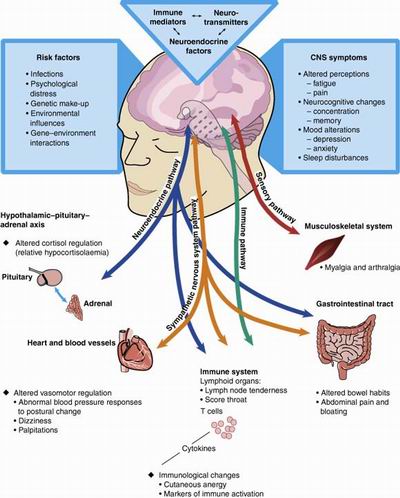
- The etiology and pathophysiology remain unknown.[6][7][8] Earlier theories focused on the prominence of symptoms that suggested an acute viral illness or a psychiatric disorder. Other theories have documented abnormalities including brain structure and function, neuroendocrine responses, sleep architecture, immune function, virological studies, exercise capacity, and psychological profiles.[8]
- CFS involves complex interactions between regulating systems and seem to involve the CNS, the immune system, and the hormonal regulation system. The etiology and pathogenesis is believed to be multi-factorial.[5][8]
- Recent infection (cold, flulike illness)[5]
- High rates after Q fever and Lyme disease[5]
Personality changes[5]
- Personality characteristics of neuroticism (instability, anxiety, aggression)
- Introvert
Lifestyle changes[5]
- Inactivity in childhood and inactivity after infectious mononucleosis
- Acute physical or psychologic stress (trigger)
- Serious life events (loss of a loved one or a job)
- Studies suggest that physiological and psychological factors work together to predispose an individual to the illness and to precipitate and perpetuate the illness.[8]
Systemic Involvement[edit | edit source]
Neurological
- Symptoms reported by chronic fatigue syndrome patients-including fatigue; impaired concentration, attention, memory; and headache.[8]
- Decline in grey matter volume due to decrease in physical activitiy.[2]
- Lesions in the white matter in CFS seen with or without depression.[2]
- Decrease upregulated serotonin receptors most marked in the hippocampus bilaterally.[2]
Endocrine
- Research suggests abnormalities in the hypothalamic-pituitary-adrenal (HPA) axis and serotonin pathways, suggesting an altered physiological response to stress.[8]
- Abnormal cortisol secretion which correlates with health and physical function. [2]
- Reduced adrenal gland size by over 50%, significant of adrenal gland atrophy.[2]
Immune System
- Increase in the number of B cells expressing CD20 and CD21 markers. [2]
- Deficiency in cellular immunity in patients with CFS. The Transforming Growth Factor Beta 1 (TGF-B1) appears to be reduced. This growth factor is an anti-inflammatory cytokine and a reduction in the transcription of this protein may increase the likelihood of inflammation. [2]
http://www.medicalook.com/Nutritional_supplement/Chronic_Fatigue_Syndrome.html
Medical Management (current best evidence)[edit | edit source]
There is no known cure for CFS, therefore focus is aimed at symptom relief and improved function. A combination of drug and nondrug therapies is recommended. However, no single therapy has proven to help all individuals with CFS.[5]
Focus on lifestyle changes:[5]
- Prevention of overexertion
- Reduced Stress
- Dietary restrictions
- Gentle Stretching
- Nutritional supplementation
Drug Therapy to address:[5]
- Sleep disturbances
- Pain
Systematic Reviews have shown effectiveness and benefits with cognitive behavior therapy and graded exercise therapy.[5]
Physical Therapy Management (current best evidence)[edit | edit source]
Physical therapy begins by assessing the patient’s current health status to see if signs of deconditioning exist. If so, Goodman suggests starting with a strengthening program and then progressing to activities that test the cardiovascular system.[5] Physical therapy management of CFS is focused on progressing from minimal activity to 30 minutes of continuous exercise during periods of remission,[5] always focusing on gentle, graded, flexible exercise that is monitored continuously.[6] Goodman suggests monitoring vital signs and assessing fatigue levels using a 5-point scale during exercise and activities.[5] Education about the syndrome, the importance of exercise, and how to pace oneself in everyday activities to avoid fatigue and relapse is a key component in the management of CFS.[5] One study states that due to the necessary and unique components of helping individuals manage chronic fatigue, physical therapists need to be trained on how to both deliver pain management and exercise programs to these individuals.[6]
Graded exercise therapy (GET) has been shown to be a more effective treatment option than stretching and relaxation exercises for individuals with CFS, while all the above options are important aspects of care for the individual.[5] GET results are still variable (see chart below[6]) and will benefit from further research to determine effects on individuals with CFS.[6]
A 2011 study assessed the effectiveness of receiving specialist medical care (SMC) only or with adaptive pacing therapy (APT), cognitive behavior therapy (CBT), or graded exercises therapy (GET).[9] Fatigue levels were decreased and physical function improved in the randomized groups who received CBT or GET in combination with SMC.[9] These 2 groups demonstrated greater improvements in the outcomes used than the other interventions studied.[9]
Psychological Management (current best evidence)[edit | edit source]
Cognitive Behavior Therapy (CBT) has been used to manage CFS, especially in reducing fatigue and decreasing pain.[2][8][6][10] CBT is one of the few nonpharmacological management techniques recommended for individuals with CFS;[6] however, it, too, has had mixed results in individuals with CFS. If an individual is experiencing high levels of pain, Marshall suggests other treatment strategies be used in combination because CBT is aimed more specifically at managing fatigue levels.[6] CBT is an individualized, proactive approach on the patient’s part, involving self-reflection and monitoring in the hopes of discovering what kinds of behaviors or thoughts are causing the CFS symptoms.[2][10] CBT also involves learning coping strategies and initiating a daily schedule of rest and activity in order to address fatigue levels and optimize function.[2]
Roberts found that individuals with hypocortisolism and CFS do not respond as well as others after 12-15 sessions of CBT.[10] The study questions if these individuals require a longer duration of CBT, a modified version, or a combination of therapies including hydrocortisone replacement therapy.[10] Further studies are necessary in order to address these questions.
Self Management[edit | edit source]
Marshall[6] stated that in their study, individuals with CFS reported trying to self-manage their symptoms in addition to physical therapy or alternative techniques. Self-pacing, stretches, breathing exercises, and yoga were among the kinds of activities reported; with stretches and breathing exercises managing pain levels the best (see chart below).[6]
Differential Diagnosis[edit | edit source]
The following are possible differential diagnoses:[5]
- Fibromyalgia
Patients usually demonstrate with increased pain, while patients with CFS experience greater fatigue. Some consider CFS and fibromyalgia to be one in the same; others believe CFS is an early form of fibromyalgia.
- Mononucleosis
- Lyme Disease
- Thyroid conditions
- Diabetes
- MS
- Various Cancers
- Depression
- Bipolar disorder
- Myalgic encephalomyelitis[9]
Case Reports/ Case Studies
[edit | edit source]
Chronic Fatigue Syndrome Case Report: www.ncbi.nlm.nih.gov/pmc/articles/PMC3028106/[11].
Chronic Fatigue and Recovery:
Interview of an Individual with Chronic Fatigue:
Lewis, C. Personal communication. April 12, 2012.
Resources
[edit | edit source]
Support Group & CFS Information: www.chronicfatiguesyndrome.me.uk/[13]
Recent Related Research (from Pubmed)[edit | edit source]
see tutorial on Adding PubMed Feed
References[edit | edit source]
see adding references tutorial.
- ↑ 1.0 1.1 Teitel AD MD MBA, Zieve D MD MHA. Chronic fatigue syndrome. PubMed Health: A.D.A.M. Medical Encyclopedia. 2012. Available from: PubMed.
- ↑ 2.00 2.01 2.02 2.03 2.04 2.05 2.06 2.07 2.08 2.09 2.10 2.11 2.12 2.13 2.14 2.15 2.16 Gur, A., Oktayoglu, P. Central nervous system abnormalities in fibromyalgia and chronic fatigue syndrome: new concepts in treatment. Current Pharmaceutical Design. 2008: 14;1274-1294. Available from: PubMed.
- ↑ MacAllister WS PhD, Krupp LB MD. Multiple sclerosis—related fatigue. Phys Med and Rehabilitation Clinics of North America. 2005:16;483-502.
- ↑ Vinjamury, S.P. MD, Singh, B.S. PhD. Ayurvedic Treatment of chronic fatigue syndrome-a case report. Alternative Therapies in Health and Medicine. Sept/Oct 2005: 11(5);76-78. Available from: PubMed.
- ↑ 5.00 5.01 5.02 5.03 5.04 5.05 5.06 5.07 5.08 5.09 5.10 5.11 5.12 5.13 5.14 5.15 5.16 5.17 Goodman CC., Fuller KS. Pathology: implications for the physical therapist. 3rd ed. St. Louis: Saunders; 2009.
- ↑ 6.00 6.01 6.02 6.03 6.04 6.05 6.06 6.07 6.08 6.09 6.10 6.11 Marshall, R BSc (HONS), Paul, L PhD, Wood, L PhD. The search for pain relief in people with chronic fatigue syndrome: a descriptive study. Physiotherapy Theory and Practice. 2011:27(5);373-383. Available from: PubMed.
- ↑ Reeves W, et al. Indentification of ambiguities in the 1994 chronic fatigue syndrome research case definition and recommendations for resolution. BMC Health Services Research. 2003:3(25). Available from: BioMed Central.
- ↑ 8.0 8.1 8.2 8.3 8.4 8.5 8.6 Afari, N PhD, Buchwald, D MD. Chronic fatigue syndrome: a review. The American Journal of Psychiatry. 2003:160(2);221-236. Available from: PubMed.
- ↑ 9.0 9.1 9.2 9.3 White PD, Goldsmith KA, Johnson AL, et al. Comparison of adaptive pacing therapy, cognitive behaviour therapy, graded exercise therapy, and specialist medical care for chronic fatigue syndrome (PACE): a randomized trial. Lancet. 2011;377:823-836.
- ↑ 10.0 10.1 10.2 10.3 Roberts, A.D.L., Charler, M.L., Papadopoulos, A., Wessely, S., Chalder, T. Cleare, A.J. Does hypocortisolism predict a poor response to cognitive behavioural therapy in chronic fatigue syndrome? Psychological Medicine. 2010: 40;515–522. Available from: ProQuest.
- ↑ Geller RD, Giclas PC. Chronic fatigue syndrome and complement activation. BMJ Case Reports. 2009. Available from: PubMed Central.
- ↑ <ref>LatestNutrition. How to spot symptoms of chronic fatigue syndrome [NBC: 6-20-2011]. Available from: http://www.youtube.com/watch?v=tp2OA0kSosQ [last accessed 4/3/12]</ref>
- ↑ Sheppard, L. Chronic fatigue syndrome: an invisible illness. [place unknown]:Sheppard, L; updated 2010. Available from: http://www.chronicfatiguesyndrome.me.uk/.