Lateral Epicondylitis: Difference between revisions
No edit summary |
No edit summary |
||
| (167 intermediate revisions by 22 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox"> | <div class="editorbox"> | ||
''' | '''Original Editors ''' - [[User:Hannah Norton|Hannah Norton]] | ||
''' | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | ||
</div> | </div> | ||
== | == Description == | ||
[[File:Tennis.png|right|frameless|267x267px]] | |||
Lateral epicondylitis, also commonly referred to as [[Tennis Elbow Management|tennis elbow]], describes an overuse injury that occurs secondary to an eccentric overload of the common extensor tendon at the origin of the extensor carpi radialis brevis (ECRB) tendon. <ref>Buchanan BK, Varacallo M. Tennis Elbow (Lateral Epicondylitis) [Internet]. Nih.gov. StatPearls Publishing; 2019. Available from: https://www.ncbi.nlm.nih.gov/books/NBK431092/ | |||
</ref>These muscles originate on the lateral epicondylar region of the distal [[humerus]]. In many cases, the insertion of the extensor carpi radialis brevis is involved. | |||
<ref> | It should be remembered that only 5% of people suffering from tennis elbow relate the injury to tennis! Contractile overloads that chronically stress the [[Tendon Anatomy|tendon]] near the attachment on the [[humerus]] are the primary cause of LET. It occurs often in repetitive upper extremity activities such as computer use, heavy lifting, forceful forearm pronation and supination, and repetitive vibration. Despite the name, you will also commonly see this chronic condition in other sports such as squash, badminton, baseball, swimming and field throwing events. People with repetitive one-sided movements in their jobs such as electricians, carpenters, gardeners, desk bound jobs also commonly present with this condition.<ref name=":7">Alexander J, et al. [https://www.ajronline.org/doi/10.2214/ajr.181.1.1810219 Sonography and MR Imaging of Posterior Interosseous Nerve Syndrome with Surgical Correlation.] AJR Am J Roentgenology 2003; 181(1): 219-221</ref><ref name=":4">Walz D, et al. [https://pubs.rsna.org/doi/10.1148/rg.301095078?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%20%200pubmed Epicondylitis: Pathogenesis, Imaging, and Treatment]. RadioGraphics. 2010; 30(1): 167 - 184</ref> <ref name=":2">Pienimäki T, et al. [https://journals.lww.com/clinicalpain/Abstract/2002/05000/Associations_Between_Pain,_Grip_Strength,_and.5.aspx Associations Between Pain, Grip Strength, and Manual Tests in the Treatment Evaluation of Chronic Tennis Elbow] . Clin J Pain 2002; 18(3):164-170 </ref><ref name=":3">Whaley A, Baker C. [https://pubmed.ncbi.nlm.nih.gov/15474229/ Lateral epicondylitis.] Clin Sports Med 2004;23(4):677– 691</ref><ref name=":11">Page P. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2971639/pdf/najspt-05-189.pdf A new exercise for tennis elbow that works!] N Am J Sports Phys Ther 2010; 5(3): 189–193</ref> | ||
== Clinically Relevant Anatomy == | == Clinically Relevant Anatomy == | ||
[[File:Bonyanat.jpg|thumb|231x231px|Bony Anatomy of the elbow]] | |||
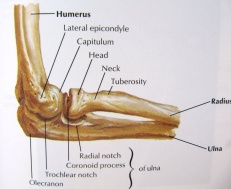
The elbow joint is made up of three bones: the humerus (upper arm bone), the radius and ulna (two bones in the forearm). At the distal end of the humerus there are two epicondyles, one lateral (on the outside) and one medial (on the inside). | The [[Elbow|elbow joint]] is made up of three bones: the [[humerus]] (upper arm bone), the [[radius]] and [[ulna]] (two bones in the forearm). At the distal end of the humerus there are two epicondyles, one lateral (on the outside) and one medial (on the inside). | ||
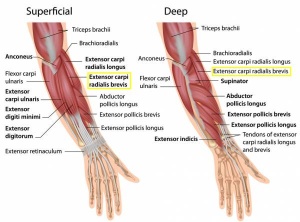
The area of maximal tenderness is usually an area just distal to the origin of the extensor muscles of the forearm at the lateral epicondyle. Most commonly, the extensor carpi radialis brevis (ECRB) is involved, but others may include the [[Extensor Digitorum Communis|extensor digitorum]], [[extensor carpi radialis longus]] (ECRL), and extensor carpi ulnaris. <ref name=":4" /><ref>Stasinopoulos D, Johnson M. [https://bjsm.bmj.com/content/bjsports/38/6/675.full.pdf Cyriax physiotherapy for tennis elbow/lateral epicondylitis.] Br J Sports Med 2004; 38:675-677 </ref> | |||
The radial nerve is also in close proximity to this region, and divides into the superficial radial nerve and the posterior interosseous nerve. | The [[radial nerve]] is also in close proximity to this region, and divides into the superficial radial nerve and the posterior interosseous nerve. | ||
== Epidemiology / | == Epidemiology/Aetiology == | ||
[[File:Muscle elbow.jpg|thumb|Muscular anatomy of the lateral elbow | |||
]]LET is classified as an overuse injury that may result in hyaline degeneration of the origin of the extensor tendon. Overuse of the muscles and tendons of the forearm and elbow together with repetitive contractions or manual tasks can put too much strain on the elbow tendons. These contractions or manual tasks require manipulation of the hand that causes maladaptations in tendon structure that lead to pain over the lateral epicondyle. Mostly, the pain is located anterior and distal from the lateral epicondyle.<ref name=":2" /> | |||
Elbow tendinopathy occurs at least five times more often and predominantly occurs on the lateral rather than on the medial aspect of the joint, with a 4:1 to 7:1 ratio. It affects 1-3% of the population, with those 35-50 years old most commonly being affected. <ref name=":25">Karanasios S. et al. [https://pubmed.ncbi.nlm.nih.gov/33814224/ Diagnostic accuracy of examination tests for lateral elbow tendinopathy (LET)] - A systematic review. Journal of Hand Therapy 2021; S0894-1130(21)0039-9 </ref> <ref>Vaquero-Picado A, Barco R, Antuña SA. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5367546/ Lateral epicondylitis of the elbow.] EFORT Open Rev. 2017 Mar 13;1(11):391-397. </ref>If a patient is <35 , it is important to consider differential diagnosis (growth plate disorder, referral from the cervical spine). If a patient is >50, consider osteoarthritis ([[Osteoarthritis|OA]]), referred cervical spine pain. In a study by Nirschl, <ref name=":21">Nirschl R. Tennis elbow. Orthop North Am. 1973;4:787-99.</ref> of 200 tennis players aged >30, 50% had symptoms of LET at some stage. | |||
This injury is often work-related, any activity involving wrist extension, pronation or supination during manual labour, housework and hobbies are considered as important causal factors.<ref name=":5">Van Rijn R, et al. [https://pubmed.ncbi.nlm.nih.gov/19224937/ Associations between work-related factors and specific disorders at the elbow: a systematic literature review.] Rheumatology (Oxford) 2009;48(5):528-36. </ref> LET is equally common in both sexes. <ref>Calfee R, et al. [https://pubmed.ncbi.nlm.nih.gov/18180389/ Management of lateral epicondylitis: Current concepts.] J Am Acad Orthop Surg 2008; 16(1):19-29</ref> Between the ages of 30-50 years the disease is most prevalent. <ref name=":25" /> Obtaining the condition at both lateral epicondyles is rare, the dominant arm has the greatest chance of the occurrence of LET. Twenty percent of cases persist for more than a year. <ref name=":4" /> | |||
A systematic review identified 3 risk factors: handling tools heavier than 1 kg, handling loads heavier than 20 kg at least 10 times per day, and repetitive movements for more than 2 hours per day. Other risk factors are overuse, repetitive movements, training errors, misalignments, flexibility problems, ageing, poor circulation, strength deficits or muscle imbalance and psychological factors.<ref>Van Rijn R, et al. [https://pubmed.ncbi.nlm.nih.gov/19224937/ Associations between work-related factors and specific disorders at the elbow: a systematic literature review.] Rheumatology (Oxford) 2009;48(5):528-536</ref> | |||
There are several opinions concerning the cause of LET: | |||
'''1.Inflammation''' | |||
Although the previous term epicondylitis implies the presence of an inflammatory condition, inflammation is present only in the earliest stages of the disease process. <ref name=":10">Baker C, Plancher K. [https://link.springer.com/book/10.1007/b97243 Operative treatment of elbow injuries.] New York: Springer, 2002.</ref> | |||
<u> | <u></u>'''2. Microscopic tearing''' | ||
*Nirschl and Pettrone <ref>Nirschl R, Pettrone F. [https://pubmed.ncbi.nlm.nih.gov/479229/ Tennis elbow. The surgical treatment of lateral epicondylitis.] J Bone Joint Surg Am 1979; 61(6A):832-839</ref> attributed the cause to microscopic tearing with formation of reparative tissue (angiofibroblastic hyperplasia) in the origin of the extensor carpi radialis brevis (ECRB) muscle. This micro-tearing and repair response can lead to macroscopic tearing and structural failure of the origin of the ECRB muscle. | |||
*That microscopic or macroscopic tears of the common extensor origin were involved in the disease process, was postulated by Cyriax in 1936. <ref name=":22">Cyriax J. [https://journals.lww.com/jbjsjournal/abstract/1936/18040/the_pathology_and_treatment_of_tennis_elbow.11.aspx The pathology and treatment of tennis elbow]. J Bone Joint Surg 1936; 18(4): 921–940 | |||
</ref> | |||
*The first to describe macroscopic tearing in association with the histological findings were Coonrad and Hooper. <ref name=":23">Coonrad R, Hooper W. [https://pubmed.ncbi.nlm.nih.gov/4758032/ Tennis elbow: its course, natural history, conservative and surgical management.] J Bone Joint Surg Am 1973; 55(6):1177-1182 </ref> | |||
*Histology of tissue samples shows "collagen disorientation, disorganisation, and fibre separation by increased proteoglycan content, increased cellularity, neovascularisation, with local necrosis." Nirschl <ref name=":21" /> termed these histological findings bangiofibroblastic hyperplasia. The term has since been modified to bangiofibroblastic tendinosis. He noted that the tissue was characterised by disorganized, immature collagen formation with immature fibroblastic and vascular elements. This grey, friable tissue is found in association with varying degrees of tearing involving the extensor carpi radialis brevis. | |||
'''3. Degenerative Process''' | |||
== | The histopathological features of 11 patients who had LET were examined by Regan et al. <ref>Regan W, et al. [https://pubmed.ncbi.nlm.nih.gov/1280910/ Microscopic histopathology of chronic refractory lateral epicondylitis.] Am J Sports Med 1992; 20(6):746-749. </ref> They determined that the cause of LET was more indicative of a degenerative process than an inflammatory process. The condition is degenerative with increased fibroplasts, vascular hyperplasia, proteoglycans and glycosaminoglycans, and disorganized and immature collagen. Repetitive eccentric or concentric overloading of the extensor muscle mass is thought to be the cause of this angiofibroplastic tendinosis of the ECRB. LET is a degenerative condition in which increased fibroplastic activity and granulation tissue formation occur within the tendon. <ref name=":2" /> <ref name=":3" /> | ||
'''4. Hypovascularity''' | |||
Because this tendinous region contains areas that are relatively hypovascular, the tendinous unit is unable to respond adequately to repetitive forces transmitted through the muscle, resulting in declining functional tolerance. <ref>Davenport T, et al. [https://pubmed.ncbi.nlm.nih.gov/16180958/ The EdUReP Model for Nonsurgical Management of Tendinopathy.] Phys Ther 2005;85(10):1093-103</ref> | |||
== | == Clinical Presentation == | ||
< | The most prominent symptom of LET is pain, which can be produced by palpation on the extensor muscles origin on the lateral epicondyle. The pain can radiate upwards along the upper arm and downwards along the outside of the forearm and in rare cases even to the third and fourth fingers. Furthermore, it is also often seen that the flexibility and strength in the wrist extensor and posterior shoulder muscles are deficient. <ref name=":2" /> <ref name=":3" /> | ||
< | According to Warren <ref name=":6">Warren, R. Tennis elbow (epicondylitis): epidemiology and conservative treatment. Pettrone F. AAOS Symposium and Upper Extremity Injuries in Athletes, Ed. St. Louis: C.V. Mosby, 1986; 233-243. | ||
</ref>, there are four stages on the development of this injury with regard to the intensity of the symptoms.<br>1. Faint pain a couple of hours after the provoking activity.<br>2. Pain at the end of or immediately after the provoking activity.<br>3. Pain during the provoking activity, which intensifies after ceasing that activity.<br>4. Constant pain, which prohibits any activity. | |||
< | Furthermore, it is often seen that the flexibility and strength in the wrist extensor and posterior shoulder muscles are deficient. At least patients report weakness in their grip strength or difficulty carrying objects in their hand, especially with the elbow extended. This weakness is due to finger extensor and supinator weakness. Some people have a sense of paralysis but this is rare. <ref name=":5" /><ref name=":6" /> <ref>Birrer R. Sport Medicine for the Primary Care Physician, CRC Press, 2002. </ref> | ||
< | Symptoms last, on average, from 2 weeks to 2 years. 89% of the patients recover within 1 year without any treatment except perhaps avoidance of the painful movements (sport injuries) <ref name=":22" /><ref>Wright J. Evidence-based orthopaedics: the best answers to clinical questions. Philadelphia: Saunders Elsevier, 2008.</ref> <ref name=":27">Smidt N, et al. [https://pubmed.ncbi.nlm.nih.gov/11879861/ Corticosteroid injections, physiotherapy, or a wait-and-see policy for lateral epicondylitis: a randomised controlled trial.] Lancet 2002; 359: 657–62</ref> | ||
=== Assessment Findings === | |||
A thorough assessment and examination are key elements in ensuring that the correct treatment plan is implemented, enhancing the recovery process. The assessment should also include elements to exclude a differential diagnosis. | |||
< | Possible subjective assessment findings may include: | ||
* Onset of pain 24-72 hours after provocative activity involving wrist extension | |||
* Pain may radiate down forearm as far as the wrist and hand | |||
* Difficulty with lift and grip (pain+/- weakness) | |||
* Changes in biomechanical factors e.g. new tennis racquet, wet ball, over training, poor technique, shoulder injury<ref name=":0">Nirschl R, Ashman E. [https://pubmed.ncbi.nlm.nih.gov/14560549/ Elbow tendinopathy: tennis elbow.] Clin Sports Med 2003;22(4):813-836.</ref><ref name=":1">Brukner P. Brukner & Khan's clinical sports medicine. North Ryde: McGraw-Hill; 2012.</ref> | |||
< | In the objective assessment, one may find: | ||
* Pain and point tenderness over lateral epicondyle and/or 1-2 cm distal to epicondyle | |||
* Pain and weakness on resisted wrist extension | |||
* Weakness on grip strength testing (Dynamo-meter) | |||
* Pain and/or decreased movement on passive elbow extension, wrist flexion and ulnar deviation and pronation | |||
* Weak elbow extensors and flexors<ref name=":0" /><ref name=":1" /> | |||
== Diagnostic Procedures == | |||
The diagnosis starts with history taking and questions about the activity level, occupational risk factors, recreational sports participation, medication and other medical problems. It’s important to know which activities cause symptoms and where on your arm the symptoms occur.<ref name=":7" /> | |||
During the physical exam, the structure of the elbow and other joints is assessed. Also the nerves, muscles, bones and skin are examined. The diagnosis of LET is substantiated by tenderness over the ECRB or common extensor origin. By the following methods, the therapist or physiotherapist should be able to reproduce the typical pain: | |||
* | *To examine the severity of the tennis elbow, there is a dynamometer and a Patient-rated Tennis Elbow Evaluation Questionnaire (PrTEEQ).<ref>Rompe J, et al. [https://pubmed.ncbi.nlm.nih.gov/17254903/ Validation of the Patient-rated Tennis Elbow Evaluation Questionnaire.] J Hand Ther. 2007;20(1):3-10. </ref> <ref>MacDermid J. [https://www.researchgate.net/publication/228501961_The_Patient-Rated_Tennis_Elbow_Evaluation_PRTEEC_User_Manual The Patient-Rated Tennis Elbow Evaluation (PRTEE)©] User Manual, 2007 </ref> The dynamometer measures grip strength. <ref>Mathiowetz V. [https://pubmed.ncbi.nlm.nih.gov/12374997/ Comparison of Rolyan and Jamar dynamometers for measuring grip strength.] Occup Ther Int. 2002;9(3):201-209.</ref> The PrTEEQ is a 15-item questionnaire, designed to measure forearm pain and disability in patients with lateral epicondylitis. The patients have to rate their levels of tennis elbow pain and disability from 0 to 10, and consists of 2 subscales. There is a pain subscale (0 = no pain, 10 = worst imaginable) and a function subscale (0 = no difficulty, 10 = unable to do). | ||
* | *[http://www.physio-pedia.com/Cozen%E2%80%99s_Test Cozen’s test:] Cozen’s test is also known as the resisted wrist extension test. The elbow is stabilised in 90° flexion. The therapist palpates the lateral epicondyle and the other hand of the therapist positions the patient’s hand into radial deviation and forearm pronation. Then the patient is asked to resist wrist extension. The test is positive if the patient experiences a sharp, sudden, severe pain over the lateral epicondyle.<ref>Cooper G. [https://link.springer.com/book/10.1007/978-1-59745-009-6 Pocket guide to musculoskeletal diagnosis.] New Jersey: Humana Press, 2006 | ||
</ref> <ref>Bhargava A, et al. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2944326/ Grip strength measurements at two different wrist extension positions in chronic lateral epicondylitis-comparison of involved vs. uninvolved side in athletes and non athletes: a case-control study.] Sports Med Arthrosc Rehabil Ther Technol. 2010;2:22. </ref>[<ref name=":8">Frydrychowicz A, et al. [https://pubmed.ncbi.nlm.nih.gov/22334493/ Hepatobiliary MR imaging with gadolinium-based contrast agents.] J Magn Reson Imaging 2012; 35 (3): 492–511</ref> High sensitivity <ref name=":25" /> <ref name=":24">Saroja G. et al. [https://www.ijmhr.org/ijpr.2.6/IJPR.2014.699.pdf Diagnostic accuracy of provocative test in lateral epicondylitis.] Int J Physiother Res 2014; 2(6):815-823.</ref> has been found with positive findings suggesting the presence of LET but poor specificity to exclude other differential diagnoses. | |||
* | *Chair test: The patient grasps the back of the chair while standing behind it and attempts to lift the chair by using a three finger pinch (thumb, index long fingers) and the elbow fully extended. The test is positive when pain occurs at the lateral epicondyle. <ref name=":8" /> | ||
* | *[http://www.physio-pedia.com/Mill%E2%80%99s_Test Mill's Test]: The patient is seated with the upper extremity relaxed at the side and the elbow extended. The examiner passively stretches the wrist in flexion and pronation. Pain at the lateral epicondyle or proximal musculotendinous junction of the wrist extensors is a positive sign for LET. <ref name=":2" /><ref name=":8" /><ref name=":9">Valdes K, LaStayo P. T[https://pubmed.ncbi.nlm.nih.gov/23062797/ he value of provocative tests for the wrist and elbow: a literature review.] J Hand Therapy, 2013; 26: 32-43</ref> | ||
* | *[http://www.physio-pedia.com/Maudsley's_test Maudsley’s test]: The examiner resists extension of the third digit of the hand, while palpating the lateral epicondyle. A positive test is indicated by pain over the lateral epicondyle.<ref name=":2" /><ref name=":9" />An 88% sensitivity has been found for including the LET diagnosis but not excluding it with confidence. <ref name=":24" /> | ||
* | *The coffee cup test <ref name=":23" />: The test is performed while doing a specific activity such as picking up a full cup of coffee or a milk bottle. The patient is asked to rate their pain on a scale of zero to ten.<ref name=":2" /><ref name=":9" /> | ||
A differential diagnosis should also be considered. | |||
=== Differential diagnosis === | |||
#''Radial Tunnel Syndrome'' <ref>Roles N, Maudsley R. [https://pubmed.ncbi.nlm.nih.gov/4340924/ Radial tunnel syndrome: Resistant tennis elbow as nerve entrapment.] J Bone Joint Surg Br 1972; 54:499-508</ref> | |||
#*Pain in the posterolateral area of the forearm | |||
#*Pain sometimes spreads to the dorsal side of the wrist | |||
#*Parasthesia | |||
#*Weakness (overuse injuries of the musculoskeletal system) | |||
#''[https://physio-pedia.com/Posterior_interosseous_nerve_syndrome Posterior interosseus nerve syndrome]'' <ref>Portilla M, et al. [https://pubmed.ncbi.nlm.nih.gov/9651775/ The posterior interosseous nerve and the radial tunnel syndrome: an antatomical study.] Int Orthop 1998; 22(2):102-106. | |||
</ref> <ref>Chien A, et al. [https://pubmed.ncbi.nlm.nih.gov/12818863/ Sonography and MR Imaging of Posterior Interosseous Nerve Syndrome with Surgical Correlation.] Am J Roentgenol 2003; 181: 219-221. </ref><ref>Bionka M, et al. Interventions for treating the posterior interosseus nerve syndrome: a systematic review of observational studies. J Peripher Nerv Syst 2006; 11(2):101-110</ref> | |||
#*Pain | |||
#*Weakness involving wrist extension and finger extension | |||
#*Motor deficits | |||
#''[[Elbow osteoarthritis]]'' | |||
#*Pain | |||
#*Loss of range of motion | |||
#[[Fracture|Fractures]] | |||
#*Distal Radial Fracture | |||
#*Radial Head Fracture | |||
#*Olecranon Fracture | |||
#''[[Cervical Radiculopathy]]'' | |||
#*Radiating arm pain corresponding to the [[dermatomes]] | |||
#*Neck pain | |||
#*Parasthesia | |||
#*Muscle weakness in myotome | |||
#*Reflex impairment/loss | |||
#*[[Headache]] | |||
#*Scapular pain | |||
#*Sensory and motor dysfunction in upper extremities and neck | |||
#Cervical Disc Disease | |||
#Cervical Myofascial Pain | |||
#[[Cervical Spondylosis]] | |||
#[[Fibromyalgia]] | |||
#[[Medial Epicondylitis]] | |||
== | === '''Further Diagnostic Investigations''' === | ||
Investigations are usually not performed in the straightforward case of lateral elbow pain. | |||
'''Ultrasound examination''' may be used in the investigation of patients with lateral elbow pain to demonstrate the degree of tendon damage as well as the presence of a bursa. <ref name=":1" /> | |||
In longstanding cases, '''plain X-ray''' (AP and lateral views) of the elbow may be taken to rule out arthritis of the elbow. Calcification along the lateral epicondyle <ref name=":1" />, osteochondritis dissecans, degenerative joint changes or evidence of heterotopic calcification are among the common findings. | |||
'''Electromyography (EMG)''' may be used to rule out nerve compression. Many nerves travel around the elbow, and the symptoms of nerve compression are similar to those of tennis elbow. | |||
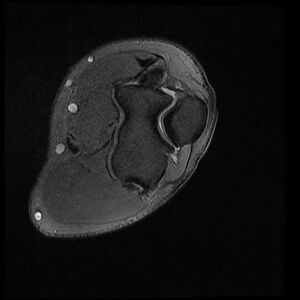
[[File:Axial PD fat sat.jpg|thumb|300x300px|MRI findings: <ref>Rasuli, B. Lateral epicondylitis - tennis elbow. Case study, Radiopedia.org (accessed on 13 April 2022) https://doi.org/10.53347/rlD-98132</ref>Partial-thickness tear of the common extensor tendons with a small fluid-filled gap - Axial PD fat sat]] | |||
If there is suspicion that the symptoms are neck-related, a '''Magnetic Resonance Imaging (MRI)''' scan may be ordered. | |||
This might show if there is a possible herniated disk or arthritis in the area of the neck. Both of these conditions often produce arm pain. | |||
An MRI may also show thickening, hypoechogenicity or defects in the tendo-osseous enthesis in the case of LET, <ref name=":1" />but the presence of these findings should be interpreted with caution when directing clinical decisions. <ref name=":25" /> <ref>Johns N, Shridhar V. [https://pubmed.ncbi.nlm.nih.gov/33123709/ Lateral epicondylitis: Current concepts.] AJGP 2020; 49(11):707-709.</ref> | |||
== Outcome Measures == | |||
The use of outcome measures in LET elbow clinical practice and research is not widely established. <ref>Evans J, et al. [https://pubmed.ncbi.nlm.nih.gov/29444754/ Clinical rating systems in elbow research - a systematic review exploring trends and distributions of use.] J Shoulder Elbow Surg 2018;27:e98-106</ref> <ref name=":26">Samaras P, et al. [https://www.sciencedirect.com/science/article/abs/pii/S2468781222000017 Greek physiotherapists' contemporary knowledge and practice for lateral elbow tendinopathy: an online survey.] Musculoskeletal Science and Practice 2022; 57:102502</ref> However, some commonly used scales are the following: | |||
*Pain reported outcome measures; | |||
**[[Numeric Pain Rating Scale]] (NPRS) | |||
**[[Visual Analogue Scale]] (VAS) | |||
*Self-reported Questionnaires; | |||
** The Upper Limb Functional Index (ULFI): | |||
** Patient Rated Tennis Elbow Evaluation (PRTEE): | |||
**[[DASH Outcome Measure|QuickDASH]] (Disabilities of the Arm Shoulder and Hand): | |||
**[[Patient Specific Functional Scale]] (PSFS) - although the PSFS has not yet been validated for LET, it has been shown to be valid, reliable and responsive to change in other conditions such as knee dysfunction, cervical radiculopathy, acute low back pain, mechanical low back pain, and neck dysfunction (Pain ICC = 0.89-0.99, Function ICC = 0.83-0.99, Total ICC = 0.89-0.99)<ref>Leung H, Yen C, Tse P. [https://pubmed.ncbi.nlm.nih.gov/15181221/ Reliability of Hong Kong Chinese version of the Patient rated Forearm Evaluation Questionnaire for lateral epicondylitis.] Hong Kong Med J 2004;10:172-177.</ref><ref>Newcomer K, et al. [https://pubmed.ncbi.nlm.nih.gov/16271686/ Sensitivity of the Patient-rated Forearm Evaluation Questionnaire in lateral epicondylitis.] J Hand Ther 2005;18:400-406</ref><ref>Overend T, et al. [https://pubmed.ncbi.nlm.nih.gov/10192633/ Reliability of a patient-rated forearm evaluation questionnaire for patients with lateral epicondylitis.] J Hand Ther 1999;12:31-37</ref> | |||
Recently, an international group of experts in the field of tendinopathy published a consensus paper proposing nine health-related core domains against which clinicians and researchers measure outcomes, <ref>Vicenzino B, et al. [https://www.geldersevallei.nl/wcm/connect/www/0b88b3dc-c4e4-49a3-95f8-e3aee535b26a/bjsports-2019-101214.full-editorial.pdf?MOD=AJPERES Icon 2019-International scientific tendinopathy symposium consensus:there are nine core health-related domains for tendinopathy (core domains):Delphi study of healthcare professionals and patients]. Br J Sports Med 2019;54(8):444-451 </ref>: | |||
* Patient rating of condition | |||
* Participation in life activities | |||
* Pain on activity/loading | |||
* Function | |||
* Psychological factors | |||
* Physical function capacity | |||
* Disability | |||
* Quality of life | |||
* Pain over a specified time | |||
Attempts are under way to develop a core outcome set for LET (COS-LET). <ref>Bateman M, et al. [https://bjsm.bmj.com/content/early/2022/02/07/bjsports-2021-105044 Development of a core outcome set for lateral elbow tendinopathy (COS-LET) using best available evidence and an international consensus process.] Br J Sports Med 2022;0:1-10</ref> | |||
== Medical Management == | |||
== Medical | === Non-Operative Medical Treatment === | ||
Non-operative medical treatment of LET is the first-line management of LET. It is initially based on the following principles: relieving pain and controlling inflammation. This may include: | |||
== | * '''Advice''' for relieving pain commonly includes rest and activity modification. | ||
* '''NSAIDs''' may be used in the acute cases for controlling the inflammation and relieving pain in the short-term. <ref>Pattanittum P, et al. [https://pubmed.ncbi.nlm.nih.gov/23728646/ Non-steroidal anti-inflammatory drugs for (NSAIDs) for treating lateral elbow pain in adults.] Cochrane Database Syst Rev 2013; 2013 (5): CD003686</ref> The use of ice three times per day for 15 minutes is also recommended for reducing the inflammatory response and swelling by decreasing the level of chemical activity and by vasocoinstriction. Elevation of the extremity is also indicated if an oedema of the wrist or fingers is present.<ref name=":3" /> | |||
* '''An elbow counterforce brace''' may also be effective in reducing the LET pain during contraction. <ref>Heales L, et al. [https://pubmed.ncbi.nlm.nih.gov/32452393/ Evaluating the immediate effect of forearm and wrist orthoses on pain and function in individuals with lateral elbow tendinopathy: a systematic review.] Musculoskeletal Science and Practice 2020; 47:102-147</ref> As a forearm orthosis, it may play a role of a secondary muscle attachment site and relieve tension on the insertion at the lateral epicondyle. The brace is applied around the forearm (below the head of the radius) and is tightened enough so that, when the patient contracts the wrist extensors, he or she does not fully contract the muscles.<ref name=":7" /> | |||
* '''Injections''' may be given subperiosteally to the extensor brevis origin. These injections are reported to have an early and beneficial effect. However, during the initial 24-28 hours, increased pain may be experienced. A steroid injection is usually followed by 1-2 weeks’ rest and should not be repeated more than 2 times. Steroid and hyaluronic acid injections are reported to be effective for about 3 months, indicating that the patient must continue with the exercise program.<ref name=":3" /> <ref>Zinger G, et al. [https://bmcsportsscimedrehabil.biomedcentral.com/articles/10.1186/s13102-022-00399-0 Hyaluronic acid injections for chronic tennis elbow.] BMC Sports Science, Medicine and Rehabilitation 2022; 14:1-8</ref> Platelet-rich plasma and autologous blood injections vary in preparation and efficacy. <ref>Simental-Mendia M, et al. [https://pubmed.ncbi.nlm.nih.gov/32103373/ Clinical efficacy of platelet-rich plasma in the treatment of lateral epicondylitis: a systematic review and meta-analysis of randomised placebo-controlled clinical trials.] Clin Rheumatol 2020;39:2255-2265</ref> <ref>Houck D, et al. T[https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6419259/ reatment of lateral epicondylitis with autologous blood, platelet-rich plasma or corticosteroid injections: a systematic review of overlapping meta-analyses.] Orthop J Sports Med 2019; 7(3):2325967119831052</ref> No clear benefit for injections has been shown over a placebo in the intermediate or long-term <ref>Sayegh E, Strauch R. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4317462/ Does nonsurgical treatment improve longitudinal outcomes of lateral epicondylitis over no treatment? A meta-analysis.] Clin Orthop Relat Res 2015; 473(3):1093-1107.</ref>and a consideration of possible re-occurence should be taken into account. <ref>Bisset L, et al. [https://pubmed.ncbi.nlm.nih.gov/17012266/ Mobilisation with movement and exercise, corticosteroid injection, or wait and see for tennis elbow: randomized trial.] BMJ 2006; 333(7575):939-944</ref> | |||
=== Surgical treatment === | |||
If non-operative management fails for more than 6 months., surgical treatment may be indicated. <ref>Sanders T, et al. [https://journals.sagepub.com/doi/full/10.1177/0363546514568087 The epidemiology and health care burden of tennis elbow: a population -based study.] Am J Sports Med 2015;43:1066-1071</ref> Most surgical procedures for this condition involve removing diseased muscle and reattaching healthy muscle back to bone. The right surgical approach will depend on a range of factors. These include the scope of injury, general health, and personal needs. | |||
* '''Open surgery'''.<ref name=":7" /><ref name=":10" /> This is the most common approach to LET repair. It involves making an incision over the elbow. Open surgery is usually performed as an outpatient surgery. It rarely requires an overnight stay at the hospital. | |||
* '''Arthroscopic surgery'''.<ref name=":7" /> <ref name=":10" /> LET can also be repaired using tiny instruments and small incisions. Like open surgery, this is a same-day or outpatient procedure. | |||
== Physiotherapy Management == | |||
General physiotherapy management methods for LET may include: <ref name=":1" /><ref name=":26" /> | |||
* Education/Advice on pain control and/or modification of activities | |||
* Modalities- Ice, Massage, Ultrasound, Transcutaneous Electrical Nerve Stimulation (TENS), Laser, Shockwave Therapy | |||
* Supervised Exercises- Strengthening and Stretching | |||
* Manual therapy- [[Mulligan Concept|Mulligan]] - Mobilisation with movement | |||
* Sport/Occupation Specific Rehabilitation | |||
< | ===Evidence for Physiotherapy=== | ||
Evidence regarding the optimal use of physiotherapy methods in the management of LET is still lacking. <ref name=":27" /> <ref>Sims S, et al. [https://journals.sagepub.com/doi/abs/10.1007/s11552-014-9642-x Non-surgical treatment of lateral epicondylitis: a systematic review of randomized controlled trials.] Hand 2014; 9(4):419-446</ref> <ref>Weber C, et al. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4549077/ Efficacy of physical therapy for the treatment of lateral epicondylitis: a meta-analysis.] BMC Musculoskeletal Disord 2015;16:223 </ref> <ref>Lapner P, et al. [https://www.sciencedirect.com/science/article/pii/S2666638321002590 Non-operative treatment of lateral epicondylitis: a systematic review and meta-analysis.] JSES International 2022; 6(2):321-330</ref><ref>Kim Y, et al. [https://pubmed.ncbi.nlm.nih.gov/33002980/ Efficacy of non-operative treatments for lateral epicondylitis: a systematic review and meta-analysis.] Plast Reconstr Surg 2021;147:112-125</ref> <ref>Dongni L, et al. [https://pubmed.ncbi.nlm.nih.gov/35212276/ The effect of ultrasound therapy on lateral epicondylitis. A meta-analysis.] Medicine 2022 Feb; 101(8):e28822</ref> Thus, the selection and/or combination of appropriate methods may vary for clinicians and patients. | |||
Below you can find some further information on some of the aforementioned physiotherapy methods. [[File:ESWT.jpg|thumb|346x346px|ESWT for LET |alt=]] | |||
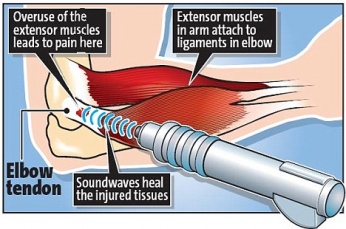
==== '''Extracorporeal Shockwave therapy (ESWT)''' ==== | |||
ESWT is a treatment method used in multiple tendonopathies including LET. Patients are exposed to strong mechanical wave impulses which can be used on a fairly accurate position. Several studies examine the effects of ESTW on LET.<ref name=":12">Hammer D, et al. [https://pubmed.ncbi.nlm.nih.gov/10853901/ Extracorporal shock wave therapy in patients with tennis elbow and painful heel.] Arch Orthop Trauma Surg 2000;120(5):304-307.</ref><ref name=":13">Crowther M, et al. [https://pubmed.ncbi.nlm.nih.gov/12188483/ A prospective, randomised study to compare extracorporeal shock-wave therapy and injection of steroid for the treatment of tennis elbow.] J Bone Joint Surg Br 2002;84(5):678-679</ref><ref name=":14">Rompe J, et al. [https://pubmed.ncbi.nlm.nih.gov/8881885/ Low-energy extracorporal shock wave therapy for persistent tennis elbow.] Int Orthop. 1996;20(1):23-27</ref><ref name=":15">Krischek O, et al. [https://pubmed.ncbi.nlm.nih.gov/10076947/ Shock-wave therapy for tennis and golfer’s elbow–1 year follow-up.] Arch Orthop Trauma Surg 1999;119(1):62-66</ref><ref name=":16">Stasinopoulos D, Johnson, M. [https://bjsm.bmj.com/content/39/3/132 Effectiveness of extracorporeal shock wave therapy for tennis elbow (lateral epicondylitis).] Br J Sports Med 2005; 39(3): 132-136</ref> Although the technique is widely reported as safe, there is a potential for haemorrhage and local soft tissue damage through cavitation and this appears to be more likely with high doses. <br> | |||
[[ | ==== '''Cyriax Physiotherapy''' ==== | ||
Cyriax physiotherapy combines the use of deep transverse friction (DTF) with Mill’s manipulations in LET. Both treatment components must be used jointly in the sequence specified. Patient must follow the protocol three times a week for four weeks.<ref name=":17">Viswas R., et al. [https://pubmed.ncbi.nlm.nih.gov/22629225/ Comparison of Effectiveness of Supervised Exercise Program and Cyriax Physiotherapy in Patients with Tennis Elbow (Lateral Epicondylitis): A Randomized Clinical Trial.] Scientific World Journal 2012; 2012:939645</ref> There are several contraindications regard to this therapy: active infections, bursitis, disorders of the nerve structures, ossification and calcification of the soft tissues, active rheumatoid arthritis, anticoagulant. Cyriax physiotherapy is suggested to be a better treatment compared to phonophoresis and exercise for treating LET with significantly better scores for all measurements at follow up (p<0.05). <ref>Mit V. et al. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2762836/ Cyriax Physiotherapy Versus Phonophoresis with Supervised Exercise in Subjects with LateralEpicondylalgia: A Randomized Clinical Trial,] J Man Manip Ther 2009; 17(3): 171-178</ref> | |||
[[File:Frictions.jpg|thumb|Deep transverse frictions for tennis elbow]] | |||
'''Deep Transverse Frictions'''<br>Deep transverse friction is a specific type of connective tissue massage applied precisely to the soft tissue structures. The therapist must try to reach an analgesic effect applying the DTF at the point of the lesion for 10 min till a numbing effect has been reached, that all for preparing the tendon for Mill’s manipulations. Pain during the friction massage is considered as a wrong indication. An interval of 48 hours between two sessions is necessary. <ref name=":17" />The purpose of the deep friction massage is to maintain the mobility within the soft tissue structures. <ref>Chamberlain G. Cyriax's Friction Massage: A Review. J Orthop Sports Phys Ther 1982;4(1):16-22</ref> It seems to have a pain relief function, due to modulation of the nociceptive impulses (gate control theory), a better alignment of connective tissue fibrils, softens the scar tissue, and blood flow increases, but further studies are needed.<br>The patient should be positioned with arm fully supinated in 90° of elbow flexion, identify the area of tenderness on the lateral epicondyle and apply pressure (DTF), with the tip of the thumb on the lateral epicondyle, in a posterior direction on the teno-osseous junction. The other hand stabilises the patient’s wrist.<ref name=":17" /> | |||
'''Mills Radial Head Manipulation''' | |||
<clinicallyrelevant id="172115631" title="Mills Radial Head Manipulation" /> | |||
<br> | Mill's manipulation is the most common technique used by physiotherapists and is a small-amplitude high-velocity thrust performed at the end of elbow extension while the wrist and hand are held flexed.<ref name=":18">Vicenzino B, et al. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2565595/ Joint Manipulation in the Management of Lateral Epicondylalgia: A Clinical Commentary]. J Man Manip Ther 2007; 15(1): 50–56 </ref> The aim of this technique is to elongate the scar tissue by rupturing adhesions within the teno-oseous junction, making the area mobile and pain free. It’s used to imitate the mechanism of spontaneous recovery. <ref name=":18" />Mill’s intention was to shift the annular ligament and replace it. Cyriax found that the annular ligament applies the greatest possible stretching tension to the extensor carpi radialis muscles, that’s why the manipulative procedure should be carried out with a sharp jerk, in order to open the tear in the tendon and relieve tension on the tendon scar by converting a tear.<ref name=":18" />This manipulation must only be performed if a fully pain-free elbow extension can be achieved, and with a properly technique. To prevent symptoms worsening, full wrist flexion must be achieved during the procedure. <ref name=":18" />Patient seated with the affected extremity in 90° abduction and internal rotation (olecranon faced up).Therapist stands behind the patient, stabilises the patient’s wrist in full pronation and flexion, while the other hand is placed on the olecranon. The maintenance of full wrist flexion is important as failure to maintain this position could lead to a majority of the thrusting force being bome by the humeroulnar joint. The high-velocity low amplitude (HVLA) thrust at the end range of elbow extension, is a quick movement in the direction illustrated.<ref name=":19">Nagrale V, et al. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2762836/ Cyriax Physiotherapy Versus Phonophoresis with Supervised Exercise in Subjects with LateralEpicondylalgia: A Randomized Clinical] Trial. J Man Manip Ther 2009; 17(3): 171-178 </ref><br>This manipulation may produce mild discomfort at the instant of its performance. The clinician may apply this procedure a 2-3 times a week, with a range of 4-12 sessions.<ref name=":19" /> | ||
<br> | ==== '''Exercise therapy''' ==== | ||
Exercise therapy is a regimen or plan of physical activities designed and prescribed for specific therapeutic goals. Its purpose is to restore normal musculoskeletal function or to reduce pain caused by diseases or injuries. Strength, stamina and mobility should be improved by exercises once the pain and inflammation are under control. <ref name=":17" /><ref name=":19" /> Supervised exercise programmes may be the first treatment in managing LET compared to Cyriax physiotherapy. <ref name=":17" />Combinations of exercise/manipulation and exercise/stretching may have a short-term effect, with the latter also having a long-term effect.<ref name=":7" /><br> | |||
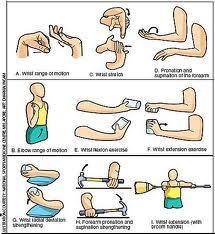
'''Stretching''' | |||
- | Strengthening and stretching exercises are one of the most important components of exercise programmes. The underlying principle of stretching is that, by lengthening the tendon during relaxation, we can reduce its stretching during offending movements. The best stretching position for the [[Extensor Carpi Radialis Brevis]] tendon, is reached with the elbow in extension, forearm in pronation, wrist in flexion and with ulnar deviation of the wrist, according to the patient’s tolerance. This stretching should be held for 30- 45 s and 3 times before and after the eccentric exercises, during each treatment session with a 30 s rest interval.<br> | ||
Other programs suggest that stretching exercises for the extensor muscles of the wrist and fingers should be performed in the following manner: fully extend the elbow and palmary flex the wrist. Remain in the point of maximum non painful extension for a period of 15 to 25s. this exercises is repeated four to five times a day with two series of ten exercises in each session: the patient should always stop at the first sign of pain. In this phase of therapy, the patient should also perform isotonic exercises, once a day, according to the following plan:<ref name=":17" /> <br>1. Stretching exercises = repeat 10 times (15-25 seconds)<br>2. Isotonic exercises = repeat 15 times (3 series)<br>3. Stretching exercises = repeat 10 times (15-25 seconds)<br>4. Icing = massage the tender area with ice or crushed ice for 10-15 minutes<br> [[File:Exercisesd.jpg|thumb|234x234px|Sample eccentric exercises for tennis elbow]] | |||
'''Eccentric exercises''' | |||
There are three principles of eccentric exercises. These are load ( resistance), speed (velocity) and frequency of contractions.<ref name=":20">Stanish W, et al. [https://pubmed.ncbi.nlm.nih.gov/3720143/ Eccentric exercise in chronic tendinitis]. Clin Orthop Relat Res 1986;208:65-68</ref> | |||
# ''Load ( resistance):'' Increasing the load ensures the tendon is subjected to greater stress and forms the fundamental basis of the progression of the exercise programme. The basis of all physical training programmes is formed by this principle of progressive overloading. According to the patient’s symptoms, it is important that the load of these eccentric exercises should be increased. If it’s not increased then the possibility of re-injury will be high. | |||
# ''Speed ( velocity):'' The speed (velocity) of contractions is also a fundamental principle of successful eccentric exercises. In each treatment session the speed of the eccentric training should be increased. Hence the load on the tendon increases to stimulate the mechanism of the injury. However the therapists must ensure that the patients perform the eccentric exercises slowly to avoid pain. | |||
# ''Frequency of contractions:'' The frequency of contractions is the third principle of eccentric exercises. There can be variations of sets and repetitions in the literature. According to the therapists 3 sets of 10 repetitions can normally be performed without overloading the injured tendon, as determined by the tolerance of the patient. The elbow is in full extension, forearm in pronation and the arm is supported. The greatest strengthening result for the extensor tendons of the wrist is reached in this position. This is a recommendation and the frequency must be patient specific.<ref name=":20" /> | |||
<br>'''Theraband Exercise:'''<br>Theraband exercises (or exercises with a small weight) are performed each day for 3 sets of 10. You fix one side of the theraband under you feet or another place and you take the other side in your hand or you have a small weight in your hand. <br>The patient starts the exercise in wrist flexion, then he/she does a wrist extension and comes back to the start position very slowly. <ref name=":6" /> This exercise is an concentric and eccentric exercise for the wrist extensors. Supervised exercise consisting of static stretching and eccentric strengthening for 4 weeks is suggested to have larger effects in reducing pain, strength and function, compared to the Cyriax physiotherapy approach. Once the patients can do this, they can progress to another colour of theraband or you increase the weight. <ref name=":6" />[[File:Flexbar.jpg|thumb|Flexbar for tennis elbow<ref>https://goo.gl/images/dG2t3E</ref>]] | |||
'''Flexbar® Exercises''' | |||
= | The Flexbar® is a resistance device which can be used at home. <ref name=":11" /> | ||
The FlexBar® exercise is performed each day for 3 sets of 15. It takes 4 seconds to complete each repetition and between each set of 15 repetitions there is 30 seconds of rest. Once the patients can perform 3 sets of 15, they progress to another colour FlexBar® with a higher intensity of eccentric resistance.The treatment continues until the patient has a resolution of symptoms. | |||
< | == Taping == | ||
Diamond taping method by rigid tape may be useful for reducing pain and improving grip strength and functional performance<ref>Mehta J, et al. [http://www.medtextpublications.com/open-access/effect-of-taping-on-pain-grip-strength-and-function-in-deskbound-workers-with-lateral-epicondylalgia-285.pdf Effect of Taping on Pain, Grip Strength, and Function in Deskbound Workers with Lateral Epicondylalgia] World J Phys Med Rehab 2019; 1.</ref> | |||
== Clinical Bottom Line == | |||
LET is the most common overuse syndrome in the elbow. It is an injury involving the extensor muscles of the forearm. In the majority of cases, the insertion of the extensor carpi radialis brevis is involved. Contractile overloads that chronically tension or stress the tendon near the attachment on the humerus are the primary cause of LET. It occurs often in repetitive upper extremity activities such as computer use, heavy lifting, forceful forearm pronation and supination, and repetitive vibration. Non-operative management may consist of NSAIDs, ice, elevation and the use of an elbow counterforce brace. If the symptoms are resistant, surgical treatment may be indicated. Concerning physical therapy management, there are different types of methods to treat LET. The selection and/or combination of appropriate methods may vary for clinicians and patients. | |||
In a study conducted to investigate the effects of prolotherapy, physiotherapist guided manual therapy/exercise program, or the combination of both interventions in the management of LET, it was concluded that single modality treatments (prolotherapy or physiotherapy) are clinically and cost effective <ref>Yelland M, Rabago D, Ryan M, Ng SK, Vithanachchi D, Manickaraj N, Bisset L. Prolotherapy injections and physiotherapy used singly and in combination for lateral epicondylalgia: a single-blinded randomised clinical trial. BMC musculoskeletal disorders. 2019 Dec;20(1):1-0.</ref>. | |||
== References == | |||
<references /> | |||
[[Category:Conditions]] | |||
[[Category:Elbow - Conditions]] | |||
[[Category:Joints]] | |||
[[Category:Musculoskeletal/Orthopaedics]] | |||
[[Category:Elbow]] | |||
[[Category:Sports Injuries]] | |||
[[Category:Sports Medicine]] | |||
[[Category:Tendinopathy]] | |||
[[Category: | |||
Latest revision as of 21:11, 29 March 2024
Original Editors - Hannah Norton
Top Contributors - Angeliki Chorti, Adam Vallely Farrell, Admin, Charlotte Sirago, Elien Vanderlinden, Nikhil Benhur Abburi, Vanwymeersch Celine, Kim Jackson, Johnathan Fahrner, Evan Thomas, Celien Van den Meerssche, Rachael Lowe, Hannah Norton, Assia Dad, Ruben Vellemans, Simisola Ajeyalemi, Kai A. Sigel, Quentin Desantoine, Jelien Wouters, Wanda van Niekerk, Maëlle Cormond, Pacifique Dusabeyezu, Wendy Walker, Candace Goh, Naomi O'Reilly, Irene Leahy and Jolien Rottie
Description[edit | edit source]
Lateral epicondylitis, also commonly referred to as tennis elbow, describes an overuse injury that occurs secondary to an eccentric overload of the common extensor tendon at the origin of the extensor carpi radialis brevis (ECRB) tendon. [1]These muscles originate on the lateral epicondylar region of the distal humerus. In many cases, the insertion of the extensor carpi radialis brevis is involved.
It should be remembered that only 5% of people suffering from tennis elbow relate the injury to tennis! Contractile overloads that chronically stress the tendon near the attachment on the humerus are the primary cause of LET. It occurs often in repetitive upper extremity activities such as computer use, heavy lifting, forceful forearm pronation and supination, and repetitive vibration. Despite the name, you will also commonly see this chronic condition in other sports such as squash, badminton, baseball, swimming and field throwing events. People with repetitive one-sided movements in their jobs such as electricians, carpenters, gardeners, desk bound jobs also commonly present with this condition.[2][3] [4][5][6]
Clinically Relevant Anatomy[edit | edit source]
The elbow joint is made up of three bones: the humerus (upper arm bone), the radius and ulna (two bones in the forearm). At the distal end of the humerus there are two epicondyles, one lateral (on the outside) and one medial (on the inside).
The area of maximal tenderness is usually an area just distal to the origin of the extensor muscles of the forearm at the lateral epicondyle. Most commonly, the extensor carpi radialis brevis (ECRB) is involved, but others may include the extensor digitorum, extensor carpi radialis longus (ECRL), and extensor carpi ulnaris. [3][7]
The radial nerve is also in close proximity to this region, and divides into the superficial radial nerve and the posterior interosseous nerve.
Epidemiology/Aetiology[edit | edit source]
LET is classified as an overuse injury that may result in hyaline degeneration of the origin of the extensor tendon. Overuse of the muscles and tendons of the forearm and elbow together with repetitive contractions or manual tasks can put too much strain on the elbow tendons. These contractions or manual tasks require manipulation of the hand that causes maladaptations in tendon structure that lead to pain over the lateral epicondyle. Mostly, the pain is located anterior and distal from the lateral epicondyle.[4]
Elbow tendinopathy occurs at least five times more often and predominantly occurs on the lateral rather than on the medial aspect of the joint, with a 4:1 to 7:1 ratio. It affects 1-3% of the population, with those 35-50 years old most commonly being affected. [8] [9]If a patient is <35 , it is important to consider differential diagnosis (growth plate disorder, referral from the cervical spine). If a patient is >50, consider osteoarthritis (OA), referred cervical spine pain. In a study by Nirschl, [10] of 200 tennis players aged >30, 50% had symptoms of LET at some stage.
This injury is often work-related, any activity involving wrist extension, pronation or supination during manual labour, housework and hobbies are considered as important causal factors.[11] LET is equally common in both sexes. [12] Between the ages of 30-50 years the disease is most prevalent. [8] Obtaining the condition at both lateral epicondyles is rare, the dominant arm has the greatest chance of the occurrence of LET. Twenty percent of cases persist for more than a year. [3]
A systematic review identified 3 risk factors: handling tools heavier than 1 kg, handling loads heavier than 20 kg at least 10 times per day, and repetitive movements for more than 2 hours per day. Other risk factors are overuse, repetitive movements, training errors, misalignments, flexibility problems, ageing, poor circulation, strength deficits or muscle imbalance and psychological factors.[13]
There are several opinions concerning the cause of LET:
1.Inflammation
Although the previous term epicondylitis implies the presence of an inflammatory condition, inflammation is present only in the earliest stages of the disease process. [14]
2. Microscopic tearing
- Nirschl and Pettrone [15] attributed the cause to microscopic tearing with formation of reparative tissue (angiofibroblastic hyperplasia) in the origin of the extensor carpi radialis brevis (ECRB) muscle. This micro-tearing and repair response can lead to macroscopic tearing and structural failure of the origin of the ECRB muscle.
- That microscopic or macroscopic tears of the common extensor origin were involved in the disease process, was postulated by Cyriax in 1936. [16]
- The first to describe macroscopic tearing in association with the histological findings were Coonrad and Hooper. [17]
- Histology of tissue samples shows "collagen disorientation, disorganisation, and fibre separation by increased proteoglycan content, increased cellularity, neovascularisation, with local necrosis." Nirschl [10] termed these histological findings bangiofibroblastic hyperplasia. The term has since been modified to bangiofibroblastic tendinosis. He noted that the tissue was characterised by disorganized, immature collagen formation with immature fibroblastic and vascular elements. This grey, friable tissue is found in association with varying degrees of tearing involving the extensor carpi radialis brevis.
3. Degenerative Process
The histopathological features of 11 patients who had LET were examined by Regan et al. [18] They determined that the cause of LET was more indicative of a degenerative process than an inflammatory process. The condition is degenerative with increased fibroplasts, vascular hyperplasia, proteoglycans and glycosaminoglycans, and disorganized and immature collagen. Repetitive eccentric or concentric overloading of the extensor muscle mass is thought to be the cause of this angiofibroplastic tendinosis of the ECRB. LET is a degenerative condition in which increased fibroplastic activity and granulation tissue formation occur within the tendon. [4] [5]
4. Hypovascularity
Because this tendinous region contains areas that are relatively hypovascular, the tendinous unit is unable to respond adequately to repetitive forces transmitted through the muscle, resulting in declining functional tolerance. [19]
Clinical Presentation[edit | edit source]
The most prominent symptom of LET is pain, which can be produced by palpation on the extensor muscles origin on the lateral epicondyle. The pain can radiate upwards along the upper arm and downwards along the outside of the forearm and in rare cases even to the third and fourth fingers. Furthermore, it is also often seen that the flexibility and strength in the wrist extensor and posterior shoulder muscles are deficient. [4] [5]
According to Warren [20], there are four stages on the development of this injury with regard to the intensity of the symptoms.
1. Faint pain a couple of hours after the provoking activity.
2. Pain at the end of or immediately after the provoking activity.
3. Pain during the provoking activity, which intensifies after ceasing that activity.
4. Constant pain, which prohibits any activity.
Furthermore, it is often seen that the flexibility and strength in the wrist extensor and posterior shoulder muscles are deficient. At least patients report weakness in their grip strength or difficulty carrying objects in their hand, especially with the elbow extended. This weakness is due to finger extensor and supinator weakness. Some people have a sense of paralysis but this is rare. [11][20] [21]
Symptoms last, on average, from 2 weeks to 2 years. 89% of the patients recover within 1 year without any treatment except perhaps avoidance of the painful movements (sport injuries) [16][22] [23]
Assessment Findings[edit | edit source]
A thorough assessment and examination are key elements in ensuring that the correct treatment plan is implemented, enhancing the recovery process. The assessment should also include elements to exclude a differential diagnosis.
Possible subjective assessment findings may include:
- Onset of pain 24-72 hours after provocative activity involving wrist extension
- Pain may radiate down forearm as far as the wrist and hand
- Difficulty with lift and grip (pain+/- weakness)
- Changes in biomechanical factors e.g. new tennis racquet, wet ball, over training, poor technique, shoulder injury[24][25]
In the objective assessment, one may find:
- Pain and point tenderness over lateral epicondyle and/or 1-2 cm distal to epicondyle
- Pain and weakness on resisted wrist extension
- Weakness on grip strength testing (Dynamo-meter)
- Pain and/or decreased movement on passive elbow extension, wrist flexion and ulnar deviation and pronation
- Weak elbow extensors and flexors[24][25]
Diagnostic Procedures[edit | edit source]
The diagnosis starts with history taking and questions about the activity level, occupational risk factors, recreational sports participation, medication and other medical problems. It’s important to know which activities cause symptoms and where on your arm the symptoms occur.[2]
During the physical exam, the structure of the elbow and other joints is assessed. Also the nerves, muscles, bones and skin are examined. The diagnosis of LET is substantiated by tenderness over the ECRB or common extensor origin. By the following methods, the therapist or physiotherapist should be able to reproduce the typical pain:
- To examine the severity of the tennis elbow, there is a dynamometer and a Patient-rated Tennis Elbow Evaluation Questionnaire (PrTEEQ).[26] [27] The dynamometer measures grip strength. [28] The PrTEEQ is a 15-item questionnaire, designed to measure forearm pain and disability in patients with lateral epicondylitis. The patients have to rate their levels of tennis elbow pain and disability from 0 to 10, and consists of 2 subscales. There is a pain subscale (0 = no pain, 10 = worst imaginable) and a function subscale (0 = no difficulty, 10 = unable to do).
- Cozen’s test: Cozen’s test is also known as the resisted wrist extension test. The elbow is stabilised in 90° flexion. The therapist palpates the lateral epicondyle and the other hand of the therapist positions the patient’s hand into radial deviation and forearm pronation. Then the patient is asked to resist wrist extension. The test is positive if the patient experiences a sharp, sudden, severe pain over the lateral epicondyle.[29] [30][[31] High sensitivity [8] [32] has been found with positive findings suggesting the presence of LET but poor specificity to exclude other differential diagnoses.
- Chair test: The patient grasps the back of the chair while standing behind it and attempts to lift the chair by using a three finger pinch (thumb, index long fingers) and the elbow fully extended. The test is positive when pain occurs at the lateral epicondyle. [31]
- Mill's Test: The patient is seated with the upper extremity relaxed at the side and the elbow extended. The examiner passively stretches the wrist in flexion and pronation. Pain at the lateral epicondyle or proximal musculotendinous junction of the wrist extensors is a positive sign for LET. [4][31][33]
- Maudsley’s test: The examiner resists extension of the third digit of the hand, while palpating the lateral epicondyle. A positive test is indicated by pain over the lateral epicondyle.[4][33]An 88% sensitivity has been found for including the LET diagnosis but not excluding it with confidence. [32]
- The coffee cup test [17]: The test is performed while doing a specific activity such as picking up a full cup of coffee or a milk bottle. The patient is asked to rate their pain on a scale of zero to ten.[4][33]
A differential diagnosis should also be considered.
Differential diagnosis[edit | edit source]
- Radial Tunnel Syndrome [34]
- Pain in the posterolateral area of the forearm
- Pain sometimes spreads to the dorsal side of the wrist
- Parasthesia
- Weakness (overuse injuries of the musculoskeletal system)
- Posterior interosseus nerve syndrome [35] [36][37]
- Pain
- Weakness involving wrist extension and finger extension
- Motor deficits
- Elbow osteoarthritis
- Pain
- Loss of range of motion
- Fractures
- Distal Radial Fracture
- Radial Head Fracture
- Olecranon Fracture
- Cervical Radiculopathy
- Radiating arm pain corresponding to the dermatomes
- Neck pain
- Parasthesia
- Muscle weakness in myotome
- Reflex impairment/loss
- Headache
- Scapular pain
- Sensory and motor dysfunction in upper extremities and neck
- Cervical Disc Disease
- Cervical Myofascial Pain
- Cervical Spondylosis
- Fibromyalgia
- Medial Epicondylitis
Further Diagnostic Investigations[edit | edit source]
Investigations are usually not performed in the straightforward case of lateral elbow pain.
Ultrasound examination may be used in the investigation of patients with lateral elbow pain to demonstrate the degree of tendon damage as well as the presence of a bursa. [25]
In longstanding cases, plain X-ray (AP and lateral views) of the elbow may be taken to rule out arthritis of the elbow. Calcification along the lateral epicondyle [25], osteochondritis dissecans, degenerative joint changes or evidence of heterotopic calcification are among the common findings.
Electromyography (EMG) may be used to rule out nerve compression. Many nerves travel around the elbow, and the symptoms of nerve compression are similar to those of tennis elbow.
If there is suspicion that the symptoms are neck-related, a Magnetic Resonance Imaging (MRI) scan may be ordered.
This might show if there is a possible herniated disk or arthritis in the area of the neck. Both of these conditions often produce arm pain.
An MRI may also show thickening, hypoechogenicity or defects in the tendo-osseous enthesis in the case of LET, [25]but the presence of these findings should be interpreted with caution when directing clinical decisions. [8] [39]
Outcome Measures[edit | edit source]
The use of outcome measures in LET elbow clinical practice and research is not widely established. [40] [41] However, some commonly used scales are the following:
- Pain reported outcome measures;
- Numeric Pain Rating Scale (NPRS)
- Visual Analogue Scale (VAS)
- Self-reported Questionnaires;
- The Upper Limb Functional Index (ULFI):
- Patient Rated Tennis Elbow Evaluation (PRTEE):
- QuickDASH (Disabilities of the Arm Shoulder and Hand):
- Patient Specific Functional Scale (PSFS) - although the PSFS has not yet been validated for LET, it has been shown to be valid, reliable and responsive to change in other conditions such as knee dysfunction, cervical radiculopathy, acute low back pain, mechanical low back pain, and neck dysfunction (Pain ICC = 0.89-0.99, Function ICC = 0.83-0.99, Total ICC = 0.89-0.99)[42][43][44]
Recently, an international group of experts in the field of tendinopathy published a consensus paper proposing nine health-related core domains against which clinicians and researchers measure outcomes, [45]:
- Patient rating of condition
- Participation in life activities
- Pain on activity/loading
- Function
- Psychological factors
- Physical function capacity
- Disability
- Quality of life
- Pain over a specified time
Attempts are under way to develop a core outcome set for LET (COS-LET). [46]
Medical Management[edit | edit source]
Non-Operative Medical Treatment[edit | edit source]
Non-operative medical treatment of LET is the first-line management of LET. It is initially based on the following principles: relieving pain and controlling inflammation. This may include:
- Advice for relieving pain commonly includes rest and activity modification.
- NSAIDs may be used in the acute cases for controlling the inflammation and relieving pain in the short-term. [47] The use of ice three times per day for 15 minutes is also recommended for reducing the inflammatory response and swelling by decreasing the level of chemical activity and by vasocoinstriction. Elevation of the extremity is also indicated if an oedema of the wrist or fingers is present.[5]
- An elbow counterforce brace may also be effective in reducing the LET pain during contraction. [48] As a forearm orthosis, it may play a role of a secondary muscle attachment site and relieve tension on the insertion at the lateral epicondyle. The brace is applied around the forearm (below the head of the radius) and is tightened enough so that, when the patient contracts the wrist extensors, he or she does not fully contract the muscles.[2]
- Injections may be given subperiosteally to the extensor brevis origin. These injections are reported to have an early and beneficial effect. However, during the initial 24-28 hours, increased pain may be experienced. A steroid injection is usually followed by 1-2 weeks’ rest and should not be repeated more than 2 times. Steroid and hyaluronic acid injections are reported to be effective for about 3 months, indicating that the patient must continue with the exercise program.[5] [49] Platelet-rich plasma and autologous blood injections vary in preparation and efficacy. [50] [51] No clear benefit for injections has been shown over a placebo in the intermediate or long-term [52]and a consideration of possible re-occurence should be taken into account. [53]
Surgical treatment[edit | edit source]
If non-operative management fails for more than 6 months., surgical treatment may be indicated. [54] Most surgical procedures for this condition involve removing diseased muscle and reattaching healthy muscle back to bone. The right surgical approach will depend on a range of factors. These include the scope of injury, general health, and personal needs.
- Open surgery.[2][14] This is the most common approach to LET repair. It involves making an incision over the elbow. Open surgery is usually performed as an outpatient surgery. It rarely requires an overnight stay at the hospital.
- Arthroscopic surgery.[2] [14] LET can also be repaired using tiny instruments and small incisions. Like open surgery, this is a same-day or outpatient procedure.
Physiotherapy Management[edit | edit source]
General physiotherapy management methods for LET may include: [25][41]
- Education/Advice on pain control and/or modification of activities
- Modalities- Ice, Massage, Ultrasound, Transcutaneous Electrical Nerve Stimulation (TENS), Laser, Shockwave Therapy
- Supervised Exercises- Strengthening and Stretching
- Manual therapy- Mulligan - Mobilisation with movement
- Sport/Occupation Specific Rehabilitation
Evidence for Physiotherapy[edit | edit source]
Evidence regarding the optimal use of physiotherapy methods in the management of LET is still lacking. [23] [55] [56] [57][58] [59] Thus, the selection and/or combination of appropriate methods may vary for clinicians and patients.
Below you can find some further information on some of the aforementioned physiotherapy methods.
Extracorporeal Shockwave therapy (ESWT)[edit | edit source]
ESWT is a treatment method used in multiple tendonopathies including LET. Patients are exposed to strong mechanical wave impulses which can be used on a fairly accurate position. Several studies examine the effects of ESTW on LET.[60][61][62][63][64] Although the technique is widely reported as safe, there is a potential for haemorrhage and local soft tissue damage through cavitation and this appears to be more likely with high doses.
Cyriax Physiotherapy[edit | edit source]
Cyriax physiotherapy combines the use of deep transverse friction (DTF) with Mill’s manipulations in LET. Both treatment components must be used jointly in the sequence specified. Patient must follow the protocol three times a week for four weeks.[65] There are several contraindications regard to this therapy: active infections, bursitis, disorders of the nerve structures, ossification and calcification of the soft tissues, active rheumatoid arthritis, anticoagulant. Cyriax physiotherapy is suggested to be a better treatment compared to phonophoresis and exercise for treating LET with significantly better scores for all measurements at follow up (p<0.05). [66]
Deep Transverse Frictions
Deep transverse friction is a specific type of connective tissue massage applied precisely to the soft tissue structures. The therapist must try to reach an analgesic effect applying the DTF at the point of the lesion for 10 min till a numbing effect has been reached, that all for preparing the tendon for Mill’s manipulations. Pain during the friction massage is considered as a wrong indication. An interval of 48 hours between two sessions is necessary. [65]The purpose of the deep friction massage is to maintain the mobility within the soft tissue structures. [67] It seems to have a pain relief function, due to modulation of the nociceptive impulses (gate control theory), a better alignment of connective tissue fibrils, softens the scar tissue, and blood flow increases, but further studies are needed.
The patient should be positioned with arm fully supinated in 90° of elbow flexion, identify the area of tenderness on the lateral epicondyle and apply pressure (DTF), with the tip of the thumb on the lateral epicondyle, in a posterior direction on the teno-osseous junction. The other hand stabilises the patient’s wrist.[65]
Mills Radial Head Manipulation
Mills Radial Head Manipulation video provided by Clinically Relevant
Mill's manipulation is the most common technique used by physiotherapists and is a small-amplitude high-velocity thrust performed at the end of elbow extension while the wrist and hand are held flexed.[68] The aim of this technique is to elongate the scar tissue by rupturing adhesions within the teno-oseous junction, making the area mobile and pain free. It’s used to imitate the mechanism of spontaneous recovery. [68]Mill’s intention was to shift the annular ligament and replace it. Cyriax found that the annular ligament applies the greatest possible stretching tension to the extensor carpi radialis muscles, that’s why the manipulative procedure should be carried out with a sharp jerk, in order to open the tear in the tendon and relieve tension on the tendon scar by converting a tear.[68]This manipulation must only be performed if a fully pain-free elbow extension can be achieved, and with a properly technique. To prevent symptoms worsening, full wrist flexion must be achieved during the procedure. [68]Patient seated with the affected extremity in 90° abduction and internal rotation (olecranon faced up).Therapist stands behind the patient, stabilises the patient’s wrist in full pronation and flexion, while the other hand is placed on the olecranon. The maintenance of full wrist flexion is important as failure to maintain this position could lead to a majority of the thrusting force being bome by the humeroulnar joint. The high-velocity low amplitude (HVLA) thrust at the end range of elbow extension, is a quick movement in the direction illustrated.[69]
This manipulation may produce mild discomfort at the instant of its performance. The clinician may apply this procedure a 2-3 times a week, with a range of 4-12 sessions.[69]
Exercise therapy[edit | edit source]
Exercise therapy is a regimen or plan of physical activities designed and prescribed for specific therapeutic goals. Its purpose is to restore normal musculoskeletal function or to reduce pain caused by diseases or injuries. Strength, stamina and mobility should be improved by exercises once the pain and inflammation are under control. [65][69] Supervised exercise programmes may be the first treatment in managing LET compared to Cyriax physiotherapy. [65]Combinations of exercise/manipulation and exercise/stretching may have a short-term effect, with the latter also having a long-term effect.[2]
Stretching
Strengthening and stretching exercises are one of the most important components of exercise programmes. The underlying principle of stretching is that, by lengthening the tendon during relaxation, we can reduce its stretching during offending movements. The best stretching position for the Extensor Carpi Radialis Brevis tendon, is reached with the elbow in extension, forearm in pronation, wrist in flexion and with ulnar deviation of the wrist, according to the patient’s tolerance. This stretching should be held for 30- 45 s and 3 times before and after the eccentric exercises, during each treatment session with a 30 s rest interval.
Other programs suggest that stretching exercises for the extensor muscles of the wrist and fingers should be performed in the following manner: fully extend the elbow and palmary flex the wrist. Remain in the point of maximum non painful extension for a period of 15 to 25s. this exercises is repeated four to five times a day with two series of ten exercises in each session: the patient should always stop at the first sign of pain. In this phase of therapy, the patient should also perform isotonic exercises, once a day, according to the following plan:[65]
1. Stretching exercises = repeat 10 times (15-25 seconds)
2. Isotonic exercises = repeat 15 times (3 series)
3. Stretching exercises = repeat 10 times (15-25 seconds)
4. Icing = massage the tender area with ice or crushed ice for 10-15 minutes
Eccentric exercises
There are three principles of eccentric exercises. These are load ( resistance), speed (velocity) and frequency of contractions.[70]
- Load ( resistance): Increasing the load ensures the tendon is subjected to greater stress and forms the fundamental basis of the progression of the exercise programme. The basis of all physical training programmes is formed by this principle of progressive overloading. According to the patient’s symptoms, it is important that the load of these eccentric exercises should be increased. If it’s not increased then the possibility of re-injury will be high.
- Speed ( velocity): The speed (velocity) of contractions is also a fundamental principle of successful eccentric exercises. In each treatment session the speed of the eccentric training should be increased. Hence the load on the tendon increases to stimulate the mechanism of the injury. However the therapists must ensure that the patients perform the eccentric exercises slowly to avoid pain.
- Frequency of contractions: The frequency of contractions is the third principle of eccentric exercises. There can be variations of sets and repetitions in the literature. According to the therapists 3 sets of 10 repetitions can normally be performed without overloading the injured tendon, as determined by the tolerance of the patient. The elbow is in full extension, forearm in pronation and the arm is supported. The greatest strengthening result for the extensor tendons of the wrist is reached in this position. This is a recommendation and the frequency must be patient specific.[70]
Theraband Exercise:
Theraband exercises (or exercises with a small weight) are performed each day for 3 sets of 10. You fix one side of the theraband under you feet or another place and you take the other side in your hand or you have a small weight in your hand.
The patient starts the exercise in wrist flexion, then he/she does a wrist extension and comes back to the start position very slowly. [20] This exercise is an concentric and eccentric exercise for the wrist extensors. Supervised exercise consisting of static stretching and eccentric strengthening for 4 weeks is suggested to have larger effects in reducing pain, strength and function, compared to the Cyriax physiotherapy approach. Once the patients can do this, they can progress to another colour of theraband or you increase the weight. [20]

Flexbar® Exercises
The Flexbar® is a resistance device which can be used at home. [6]
The FlexBar® exercise is performed each day for 3 sets of 15. It takes 4 seconds to complete each repetition and between each set of 15 repetitions there is 30 seconds of rest. Once the patients can perform 3 sets of 15, they progress to another colour FlexBar® with a higher intensity of eccentric resistance.The treatment continues until the patient has a resolution of symptoms.
Taping[edit | edit source]
Diamond taping method by rigid tape may be useful for reducing pain and improving grip strength and functional performance[72]
Clinical Bottom Line[edit | edit source]
LET is the most common overuse syndrome in the elbow. It is an injury involving the extensor muscles of the forearm. In the majority of cases, the insertion of the extensor carpi radialis brevis is involved. Contractile overloads that chronically tension or stress the tendon near the attachment on the humerus are the primary cause of LET. It occurs often in repetitive upper extremity activities such as computer use, heavy lifting, forceful forearm pronation and supination, and repetitive vibration. Non-operative management may consist of NSAIDs, ice, elevation and the use of an elbow counterforce brace. If the symptoms are resistant, surgical treatment may be indicated. Concerning physical therapy management, there are different types of methods to treat LET. The selection and/or combination of appropriate methods may vary for clinicians and patients.
In a study conducted to investigate the effects of prolotherapy, physiotherapist guided manual therapy/exercise program, or the combination of both interventions in the management of LET, it was concluded that single modality treatments (prolotherapy or physiotherapy) are clinically and cost effective [73].
References[edit | edit source]
- ↑ Buchanan BK, Varacallo M. Tennis Elbow (Lateral Epicondylitis) [Internet]. Nih.gov. StatPearls Publishing; 2019. Available from: https://www.ncbi.nlm.nih.gov/books/NBK431092/
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 Alexander J, et al. Sonography and MR Imaging of Posterior Interosseous Nerve Syndrome with Surgical Correlation. AJR Am J Roentgenology 2003; 181(1): 219-221
- ↑ 3.0 3.1 3.2 Walz D, et al. Epicondylitis: Pathogenesis, Imaging, and Treatment. RadioGraphics. 2010; 30(1): 167 - 184
- ↑ 4.0 4.1 4.2 4.3 4.4 4.5 4.6 Pienimäki T, et al. Associations Between Pain, Grip Strength, and Manual Tests in the Treatment Evaluation of Chronic Tennis Elbow . Clin J Pain 2002; 18(3):164-170
- ↑ 5.0 5.1 5.2 5.3 5.4 Whaley A, Baker C. Lateral epicondylitis. Clin Sports Med 2004;23(4):677– 691
- ↑ 6.0 6.1 Page P. A new exercise for tennis elbow that works! N Am J Sports Phys Ther 2010; 5(3): 189–193
- ↑ Stasinopoulos D, Johnson M. Cyriax physiotherapy for tennis elbow/lateral epicondylitis. Br J Sports Med 2004; 38:675-677
- ↑ 8.0 8.1 8.2 8.3 Karanasios S. et al. Diagnostic accuracy of examination tests for lateral elbow tendinopathy (LET) - A systematic review. Journal of Hand Therapy 2021; S0894-1130(21)0039-9
- ↑ Vaquero-Picado A, Barco R, Antuña SA. Lateral epicondylitis of the elbow. EFORT Open Rev. 2017 Mar 13;1(11):391-397.
- ↑ 10.0 10.1 Nirschl R. Tennis elbow. Orthop North Am. 1973;4:787-99.
- ↑ 11.0 11.1 Van Rijn R, et al. Associations between work-related factors and specific disorders at the elbow: a systematic literature review. Rheumatology (Oxford) 2009;48(5):528-36.
- ↑ Calfee R, et al. Management of lateral epicondylitis: Current concepts. J Am Acad Orthop Surg 2008; 16(1):19-29
- ↑ Van Rijn R, et al. Associations between work-related factors and specific disorders at the elbow: a systematic literature review. Rheumatology (Oxford) 2009;48(5):528-536
- ↑ 14.0 14.1 14.2 Baker C, Plancher K. Operative treatment of elbow injuries. New York: Springer, 2002.
- ↑ Nirschl R, Pettrone F. Tennis elbow. The surgical treatment of lateral epicondylitis. J Bone Joint Surg Am 1979; 61(6A):832-839
- ↑ 16.0 16.1 Cyriax J. The pathology and treatment of tennis elbow. J Bone Joint Surg 1936; 18(4): 921–940
- ↑ 17.0 17.1 Coonrad R, Hooper W. Tennis elbow: its course, natural history, conservative and surgical management. J Bone Joint Surg Am 1973; 55(6):1177-1182
- ↑ Regan W, et al. Microscopic histopathology of chronic refractory lateral epicondylitis. Am J Sports Med 1992; 20(6):746-749.
- ↑ Davenport T, et al. The EdUReP Model for Nonsurgical Management of Tendinopathy. Phys Ther 2005;85(10):1093-103
- ↑ 20.0 20.1 20.2 20.3 Warren, R. Tennis elbow (epicondylitis): epidemiology and conservative treatment. Pettrone F. AAOS Symposium and Upper Extremity Injuries in Athletes, Ed. St. Louis: C.V. Mosby, 1986; 233-243.
- ↑ Birrer R. Sport Medicine for the Primary Care Physician, CRC Press, 2002.
- ↑ Wright J. Evidence-based orthopaedics: the best answers to clinical questions. Philadelphia: Saunders Elsevier, 2008.
- ↑ 23.0 23.1 Smidt N, et al. Corticosteroid injections, physiotherapy, or a wait-and-see policy for lateral epicondylitis: a randomised controlled trial. Lancet 2002; 359: 657–62
- ↑ 24.0 24.1 Nirschl R, Ashman E. Elbow tendinopathy: tennis elbow. Clin Sports Med 2003;22(4):813-836.
- ↑ 25.0 25.1 25.2 25.3 25.4 25.5 Brukner P. Brukner & Khan's clinical sports medicine. North Ryde: McGraw-Hill; 2012.
- ↑ Rompe J, et al. Validation of the Patient-rated Tennis Elbow Evaluation Questionnaire. J Hand Ther. 2007;20(1):3-10.
- ↑ MacDermid J. The Patient-Rated Tennis Elbow Evaluation (PRTEE)© User Manual, 2007
- ↑ Mathiowetz V. Comparison of Rolyan and Jamar dynamometers for measuring grip strength. Occup Ther Int. 2002;9(3):201-209.
- ↑ Cooper G. Pocket guide to musculoskeletal diagnosis. New Jersey: Humana Press, 2006
- ↑ Bhargava A, et al. Grip strength measurements at two different wrist extension positions in chronic lateral epicondylitis-comparison of involved vs. uninvolved side in athletes and non athletes: a case-control study. Sports Med Arthrosc Rehabil Ther Technol. 2010;2:22.
- ↑ 31.0 31.1 31.2 Frydrychowicz A, et al. Hepatobiliary MR imaging with gadolinium-based contrast agents. J Magn Reson Imaging 2012; 35 (3): 492–511
- ↑ 32.0 32.1 Saroja G. et al. Diagnostic accuracy of provocative test in lateral epicondylitis. Int J Physiother Res 2014; 2(6):815-823.
- ↑ 33.0 33.1 33.2 Valdes K, LaStayo P. The value of provocative tests for the wrist and elbow: a literature review. J Hand Therapy, 2013; 26: 32-43
- ↑ Roles N, Maudsley R. Radial tunnel syndrome: Resistant tennis elbow as nerve entrapment. J Bone Joint Surg Br 1972; 54:499-508
- ↑ Portilla M, et al. The posterior interosseous nerve and the radial tunnel syndrome: an antatomical study. Int Orthop 1998; 22(2):102-106.
- ↑ Chien A, et al. Sonography and MR Imaging of Posterior Interosseous Nerve Syndrome with Surgical Correlation. Am J Roentgenol 2003; 181: 219-221.
- ↑ Bionka M, et al. Interventions for treating the posterior interosseus nerve syndrome: a systematic review of observational studies. J Peripher Nerv Syst 2006; 11(2):101-110
- ↑ Rasuli, B. Lateral epicondylitis - tennis elbow. Case study, Radiopedia.org (accessed on 13 April 2022) https://doi.org/10.53347/rlD-98132
- ↑ Johns N, Shridhar V. Lateral epicondylitis: Current concepts. AJGP 2020; 49(11):707-709.
- ↑ Evans J, et al. Clinical rating systems in elbow research - a systematic review exploring trends and distributions of use. J Shoulder Elbow Surg 2018;27:e98-106
- ↑ 41.0 41.1 Samaras P, et al. Greek physiotherapists' contemporary knowledge and practice for lateral elbow tendinopathy: an online survey. Musculoskeletal Science and Practice 2022; 57:102502
- ↑ Leung H, Yen C, Tse P. Reliability of Hong Kong Chinese version of the Patient rated Forearm Evaluation Questionnaire for lateral epicondylitis. Hong Kong Med J 2004;10:172-177.
- ↑ Newcomer K, et al. Sensitivity of the Patient-rated Forearm Evaluation Questionnaire in lateral epicondylitis. J Hand Ther 2005;18:400-406
- ↑ Overend T, et al. Reliability of a patient-rated forearm evaluation questionnaire for patients with lateral epicondylitis. J Hand Ther 1999;12:31-37
- ↑ Vicenzino B, et al. Icon 2019-International scientific tendinopathy symposium consensus:there are nine core health-related domains for tendinopathy (core domains):Delphi study of healthcare professionals and patients. Br J Sports Med 2019;54(8):444-451
- ↑ Bateman M, et al. Development of a core outcome set for lateral elbow tendinopathy (COS-LET) using best available evidence and an international consensus process. Br J Sports Med 2022;0:1-10
- ↑ Pattanittum P, et al. Non-steroidal anti-inflammatory drugs for (NSAIDs) for treating lateral elbow pain in adults. Cochrane Database Syst Rev 2013; 2013 (5): CD003686
- ↑ Heales L, et al. Evaluating the immediate effect of forearm and wrist orthoses on pain and function in individuals with lateral elbow tendinopathy: a systematic review. Musculoskeletal Science and Practice 2020; 47:102-147
- ↑ Zinger G, et al. Hyaluronic acid injections for chronic tennis elbow. BMC Sports Science, Medicine and Rehabilitation 2022; 14:1-8
- ↑ Simental-Mendia M, et al. Clinical efficacy of platelet-rich plasma in the treatment of lateral epicondylitis: a systematic review and meta-analysis of randomised placebo-controlled clinical trials. Clin Rheumatol 2020;39:2255-2265
- ↑ Houck D, et al. Treatment of lateral epicondylitis with autologous blood, platelet-rich plasma or corticosteroid injections: a systematic review of overlapping meta-analyses. Orthop J Sports Med 2019; 7(3):2325967119831052
- ↑ Sayegh E, Strauch R. Does nonsurgical treatment improve longitudinal outcomes of lateral epicondylitis over no treatment? A meta-analysis. Clin Orthop Relat Res 2015; 473(3):1093-1107.
- ↑ Bisset L, et al. Mobilisation with movement and exercise, corticosteroid injection, or wait and see for tennis elbow: randomized trial. BMJ 2006; 333(7575):939-944
- ↑ Sanders T, et al. The epidemiology and health care burden of tennis elbow: a population -based study. Am J Sports Med 2015;43:1066-1071
- ↑ Sims S, et al. Non-surgical treatment of lateral epicondylitis: a systematic review of randomized controlled trials. Hand 2014; 9(4):419-446
- ↑ Weber C, et al. Efficacy of physical therapy for the treatment of lateral epicondylitis: a meta-analysis. BMC Musculoskeletal Disord 2015;16:223
- ↑ Lapner P, et al. Non-operative treatment of lateral epicondylitis: a systematic review and meta-analysis. JSES International 2022; 6(2):321-330
- ↑ Kim Y, et al. Efficacy of non-operative treatments for lateral epicondylitis: a systematic review and meta-analysis. Plast Reconstr Surg 2021;147:112-125
- ↑ Dongni L, et al. The effect of ultrasound therapy on lateral epicondylitis. A meta-analysis. Medicine 2022 Feb; 101(8):e28822
- ↑ Hammer D, et al. Extracorporal shock wave therapy in patients with tennis elbow and painful heel. Arch Orthop Trauma Surg 2000;120(5):304-307.
- ↑ Crowther M, et al. A prospective, randomised study to compare extracorporeal shock-wave therapy and injection of steroid for the treatment of tennis elbow. J Bone Joint Surg Br 2002;84(5):678-679
- ↑ Rompe J, et al. Low-energy extracorporal shock wave therapy for persistent tennis elbow. Int Orthop. 1996;20(1):23-27
- ↑ Krischek O, et al. Shock-wave therapy for tennis and golfer’s elbow–1 year follow-up. Arch Orthop Trauma Surg 1999;119(1):62-66
- ↑ Stasinopoulos D, Johnson, M. Effectiveness of extracorporeal shock wave therapy for tennis elbow (lateral epicondylitis). Br J Sports Med 2005; 39(3): 132-136
- ↑ 65.0 65.1 65.2 65.3 65.4 65.5 Viswas R., et al. Comparison of Effectiveness of Supervised Exercise Program and Cyriax Physiotherapy in Patients with Tennis Elbow (Lateral Epicondylitis): A Randomized Clinical Trial. Scientific World Journal 2012; 2012:939645
- ↑ Mit V. et al. Cyriax Physiotherapy Versus Phonophoresis with Supervised Exercise in Subjects with LateralEpicondylalgia: A Randomized Clinical Trial, J Man Manip Ther 2009; 17(3): 171-178
- ↑ Chamberlain G. Cyriax's Friction Massage: A Review. J Orthop Sports Phys Ther 1982;4(1):16-22
- ↑ 68.0 68.1 68.2 68.3 Vicenzino B, et al. Joint Manipulation in the Management of Lateral Epicondylalgia: A Clinical Commentary. J Man Manip Ther 2007; 15(1): 50–56
- ↑ 69.0 69.1 69.2 Nagrale V, et al. Cyriax Physiotherapy Versus Phonophoresis with Supervised Exercise in Subjects with LateralEpicondylalgia: A Randomized Clinical Trial. J Man Manip Ther 2009; 17(3): 171-178
- ↑ 70.0 70.1 Stanish W, et al. Eccentric exercise in chronic tendinitis. Clin Orthop Relat Res 1986;208:65-68
- ↑ https://goo.gl/images/dG2t3E
- ↑ Mehta J, et al. Effect of Taping on Pain, Grip Strength, and Function in Deskbound Workers with Lateral Epicondylalgia World J Phys Med Rehab 2019; 1.
- ↑ Yelland M, Rabago D, Ryan M, Ng SK, Vithanachchi D, Manickaraj N, Bisset L. Prolotherapy injections and physiotherapy used singly and in combination for lateral epicondylalgia: a single-blinded randomised clinical trial. BMC musculoskeletal disorders. 2019 Dec;20(1):1-0.