Juvenile Idiopathic Arthritis
Original Editors - Emily Betz from Bellarmine University's Pathophysiology of Complex Patient Problems project.
Top Contributors - Emily Betz, Lucinda hampton, Jess Bell, Ines Musabyemariya, Admin, Naomi O'Reilly, Khloud Shreif, Kim Jackson, Elaine Lonnemann, Wendy Walker, George Prudden, WikiSysop, Meaghan Rieke and Mande Jooste
Introduction[edit | edit source]
Image 1: Swollen right knee in JIA patient Juvenile idiopathic arthritis (JIA) reflects a group of clinically heterogeneous, autoimmune disorders in children and teens under the age of 16, characterized by chronic arthritis and hallmarked by elevated levels of circulating immune complexes (CICs) and associated complement activation by-products in their sera.[1]
JIA can appear in many different ways and can range in severity. It mostly affects the joints and the surrounding tissues, although it can affect other organs like the eyes.
Symptoms of JIA include joint pain, swelling and stiffness.[2]
Etiology[edit | edit source]
The cause and trigger of chronic arthritis in JIA remain unclear.
- Abnormal immune responses triggered by the interactions between environmental factors in a genetically susceptible individual is speculative.
- JIA is not hereditary – it is not passed on from parent to child. It is rare for two children in the same family to have JIA, although this can happen[3].
- Some environmental factors such as antibiotic exposure and C-section deliveries are potential risks; however, breastfeeding and household siblings are possible protectives.[4]
Epidemiology[edit | edit source]
JIA is the most common rheumatic disease reported in children of the Western world. The incidence and prevalence are varied among 1.6 to 23 new cases for 100000 children[4].
- JIA affects 30,000 to 50,000 children in the United States.[5]
- JIA affects at least one child in every 1,000 in Australia[3]. For unknown reasons, it has been shown to be more prevalent in Norway and Australia.[6]
- Effects more than twice as many girls as their male counterparts.
- The mean age of onset is 1-3 years old.[6]
Pathology[edit | edit source]
There are several subtypes of JIA:
1.Oligoarticular JIA (Pauciarticular)
- affected ≤4 joints in the first six months of illness
- peak age: 1-6 years
- mainly affects medium and large joints
2. Polyarticular JIA (pJIA)
- ≥5 joints are affected
- peak age: 1-4 years; 7-10 years
- mainly affects small and medium joints
3. Systemic onset JIA (Still's disease, not to be confused with adult onset Still's disease)
- arthritis may present weeks to months after the onset of systemic symptoms[7]
4. Enthesitis-related JIA
5. Psoriatic JIA
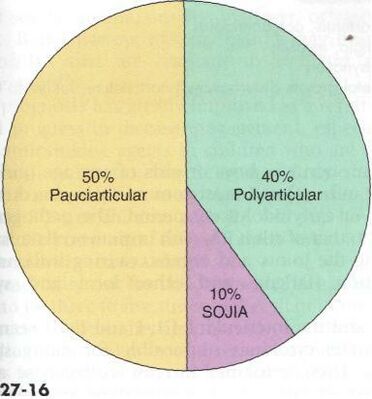
6. Undifferentiated JIA[2].Image 2: Prevalence of major subtypes of JIA[5]
Characteristics/Clinical Presentation[edit | edit source]
The symptoms the child experiences will depend on the type of arthritis they have. Common symptoms include:
- pain, swelling and stiffness in one or more joints
- skin over the affected joints may be warm or red
- mental and physical tiredness, or fatigue.
- Less common symptoms include:
- fever
- rash
- feeling generally unwell
- eye inflammation (uveitis)[2],see image 3.
Medications[edit | edit source]
An aggressive course of medications is now accepted as the standard of care for JIA. A larger factor in the symptoms management with medications is dealing with the adverse side-effects. The main goals of treatment with medications are pain control, joint preservation (mobility and function), assist in the normal growth of the child, decrease and control other systemic symptoms of JIA and in some cases the disease is prevented from progressing.[5]
The following categories of medications are currently used in the treatment of JIA[8]:
- Disease-modifying antirheumatic drugs or DMARDs - [Methotrexate:Rheumatrex; Sulfasalazine: Azulfidine] used in combination with NSAIDs, slow the progression of JIA {side effects: nausea and liver problems}
- Immunosuppressants - slow inflammation reactions {side effects: increased risk of infection and other immune threats}
- Tumor necrosis factor (TNF) inhibitors - [Etanercept:Enbrel; Infliximab: Remicade] biologic agents that help reduce pain, joint swelling and morning stiffness. {side effects: increased risk of infection and cancer}
- NSAIDs - [ibprofen:Advil, Motrin; naproxen:Aleve] reduce pain and swelling {side effects: bleeding, liver and stomach problems}
- Corticosteroids - [Prednisone] for those with severe JIA, used to control symptoms until DMARDs take effect or to prevent complications of JIA. {side effects: interfere with growth hormone, increase risk of infection}
- Analgesics - [Acetominophen, Tramadol, Codeine, Opiates] used to reduce pain when a child cannot take NSAIDs due to hypersensitivity, ulcers, liver or stomach irritations, or interactions with other drugs, the downside with analgesics they have no effect of inflammation, swelling or joint destruction. {side effects: liver problems}[6]
Diagnostic Tests/Lab Tests/Lab Values[edit | edit source]
JIA is diagnoses according to patient and family medical history, symptoms, number of joints involved, lab tests and sometimes imaging.
Juvenile idiopathic arthritis is diagnosed using a number of tests including:
- medical history
- physical examination
- blood tests – however, most children diagnosed with juvenile idiopathic arthritis do not have rheumatoid factor in their blood, so blood tests do not eliminate juvenile idiopathic arthritis
- x-rays and scans
- eye examination.[2]
Medical Management[edit | edit source]
The goal of treatment of JIA is to stop or slow the progression of inflammation, relieving symptoms (swelling, pain, stiffness), improving function (maintain full/functional ROM), and prevent further joint damage.[6] These goals are met by finding the correct combination of medications that best benefit the child.
The most common types of medications used for JIA are:
- Analgesics – for temporary pain relief
- Creams and ointments – can be rubbed into the skin over a painful joint to provide temporary pain relief
- Eye drops – to treat eye inflammation
- Non-steroidal anti-inflammatory drugs (NSAIDs) – to control inflammation and provide pain relief
- Corticosteroids – used to quickly control or reduce inflammation. They can be taken as tablets or given by injection directly into a joint, muscle or other soft tissue
- Disease modifying anti-rheumatic medications (DMARDs) – work on controlling the immune system. These medications help relieve pain and inflammation, and can also reduce or prevent joint damage
- Biologics and biosimilar medicines (bDMARDs) – are also a type of disease modifying drug. They also work on controlling the immune system. However unlike other disease modifying drugs, biologics target specific cells and proteins that are causing the inflammation and damage, rather than suppressing the entire immune system[2].
Physical Therapy Management[edit | edit source]
Physical therapy is an important part of the treatment of JIA. It is important for the child to remain active and involved in sports and activities with their peers and friends. While pain may limit the amount of activity a child can handle it is important to encourage involvement during periods or remission and allow rest and symptom reducing therapies during periods of flare-ups. Regular activity and general exercise programs help to maintain range of motion in affective joints, build and maintain strength, maintain function and can even help with symptom reduction.
Aspects that should be focused on during a physical therapy session are as follows[6]:
- Muscle tone
- Strengthening
- Range of motion
- Stretching
- Education on joint protection
- Home exercise plan
- Education on pain reducing techniques
- Muscle relaxation techniques
- Splints or orthotics maybe be beneficial to help maintain normal bone and joint growth/prevent deformities during growth[9]
Some modalities that can be used to help reduce symptoms such as pain are:
- Ultrasound
- Paraffin wax dips (hands and feet primarily)
- Moist compress (hot pack)
- Hydrotherapy (warm)
- Cold packs
Differential Diagnosis[edit | edit source]
Some signs and symptoms of JIA are shared with those of the following diseases[6][10]:
- Lyme Disease
- Rheumatic fever
- Osteomyelitis
- Psoriatic arthritis
- Inflammatory bowel disease
- Leukemia
- Caffey Disease
- Chronic Eosinophilic Granuloma
- Osteoporosis
- Involutional Osteoarthritis
Case Reports/ Case Studies[edit | edit source]
- Condon C, Gormley J, Hussey J. A review of the physical activity levels of children with juvenile arthritis. Physical Therapy Reviews [serial online]. December 2009;14(6):411-417. Available from: Academic Search Premier, Ipswich, MA.
- Hoffart C., Sherry D.. proquest.umi.com.libproxy.bellarmine.edu/pqdweb. The Journal of Musculoskeletal Medicine [serial online]. 2010;27:106-108. Available from: ProQuest Nursing & Allied Health Source. Document ID: 2096479861.
- Hutzal C, Wright F, Stephens S, Schneiderman-Walker J, Feldman B. A Qualitative Study of Fitness Instructors' Experiences Leading an Exercise Program for Children with Juvenile Idiopathic Arthritis. Physical & Occupational Therapy in Pediatrics [serial online]. November 2009;29(4):409-425. Available from: Academic Search Premier, Ipswich, MA.
- Fragala-Pinkham M, Dumas H, Barlow C, Pasternak A. An aquatic physical therapy program at a pediatric rehabilitation hospital: a case series. Pediatric Physical Therapy [serial online]. March 2009;21(1):68-78. Available from: CINAHL with Full Text, Ipswich, MA.
Resources[edit | edit source]
- National Center for Biotechnology Information, U.S. National Library of Medicine www.ncbi.nlm.nih.gov/pubmedhealth
- eMedicine from WebMD emedicine.medscape.com/
- Arthritis Foundation www.arthritis.org/
- Arthritis Today www.arthritistoday.org/
- Kids Health kidshealth.org/
- Rheumatology Image Bank images.rheumatology.org/albums.php
Clinical Trials:
- Juvenile Rheumatoid Arthritis Research Registry (Sponsored by National Institute of Arthritis and Musculoskeletal and Skin Diseases, Cincinnati Children's Hospital Medical Center, Cinncinnati, OH) clinicaltrials.gov/ct/show/NCT00090571
- Current JRA clinical trials: www.clinicaltrials.gov/ct2/results
References[edit | edit source]
see adding references tutorial.
- ↑ Moore TL. Immune complexes in juvenile idiopathic arthritis. Frontiers in immunology. 2016 May 20;7:177.Available:https://www.frontiersin.org/articles/10.3389/fimmu.2016.00177/full (accessed 18.10.2021)
- ↑ 2.0 2.1 2.2 2.3 2.4 better Health Juvenile Arthritis Available: https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/arthritis-juvenile(accessed 18.10.2021)
- ↑ 3.0 3.1 Arthritis org. JIA Available:https://www.arthritisact.org.au/juvenile-arthritis/ (accessed 18.10.2021)
- ↑ 4.0 4.1 Thatayatikom A, De Leucio A. Juvenile Idiopathic Arthritis. StatPearls [Internet]. 2020 Aug 10. Available: https://www.ncbi.nlm.nih.gov/books/NBK554605/(accessed 18.10.2021)
- ↑ 5.0 5.1 5.2 Goodman C, Fuller K. Pathology: Implications for the Physical Therapist. 3rd ed. . St. Louis, MO: Saunders, an imprint of Elsevier Inc, 2009.
- ↑ 6.0 6.1 6.2 6.3 6.4 6.5 6.6 eMedicine. Disease fact sheet: juvenile rheumatoid arthritis. http://emedicine.medscape.com/article/409980-overview (accessed 10 March 2011)
- ↑ Radiopedia JIA Available: https://radiopaedia.org/articles/juvenile-idiopathic-arthritis (accessed 18.10.2021)
- ↑ Mayo Clinic. Disease fact sheet: juvenile rheumatoid arthritis. http://www.mayoclinic.com/health/juvenile-rheumatoid-arthritis/DS00018 (accessed 10 March 2011)
- ↑ National Institute of Arthritis and Musculoskeletal and Skin Diseases. Health information: juvenile arthritis. http://www.niams.nih.gov/Health_Info/Juv_Arthritis/default.asp (accessed 10 March 2011)
- ↑ National Center for Biotechnology Information, U.S. National Library of Medicine. Disease fact sheet: http://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0001487/ (10 March 2011)
[[Category:Paediatrics]