Juvenile Idiopathic Arthritis: Difference between revisions
No edit summary |
No edit summary |
||
| Line 10: | Line 10: | ||
JIA can appear in many different ways and can range in severity. It mostly affects the joints and the surrounding tissues, although it can affect other organs like the eyes. | JIA can appear in many different ways and can range in severity. It mostly affects the joints and the surrounding tissues, although it can affect other organs like the eyes. | ||
Symptoms of JIA include joint pain, swelling and stiffness.<ref>better Health [https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/arthritis-juvenile Juvenile Arthritis] Available: https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/arthritis-juvenile<nowiki/>(accessed 18.10.2021)</ref> | Symptoms of JIA include joint pain, swelling and stiffness.<ref name=":2">better Health [https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/arthritis-juvenile Juvenile Arthritis] Available: https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/arthritis-juvenile<nowiki/>(accessed 18.10.2021)</ref> | ||
== Etiology == | == Etiology == | ||
| Line 17: | Line 17: | ||
# Abnormal [[Immune System|immune]] responses triggered by the interactions between environmental factors in a [[Genetic Conditions and Inheritance|genetically]] susceptible individual is speculative. | # Abnormal [[Immune System|immune]] responses triggered by the interactions between environmental factors in a [[Genetic Conditions and Inheritance|genetically]] susceptible individual is speculative. | ||
# JIA is not hereditary – it is not passed on from parent to child. It is rare for two children in the same family to have JIA, although this can happen<ref name=":0">Arthritis org. JIA Available:https://www.arthritisact.org.au/juvenile-arthritis/ (accessed 18.10.2021)</ref>. | # JIA is not hereditary – it is not passed on from parent to child. It is rare for two children in the same family to have JIA, although this can happen<ref name=":0">Arthritis org. JIA Available:https://www.arthritisact.org.au/juvenile-arthritis/ (accessed 18.10.2021)</ref>. | ||
# Some environmental factors such as [[Antibiotics|antibiotic]] exposure and [[Cesarean Section|C-section deliveries]] are potential risks; however, breastfeeding and household siblings are possible protectives.<ref name=":1">Thatayatikom A, De Leucio A. [https://www.ncbi.nlm.nih.gov/books/NBK554605/ Juvenile Idiopathic Arthritis]. StatPearls [Internet]. 2020 Aug 10. Available: https://www.ncbi.nlm.nih.gov/books/NBK554605/<nowiki/>(accessed 18.10.2021)</ref> | # Some environmental factors such as [[Antibiotics|antibiotic]] exposure and [[Cesarean Section|C-section deliveries]] are potential risks; however, breastfeeding and household siblings are possible protectives.<ref name=":1">Thatayatikom A, De Leucio A. [https://www.ncbi.nlm.nih.gov/books/NBK554605/ Juvenile Idiopathic Arthritis]. StatPearls [Internet]. 2020 Aug 10. Available: https://www.ncbi.nlm.nih.gov/books/NBK554605/<nowiki/>(accessed 18.10.2021)</ref> | ||
== Epidemiology == | == Epidemiology == | ||
| Line 27: | Line 27: | ||
* The mean age of onset is 1-3 years old.<ref name="eMedicine" /> | * The mean age of onset is 1-3 years old.<ref name="eMedicine" /> | ||
== Pathology == | |||
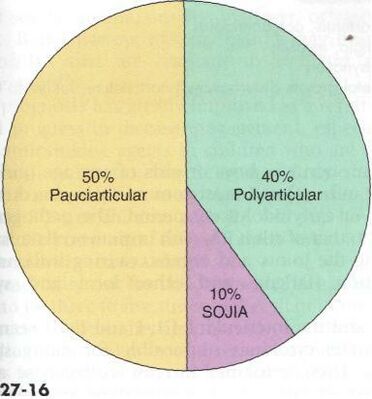
[[Image:JIA-prevalence.jpg|border|399x399px|Prevalence of subtypes of JIA|right|alt=|frameless]]There are several subtypes of JIA: | |||
1.Oligoarticular JIA (Pauciarticular) | |||
* affected ≤4 joints in the first six months of illness | |||
* peak age: 1-6 years | |||
* mainly affects medium and large joints | |||
2. Polyarticular JIA (pJIA) | |||
* ≥5 joints are affected | |||
* peak age: 1-4 years; 7-10 years | |||
* mainly affects small and medium joints | |||
3. Systemic onset JIA (Still's disease, not to be confused with adult onset Still's disease) | |||
* arthritis may present weeks to months after the onset of systemic symptoms<ref>Radiopedia [https://radiopaedia.org/articles/juvenile-idiopathic-arthritis JIA] Available: https://radiopaedia.org/articles/juvenile-idiopathic-arthritis (accessed 18.10.2021)</ref> | |||
* | |||
4. Enthesitis-related JIA | |||
5. Psoriatic JIA | |||
6. Undifferentiated JIA<ref name=":2" />.<sup></sup>'''Image 2: Prevalence of major subtypes of JIA'''<ref name="Pathology" /> | |||
== Characteristics/Clinical Presentation == | |||
The symptoms the child experiences will depend on the type of arthritis they have. Common symptoms include: | |||
* pain, swelling and stiffness in one or more joints | |||
* skin over the affected joints may be warm or red | |||
* mental and physical tiredness, or fatigue. | |||
* Less common symptoms include: | |||
* fever | |||
* rash | |||
* feeling generally unwell | |||
* eye inflammation (uveitis)<ref name=":2" />. | |||
[[Image:JIA-rash2.jpg|frame|right|http://search.creativecommons.org/?q=juvenile%20rheumatoid%20arthritis] | |||
* | |||
[[Image:JIA-swollenjoint.jpg|200x300px|http://search.creativecommons.org/?q=juvenile%20rheumatoid%20arthritis]] Swollen right knee in JIA patient [[Image:Uveitis.jpg|center]] | |||
# | |||
= | |||
* | |||
= | |||
== Associated Co-morbidities == | == Associated Co-morbidities == | ||
| Line 160: | Line 96: | ||
*Erythrocyte Sedimentation Rate (ESR or sed rate): A nonspecific marker for JIA, it is used more to rule out other conditions and to aid in determining the classification of JIA subtype. An elevated rate can indicate inflammation. In systemic JIA the sed rate will be elevated, polyarticular JIA usually results in an elevated sed rate, and the sed rate is often normal in pauciarticular JIA.<ref name="eMedicine" /> | *Erythrocyte Sedimentation Rate (ESR or sed rate): A nonspecific marker for JIA, it is used more to rule out other conditions and to aid in determining the classification of JIA subtype. An elevated rate can indicate inflammation. In systemic JIA the sed rate will be elevated, polyarticular JIA usually results in an elevated sed rate, and the sed rate is often normal in pauciarticular JIA.<ref name="eMedicine" /> | ||
*Anti-Nuclear Antibody (ANA): Detects the anti-nuclear bodies that are commonly present in those with an autoimmune disease. In pauciarticular JIA the ANA usually tests positive. In those with systemic JIA the ANA usually tests negative. ANA is more likely to test positive in diseases that could be a differential diagnosis for JIA (SLE or scleroderma) than it would in JIA. A positive ANA that is extremely elevated could indicate an increased risk of eye involvement and may indicate that JIA could progress to an adult-type SLE.<ref name="eMedicine" /><ref name="NIAMS" /> | *Anti-Nuclear Antibody (ANA): Detects the anti-nuclear bodies that are commonly present in those with an autoimmune disease. In pauciarticular JIA the ANA usually tests positive. In those with systemic JIA the ANA usually tests negative. ANA is more likely to test positive in diseases that could be a differential diagnosis for JIA (SLE or scleroderma) than it would in JIA. A positive ANA that is extremely elevated could indicate an increased risk of eye involvement and may indicate that JIA could progress to an adult-type SLE.<ref name="eMedicine" /><ref name="NIAMS">National Institute of Arthritis and Musculoskeletal and Skin Diseases. Health information: juvenile arthritis. http://www.niams.nih.gov/Health_Info/Juv_Arthritis/default.asp (accessed 10 March 2011)</ref> | ||
*Complete Blood Count (CBC): A nonspecific test for JIA. Anemia is common in children with JIA, therefore a low level of hemoglobin could be detected. White blood cells and platelets are often normal in those with JIA.<ref name="eMedicine" /> | *Complete Blood Count (CBC): A nonspecific test for JIA. Anemia is common in children with JIA, therefore a low level of hemoglobin could be detected. White blood cells and platelets are often normal in those with JIA.<ref name="eMedicine" /> | ||
*Rheumatoid Factor (RF): Though more commonly found in adults with RA, a positive RF could be found in those with polyarticular JIA. RF is usually used to aid in classification of the JIA subtype. A positive RF could indicate the JIA will progress to adult RA.<ref name="eMedicine" /> | *Rheumatoid Factor (RF): Though more commonly found in adults with RA, a positive RF could be found in those with polyarticular JIA. RF is usually used to aid in classification of the JIA subtype. A positive RF could indicate the JIA will progress to adult RA.<ref name="eMedicine" /> | ||
Revision as of 05:38, 18 October 2021
Original Editors - Emily Betz from Bellarmine University's Pathophysiology of Complex Patient Problems project.
Top Contributors - Emily Betz, Lucinda hampton, Jess Bell, Ines Musabyemariya, Admin, Naomi O'Reilly, Khloud Shreif, Kim Jackson, Elaine Lonnemann, WikiSysop, Meaghan Rieke, Mande Jooste, Wendy Walker and George Prudden
Definition/Description[edit | edit source]
Juvenile idiopathic arthritis (JIA) reflects a group of clinically heterogeneous, autoimmune disorders in children and teens under the age of 16, characterized by chronic arthritis and hallmarked by elevated levels of circulating immune complexes (CICs) and associated complement activation by-products in their sera.[1]
JIA can appear in many different ways and can range in severity. It mostly affects the joints and the surrounding tissues, although it can affect other organs like the eyes.
Symptoms of JIA include joint pain, swelling and stiffness.[2]
Etiology[edit | edit source]
The cause and trigger of chronic arthritis in JIA remain unclear.
- Abnormal immune responses triggered by the interactions between environmental factors in a genetically susceptible individual is speculative.
- JIA is not hereditary – it is not passed on from parent to child. It is rare for two children in the same family to have JIA, although this can happen[3].
- Some environmental factors such as antibiotic exposure and C-section deliveries are potential risks; however, breastfeeding and household siblings are possible protectives.[4]
Epidemiology[edit | edit source]
JIA is the most common rheumatic disease reported in children of the Western world. The incidence and prevalence are varied among 1.6 to 23 new cases for 100000 children[4].
- JIA affects 30,000 to 50,000 children in the United States.[5]
- JIA affects at least one child in every 1,000 in Australia[3]. For unknown reasons, it has been shown to be more prevalent in Norway and Australia.[6]
- Effects more than twice as many girls as their male counterparts.
- The mean age of onset is 1-3 years old.[6]
Pathology[edit | edit source]
There are several subtypes of JIA:
1.Oligoarticular JIA (Pauciarticular)
- affected ≤4 joints in the first six months of illness
- peak age: 1-6 years
- mainly affects medium and large joints
2. Polyarticular JIA (pJIA)
- ≥5 joints are affected
- peak age: 1-4 years; 7-10 years
- mainly affects small and medium joints
3. Systemic onset JIA (Still's disease, not to be confused with adult onset Still's disease)
- arthritis may present weeks to months after the onset of systemic symptoms[7]
4. Enthesitis-related JIA
5. Psoriatic JIA
6. Undifferentiated JIA[2].Image 2: Prevalence of major subtypes of JIA[5]
Characteristics/Clinical Presentation[edit | edit source]
The symptoms the child experiences will depend on the type of arthritis they have. Common symptoms include:
- pain, swelling and stiffness in one or more joints
- skin over the affected joints may be warm or red
- mental and physical tiredness, or fatigue.
- Less common symptoms include:
- fever
- rash
- feeling generally unwell
- eye inflammation (uveitis)[2].
[[Image:JIA-rash2.jpg|frame|right|http://search.creativecommons.org/?q=juvenile%20rheumatoid%20arthritis]
http://search.creativecommons.org/?q=juvenile%20rheumatoid%20arthritis Swollen right knee in JIA patient
Associated Co-morbidities[edit | edit source]
See each subtype of JIA above.
Medications[edit | edit source]
An aggressive course of medications is now accepted as the standard of care for JIA. A larger factor in the symptoms management with medications is dealing with the adverse side-effects. The main goals of treatment with medications are pain control, joint preservation (mobility and function), assist in the normal growth of the child, decrease and control other systemic symptoms of JIA and in some cases the disease is prevented from progressing.[5]
The following categories of medications are currently used in the treatment of JIA[8]:
- Disease-modifying antirheumatic drugs or DMARDs - [Methotrexate:Rheumatrex; Sulfasalazine: Azulfidine] used in combination with NSAIDs, slow the progression of JIA {side effects: nausea and liver problems}
- Immunosuppressants - slow inflammation reactions {side effects: increased risk of infection and other immune threats}
- Tumor necrosis factor (TNF) inhibitors - [Etanercept:Enbrel; Infliximab: Remicade] biologic agents that help reduce pain, joint swelling and morning stiffness. {side effects: increased risk of infection and cancer}
- NSAIDs - [ibprofen:Advil, Motrin; naproxen:Aleve] reduce pain and swelling {side effects: bleeding, liver and stomach problems}
- Corticosteroids - [Prednisone] for those with severe JIA, used to control symptoms until DMARDs take effect or to prevent complications of JIA. {side effects: interfere with growth hormone, increase risk of infection}
- Analgesics - [Acetominophen, Tramadol, Codeine, Opiates] used to reduce pain when a child cannot take NSAIDs due to hypersensitivity, ulcers, liver or stomach irritations, or interactions with other drugs, the downside with analgesics they have no effect of inflammation, swelling or joint destruction. {side effects: liver problems}[6]
Diagnostic Tests/Lab Tests/Lab Values[edit | edit source]
JIA is diagnoses according to patient and family medical history, symptoms, number of joints involved, lab tests and sometimes imaging.
Lab Tests:
- Erythrocyte Sedimentation Rate (ESR or sed rate): A nonspecific marker for JIA, it is used more to rule out other conditions and to aid in determining the classification of JIA subtype. An elevated rate can indicate inflammation. In systemic JIA the sed rate will be elevated, polyarticular JIA usually results in an elevated sed rate, and the sed rate is often normal in pauciarticular JIA.[6]
- Anti-Nuclear Antibody (ANA): Detects the anti-nuclear bodies that are commonly present in those with an autoimmune disease. In pauciarticular JIA the ANA usually tests positive. In those with systemic JIA the ANA usually tests negative. ANA is more likely to test positive in diseases that could be a differential diagnosis for JIA (SLE or scleroderma) than it would in JIA. A positive ANA that is extremely elevated could indicate an increased risk of eye involvement and may indicate that JIA could progress to an adult-type SLE.[6][9]
- Complete Blood Count (CBC): A nonspecific test for JIA. Anemia is common in children with JIA, therefore a low level of hemoglobin could be detected. White blood cells and platelets are often normal in those with JIA.[6]
- Rheumatoid Factor (RF): Though more commonly found in adults with RA, a positive RF could be found in those with polyarticular JIA. RF is usually used to aid in classification of the JIA subtype. A positive RF could indicate the JIA will progress to adult RA.[6]
- Anti-Cyclic Citrullinated Peptide (anti-CCP) Antibodies: Can be detected in healthy individuals before the onset of RA, and can predict the development of undifferentiated arthritis into rheumatoid arthritis.[9]
Imaging: Though imaging is nonspecific for testing for JIA it can show damage to the joint, fractures, tumors, infection and/or congenital defects all in which would help to narrow down or rule out diseases with similar signs and symptoms.
- X-rays
- Bone scan
- MRI
- CT scan
- Duel-Energy X-Ray Absorptiometry (DEXA)
Other Tests:
- Arthrocentesis: Often known as joint aspiration. Removing and testing the synovial fluid of affected joints can be used to rule out infection and aid in identifying the cause of the arthritis. [6][8]
- Synovial Biopsy: Removal of a small portion of the synovial tissue from the affected joint can aid in determining the cause of the inflammation and synovial damage.[6]
Etiology/Causes[edit | edit source]
Etiology is largely unknown. Some evidence supports environmental triggers, viral or bacterial infections or genetic predisposition. With further research there are hopes of identifying molecular biomarkers to aid in the diagnosis and treatment of JIA.[5]
The disease is accepted to be an autoimmune disease, which means that the body's immune system attacks it's own tissue, instead of foreign tissues. In JIA the body's immune cells and autoanitbodies attack the synovium. As a reaction to the attack the synovium becomes inflamed and irritated. This reaction causes the synovium to thicken and grow abnormally, this abnormal growth eventually will cause damage to the bone and cartilage of the joint and surrounding tissues.[6]
Researchers are beginning to believe that not all forms of JIA are autoimmune. Systemic JIA is now being more accurately defines at an autoinflammatory disease as opposed to autoimmune. This means that while the body's immune system is still over active, like in autoimmune diseases, the inflammation and immune activity is not caused by autoantibodies but rather by a different part of the immune system that when working properly should cause white blood cells to destroy harmful invaders. When this system is not working properly it causes inflammation, fever and rash for unknown reasons.[9]
Systemic Involvement[edit | edit source]
See each subtype of JIA above.
Medical Management (current best evidence)[edit | edit source]
The goal of treatment of JIA is to stop or slow the progression of inflammation, relieving symptoms (swelling, pain, stiffness), improving function (maintain full/functional ROM), and prevent further joint damage.[6] These goals are met by finding the correct combination of medications (listed above) that best benefit the child.
JIA should be followed by a rheumatologist (ideally a pediatric rheumatologist) or a family practice physician. A team approach is best when treating children with JIA, a team could include any combination of the following healthcare professionals:[9]
- Rheumatologist, pediatric rheumatologist - manage the progression of JIA and develop the correct medical treatment plan specific to the child
- Pediatrician or family practice physician - monitor the patient's health over all
- Physical therapist - maintain joint function and strength, teach joint protection, energy conservation, minimize muscle pain
- Occupational therapist - help with joint protection, energy conservation, maintain upper extremity (hands) function
- Ophthalmologist - monitor possible eye complications that can accompany JIA and/or are side effects from medications
- Dentist and orthodontist - help to monitor jaw involvement, and aid in oral care due to possible limitations of hand function secondary to JIA
- Counselor or psychologist - aid the child and family in keeping their feelings about the disease and its treatment "sorted out"
- Orthopedic surgeon - in the event that surgery is necessary during the treatment course of JIA
- Dietician - it is important for children with JIA to maintain a healthy weight to ease some of the burden on weight bearing joints. It is also important to ensure the child has a balanced diet with all essential nutrients
- Pharmacist - another level to ensure that the medications prescribed for the treatment of JIA and any other medications the child might be taking do not potentially negatively interact with each other and/or food the child might consume
- Social worker - may help the child and the family to identify helpful resources for the treatment of JIA
- Rheumatology nurse - serve as a way-lay between the doctor and patient in between office visits
- School nurse - help the child manage the disease while at school, if school-age
In addition to medications to treat JIA other symptom reducers include:
- Hot or cold packs
- Warm baths or showers
- Gentle ROM
- Staying active to maintain function and ROM, a great form of exercise is swimming because it is low impact and does not require repetitive stress to load bearing joints
- Maintaining a healthy weight is extremely important to reduce the stress of weight bearing joints
- Physical therapy treatments
- Relaxation techniques for releasing muscle tension[6]
Physical Therapy Management (current best evidence)[edit | edit source]
Physical therapy is an important part of the treatment of JIA. It is important for the child to remain active and involved in sports and activities with their peers and friends. While pain may limit the amount of activity a child can handle it is important to encourage involvement during periods or remission and allow rest and symptom reducing therapies during periods of flare-ups. Regular activity and general exercise programs help to maintain range of motion in affective joints, build and maintain strength, maintain function and can even help with symptom reduction.
Aspects that should be focused on during a physical therapy session are as follows[6]:
- Muscle tone
- Strengthening
- Range of motion
- Stretching
- Education on joint protection
- Home exercise plan
- Education on pain reducing techniques
- Muscle relaxation techniques
- Splints or orthotics maybe be beneficial to help maintain normal bone and joint growth/prevent deformities during growth[9]
Some modalities that can be used to help reduce symptoms such as pain are:
- Ultrasound
- Paraffin wax dips (hands and feet primarily)
- Moist compress (hot pack)
- Hydrotherapy (warm)
- Cold packs
Preferred Practice Patterns[5]:[edit | edit source]
Juvenile Idiopathic (Rheumatoid) Arthritis[edit | edit source]
- 4A: Primary Prevention/Risk Reduction for Skeletal Demineralization (low bone density)
- 4E: Impaired Joint Mobility, Motor Function, Muscle Performance, and Range of Motion Associated with Localized Inflammation
- 5B: Impaired Neuromotor Development
Adult Rheumatoid Arthritis[edit | edit source]
- 4A
- 4B: Impaired Posture (cervical involvement)
- 4C: Impaired Muscle Performance
- 4D: Impaired Joint Mobility, Motor Function, Muscle Performance, and Range of Motion Associated with Connective Tissue Dysfunction
- 4H: Impaired Joint Mobility, Motor Function, Muscle Performance, and Range of Motion Associated with Joint Arthroplasty
- 4I: Impaired Joint Mobility, Motor Function, Muscle Performance, and Range of Motion Associated with Bony or Soft Tissue Surgery ( tenosynovectomy, tendon reconstruction)
- 5H: Impaired Motor Function, Peripheral Nerve Integrity, and Sensory Integrity Associate with Nonprogressive Disorders of the Spinal Cord (cervical spine)
- 6B: Impaired Aerobic Capacity/Endurance Associated with Deconditioning
Differential Diagnosis[edit | edit source]
Some signs and symptoms of JIA are shared with those of the following diseases[6][10]:
- Lyme Disease
- Rheumatic fever
- Osteomyelitis
- Psoriatic arthritis
- Inflammatory bowel disease
- Leukemia
- Caffey Disease
- Chronic Eosinophilic Granuloma
- Osteoporosis
- Involutional Osteoarthritis
Case Reports/ Case Studies[edit | edit source]
- Condon C, Gormley J, Hussey J. A review of the physical activity levels of children with juvenile arthritis. Physical Therapy Reviews [serial online]. December 2009;14(6):411-417. Available from: Academic Search Premier, Ipswich, MA.
- Hoffart C., Sherry D.. proquest.umi.com.libproxy.bellarmine.edu/pqdweb. The Journal of Musculoskeletal Medicine [serial online]. 2010;27:106-108. Available from: ProQuest Nursing & Allied Health Source. Document ID: 2096479861.
- Hutzal C, Wright F, Stephens S, Schneiderman-Walker J, Feldman B. A Qualitative Study of Fitness Instructors' Experiences Leading an Exercise Program for Children with Juvenile Idiopathic Arthritis. Physical & Occupational Therapy in Pediatrics [serial online]. November 2009;29(4):409-425. Available from: Academic Search Premier, Ipswich, MA.
- Fragala-Pinkham M, Dumas H, Barlow C, Pasternak A. An aquatic physical therapy program at a pediatric rehabilitation hospital: a case series. Pediatric Physical Therapy [serial online]. March 2009;21(1):68-78. Available from: CINAHL with Full Text, Ipswich, MA.
Resources[edit | edit source]
- National Center for Biotechnology Information, U.S. National Library of Medicine www.ncbi.nlm.nih.gov/pubmedhealth
- eMedicine from WebMD emedicine.medscape.com/
- Arthritis Foundation www.arthritis.org/
- Arthritis Today www.arthritistoday.org/
- Kids Health kidshealth.org/
- Rheumatology Image Bank images.rheumatology.org/albums.php
Clinical Trials:
- Juvenile Rheumatoid Arthritis Research Registry (Sponsored by National Institute of Arthritis and Musculoskeletal and Skin Diseases, Cincinnati Children's Hospital Medical Center, Cinncinnati, OH) clinicaltrials.gov/ct/show/NCT00090571
- Current JRA clinical trials: www.clinicaltrials.gov/ct2/results
References[edit | edit source]
see adding references tutorial.
- ↑ Moore TL. Immune complexes in juvenile idiopathic arthritis. Frontiers in immunology. 2016 May 20;7:177.Available:https://www.frontiersin.org/articles/10.3389/fimmu.2016.00177/full (accessed 18.10.2021)
- ↑ 2.0 2.1 2.2 better Health Juvenile Arthritis Available: https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/arthritis-juvenile(accessed 18.10.2021)
- ↑ 3.0 3.1 Arthritis org. JIA Available:https://www.arthritisact.org.au/juvenile-arthritis/ (accessed 18.10.2021)
- ↑ 4.0 4.1 Thatayatikom A, De Leucio A. Juvenile Idiopathic Arthritis. StatPearls [Internet]. 2020 Aug 10. Available: https://www.ncbi.nlm.nih.gov/books/NBK554605/(accessed 18.10.2021)
- ↑ 5.0 5.1 5.2 5.3 5.4 Goodman C, Fuller K. Pathology: Implications for the Physical Therapist. 3rd ed. . St. Louis, MO: Saunders, an imprint of Elsevier Inc, 2009.
- ↑ 6.00 6.01 6.02 6.03 6.04 6.05 6.06 6.07 6.08 6.09 6.10 6.11 6.12 6.13 6.14 eMedicine. Disease fact sheet: juvenile rheumatoid arthritis. http://emedicine.medscape.com/article/409980-overview (accessed 10 March 2011)
- ↑ Radiopedia JIA Available: https://radiopaedia.org/articles/juvenile-idiopathic-arthritis (accessed 18.10.2021)
- ↑ 8.0 8.1 Mayo Clinic. Disease fact sheet: juvenile rheumatoid arthritis. http://www.mayoclinic.com/health/juvenile-rheumatoid-arthritis/DS00018 (accessed 10 March 2011)
- ↑ 9.0 9.1 9.2 9.3 9.4 National Institute of Arthritis and Musculoskeletal and Skin Diseases. Health information: juvenile arthritis. http://www.niams.nih.gov/Health_Info/Juv_Arthritis/default.asp (accessed 10 March 2011)
- ↑ National Center for Biotechnology Information, U.S. National Library of Medicine. Disease fact sheet: http://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0001487/ (10 March 2011)
[[Category:Paediatrics]