Hypothyroidism
Original Editors - Beth Lee from Bellarmine University's Pathophysiology of Complex Patient Problems project.
Top Contributors - Beth Lee, Admin, Kim Jackson, Lucinda hampton, Dave Pariser, Candace Goh, 127.0.0.1, Elaine Lonnemann, Wendy Walker and WikiSysop
Introduction[edit | edit source]
Hypothyroidism results from low levels of thyroid hormone. It has varied etiology and manifestations. The thyroid gland secretes thyroid hormones and is essential for multiple metabolic functions for many organ systems. Hypothyroidism is treated with with levothyroxine, left untreated hypothyroidism leads to ill health and possibly death.[1]
Etiology[edit | edit source]
Iodine deficiency is the most common cause of hypothyroidism worldwide. In iodine sufficient countries however, like Australia and USA, autoimmune thyroid diseases is the most common aetiology.[2]
Other typical causes of hypothyroidism include: drugs (eg amiodarone and lithium); thyroid radioactive iodine therapy or thyroid surgery; radiotherapy to head or neck area; central hypothyroidism from neoplastic, infiltrative, inflammatory, or iatrogenic disorders of the pituitary or hypothalamus.[1]
Epidemiolgy[edit | edit source]
Hypothyroidism is more prevalent in women who have a four to ten times greater likelihood of developing this than men. Hypothyroidism can be present at birth, but has a higher occurrence rate between the ages of 30 and 60. It occurs in close to 10% of women and 6% of men over the age of 65. Primary Hypothyroidism is more common than secondary with approximately 95% of all people diagnosed categorized as the primary type. [3][4][5]
Clinical Presentation[edit | edit source]
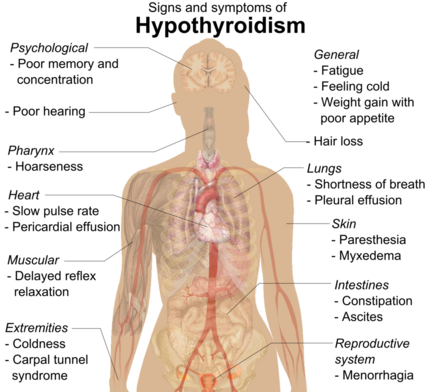
Clinical signs are widespread and affect numerous body systems. With early onset of the disease, signs may be indistinct and go undetected such as general fatigue, slight weight gain from fluid retention and decreased metabolism, dry skin, or cold sensitivity.
- Elderly patients have significantly fewer symptoms than do younger adults, and complaints are often subtle. Many elderly patients with hypothyroidism present with nonspecific geriatric symptoms like confusion, falling, incontinence, and decreased mobility.
- With progression, clinical signs become more obvious and severe. Myxedema usually appears in the later stages if not treated resulting in nonpitting edema present around the eyes, hands, and feet. Myxedema may also cause thickening of the tongue and tissues of the larynx and pharynx, slurred speech and hoarseness.
- Rarely, a goiter may be present if not medically treated and presents as a large swelling on the anterior neck resulting from marked thyroid gland growth.. [7][4][5][8]
- Symptoms of depression, anxiety, psychosis, cognitive impairments (eg memory loss) can be present.[1]
Below is a picture of Myxedema of the hands and legs and a man before and after treatment for Myxedema[9]:
Image:Myxedema_2.jpg File:Myxedema.jpg
Medical Management[edit | edit source]
Hypothyroidism is mainly treated with levothyroxine monotherapy. The hormone replacement is started at a low dose and then is gradually increased until a proper level is achieved and maintained. This is especially true for the elderly population who may have heart comorbidities because this drug therapy can create temporary levels of hyperthyroidism for several hours and increases the risk for cardiac events.
- Advise patients that treatment for hypothyroidism is lifelong.
- Clients take medications 30-60 minutes before the first meal of the day.[1]
Diagnostic Tests/Lab Tests/Lab Values[edit | edit source]
When the body senses that there is a decreased amount of thyroid hormone being produced the anterior pituitary gland increases the amount of thyroid-stimulating hormone (TSH) being released in an effort to promote thyroid hormone production. With Hypothyroidism, the thyroid gland does not respond properly to the TSH so the pituitary gland continues to increase its secretion causing elevated levels of TSH to be present in the blood.
Elevated TSH levels found in the blood are used most often to diagnose Hypothyroidism because it is the most sensitive indication of the disorder. TSH levels are always elevated in Primary Hypothyroidism. In severe cases T4 hormone levels may be decreased in the blood. T3 levels are typically close to normal in most cases. Cholesterol and triglyceride levels may also be elevated. [7][4][5][8]
Physical Therapy Management[edit | edit source]
Preferred Practice Patterns for Physical Therapy:
- Impaired Muscle Performance
- Impaired Joint Mobility, Motor Function, Muscle Performance, and Range of Motion Associated with Connective Tissue Dysfunction.
- Impaired Joint Mobility, Motor Function, Muscle Performance and Range of Motion Associated with Localized Inflammation.
- Impaired Joint Mobility, Motor Function, Muscle Performance, Range of Motion and Reflex Integrity Associated with Spinal Disorders
- Impaired Aerobic Capacity/Endurance Associated with Deconditioning.
- Primary Prevention/Risk Reduction for Integumentary Disorders.
When myedematous hypothyroidism is treated it may cause the patient to develop pseudogout in the joints and may affect the spine as well. Pseudogout may cause crystals to be deposited into the ligamentum flavum and OA ligament causing spinal stenosis and other neurologic issues. The physical therapist’s role is like that when treating rheumatoid arthritis. The patient may have complaints of muscle aches, pain, or stiffness and may cause the development of trigger points. This will require hormone therapy to resolve the symptoms and cannot be helped with simple myofascial release.
The therapist working with a patient with hypothyroidism in the acute care setting must be aware that dry, edematous skin is prone to breakdown or tears. Prevention may be a key goal for the therapist to keep in mind and should work to monitor and relieve pressure points on the sacrum, coccyx, elbows and heels whenever necessary.
The therapist working in the outpatient setting must be aware that patients with hypothyroidism present with a multitude of varying symptoms that mimic musculoskeletal or neural disorders. When treating a patient with widespread muscle weakness, general fatigue, widespread trigger points, or overall decreased deep tendon reflexes it is important to take an in-depth history so that all symptoms can be reported, because the patient may not be able to connect symptoms to one another. Also, in cases of patient reported carpal tunnel it is important to get a thorough history to understand if the mechanism of injury is truly related to causes treatable by the therapist such as ergonomics or if the patient needs to be referred on so that the underlying issue may be resolved.
Developing an exercise program for a patient with Hypothyroidism can be helpful in many ways. First, it helps to rebuild activity tolerance, increase muscle strength, and reduce apathy secondary to the decreased metabolism caused by the disorder. Exercise to help correct such problems should only be implemented once the patient has begun hormone replacement therapy, otherwise the issues cannot be resolved. Increasing the patient’s exercise tolerance can also be extremely helpful for patients who are severely constipated from the disorder. It helps increase the peristaltic activity and overall metabolism. Also, because many patients with hypothyroidism have co morbid heart conditions, increasing aerobic activity can have benefits on the cardiovascular health of the patient and reduce risk factors for cardiac events. [7][11][8]
Differential Diagnosis[edit | edit source]
- Polymyalgia Rheumatica
- Polymyositis
- Dementia
- Depression
- Parkinson’s disease
- Fibromyalgia
- Diabetes
- Carpal Tunnel Syndrome
- Menopause
- Congestive Heart Failure
- Anemia
- Infectious Mononucleosis
- De Quervain Syndrome
- Hyperlipidemia
- Stress
- Euthyroid Sick Syndrome
- Amyloidosis
- Myalgic Encephalomyelitis or Chronic Fatigue Syndrome
Case Reports[edit | edit source]
- A case study of a 15 year old girl who was diagnosed with a rare triad of primary amenorrhea, hypothyroidism, and Addison disease : An Unusual Cause of Primary Amenorrhea[12]
- Hypothyroidism can be linked to Sleep Apnea. A case study was done on an 84 year old woman with a history of hypothyroidism: Case Study: Obstructive Sleep Apnea[13]
- A case study of a woman who was diagnosed with hypothyroidism in her mid-twenties and now ten years later is pregnant with her first child: Case Study: Management of Hypothyroidism during Pregnancy[14]
- A case study presented to show how to deal with newly diagnosed hypothyroid patients: Newly Diagnosed Hypothyroidism[15]
- A case study presented about a 78 year old being treated for 6 chronic conditions including Hypothyroidism: Rehabilitation of a Functionally Limited, Chronically Ill Older Adult: A Case Study[16]
- A case report about a 74 year old woman that presented with increasing abdominal swelling over four months: Hypothyroidism Mimicking Intra-abdominal Malignancy [17]
- A case report about how acquired ataxia has been described with hypothyroidism and is typically reversible by thyroid hormone replacement therapy: Ataxia associated with Hashimoto's disease: Progressive non-familial adult onset cerebellar degeneration with autoimmune thyroiditis[18]
Resources[edit | edit source]
American Thyroid Association: http://thyroid.org
Clinical Thyroidology for Patients: http://thyroid.org/patients/ct/index.html
Thyroid Foundation of Canada: www.thyroid.ca
American Association of Clinical Endocrinologists: www.aace.com
Clinical Center, National Institutes of Health: www.cc.nih.gov
Hormone Foundation: www.hormone.org
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 Patil N, Rehman A, Jialal I, Saathoff AD. Hypothyroidism (Nursing). Available:https://www.ncbi.nlm.nih.gov/books/NBK568746/ (accessed 13.1.2023)
- ↑ Topliss DJ, Eastman CJ. 5: Diagnosis and management of hyperthyroidism and hypothyroidism. Medical journal of Australia. 2004 Feb 16;180(4):186-94.Available:https://pubmed.ncbi.nlm.nih.gov/14960142/ (accessed 13.1.2023)
- ↑ Goodman C, Snyder T. Differential Diagnosis for Physical Therapists: Screening for Referral. St. Louis, Missouri: Saunders Elsevier, 2007.
- ↑ 4.0 4.1 4.2 4.3 Goodman C, Fuller K. Pathology: Implications for the Physical Therapist. St. Louis, Missouri: Saunders Elsevier; 2009.
- ↑ 5.0 5.1 5.2 5.3 Porter R, Hypothyroidism. The Merck Manual Online Medical Library. 2008. Available at: http://www.merck.com/mmpe/index.html . Accessed February 17, 2010.
- ↑ Hypothyroidism:What is it, Causes, Symptoms and Treatments. Available from: https://www.youtube.com/watch?v=h9WIzDa9big [last accessed 29/12/19]
- ↑ 7.0 7.1 7.2 7.3 Goodman C, Snyder T. Differential Diagnosis for Physical Therapists: Screening for Referral. St. Louis, Missouri: Saunders Elsevier, 2007.
- ↑ 8.0 8.1 8.2 8.3 Allahabadia A., Razvi S., Abraham P., Franklyn . Diagnosis and treatment of primary hypothyroidism. British Medical Journal (International Edition) [serial online]. 2009;338:1090. Available from: Health Module. Accessed February 19, 2010, Document ID: 1731734701.
- ↑ Types of Hypothyroidism. Available at: http://www.type2hypothyroidism.com/Type1VsType2.html. Accessed February 17. 2010.
- ↑ Secondary Hypothyroidism. Available from: https://www.youtube.com/watch?v=zj1UZKtWgFM [last accessed 29/12/19]
- ↑ Vaidya B., Pearce S.. Management of hypothyroidism in adults. British Medical Journal (International Edition) [serial online]. 2008;337:284. Available from: Health Module. Accessed February 19, 2010, Document ID: 1542959701.
- ↑ Persson E., Chapados I.. An Unusual Cause of Primary Amenorrhea. Clinical Pediatrics [serial online]. 2008;47:309. Available from: Health Module. Accessed February 19, 2010, Document ID: 1455542621.
- ↑ Berry D.. Case Study: Obstructive Sleep Apnea. Medsurg Nursing [serial online]. 2008;17:11-6; quiz 17. Available from: ProQuest Medical Library. Accessed February 19, 2010, Document ID: 1474547051
- ↑ Tammy J Bungard, Mary Hurlburt. Management of hypothyroidism during pregnancy. Canadian Medical Association. Journal [serial online]. 2007;176:1077-8. Available from: ProQuest Medical Library. Accessed February 19, 2010, Document ID: 1260001101.
- ↑ H U Rehman, T A Bajwa. Newly diagnosed hypothyroidism. British Medical Journal (International Edition) [serial online]. 2004;329:1271. Available from: Health Module. Accessed February 19, 2010, Document ID: 758626471.
- ↑ Robert Topp, Jessica Sobolewski, Debra Boardley, Amy L Morgan, et al. Rehabilitation of a functionally limited, chronically ill older adult: A case study. Rehabilitation Nursing [serial online]. 2003;28:154-8. Available from: ProQuest Medical Library. Accessed February 19, 2010, Document ID: 417139371.
- ↑ S T M Krishnan, Z Philipose, G Rayman. Hypothyroidism mimicking intra-abdominal malignancy. British Medical Journal (International Edition) [serial online]. 2002;325:946-7. Available from: Health Module. Accessed February 19, 2010, Document ID: 234072331.
- ↑ M Selim, D A Drachman. Ataxia associated with Hashimoto's disease: Progressive non-familial adult onset cerebellar degeneration with autoimmune thyroiditis. Journal of Neurology, Neurosurgery and Psychiatry [serial online]. 2001;71:81-7. Available from: ProQuest Medical Library. Accessed February 19, 2010, Document ID: 75203187.