Glasgow Coma Scale
Original Editor - Your name will be added here if you created the original content for this page.
Top Contributors - Megan Craig, Kendyl Wilson, Emily Lingerfelt, Kim Jackson, Jillian Burton, Vidya Acharya, Abbey Wright, Evan Thomas, Naomi O'Reilly, WikiSysop, Simisola Ajeyalemi, Adam Vallely Farrell, Karen Wilson, Claire Knott, Nicole Hills, Admin, Lucinda hampton, Stacy Schiurring and Tarina van der Stockt
Objective
[edit | edit source]
The Glasgow Coma Scale (GCS) was first created by Graham Teasdale and Bryan Jennett in 1974. It is a clinical scale to assess a patient’s “depth and duration of impaired consciousness and coma”[1] following an acute brain injury. Healthcare practitioners can monitor the motor responsiveness, verbal performance, and eye opening of the patient in the form of a simple chart. The GCS is the most commonly used tool internationally for this assessment and has been translated into 30 languages. It should not, however, be confused with the Glasgow Outcome Scale (GOS), which evaluates persistent disability after brain damage. [2]
Intended Population
[edit | edit source]
Method of Use[edit | edit source]
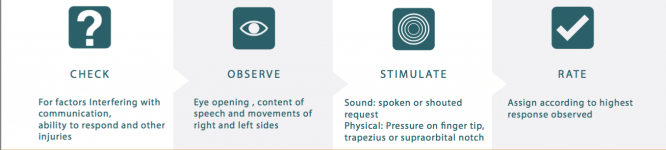
The GCS Assessment Aid has four steps to the assessment process: Check, observe, stimulate, rate.[3]
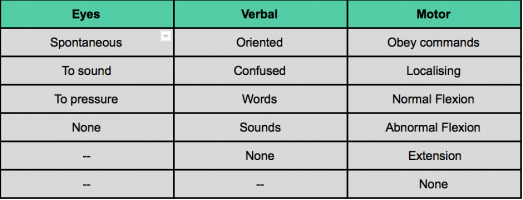
The assessor should evaluate each of the subscales as listed in the Assessment Aid. Each subscale has several components (different quantity for each subscale). Based on what the patient is able to do on assessment, they are assigned a rating. The rating is matched with a score. A higher score indicates a greater level of consciousness.
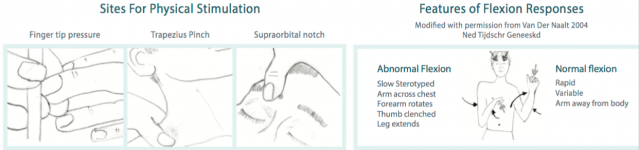
Three sites for stimulation are used. These include finger tip pressure, trapezius pinch and supraorbital notch. When stimulating these areas, health care practitioners should look for one of two responses: an abnormal flexion response or a normal flexion response.[3]
The National Institute for Health Care and Excellence (NICE) published clinical guidelines on Head injuries for assessment and early management. NICE recommends the following clinical guidelines:
- Until a patient has achieved a score of 15 on the GCS, patients should be observed every half hour.
- Once GCS score has reached 15, the patient should be re-assessed using the GCS every half hour for two consecutive hours.
- If the patient's GCS score remains above 15, the patient should be then observed once every hour for four hours and then every 2 hours after that.
Note: If a patient's’ GCS score drops below 15, the health care practitioners should revert to observing the patient every half hour.[4]
The Institute of Neurological Sciences NHS Greater Glasgow and Clyde created a YouTube Video to demonstrate how to properly use the outcome measure.
Reference
[edit | edit source]
Evidence[edit | edit source]
Reliability[edit | edit source]
The inter-rater reliabilty of the total Glasgow Coma Scale is p=0.86. Some research has subdivided the inter-rater reliabiltiy for each subscale. For the eye score the inter-rater reliability is p=0.76, the verbal score is p=0.67, and the motor score is p=0.81 [6] The research for test-retest reliability is not recent and should be updated, however the best available evidence is k=0.66-0.77 [7]
Validity[edit | edit source]
The validity of the glascow coma scale comes under fire because a lot of hospitals administer the test while patients have been sedated, often underestimating patient scores. It’s also difficult to elicit accurate scores when patients are intubated.[8] Recent research has refuted that intubation elicits significantly different survival rates with the verbal score of r=0.90 and the total score r=0.97[9] The motor score is consistently the most predictive component of the GCS[10]
Responsiveness[edit | edit source]
Given the current best available evidence, the GCS has a low sensitivity (56.1%) and a high specificity (82.2%). Therefore there are very few false positives predicting a low rate of survival in healthy individuals.[11]
Miscellaneous
[edit | edit source]
Links[edit | edit source]
Recent Related Research (from Pubmed)[edit | edit source]
Extension:RSS -- Error: Not a valid URL: feed://https://eutils.ncbi.nlm.nih.gov/entrez/eutils/erss.cgi?rss_guid=1vwc2FOtmnQ43rSLIG_ltX_vb362uUeFuFNJ9qEArduwwdiYz9%7Ccharset=UTF-8%7Cshort%7Cmax=10
References[edit | edit source]
References will automatically be added here, see adding references tutorial.
- ↑ Teasdale G, Jennett B. Assessment of coma and impaired consciousness: a practical scale. The Lancet. 1974 Jul 13;304(7872):81-4.
- ↑ Frej M, Frej J. The Glasgow Structured Approach to Assessment of the Glasgow Coma Scale [Internet]. What is GCS - Glasgow Coma Scale. Sir Graham Teasdale; [cited 2017May7]. Available from: http://www.glasgowcomascale.org/what-is-gcs/
- ↑ 3.0 3.1 Institute of Neurological Sciences NHS Greater Glasgow and Clyde. Glasgow Coma Scale: Do it this way [Internet]. Sir Graham Teasdale; 2015 [cited 2017 May 7]. Available from: http://www.glasgowcomascale.org/downloads/GCS-Assessment-Aid-English.pdf?v=3
- ↑ Head injury: Assessment and early management [Internet]. National Institute for Health and Care Excellence; 2014 [cited 7 May 2017]. Available from: https://www.nice.org.uk/guidance/cg176/resources/head-injury-assessment-and-early-management-pdf-35109755592901
- ↑ GCS at 40. Glasgow Coma Scale at 40 | The new approach to Glasgow Coma Scale assessment. Available from: https://www.youtube.com/watch?v=v6qpEQxJQO4 [last accessed 05/07/17
- ↑ Gill M, Reiley D, Green S. Interrater reliability of Glasgow Coma Scale scores in the emergency department. Annals of Emergency Medicine. 2004;43(2):215-223.
- ↑ Brott T, Adams H, Olinger C, Marler J, Barsan W, Biller J et al. Measurements of acute cerebral infarction: a clinical examination scale. Stroke. 1989;20(7):864-870.
- ↑ Marion D, Carlier P. PROBLEMS WITH INITIAL GLASGOW COMA SCALE ASSESSMENT CAUSED BY PREHOSPITAL TREATMENT OF PATIENTS WITH HEAD INJURIES. The Journal of Trauma: Injury, Infection, and Critical Care. 1994;36(1):89-95.
- ↑ Meredith W, Rutledge R, Fakhry S, Emery S, Kromhout-Schiro S. The Conundrum of the Glasgow Coma Scale in Intubated Patients. The Journal of Trauma: Injury, Infection, and Critical Care. 1998;44(5):839-845.
- ↑ Lesko M, Jenks T, Perel P, O'Brien S, Childs C, Bouamra O et al. Models of Mortality Probability in Severe Traumatic Brain Injury: Results of the Modelling by the UK Trauma Registry. Journal of Neurotrauma. 2013;30(24):2021-2030.
- ↑ Grote S, Böcker W, Mutschler W, Bouillon B, Lefering R. Diagnostic Value of the Glasgow Coma Scale for Traumatic Brain Injury in 18,002 Patients with Severe Multiple Injuries. Journal of Neurotrauma. 2011;28(4):527-534