Glasgow Coma Scale: Difference between revisions
No edit summary |
No edit summary |
||
| Line 18: | Line 18: | ||
[[Image:GCS Steps to Assessment.png|center|800x150px|GCS Steps to Assessment]]<br> | [[Image:GCS Steps to Assessment.png|center|800x150px|GCS Steps to Assessment]]<br> | ||
The assessor should evaluate each of the subscales as listed in the Assessment Aid. Each subscale has several components | The assessor should evaluate each of the subscales as listed in the [http://www.glasgowcomascale.org/downloads/GCS-Assessment-Aid-English.pdf?v=3 Assessment Aid]. Each subscale has several components. Based on the level of consciousness, a score is assigned. A higher score indicates a greater level of consciousness.<br> | ||
<br> | <br> | ||
| Line 24: | Line 24: | ||
[[Image:GCS Subscales.png|center|540x200px|GCS Subscales and Components]]<br> | [[Image:GCS Subscales.png|center|540x200px|GCS Subscales and Components]]<br> | ||
The GCS used three sites for stimulation. This includes finger tip pressure, trapezius pinch and supraorbital notch. When stimulating these areas, health care practitioners should look for one of two responses: An abnormal flexion response or a normal flexion response.<ref name="Assessment Aid" /><br> | |||
<br> | |||
[[Image:GCS Flexion Responses and Sites of Stimulation.png|center|800x150px|GCS Responses and Sites of Stimulation]] | [[Image:GCS Flexion Responses and Sites of Stimulation.png|center|800x150px|GCS Responses and Sites of Stimulation]] | ||
Revision as of 05:10, 9 May 2017
Original Editor - Your name will be added here if you created the original content for this page.
Top Contributors - Megan Craig, Kendyl Wilson, Emily Lingerfelt, Kim Jackson, Jillian Burton, Vidya Acharya, Abbey Wright, Evan Thomas, Naomi O'Reilly, Claire Knott, Nicole Hills, Admin, Lucinda hampton, Stacy Schiurring, Tarina van der Stockt, WikiSysop, Simisola Ajeyalemi, Adam Vallely Farrell and Karen Wilson
Objective
[edit | edit source]
The Glasgow Coma Scale (GCS) was first created by Graham Teasdale and Bryan Jennett in 1974. It is a clinical scale to assess a patient’s “depth and duration of impaired consciousness and coma”[1] following an acute brain injury. Healthcare practitioners can monitor the motor responsiveness, verbal performance, and eye opening of the patient in the form of a simple chart. The GCS is the most commonly used tool internationally for this assessment and has been translated into 30 languages. It should not, however, be confused with the Glasgow Outcome Scale (GOS), which evaluates persistent disability after brain damage. [2]
Intended Population
[edit | edit source]
Method of Use[edit | edit source]
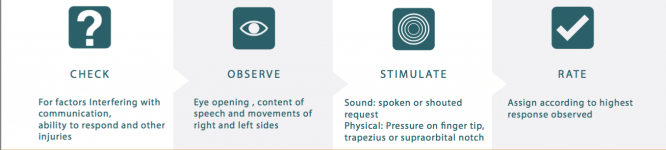
The GCS Assessment Aid has four steps to the assessment process: Check, observe, stimulate, rate.[3]
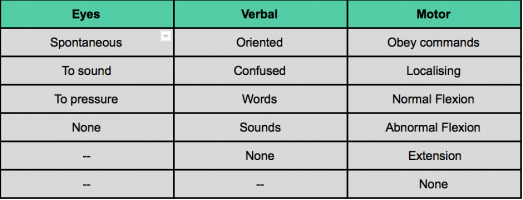
The assessor should evaluate each of the subscales as listed in the Assessment Aid. Each subscale has several components. Based on the level of consciousness, a score is assigned. A higher score indicates a greater level of consciousness.
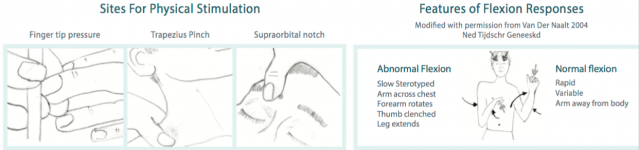
The GCS used three sites for stimulation. This includes finger tip pressure, trapezius pinch and supraorbital notch. When stimulating these areas, health care practitioners should look for one of two responses: An abnormal flexion response or a normal flexion response.[3]
The National Institute for Health Care and Excellence (NICE) published clinical guidelines on Head injuries for assessment and early management. NICE recommends the following clinical guidelines:
- Until a patient has achieved a score of 15 on the GCS, patients should be observed every half hour.
- Once GCS score has reached 15, the patient should be re-assessed using the GCS every half hour for two consecutive hours.
- If the patient's GCS score remains above 15, the patient should be then observed once every hour for four hours and then every 2 hours after that.
Note: If a patient's’ GCS score drops below 15, the health care practitioners should revert to observing the patient every half hour.[4]
The Institute of Neurological Sciences NHS Greater Glasgow and Clyde created a YouTube Video to demonstrate how to properly use the outcome measure.
Reference
[edit | edit source]
Teasdale G, Jennett B. Assessment of coma and impaired consciousness: a practical scale. The Lancet. 1974 Jul 13;304(7872):81-4.
Evidence[edit | edit source]
Reliability[edit | edit source]
The inter-rater reliabilty of the total Glasgow Coma Scale is p=0.86. Some research has subdivided the inter-rater reliabiltiy for each subscale. For the eye score the inter-rater reliability is p=0.76, the verbal score is p=0.67, and the motor score is p=0.81 [6] The research for test-retest reliability is not recent and should be updated, however the best available evidence is k=0.66-0.77 [7]
Based on a recent systematic review, the total score is typically less reliable than the individual components with a total Kappa value of 77% as compared to the eye, motor, and verbal scores which had Kappa values of 89%, 94%, and 88% respectively [8]
Validity[edit | edit source]
The validity of the glascow coma scale comes under fire because a lot of hospitals administer the test while patients have been sedated, often underestimating patient scores. It’s also difficult to elicit accurate scores when patients are intubated.[9] Recent research has refuted that intubation elicits significantly different survival rates with the verbal score of r=0.90 and the total score r=0.97[10] The motor score is consistently the most predictive component of the GCS[11]
Responsiveness[edit | edit source]
Given the current best available evidence, the GCS has a low sensitivity (56.1%) and a high specificity (82.2%). Therefore there are very few false positives predicting a low rate of survival in healthy individuals.[12]
It is argued that the GCS does not accuratley score patients who are intubated and does not assess brainstem reflexes and that can account for its low predictive capacity. A GCS administered at 24 hours post injury has a odds ratio of 0.4 in predicting in-hospital mortality. When administered at 72 hours post injury, the odds ratio improve to 0.59 in predicinting in-hospital mortality.[13]
Evidence suggests that the Glasgow Coma scale has a 71% accuracy in predicting functional independence post-injury. The GCS also modestly correlates with the Disability Rating Scale (-0.28) and the cognitive component of the Functional Independence Measure (0.37)[14]
Miscellaneous
[edit | edit source]
Links[edit | edit source]
The Glasgow Structured Approach to Assessment of the Glasgow Coma Scale http://www.glasgowcomascale.org
NICE Guideline to Head Injury Assessment and Early Management
https://www.nice.org.uk/guidance/cg176/resources/head-injury-assessment-and-early-management-pdf-35109755592901
Recent Related Research (from Pubmed)[edit | edit source]
Extension:RSS -- Error: Not a valid URL: feed://https://eutils.ncbi.nlm.nih.gov/entrez/eutils/erss.cgi?rss_guid=1vwc2FOtmnQ43rSLIG_ltX_vb362uUeFuFNJ9qEArduwwdiYz9%7Ccharset=UTF-8%7Cshort%7Cmax=10
References[edit | edit source]
References will automatically be added here, see adding references tutorial.
- ↑ Teasdale G, Jennett B. Assessment of coma and impaired consciousness: a practical scale. The Lancet. 1974 Jul 13;304(7872):81-4.
- ↑ Frej M, Frej J. The Glasgow Structured Approach to Assessment of the Glasgow Coma Scale [Internet]. What is GCS - Glasgow Coma Scale. Sir Graham Teasdale; [cited 2017May7]. Available from: http://www.glasgowcomascale.org/what-is-gcs/
- ↑ 3.0 3.1 Institute of Neurological Sciences NHS Greater Glasgow and Clyde. Glasgow Coma Scale: Do it this way [Internet]. Sir Graham Teasdale; 2015 [cited 2017 May 7]. Available from: http://www.glasgowcomascale.org/downloads/GCS-Assessment-Aid-English.pdf?v=3
- ↑ Head injury: Assessment and early management [Internet]. National Institute for Health and Care Excellence; 2014 [cited 7 May 2017]. Available from: https://www.nice.org.uk/guidance/cg176/resources/head-injury-assessment-and-early-management-pdf-35109755592901
- ↑ GCS at 40. Glasgow Coma Scale at 40 | The new approach to Glasgow Coma Scale assessment. Available from: https://www.youtube.com/watch?v=v6qpEQxJQO4 [last accessed 05/07/17
- ↑ Gill M, Reiley D, Green S. Interrater reliability of Glasgow Coma Scale scores in the emergency department. Annals of Emergency Medicine. 2004;43(2):215-223.
- ↑ Brott T, Adams H, Olinger C, Marler J, Barsan W, Biller J et al. Measurements of acute cerebral infarction: a clinical examination scale. Stroke. 1989;20(7):864-870.
- ↑ Reith F, Synnot A, van den Brande R, Gruen R, Maas A. Factors Influencing the Reliability of the Glasgow Coma Scale: A Systematic Review. Neurosurgery. 2017;42:3-15.
- ↑ Marion D, Carlier P. PROBLEMS WITH INITIAL GLASGOW COMA SCALE ASSESSMENT CAUSED BY PREHOSPITAL TREATMENT OF PATIENTS WITH HEAD INJURIES. The Journal of Trauma: Injury, Infection, and Critical Care. 1994;36(1):89-95.
- ↑ Meredith W, Rutledge R, Fakhry S, Emery S, Kromhout-Schiro S. The Conundrum of the Glasgow Coma Scale in Intubated Patients. The Journal of Trauma: Injury, Infection, and Critical Care. 1998;44(5):839-845.
- ↑ Lesko M, Jenks T, Perel P, O'Brien S, Childs C, Bouamra O et al. Models of Mortality Probability in Severe Traumatic Brain Injury: Results of the Modelling by the UK Trauma Registry. Journal of Neurotrauma. 2013;30(24):2021-2030.
- ↑ Grote S, Böcker W, Mutschler W, Bouillon B, Lefering R. Diagnostic Value of the Glasgow Coma Scale for Traumatic Brain Injury in 18,002 Patients with Severe Multiple Injuries. Journal of Neurotrauma. 2011;28(4):527-534
- ↑ McNett M, Amato S, Gianakis A, Grimm D, Philippbar S, Belle J et al. The FOUR Score and GCS as Predictors of Outcome After Traumatic Brain Injury. Neurocritical Care. 2014;21(1):52-57.
- ↑ McNett M. A Review of the Predictive Ability of Glasgow Coma Scale Scores in Head-Injured Patients. Journal of Neuroscience Nursing. 2007;39(2):68-75.