Femoral Neck Fractures Biomechanics
The purpose of this article is to translate best evidence knowledge about the physiology of the femoral neck, the biomechanics involved in the initiation of a fracture, and measures that can be taken to reduce the occurrence of a femoral neck fracture.
Background[edit | edit source]
Femoral neck fractures can be detrimental to a person’s health. The occurrence of a femoral neck fracture is associated with decreased quality of life, increased morbidity, disability, and mortality in the elderly population.[1] What is also concerning about femoral neck fractures is the occurrence of non-union between the femoral neck and the femoral head. This reduces the distribution of blood flow to the femoral head which is a cause for avascular necrosis.[2]
Fracture risk is determined by the bone strength and the applied load. The main predictor of bone strength is the bone mineral density at the femoral neck. The bone mineral density can indicate fracture risk and it can be obtained via dual x-ray absorptiometry.[3]Other factors that determine fracture risk are bone geometry, cortical bone thickness, and cortical bone density.[3] The cortical bone matrix has a direct effect on the overall mechanical strength of the bone. Bone porosity, which can be assessed through a bone biopsy, is a strong predictor of mechanical strength.[3]
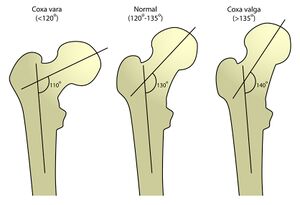
Geometrically, the normal femoral neck-shaft angle is between 124-135⁰. Femoral neck-shaft angle that is below 120⁰ is considered cox vara. If the femoral neck-shaft angle is above 135⁰ is considered coxa valga. Having a femoral neck-shaft angle that is outside of the normal ranges increases the risk for a femoral neck fracture.[4] Additionally, increased hip axis length (measured along the femoral neck axis and is defined as the distance from the inferolateral aspect of the greater trochanter to the inner pelvic brim), increased neck length, decreased cortical thickness, and decreased cross-sectional area of the femoral neck are all factors that can increase the risk of fracture.[3][4]
The initiation of fracture is typically at the superior aspect of the femoral neck, a region with less cortical thickness, and travels along through the trabecular bone.[5] The aging process reduces bone mineral density and cortical bone thickness, which is why the prevalence of femoral neck fracture is higher in the elderly population.[5]
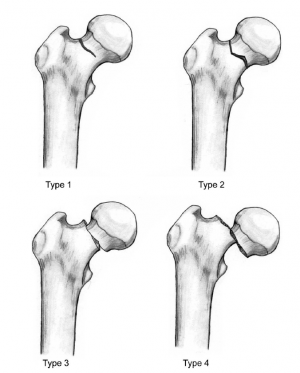
The Garden classification is the most commonly used for femoral neck fractures. This splits into four categories depending on the severity of the fracture and the degree of displacement.[6] Type I is an incomplete fracture or valgus impacted fracture. Type II is a complete fracture without displacement. Type III is a complete fracture with partial displacement of fracture fragments. Type IV is a complete fracture with total displacement of fracture fragments, allowing the femoral head to rotate back to anatomical position within the acetabulum.[6]
The Pauwel classification is based on the angle of the fracture from the horizontal. Type I is< 30⁰ from the horizontal. Type II is between 30-70⁰ from the horizontal. Type III is >70⁰ from the horizontal. Generally, there is an increase in fracture instability with an increase in fracture angle.[2]
Biomechanics Involved[edit | edit source]
The femoral neck experiences the highest stress loads within the femur. [7] Forces that are acting on the femoral neck are externally, and internally generated forces.[3][5] Externally generated forces are a result of ground reaction forces that translated from the ankle to the femoral neck as a result of the vertical impact and typically stay below 1.3 times body weight during low-speed walking. [3] Internally generated forces are a result of the muscles acting on the bone to accomplish the desired movements and maintain balance. Internally generated forces are typically 2-3 times body weight during low-speed walking. [5]
The internal and external forces produce bending and torsional moments that act on the femoral neck. The bending moments at the femoral neck are a product of vertical loading during daily activities.[3] The bending moment creates compression on the inferior aspect of the femoral neck and tension at the superior aspect of the femoral neck.[3] The majority of the vertical loading force is transferred through vertically oriented trabeculae that are located at the inferior aspect of the femoral neck.[4]
The level of strain at the femoral neck is reported to be 500-2000 microstrains for day-to-day activities.[3] The bone strain is largest at the inferior aspect of the neck. This results in a larger thickness of the bone cortex compared to the superior aspect.[3] The superior aspect of the femoral neck experiences increased strain during activities like stair climbing where there is an increase of hip flexion and abduction. The increased strain is due to the increase of torsion at the femoral neck.[5]
Femoral neck stress fractures occur when homeostatic remodeling can not keep up with the strain that is put on the bone. This is often due to repetitive loading of bone with abnormal forces and sudden increase in training volume or activity.[8] Femoral neck stress fractures are associated with activities like long-distance running, gymnastics, and ballet.[8] The cyclical loading of the tissue leads to decreased tissue tolerance. The micro-fractures that occur on the bone cannot be repaired fast enough and turn into fractures.[7]
Femoral neck stress fractures are subdivided into two categories. Category one is compressive type fractures that occur at the inferior aspect of the femoral neck. This type of fracture occurs when the forces applied to the bone are higher than the plastic properties of the bone.[8] Category two is tensile type fractures that occur at the superior aspect of the bone. In normal conditions, the gluteus medius and minimus muscles counteract the high-tension forces acting on the femoral neck. However, tension femoral neck stress fracture occurs when the muscles are fatigued, and the tensile forces are translated predominantly by the bone.[8]
Sideways falls are a leading cause of hip fracture in the elderly population.[1] Sideways falls, on the greater trochanter, induce a compressive type of load to the femoral neck.[3] The factors that are involved in falls that contribute to fractures are femoral strength, fall velocity, and effective mass.[1] Femoral strength is significantly reduced in a sideways fall scenario. The loading configuration determines the amount of force required to induce a fracture on the femoral neck. The force required to induce a fracture during a single leg stance is 7214N vs 3462N during a sideways fall ±1520N. The femoral neck can withstand a much greater force during vertical loading vs lateral loading on the greater trochanter.[1]
Fall velocities greater than 3m/s can induce a fracture on the femoral neck. Falls due to a slip or stumble have higher fall velocity than falls due to incorrect shifting of weight.[1] The effective mass is the part of the body that moves downwards and creates the impact load. A fall from a standing position is going to have a larger effective mass than a fall from a kneeling position.[1]
Prevention[edit | edit source]
The first measure of treatment is knowing the signs of a femoral neck stress fracture. Knowing how the fracture presents can lead to early diagnosis and avoid further complications.[7][8] The onset of pain occurs at the hip or groin area during activities of weight-bearing. Pain can also radiate to the anterior thigh, gluteal region and even down to the knee. There is a gradual increase of pain throughout the activities.[8] This stage is when antalgic gait is likely to present due to the pain. Eventually, pain is also noticed during periods of rest and at night. In later stages, cracking and popping can be felt in the groin region that often leads to a complete fracture of the femoral neck.[8]
In long-term care facilities, a multicomponent exercise program has been proven to reduce the risk of falls for the participants. This can be an effective measure to reduce the occurrence of a fracture at the femoral neck.[9] The benefits of the exercise program are improved balance control, improved muscular strength, and muscular endurance. The most effective exercise program should incorporate balance training, strength training followed by flexibility, and endurance training.[9] Alternatively, Taichi exercise has been proven to reduce bone mineral density loss regions of the femoral neck. This can be an effective measure to maintain bone strength and reduce fracture risk.[10]
Vitamin Dsupplementation has also been proven to reduce the occurrence of falls in long-term care facilities. This measure works best when combined with a multifaceted approach combining Vitamin D supplements with Calcium supplements, education on fall prevention, and balance exercise training.[9]
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 Sarvi MN, Luo Y. Sideways fall-induced impact force and its effect on hip fracture risk: a review. Osteoporosis international. 2017 Oct;28(10):2759-80.
- ↑ 2.0 2.1 Fuchs RK, Kersh ME, Carballido-Gamio J, Thompson WR, Keyak JH, Warden SJ. Physical activity for strengthening fracture prone regions of the proximal femur. Current osteoporosis reports. 2017 Feb 1;15(1):43-52.
- ↑ 3.00 3.01 3.02 3.03 3.04 3.05 3.06 3.07 3.08 3.09 3.10 Augat P, Bliven E, Hackl S. Biomechanics of femoral neck fractures and implications for fixation. Journal of orthopaedic trauma. 2019 Jan 1;33:S27-32.
- ↑ 4.0 4.1 4.2 Kani KK, Porrino JA, Mulcahy H, Chew FS. Fragility fractures of the proximal femur: review and update for radiologists. Skeletal radiology. 2019 Jan;48(1):29-45.
- ↑ 5.0 5.1 5.2 5.3 5.4 Basso T, Klaksvik J, Syversen U, Foss OA. Biomechanical femoral neck fracture experiments—a narrative review. Injury. 2012 Oct 1;43(10):1633-9.
- ↑ 6.0 6.1 Florschutz AV, Langford JR, Haidukewych GJ, Koval KJ. Femoral neck fractures: current management. Journal of orthopaedic trauma. 2015 Mar 1;29(3):121-9.
- ↑ 7.0 7.1 7.2 Neubauer T, Brand J, Lidder S, Krawany M. Stress fractures of the femoral neck in runners: a review. Research in Sports Medicine. 2016 Jul 2;24(3):283-97.
- ↑ 8.0 8.1 8.2 8.3 8.4 8.5 8.6 Robertson GA, Wood AM. Femoral neck stress fractures in sport: a current concepts review. Sports medicine international open. 2017 Feb;1(2):E58.
- ↑ 9.0 9.1 9.2 Karlsson MK, Magnusson H, von Schewelov T, Rosengren BE. Prevention of falls in the elderly—a review. Osteoporosis international. 2013 Mar;24(3):747-62.
- ↑ Zou L, Wang C, Chen K, Shu Y, Chen X, Luo L, Zhao X. The effect of Taichi practice on attenuating bone mineral density loss: A systematic review and meta-analysis of randomized controlled trials. International journal of environmental research and public health. 2017 Sep;14(9):1000.