Ependymoma: Difference between revisions
No edit summary |
No edit summary |
||
| Line 9: | Line 9: | ||
Unlike other kinds of cancer, ependymomas usually don’t spread to other parts of the body, but can spread to more than one area of the brain or spine. In children, these tumors are likely to come back after treatment<ref>Web Md Ependymoma Available: https://www.webmd.com/cancer/brain-cancer/what-is-ependymoma (accessed 11.5.2022)</ref>. | Unlike other kinds of cancer, ependymomas usually don’t spread to other parts of the body, but can spread to more than one area of the brain or spine. In children, these tumors are likely to come back after treatment<ref>Web Md Ependymoma Available: https://www.webmd.com/cancer/brain-cancer/what-is-ependymoma (accessed 11.5.2022)</ref>. | ||
[[File:Tentorium cerebelli.jpeg|right|frameless]] | |||
They can be divided into three groups depending on the anatomical compartment in which they are found: | They can be divided into three groups depending on the anatomical compartment in which they are found: | ||
| Line 16: | Line 16: | ||
# Spinal cord (10%) | # Spinal cord (10%) | ||
==Clinically Relevant Anatomy== | ==Clinically Relevant Anatomy== | ||
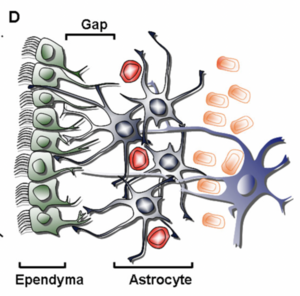
[[Glial Cells|Glial cells]]: cell type that are found between nerve cells that share a general function of holding the CNS together. Although there are about 86-100 billion neurons in the brain, there are about the same number of glial cells in the brain.<ref>Palastanga, N., Field, D. and Soames, R. (2012). ''Anatomy and Human Movement: Structure and Function''. 6th ed. Burlington: Elsevier Science.</ref> | |||
[[File:Ventricles Brain.png|thumb|Ventricles Brain]] | [[File:Ventricles Brain.png|thumb|Ventricles Brain]] | ||
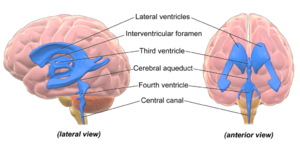
Ventricals and the Central Canal of the Spinal Cord: fluid-filled spaces within the CNS that contain cerebrospinal fluid. Both are common locations for tumours. | Ventricals and the Central Canal of the Spinal Cord: fluid-filled spaces within the CNS that contain cerebrospinal fluid. Both are common locations for tumours. | ||
| Line 26: | Line 25: | ||
Ependymomas are traditionally thought to arise from oncogenetic events that transform normal ependymal cells into tumor phenotypes. The precise nature and order of these genetic events are unknown.<ref name=":1">Emedicine.medscape.com. (2017). ''Ependymoma: Practice Essentials, Background, Pathophysiology''. [online] Available at: <nowiki>http://emedicine.medscape.com/article/277621-overview</nowiki> [Accessed 30 Aug. 2017].</ref> | Ependymomas are traditionally thought to arise from oncogenetic events that transform normal ependymal cells into tumor phenotypes. The precise nature and order of these genetic events are unknown.<ref name=":1">Emedicine.medscape.com. (2017). ''Ependymoma: Practice Essentials, Background, Pathophysiology''. [online] Available at: <nowiki>http://emedicine.medscape.com/article/277621-overview</nowiki> [Accessed 30 Aug. 2017].</ref> | ||
== | == Epidemiology == | ||
[[File:Ependymal Cells.png|thumb|Ependymal Cells Ventricle]] | |||
Ependymomas affect all age groups, with a higher frequency in children, being the third most common brain tumor in pediatric patients. As per the Central Brain Tumor Registry of the United States (CBTRUS) Statistical Report for CNS tumors from the years 2011 to 2015, ependymal tumors represent 1.7% of all brain and CNS tumors, with a median age of 44 years. | |||
Children: It represents around 6% to 12% of children brain tumor and 2% of all childhood cancer<ref name=":3">Kilday JP, Rahman R, Dyer S, Ridley L, Lowe J, Coyle B, Grundy R. Pediatric ependymoma: biological perspectives. Molecular Cancer Research. 2009 Jun 1;7(6):765-86.</ref>. The prognosis for pediatric ependymomas remains relatively poor when compared with other brain tumors in children,despite advances in neurosurgery, neuroimaging techniques, and postoperative adjuvant therapy.<ref name=":3" /> The 5-year survival rate ranges from 39% to 64%.<ref name=":3" /> | |||
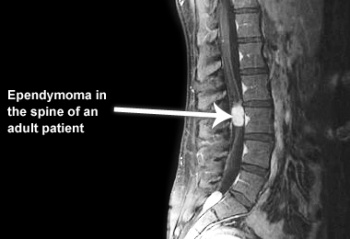
Adults: the most common primary glial neoplasm of spinal cord representing 50%–60% of all intramedullary cord neoplasms.<ref name=":4">Helseth A, Mørk SJ. Primary intraspinal neoplasms in Norway, 1955 to 1986: a population-based survey of 467 patients. Journal of neurosurgery. 1989 Dec 1;71(6):842-5</ref><ref>Mohammed W, Farrell M, Bolger C. Spinal cord ependymoma–Surgical management and outcome. Journal of Neurosciences in Rural Practice. 2019 Apr 1;10(2):316.</ref>; Most commonly occur in the spinal cord<ref name=":0">Cern-foundation.org. (2017). ''Ependymoma Basics | CERN Foundation''. [online] Available at: <nowiki>http://www.cern-foundation.org/education/ependymoma-basics</nowiki> [Accessed 24 Aug. 2017]. | |||
</ref>; Ependymomas are believed to be slow-growing tumors and exhibit benign pathology behavior<ref name=":4" />. | |||
</ref> | |||
== Clinical Presentation == | == Clinical Presentation == | ||
'''Brain tumor symptoms include:''' | |||
* Headache or pressure in the head | * Headache or pressure in the head | ||
* Nausea or vomiting | * Nausea or vomiting | ||
* Blurred vision | * Blurred vision | ||
* Weakness or numbness and tingling | * Weakness or numbness and tingling | ||
'''Spinal cord symptoms include:''' | |||
* Back pain | * Back pain | ||
* Weakness in the arms or legs | * Weakness in the arms or legs | ||
| Line 54: | Line 46: | ||
* Problems going to the bathroom or controlling bowel or bladder function<ref name=":0" /><ref>Sofuoğlu ÖE, Abdallah A. Pediatric Spinal Ependymomas. Medical science monitor: international medical journal of experimental and clinical research. 2018;24:7072.</ref> | * Problems going to the bathroom or controlling bowel or bladder function<ref name=":0" /><ref>Sofuoğlu ÖE, Abdallah A. Pediatric Spinal Ependymomas. Medical science monitor: international medical journal of experimental and clinical research. 2018;24:7072.</ref> | ||
== | == Diagnosis == | ||
To get an accurate diagnosis, a tumor biopsy is performed a ie piece of tumor tissue will be removed during surgery, if possible. A neuropathologist should then review the tumor tissue.<ref name=":2">NIH Ependymoma Available:https://www.cancer.gov/rare-brain-spine-tumor/tumors/ependymoma (accessed 11.5.2022)</ref> | |||
</ref | |||
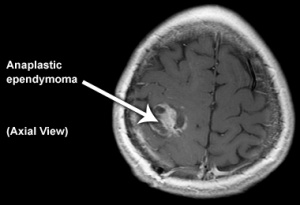
== | ==Ependymoma Grades== | ||
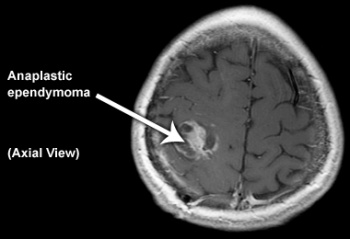
Ependymomas are grouped in three grades based on their characteristics. Within each grade, are different ependymoma subtypes. Molecular testing is used to help identify subtypes that are related to location and disease characteristics. | |||
# Grade I ependymomas: low grade tumors, cells grow slowly. The subtypes include subependymoma and myxopapillary ependymoma. Both are more common in adults than in children. Myxopapillary tumors usually occur in the spine. | |||
# Grade II ependymomas: low grade tumors and can occur in either the brain or the spine. | |||
# Grade III ependymomas: malignant (cancerous), fast-growing tumors. The subtypes include anaplastic ependymomas. These most often occur in the brain, but can also occur in the spine<ref name=":2" />. | |||
=== Treatment === | |||
Surgery: When possible, removing the tumour from the brain or spinal cord is a priority as SCI associated with spinal tumor is often managed surgically<ref>Ge L, Arul K, Mesfin A. Spinal Cord Injury From Spinal Tumors: Prevalence, Management, and Outcomes. World neurosurgery. 2019 Feb 1;122:e1551-6.</ref>. A secondary goal of surgery is obtaining a biopsy of cancerous cells for diagnosis. | |||
After surgery, there is no standard treatment for ependymomas. with many people not needing other treatment after surgery. For others, treatments may include [[Radiation Side Effects and Syndromes|radiation]], [[Chemotherapy Side Effects and Syndromes|chemotherapy]] or clinical trials. Clinical trials, with new chemotherapy, targeted therapy, or [[Immunotherapy|immunotherapy drugs]], may also be available and can be a possible treatment option. Treatments are decided by the patient’s healthcare team based on the patient’s age, remaining tumor after surgery, tumor type, and tumor location<ref name=":2" />. | |||
These | Palliative care may be necessary for patients at end-of-life. Those who undergo surgery may also develop a number of neurological deficits. These individuals may require physical therapy, speech therapy, and occupational therapy. In many cases, the neurological deficits are permanent<ref>Zamora EA, Alkherayf F. Ependymoma. InStatPearls [Internet] 2021 Jul 20. StatPearls Publishing.Available:https://www.ncbi.nlm.nih.gov/books/NBK538244/ (accessed 11.5.2022)</ref>. | ||
== Differential Diagnosis == | === Differential Diagnosis === | ||
* Astrocytoma | * Astrocytoma | ||
* Choroid Plexus Papilloma | * Choroid Plexus Papilloma | ||
| Line 104: | Line 70: | ||
* Vascular Surgery for Arteriovenous Malformations<ref name=":1" /> | * Vascular Surgery for Arteriovenous Malformations<ref name=":1" /> | ||
*<ref>Tuel SM, Cross LL, Meythaler JM, Faisant TE, Krajnik SR, Hogan P, Sewell L, Wilson B, Rodwell DW, Smith J. Interdisciplinary management of hemicorporectomy after spinal cord injury. Arch Phys Med Rehabil. 1992 Jul;73(7):669-73. PubMed PMID: 1622324.</ref> | |||
* | |||
{| class="wikitable" | {| class="wikitable" | ||
Revision as of 02:55, 11 May 2022
Original Editor - George Prudden
Top Contributors - Shaimaa Eldib, Lucinda hampton, George Prudden, Kim Jackson, Vidya Acharya and Rewan Elsayed ElkanafanyIntroduction[edit | edit source]
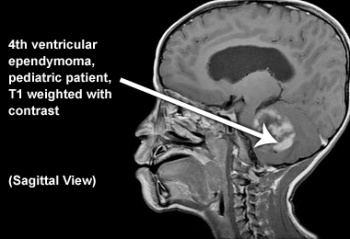
Ependymomas represent a broad group of glial tumours most often arising from the lining of the ventricles of the brain or the central canal of the spinal cord. They account for ~5% of all neuroepithelial neoplasms, ~10% of all paediatric brain tumours and up to 33% of brain tumours occurring in those less than 3 years of age[1].
Unlike other kinds of cancer, ependymomas usually don’t spread to other parts of the body, but can spread to more than one area of the brain or spine. In children, these tumors are likely to come back after treatment[2].
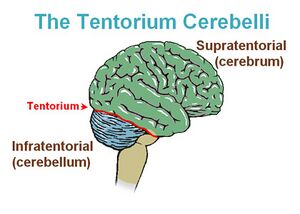
They can be divided into three groups depending on the anatomical compartment in which they are found:
- Posterior fossa (60%)
- Supratentorial (30%) ie above the tentorium cerebelli
- Spinal cord (10%)
Clinically Relevant Anatomy[edit | edit source]
Glial cells: cell type that are found between nerve cells that share a general function of holding the CNS together. Although there are about 86-100 billion neurons in the brain, there are about the same number of glial cells in the brain.[3]
Ventricals and the Central Canal of the Spinal Cord: fluid-filled spaces within the CNS that contain cerebrospinal fluid. Both are common locations for tumours.
Tentorium Cerebelli: extension of the dura matter that separates the cerebellum from the inferior aspect of the occipital lobes. Tumour below the tentorium are called infratentorial and those above are called supratentorial.
Pathological Process:[edit | edit source]
Ependymomas are traditionally thought to arise from oncogenetic events that transform normal ependymal cells into tumor phenotypes. The precise nature and order of these genetic events are unknown.[4]
Epidemiology[edit | edit source]
Ependymomas affect all age groups, with a higher frequency in children, being the third most common brain tumor in pediatric patients. As per the Central Brain Tumor Registry of the United States (CBTRUS) Statistical Report for CNS tumors from the years 2011 to 2015, ependymal tumors represent 1.7% of all brain and CNS tumors, with a median age of 44 years.
Children: It represents around 6% to 12% of children brain tumor and 2% of all childhood cancer[5]. The prognosis for pediatric ependymomas remains relatively poor when compared with other brain tumors in children,despite advances in neurosurgery, neuroimaging techniques, and postoperative adjuvant therapy.[5] The 5-year survival rate ranges from 39% to 64%.[5]
Adults: the most common primary glial neoplasm of spinal cord representing 50%–60% of all intramedullary cord neoplasms.[6][7]; Most commonly occur in the spinal cord[8]; Ependymomas are believed to be slow-growing tumors and exhibit benign pathology behavior[6].
Clinical Presentation[edit | edit source]
Brain tumor symptoms include:
- Headache or pressure in the head
- Nausea or vomiting
- Blurred vision
- Weakness or numbness and tingling
Spinal cord symptoms include:
- Back pain
- Weakness in the arms or legs
- Numbness or tingling in the arms, legs or trunk
- Problems going to the bathroom or controlling bowel or bladder function[8][9]
Diagnosis[edit | edit source]
To get an accurate diagnosis, a tumor biopsy is performed a ie piece of tumor tissue will be removed during surgery, if possible. A neuropathologist should then review the tumor tissue.[10]
Ependymoma Grades[edit | edit source]
Ependymomas are grouped in three grades based on their characteristics. Within each grade, are different ependymoma subtypes. Molecular testing is used to help identify subtypes that are related to location and disease characteristics.
- Grade I ependymomas: low grade tumors, cells grow slowly. The subtypes include subependymoma and myxopapillary ependymoma. Both are more common in adults than in children. Myxopapillary tumors usually occur in the spine.
- Grade II ependymomas: low grade tumors and can occur in either the brain or the spine.
- Grade III ependymomas: malignant (cancerous), fast-growing tumors. The subtypes include anaplastic ependymomas. These most often occur in the brain, but can also occur in the spine[10].
Treatment[edit | edit source]
Surgery: When possible, removing the tumour from the brain or spinal cord is a priority as SCI associated with spinal tumor is often managed surgically[11]. A secondary goal of surgery is obtaining a biopsy of cancerous cells for diagnosis.
After surgery, there is no standard treatment for ependymomas. with many people not needing other treatment after surgery. For others, treatments may include radiation, chemotherapy or clinical trials. Clinical trials, with new chemotherapy, targeted therapy, or immunotherapy drugs, may also be available and can be a possible treatment option. Treatments are decided by the patient’s healthcare team based on the patient’s age, remaining tumor after surgery, tumor type, and tumor location[10].
Palliative care may be necessary for patients at end-of-life. Those who undergo surgery may also develop a number of neurological deficits. These individuals may require physical therapy, speech therapy, and occupational therapy. In many cases, the neurological deficits are permanent[12].
Differential Diagnosis[edit | edit source]
- Astrocytoma
- Choroid Plexus Papilloma
- Glioblastoma Multiforme
- Tumors of the Conus and Cauda Equina
- Vascular Surgery for Arteriovenous Malformations[4]
References[edit | edit source]
- ↑ Radiopedia Ependymoma Available:https://radiopaedia.org/articles/ependymoma(accessed 11.5.2022)
- ↑ Web Md Ependymoma Available: https://www.webmd.com/cancer/brain-cancer/what-is-ependymoma (accessed 11.5.2022)
- ↑ Palastanga, N., Field, D. and Soames, R. (2012). Anatomy and Human Movement: Structure and Function. 6th ed. Burlington: Elsevier Science.
- ↑ 4.0 4.1 Emedicine.medscape.com. (2017). Ependymoma: Practice Essentials, Background, Pathophysiology. [online] Available at: http://emedicine.medscape.com/article/277621-overview [Accessed 30 Aug. 2017].
- ↑ 5.0 5.1 5.2 Kilday JP, Rahman R, Dyer S, Ridley L, Lowe J, Coyle B, Grundy R. Pediatric ependymoma: biological perspectives. Molecular Cancer Research. 2009 Jun 1;7(6):765-86.
- ↑ 6.0 6.1 Helseth A, Mørk SJ. Primary intraspinal neoplasms in Norway, 1955 to 1986: a population-based survey of 467 patients. Journal of neurosurgery. 1989 Dec 1;71(6):842-5
- ↑ Mohammed W, Farrell M, Bolger C. Spinal cord ependymoma–Surgical management and outcome. Journal of Neurosciences in Rural Practice. 2019 Apr 1;10(2):316.
- ↑ 8.0 8.1 Cern-foundation.org. (2017). Ependymoma Basics | CERN Foundation. [online] Available at: http://www.cern-foundation.org/education/ependymoma-basics [Accessed 24 Aug. 2017].
- ↑ Sofuoğlu ÖE, Abdallah A. Pediatric Spinal Ependymomas. Medical science monitor: international medical journal of experimental and clinical research. 2018;24:7072.
- ↑ 10.0 10.1 10.2 NIH Ependymoma Available:https://www.cancer.gov/rare-brain-spine-tumor/tumors/ependymoma (accessed 11.5.2022)
- ↑ Ge L, Arul K, Mesfin A. Spinal Cord Injury From Spinal Tumors: Prevalence, Management, and Outcomes. World neurosurgery. 2019 Feb 1;122:e1551-6.
- ↑ Zamora EA, Alkherayf F. Ependymoma. InStatPearls [Internet] 2021 Jul 20. StatPearls Publishing.Available:https://www.ncbi.nlm.nih.gov/books/NBK538244/ (accessed 11.5.2022)
- ↑ Tuel SM, Cross LL, Meythaler JM, Faisant TE, Krajnik SR, Hogan P, Sewell L, Wilson B, Rodwell DW, Smith J. Interdisciplinary management of hemicorporectomy after spinal cord injury. Arch Phys Med Rehabil. 1992 Jul;73(7):669-73. PubMed PMID: 1622324.