Dynamic Stabilisers of the Shoulder Complex
Original Editor - Khloud Shreif
Top Contributors - Khloud Shreif, Amanda Ager, Kim Jackson and Rishika BabburuIntroduction[edit | edit source]
The stability of the shoulder joint, like any other joint in the body depends, on both static and dynamic stabilizers. However, because of the vast range of motion of the shoulder complex (the most mobile joint of the human body), dynamic stabilizers are crucial for a strong sense of neuromuscular control throughout all movements and activities involving the upper extremities.
Neuromuscular control in this context, can be understood as the “unconscious activation of dynamic restraints occurring in preparation for, and in response to, joint motion and loading for the purpose of maintaining functional joint stability.”[1] Dynamic restraints result from neuromuscular control over the shoulder muscles, facilitated through motor control and proprioceptive input.
Moreover, the term sensorimotor system describes the sensory, motor, and central integration and processing components involved in maintaining joint homeostasis during bodily movements - more commonly understood to be functional joint stability.[2]
Lastly, proprioception within this context can be understood as an important component of the sensorimotor system; whereby the balance between mobility and stability of the glenohumeral (GH) joint is ensured by a neuromuscular interaction between capsular ligamentous receptors, the central nervous system (CNS), and the stabilizing muscles of the shoulder complex.[3]
Static stabilizers include the joint labrum and capsuloligements components of the glenohumeral joint, as well as fascia tissues throughout the shoulder complex. There is also a theory that the neuromuscular bundle (nerves, veins, arteries) can also contribute to static stability.
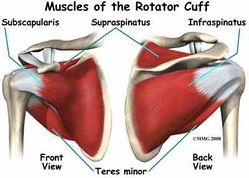
Dynamic stabilizers include the contractile tissues of the shoulder complex (tendons, muscles and tendon-muscular junctions). The most well known are the rotator cuff muscles (supraspinatus, infraspinatus, subscapularis, Teres minor), which collectively control the fine-tuning movement of the humeral head within the glenoid fossa (maintain centralization of the humeral head during static postures and dynamic movements). There are also the periscapsular muscles[4], which are very important for homogeneous shoulder movements while avoiding biomechanical misalignments, such as a shoulder impingement.
Dynamic stabilization during upper extremity movements is obtained by synergetic mechanisms of shoulder muscles’ co-contractions, appropriate positioning, control and coordination of the shoulder as well as the scapula-thoracic complex.[5][6]
The dynamic stability of shoulder complex can be divided into:
- Glenohumeral stability (Local)
- Scapulothoracic stability (Global)
Glenohumeral joint stability[edit | edit source]
Deltoid muscle[edit | edit source]
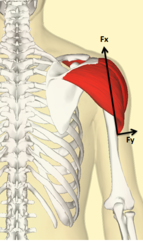
The deltoid muscle has a significant role as a stabilizer, and is generally accepted as a prime mover for glenohumeral joint during abduction, along with the supraspinatus muscle.
The deltoid is the primary muscle responsible for the abduction of the arm from 15 to 90 degrees. It also serves as a stabilizer of the humeral head, especially in instances of carrying a load.[8]
From the biomechanical figure, the line of action (line of pull) of the deltoid with the arm at the side of body, the parallel force component (fx) directed superiorly, is the largest of the three other components; resulting in a superior translation of the humeral head, and a small applied perpendicular force is directed towards rotating the humerus. Also, there is an inferior pull of force (fx), to offset the component of the middle deltoid which is active during arm elevation, as gravity cannot balance the force around the GH joint alone.[9]
Blood supply of the deltoid: The posterior circumflex humeral artery and the deltoid branch of the thoracoacromial artery are the vascular sources for the deltoid.[10]
Innervation of the deltoid: The neural supply of the deltoid is via the axillary nerve (C5, C6) from the posterior cord of the brachial plexus.[10]
Rotator Cuff muscles[edit | edit source]
Rotator cuff (RC) (collectively the following muscles: supraspinatus, subscapularis, infraspinatus, teres minor) not only abduct the shoulder, but also plays an important role as stabilizer muscles.[11] The main role of the rotator cuff is to control the fine-tuning (smaller) movements of the head of the humerus, within the glenoid fossa. The rotator cuff muscles help to maintain a centralized position of the head of the humerus during static postures and dynamic movements. This is crucial with regards to neuromuscular control, as it helps to avoid a biomechanical impingement of the soft tissues, under the subacromial arch during elevation movements.
From Figure 2 we can see three of the RC muscles (teres minor, subscapularis, infraspinatus) ,in relation to their anatomical position and their muscle fiber direction from origin to insertion. This is important to note, as they tend to have a similar inferior line of pull[7] and with the summation of three forces of rotator cuff, they nearly offset superior translation of humeral head, which is created by deltoid.
Also, the wide range of motion of the shoulder is allowed by the variety of rotational moments of the cuff muscles[12]. The teres minor and infraspinatus muscles are external rotators and participate in the clearing of the greater tubercle underneath the acromion during shoulder movements.
Supraspinatus muscle[edit | edit source]
Regarding supraspinatus location more superior than the three other rotator cuff it has a line of pull superior that can't offset deltoid force.
Even though it still an effective stabilizer due to it's larger moment arm, it's capable to elevate glenohumeral joint near normal.[7]
From illustrated above we can consider deltoid and rotator cuff as one of a force couple of glenohumeral joint.
Imbalance of one or more of these muscles consider a contribution cause to shoulder problems (impingement, bursitis, instability )
Blood supply of the supraspinatus: The suprascapular artery delivers blood to the supraspinatus muscle.[10]
Innervation of the supraspinatus: The neural supply of the supraspinatus is by the suprascapular nerve (C5, C6) from the upper trunk of the brachial plexus.[10]
Scapulothoracic joint stability[edit | edit source]
Because the scapulothoracic joint is a floating joint, it solely relies on neuromuscular control (adequate strength and control of the stabilizer muscles, as well as a healthy sense of muscular timing). Agonist, antagonist and synergist muscle control is vital for a normalized and non-pathological scapulothoracic rhythm. During movements in elevation and reaching activities, it is important to consider the force-coupling which acts on the floating joint. Such muscles to consider are the serratus anterior, serratus posterior, the trapezius (upper / middle / lower), the rhomboids, teres major, the levator scapulae, the latissimus dorsi and the flexibility and mobility of the thoracolumbar fascia.
Serratus anterior muscle and Trapezius[edit | edit source]
Serratus anterior[13][edit | edit source]
Serratus anterior muscle as a primary protractor muscle of scapula, it's capable of producing scapular protraction, upward rotation, external rotation and posterior tilting of the scapula with progress arm elevation.
The strong action of serratus as a protractor needs an apposite force to control this movement. Serratus anterior and trapezius muscles work as a primary force couple to rotate scapula upward.
Trapezius muscle[14][edit | edit source]
Trapezius has a retraction effect on scapula to counter the protraction and lateral pull of serratus anterior.
Upper trapezius[edit | edit source]
Take in consideration it's insertion to the clavicle, it produces upward rotation of scapula indirect and contributes to first degrees of clavicle elevation and retraction.
Middle trapezius[edit | edit source]
Contributes to offset the strong action of serratus anterior as a protractor and also produces an external rotation of scapula but it has a downward moment arm on scapula larger than it's upward moment arm.
Lower trapezius[edit | edit source]
With serratus anterior, lower trapezius is a primary upward rotator of scapula, it creates an upward rotation moment arm when the axis reaches acromioclavicular joint.
Serratus anterior and trapezius muscles they act agnostic for scapular movement and as a synergistic with glenohumeral forces[edit | edit source]
Rhomboid muscle and Teres major[edit | edit source]
- The rhomboid downward rotation action on scapula help to offset the undesired upward rotatory torque of teres major.
- Rhomboid acts eccentrically to control change position of scapula during arm elevation so it contributes to counter the lateral translation force of serratus anterior.
- It has another stabilization role for scapula during adduction or extension.
Clinical presentation[edit | edit source]
For smooth synchronous movement of the shoulder complex we need the force couples of glenohumeral and scapulothoracic to work in a synched timing and adequate forces to offset each other.
For example; the deltoid (middle fiber) acts to stabilize the humeral head against the glenoid cavity with small participation to abduct the arm, there are(subscapularis, teres minor, infraspinatus) their forces balance the deltoid action and along with supraspinatus that participates mainly in arm abduction.
Deficit in these forces for example; insufficient activation of rotator cuff /deltoid over activation participate to narrowing coracoacormial space (figure 3) that compress tendons in this space ( rotator cuff tendinopathy /shoulder impingement)[16]
Scapular winging, scapular dyskinesia that happen due to imbalance of scapulothoracic muscles, for example, serratus anterior, lower trapezius weakness, upper trapezius overactivation.
Physical therapy interventions[edit | edit source]
Rehabilitation should concentrate on the restoration of the normal biomechanical alignment of the shoulder complex (centralization of the GH joint, proper scapulothoracic gliding of the scapula) as well as restoring the proper force-coupling balance of the stabilizing muscles.
Appropriate strengthening of the shoulder dynamic stabilizer muscles and adequate neuromuscular control-patterns is crucial during rehabilitation as well as the prevention of shoulder injuries.[5][17]
Neuromuscular exercises typically focus on movement quality, as guided by the supervising physical therapists. Neuromuscular exercises typically included strength, coordination, balance, and proprioception components.[18]
Exercises can be performed unilaterally, or bilaterally in unstable conditions involving an increased level of postural control (standing, planking, kneeling and laying on stability ball) and/or with external overload devices challenging motor-coordination (elastics, balls, dumbbells).[19]
Resistance training exercises can promote neural and structural modifications to the shoulder complex[20][21] and can increase the sensory, biomechanical and motor-processing patterns[22] (such as to the cervico-thoracic spine, the shoulder complex and the upper extremities as a whole).
Overall, to rehabilitate the neuromuscular control of the shoulder complex, the therapist should focus on the following elements:[edit | edit source]
- Full and pain free range of motion of the cervical and thoracic spine.
- No neurological signs or symptoms from the cervical spine, throughout the upper extremities.
- Full and pain free range of motion of all distal joints (digits, thumb, wrist, elbow).
- Postural control (neutral spine, centralization of the GH joint, proper scapular setting) during static and dynamic conditions.
- Proper biomechanical alignment and accessory movements of the 4 shoulder complex joints (GH joint, acromioclavicular joint, sternoclavicular joint, and the floating scapulothoracic joint). Also prudent to verify the overall mobility of the thoracic cage and breathing movements.
- Strengthening of the typically weak / inhibited muscles (Such as the serratus anterior, rotator cuff muscles, lower trapezius, rhomboid muscles)
- Presence of tight muscles due to postural stress and neurological hyperactivity (such as the presence of trigger points).
- Tightness and lack of mobility of surrounding fascia or fascial trains.
- Lack of mobility of the upper extremity, cervical and thoracic neurological tissues (nerve flossing exercises as needed).
- Tension in any static tissues (such as the GH capsule).
- Dynamic stretching of the typically shortened and possibly over-active muscles (Pectorals muscles, upper trapezius, levator scapulae muscles)
- Reeducation of the rotator cuff muscles (working in rotations at various angles of elevation, scaption movements and functional activities).
- Eccentric exercises for rotator cuff muscles in case of a suspected rotator cuff tendinopathy, to restore collagen alignment of the tendons.
- Strengthening of surrounding supportive musculature (Biceps, triceps, latissimus dorsi, rhomboids, cervical stability muscles, dorsal spine supportive musculature).
- Muscles re-education of the agonist, antagonist and synergist muscles. Muscular timing (coordinator contractions) are a key component to focus on during shoulder rehabilitation.
Progression factors to consider to challenge the neuromuscular control of the shoulder complex:[edit | edit source]
- Postural control and positioning : static postures towards dynamic movements.
- Strengthening: body weight / rehabilitation bands / free weights / functional strengthening.
- Repetitions: endurance (high repetitions, low load), strength and performance (low repetitions, high load).
- Speed: slow movements towards quicker movements (always under control).
- Joint loading: non-weightbearing towards weight-bearing.
- Surface: stable surface (wall / floor) towards unstable surface (bosu ball, stability disc, movement boards) also incline vs. decline.
- Joint movements: Single joint movements (i.e. GH joint only) towards multi-joint movements (entire shoulder complex and upper extremity).
- Functional movements: throwing, catching, rolling and sport specific movements. Also the use of external perturbations, such as the Water Pipe (training equipment with sand or liquid inside to cause reactionary movements).
For more exercises for the rotator cuff complex:[edit | edit source]
- Selecting exercises-for rotator cuff related shoulder pain interview with hilkka virtapohja
- OrthoInfo
- Systematic review: Exercise rehabilitation for rotator cuff tears (2016)
[edit | edit source]
- Proprioception
- Neuromuscular exercise program
- Neuromuscular adaptations to exercise
- Shoulder instability
- Motor control
- Biomechanics of the shoulder
- Throwing biomechanics
Check out some more resources:[edit | edit source]
References[edit | edit source]
- ↑ Myers, J.B., C.A. Wassinger, and S.M. Lephart. Sensorimotor Contribution to Shoulder Joint Stability, in The Athlete’s Shoulder. 2009, Elsevier. p. 655-669.
- ↑ Lephart SM, Riemann BL, Fu FH. Introduction to the sensorimotor system. In: Lephart SM, Fu FH, eds. Proprioception and Neuromuscular Control in Joint Stability. Champaign, IL: Human Kinetics; 2000:37–51
- ↑ Blasier RB, Carpenter JE, Huston LJ (1994) Shoulder proprioception: effect of joint laxity, joint position and direction of motion. Orthop Rev 23:45–50.
- ↑ Curl LA, Warren RF. Glenohumeral joint stability: selective cutting studies on the static capsular restraints. Clinical Orthopaedics and Related Research®. 1996 Sep 1;330:54-65.
- ↑ 5.0 5.1 Wilk KE, Yenchak AJ, Arrigo CA, Andrews JR. The advanced throwers ten exercise program: a new exercise series for enhanced dynamic shoulder control in the overhead throwing athlete. Phys Sportsmed. 2011;39(4):91–3847. https://doi.org/10.3810/psm.2011.11.1943.
- ↑ Myers JB, Lephart SM. The role of the sensoriomotor system in the athletic shoulder. J Athl Train. 2000;35(3):351–63.
- ↑ 7.0 7.1 7.2 Levangie PK, Norkin CC. Joint Structure and Function; A Comprehensive Analysis. 5th. Philadelphia: Fadavis Company. 2012.
- ↑ Hallock GG. The hemideltoid muscle flap. Ann Plast Surg. 2000 Jan;44(1):18-22.
- ↑ Levangie PK, Norkin CC. Joint Structure and Function; A Comprehensive Analysis. 5th. Philadelphia: Fadavis Company. 2012.
- ↑ 10.0 10.1 10.2 10.3 Lam JH, Bordoni B. Anatomy, Shoulder and Upper Limb, Arm Abductor Muscles. [Updated 2020 Mar 31]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK537148/
- ↑ Escamilla RF, Yamashiro K, Paulos L, Andrews JR. Shoulder muscle activity and function in common shoulder rehabilitation exercises. Sports medicine. 2009 Aug 1;39(8):663-85.
- ↑ Longo UG, Berton A, Papapietro N, Maffulli N, Denaro V. Biomechanics of the rotator cuff: European perspective. InRotator Cuff Tear 2012 (Vol. 57, pp. 10-17). Karger Publishers.
- ↑ Neumann DA, Camargo PR. Kinesiologic considerations for targeting activation of scapulothoracic muscles: part 1: serratus anterior. Brazilian journal of physical therapy. 2019 Feb 2.
- ↑ Camargo PR, Neumann DA. Kinesiologic considerations for targeting activation of scapulothoracic muscles–part 2: trapezius. Brazilian journal of physical therapy. 2019 Feb 3.
- ↑ Muscle and Motion. Force Couple , Scapular Force Couple. Available from: http://www.youtube.com/watch?v=YbbzQs7OBoY[last accessed 12/3/2020]
- ↑ <article> Joseph B. Myers, Ji-Hye Hwang, Maria R. Pasquale, J. Troy Blackburn and Scott M. Lephart. Rotator cuff coactivation ratios in participants with subacromial impingement syndrome. Journal of Science and Medicine in Sport, Volume 12, Issue 6, November 2009, Pages 603-608 </article>
- ↑ Reinold MM, Gill TJ, Wilk KE, Andrews JR. Current concepts in the evaluation and treatment of the shoulder in overhead throwing athletes, part 2: injury prevention and treatment. Sports Health. 2010;2(2):101–15. https://doi.org/10.1177/1941738110362518.
- ↑ Eshoj, H. R., Rasmussen, S., Frich, L. H., Hvass, I., Christensen, R., Boyle, E., Juul-Kristensen, B. (2020). Neuromuscular Exercises Improve Shoulder Function More Than Standard Care Exercises in Patients With a Traumatic Anterior Shoulder Dislocation: A Randomized Controlled Trial. Orthopaedic Journal of Sports Medicine. https://doi.org/10.1177/2325967119896102
- ↑ Baritello, O., Khajooei, M., Engel, T. et al. Neuromuscular shoulder activity during exercises with different combinations of stable and unstable weight mass. BMC Sports Sci Med Rehabil 12, 21 (2020). https://doi.org/10.1186/s13102-020-00168-x.
- ↑ Aagaard P, Simonsen EB, Andersen JL, Magnusson P, Dyhre-Poulsen P. Neural adaptation to resistance training: changes in evoked V-wave and H-reflex responses. J Appl Physiol. 2002;92(6):2309–18. https://doi.org/10.1152/japplphysiol.01185.2001.
- ↑ Behm DG. Neuromuscular implications and applications of resistance training; 1995. p. 264–74.
- ↑ Behm DG, Anderson KG. The role of instability with resistance training. J strength Cond Res. 2006;20:716–22.
- ↑ White Lion Athletics. Resistance Band Exercises: Best Exercises for Shoulder Rehab and Scapular Stabilzation. Available from: http://www.youtube.com/watch?v=Vez6-NTFkS8[last accessed 11/4/2020]