Cholecystitis: Difference between revisions
Dave Pariser (talk | contribs) m (small grammatical change) |
No edit summary |
||
| (154 intermediate revisions by 11 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox"> | |||
'''Original Editors '''- [[User:David Martin|David Martin]] | '''Original Editors '''- [[User:David Martin|David Martin]] as part of the [[Pathophysiology of Complex Patient Problems|Bellarmine University's Pathophysiology of Complex Patient Problems project.]] | ||
''' | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | ||
</div> | </div> | ||
== | == Intoduction == | ||
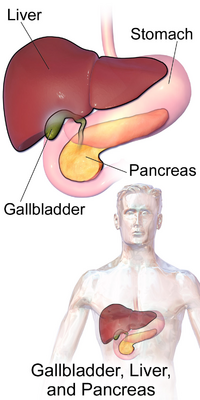
[[File:Gallbladder, Liver, and Pancreas.png|right|frameless|400x400px]] | |||
Cholecystitis is an inflammation of the gallbladder, which can be acute or chronic and occur with (calculus) or without (acalculus) gallstones<ref name="p6">HOWARD M. MEDICAL NUTRITION THERAPY IN CHOLECYSTITIS, CHOLELITHIASIS AND CHOLECYSTECTOMY. 2015.</ref>. It occurs most often as a result of impaction of the gallstones in the cystic duct, leading to obstruction of bile flow and painful distention of the gallbladder. It can be very painful and usually needs prompt medical treatment. | |||
The gallbladder is a small organ underneath the liver on the right side of the upper abdomen. It stores a thick dark green fluid called bile which the liver produces to help with digestion.<ref name=":2">Health Direct Cholecystitis Available:https://www.healthdirect.gov.au/cholecystitis-gallbladder-inflammation (accessed 3.9.2021)</ref> | |||
This 2.5 minute video gives a good summary of the condition{{#ev:youtube|SKxl_6QPMHY}} | |||
== Etiology == | |||
Cholecystitis most frequently occurs when gallstones (stones that form within the bile coming down from the liver) block the tube leading out of the gallbladder. This results in a build-up of bile, which causes inflammation. | |||
Cholecystitis can also be caused by other problems with the bile duct eg a tumour, problems with blood supply to the gallbladder, and [[Infectious Disease|infection]]<nowiki/>s. | |||
The condition may settle down on its own, but cholecystitis tends to come back. Most people eventually need [[Surgery and General Anaesthetic|surgery]] to remove the gallbladder. Sometimes, cholecystitis can lead to liver inflammation, a serious infection, a torn gallbladder, or the death of some of the tissue in the gallbladder. | |||
== Epidemiolgy == | |||
Gallstone disease is very common. About 10-20% of the world population will develop gallstones at some point in their life and about 80% of them are asymptomatic. There are approximately 500,000 cholecystectomies done yearly in the United Stated for gallbladder disease. | |||
* The incidence of gallstone formation increases yearly with age. | |||
* Over one-quarter of women older than the age of 60 will have gallstones. | |||
* Obesity increases the likelihood of gallstones, especially in women due to increases in the biliary secretion of cholesterol. On the other hand, patients with drastic weight loss or fasting have a higher chance of gallstones secondary to biliary stasis. | |||
* People with chronic illnesses such as diabetes also have an increase in gallstone formation as well as reduced gallbladder wall contractility due to neuropathy.<ref name=":0">Jones MW, Gnanapandithan K, Panneerselvam D, Ferguson T. [https://www.ncbi.nlm.nih.gov/books/NBK470236/ Chronic Cholecystitis]. Available:https://www.ncbi.nlm.nih.gov/books/NBK470236/ (accessed 3.9.2021)</ref> | |||
* Other conditions that cause the breakdown of blood cells, for example, sickle cell disease, also increase the incidence of gallstones.<ref name=":1">Jones MW, Genova R, O'Rourke MC. Acute cholecystitis.Available:https://www.ncbi.nlm.nih.gov/books/NBK459171/ (accessed 3.9.2021)</ref> | |||
< | == Pathology == | ||
[[File:Gallbladder.gif|right|frameless]] | |||
Occlusion of the cystic duct or malfunction of the mechanics of the gallbladder emptying is the basic underlying pathologies of this disease. Over 90% of chronic cholecystitis is associated with the presence of gallstones. Gallstones, by causing intermittent obstruction of the bile flow, most commonly by blocking the cystic duct lead to inflammation and edema in the gall bladder wall. Occlusion of the common bile duct such as in neoplasms or strictures can also lead to stasis of the bile flow causing gallstone formation with resultant chronic cholecystitis<ref name=":0" />. | |||
Cases of acute untreated cholecystitis could lead to perforation of the gallbladder, sepsis, and death. Gallstones form from various materials such as bilirubinate or cholesterol. These materials increase the likelihood of cholecystitis and cholelithiasis in conditions such as sickle cell disease where red blood cells are broken down forming excess bilirubin and forming pigmented stones. Patients with excessive calcium such as in hyperparathyroidism can form calcium stones. Patients with excessive cholesterol can form cholesterol stones. Occlusion of the common bile duct such as in neoplasms or strictures can also lead to stasis of the bile flow causing gallstone formation.<ref name=":1" /> | |||
Image 2: Gall Bladder | |||
== Presentation == | |||
Symptoms of cholecystitis include: | |||
* an intense pain in the middle or right side of the upper abdomen, or between the shoulders | |||
* indigestion, especially after fatty food | |||
* nausea and/or vomiting | |||
* fever | |||
* Symptoms often appear after someone has eaten a large, fatty meal. | |||
== Diagnosis == | |||
If cholecystitis is suspected, the Dr will examine the client and ask you about their medical history. They will usually order an ultrasound of your abdomen. They may also do a blood test to look for signs of liver inflammation or infection<ref name=":2" />. | |||
< | [[Laboratory Tests|Laboratory testing]] is not specific or sensitive in making a diagnosis of chronic cholecystitis. Leukocytosis and abnormal liver function tests may not be present in these patients, unlike the acute disease. However basic laboratory testing in the form of a metabolic panel, [[Liver Function Tests|liver function]]<nowiki/>s, and complete blood count should be performed. Cardiac testing including [[Electrocardiogram|EKG]] and troponins should be considered in the appropriate clinical setting<ref name=":0" />. | ||
== Treatment == | |||
Cholecystitis can sometimes settle down if you eat a low-fat diet. You may also be given medicine to dissolve gallstones. | |||
If admitted to hospital, client will be fed and hydrated through an intravenous drip and may have antibiotics to fight infection. They also will probably also need medicine for pain relief. | |||
* | * Most people have their gallbladder removed 2 to 3 days after they are admitted to hospital (preferred recommended treatment is the removal of the gallbladder). In the past, this was done through an open laparotomy incision. Now laparoscopic cholecystectomy is the procedure of choice. This procedure has low mortality and morbidity, a quick recovery time (usually one week), and good results<ref name=":1" />. | ||
* You don’t need your gallbladder, and after the operation, bile will flow straight from your liver to your small intestine<ref name=":2" />. | |||
* | |||
The diagnosis and management of cholecystitis is a multi-disciplinary team approach. A high index of suspicion is vital in the diagnosis. Referral to the surgical team followed by decision making on the need for laparoscopic surgery are the next steps. Good surgical care with good postoperative follow up is also essential. Counseling for food habits with nutritionist support and lifestyle changes are crucial in patients being treated conservatively.<ref name=":0" /> | |||
== Physical Therapy Management == | |||
< | *Systemic screen indicated if mid back, scapular, or right shoulder pain with no trauma<ref name="p7">Goodman CC, Snyder TEK. Differential diagnosis for physical therapists screening for referral. St. Louis, MO: Saunders Elsevier; 2013.</ref>. | ||
*Immediate referral: new onset myopathy (especially older adult) with a history of statin use<ref name="p7" />. | |||
*Physician referral: Hx of cancer or risk factors for hepatitis with obvious signs of hepatic disease, unknown cause arthralgias with hx or risk factors for hepatitis, bilateral carpal tunnel syndrome or asterixis, unknown sensory neuropathy with associated hepatic signs and symptoms<ref name="p7" />. | |||
*Screen for hepatic diseases if: R shoulder/scapular/midback pain with unknown cause, unable to localize shoulder pain that is not limited by painful symptoms, GI symptoms especially associated with eating, bilateral carpal or tarsal tunnel syndrome, personal hx of hepatitis, cancer, liver, gallbladder disease, recent hx of statin usage, recent operation (post-operative jaundice), injection drug use <6mo, skin or eye color changes, alcohol consumption, contact with others with jaundice<ref name="p7" />. | |||
*Usual postoperative exercises for any surgical procedure apply, especially in cases where complications may occur. Early activity assists with the return of intestinal motility, so the patient is encouraged to begin progressive movement and ambulation as soon as possible. | |||
Some examples of postoperative exercises include: | |||
== | *breathing exercises | ||
*positioning changes | |||
*coughing | |||
*wound splinting | |||
*compressive stockings | |||
*lower extremity exercises<ref name="G&B">Goodman CC, Boissonnault W. Pathology Implications for the Physical Therapist. Saunders: Philadelphia; 1998.</ref><ref name="G&F">Goodman CC, Fuller K. Pathology Implications for the Physical Therapist Third Edition. Saunders Elsevier: St. Louis; 2009.</ref> | |||
== Prognosis == | |||
The | The prognosis for acute and chronic cholecystitis is good if the patient seeks medical treatment. An increase in serum WBC count, ESR, C-reactive protein, and procalcitonin levels indicate an increase in severity of cholecystitis. Also, gangrene and abscess increase the risk of conversion<ref name="p0">Yuzbasioglu Y, Duymaz H, Tanrikulu C, Halhalli H, Koc M, Coskun F, et al. Role of Procalcitonin in Evaluation of the Severity of Acute Cholecystitis. Eurasian Journal Of Medicine [serial on the Internet]. (2016, Oct), [cited March 22, 2017]; 48(3): 162-166. Available from: Academic Search Complete.</ref>. All of these factors increase the risk of post-operative complication<ref name="p4">Terho P, Leppäniemi A, Mentula P. Laparoscopic cholecystectomy for acute calculous cholecystitis: a retrospective study assessing risk factors for conversion and complications. World Journal Of Emergency Surgery [serial on the Internet]. (2016, Nov 16), [cited March 22, 2017]; 111-9. Available from: Academic Search Complete.</ref>. Acute attacks should resolve spontaneously, but a person may experience reoccurences. This may lead to the patient having their gallbladder removed. Old age is a poor prognostic factor as mortality secondary to acute cholecystitis is 5 to 10 percent for clients that are older than 60 and have serious associated diseases<ref>Goodman CC, Fuller K. Pathology Implications for the Physical Therapist Third Edition. Saunders Elsevier: St. Louis; 2009.</ref><ref>ASİLTÜRK LÜLLECİ Z, BAŞYİĞİT S, PİRİNÇÇİ SAPMAZ F, UZMAN M, KEFELİ A, NAZLIGÜL Y, et al. Comparison of ultrasonographic and laboratory findings of acute cholecystitis between elderly and nonelderly patients. Turkish Journal Of Medical Sciences [serial on the Internet]. (2016, Oct), [cited March 21, 2017]; 46(5): 1428-1433. Available from: Academic Search Complete.</ref>. | ||
== | == Differential Diagnosis == | ||
* Appendicitis | |||
* Biliary colic | |||
* Cholangitis | |||
* Mesenteric ischemia | |||
* Gastritis | |||
* Peptic ulcer disease<ref name=":1" /> | |||
<br> | |||
== References == | == References == | ||
<references /> | <references /> | ||
[[Category:Bellarmine_Student_Project]] | [[Category:Bellarmine_Student_Project]] | ||
Latest revision as of 06:30, 3 September 2021
Original Editors - David Martin as part of the Bellarmine University's Pathophysiology of Complex Patient Problems project.
Top Contributors - David Martin, Spencer Fuehne, Admin, Lucinda hampton, Elaine Lonnemann, Laura Ritchie, Dave Pariser, 127.0.0.1, WikiSysop, Kim Jackson and Wendy Walker
Intoduction[edit | edit source]
Cholecystitis is an inflammation of the gallbladder, which can be acute or chronic and occur with (calculus) or without (acalculus) gallstones[1]. It occurs most often as a result of impaction of the gallstones in the cystic duct, leading to obstruction of bile flow and painful distention of the gallbladder. It can be very painful and usually needs prompt medical treatment.
The gallbladder is a small organ underneath the liver on the right side of the upper abdomen. It stores a thick dark green fluid called bile which the liver produces to help with digestion.[2]
This 2.5 minute video gives a good summary of the condition
Etiology[edit | edit source]
Cholecystitis most frequently occurs when gallstones (stones that form within the bile coming down from the liver) block the tube leading out of the gallbladder. This results in a build-up of bile, which causes inflammation.
Cholecystitis can also be caused by other problems with the bile duct eg a tumour, problems with blood supply to the gallbladder, and infections.
The condition may settle down on its own, but cholecystitis tends to come back. Most people eventually need surgery to remove the gallbladder. Sometimes, cholecystitis can lead to liver inflammation, a serious infection, a torn gallbladder, or the death of some of the tissue in the gallbladder.
Epidemiolgy[edit | edit source]
Gallstone disease is very common. About 10-20% of the world population will develop gallstones at some point in their life and about 80% of them are asymptomatic. There are approximately 500,000 cholecystectomies done yearly in the United Stated for gallbladder disease.
- The incidence of gallstone formation increases yearly with age.
- Over one-quarter of women older than the age of 60 will have gallstones.
- Obesity increases the likelihood of gallstones, especially in women due to increases in the biliary secretion of cholesterol. On the other hand, patients with drastic weight loss or fasting have a higher chance of gallstones secondary to biliary stasis.
- People with chronic illnesses such as diabetes also have an increase in gallstone formation as well as reduced gallbladder wall contractility due to neuropathy.[3]
- Other conditions that cause the breakdown of blood cells, for example, sickle cell disease, also increase the incidence of gallstones.[4]
Pathology[edit | edit source]
Occlusion of the cystic duct or malfunction of the mechanics of the gallbladder emptying is the basic underlying pathologies of this disease. Over 90% of chronic cholecystitis is associated with the presence of gallstones. Gallstones, by causing intermittent obstruction of the bile flow, most commonly by blocking the cystic duct lead to inflammation and edema in the gall bladder wall. Occlusion of the common bile duct such as in neoplasms or strictures can also lead to stasis of the bile flow causing gallstone formation with resultant chronic cholecystitis[3].
Cases of acute untreated cholecystitis could lead to perforation of the gallbladder, sepsis, and death. Gallstones form from various materials such as bilirubinate or cholesterol. These materials increase the likelihood of cholecystitis and cholelithiasis in conditions such as sickle cell disease where red blood cells are broken down forming excess bilirubin and forming pigmented stones. Patients with excessive calcium such as in hyperparathyroidism can form calcium stones. Patients with excessive cholesterol can form cholesterol stones. Occlusion of the common bile duct such as in neoplasms or strictures can also lead to stasis of the bile flow causing gallstone formation.[4]
Image 2: Gall Bladder
Presentation[edit | edit source]
Symptoms of cholecystitis include:
- an intense pain in the middle or right side of the upper abdomen, or between the shoulders
- indigestion, especially after fatty food
- nausea and/or vomiting
- fever
- Symptoms often appear after someone has eaten a large, fatty meal.
Diagnosis[edit | edit source]
If cholecystitis is suspected, the Dr will examine the client and ask you about their medical history. They will usually order an ultrasound of your abdomen. They may also do a blood test to look for signs of liver inflammation or infection[2].
Laboratory testing is not specific or sensitive in making a diagnosis of chronic cholecystitis. Leukocytosis and abnormal liver function tests may not be present in these patients, unlike the acute disease. However basic laboratory testing in the form of a metabolic panel, liver functions, and complete blood count should be performed. Cardiac testing including EKG and troponins should be considered in the appropriate clinical setting[3].
Treatment[edit | edit source]
Cholecystitis can sometimes settle down if you eat a low-fat diet. You may also be given medicine to dissolve gallstones.
If admitted to hospital, client will be fed and hydrated through an intravenous drip and may have antibiotics to fight infection. They also will probably also need medicine for pain relief.
- Most people have their gallbladder removed 2 to 3 days after they are admitted to hospital (preferred recommended treatment is the removal of the gallbladder). In the past, this was done through an open laparotomy incision. Now laparoscopic cholecystectomy is the procedure of choice. This procedure has low mortality and morbidity, a quick recovery time (usually one week), and good results[4].
- You don’t need your gallbladder, and after the operation, bile will flow straight from your liver to your small intestine[2].
The diagnosis and management of cholecystitis is a multi-disciplinary team approach. A high index of suspicion is vital in the diagnosis. Referral to the surgical team followed by decision making on the need for laparoscopic surgery are the next steps. Good surgical care with good postoperative follow up is also essential. Counseling for food habits with nutritionist support and lifestyle changes are crucial in patients being treated conservatively.[3]
Physical Therapy Management[edit | edit source]
- Systemic screen indicated if mid back, scapular, or right shoulder pain with no trauma[5].
- Immediate referral: new onset myopathy (especially older adult) with a history of statin use[5].
- Physician referral: Hx of cancer or risk factors for hepatitis with obvious signs of hepatic disease, unknown cause arthralgias with hx or risk factors for hepatitis, bilateral carpal tunnel syndrome or asterixis, unknown sensory neuropathy with associated hepatic signs and symptoms[5].
- Screen for hepatic diseases if: R shoulder/scapular/midback pain with unknown cause, unable to localize shoulder pain that is not limited by painful symptoms, GI symptoms especially associated with eating, bilateral carpal or tarsal tunnel syndrome, personal hx of hepatitis, cancer, liver, gallbladder disease, recent hx of statin usage, recent operation (post-operative jaundice), injection drug use <6mo, skin or eye color changes, alcohol consumption, contact with others with jaundice[5].
- Usual postoperative exercises for any surgical procedure apply, especially in cases where complications may occur. Early activity assists with the return of intestinal motility, so the patient is encouraged to begin progressive movement and ambulation as soon as possible.
Some examples of postoperative exercises include:
- breathing exercises
- positioning changes
- coughing
- wound splinting
- compressive stockings
- lower extremity exercises[6][7]
Prognosis[edit | edit source]
The prognosis for acute and chronic cholecystitis is good if the patient seeks medical treatment. An increase in serum WBC count, ESR, C-reactive protein, and procalcitonin levels indicate an increase in severity of cholecystitis. Also, gangrene and abscess increase the risk of conversion[8]. All of these factors increase the risk of post-operative complication[9]. Acute attacks should resolve spontaneously, but a person may experience reoccurences. This may lead to the patient having their gallbladder removed. Old age is a poor prognostic factor as mortality secondary to acute cholecystitis is 5 to 10 percent for clients that are older than 60 and have serious associated diseases[10][11].
Differential Diagnosis[edit | edit source]
- Appendicitis
- Biliary colic
- Cholangitis
- Mesenteric ischemia
- Gastritis
- Peptic ulcer disease[4]
References[edit | edit source]
- ↑ HOWARD M. MEDICAL NUTRITION THERAPY IN CHOLECYSTITIS, CHOLELITHIASIS AND CHOLECYSTECTOMY. 2015.
- ↑ 2.0 2.1 2.2 Health Direct Cholecystitis Available:https://www.healthdirect.gov.au/cholecystitis-gallbladder-inflammation (accessed 3.9.2021)
- ↑ 3.0 3.1 3.2 3.3 Jones MW, Gnanapandithan K, Panneerselvam D, Ferguson T. Chronic Cholecystitis. Available:https://www.ncbi.nlm.nih.gov/books/NBK470236/ (accessed 3.9.2021)
- ↑ 4.0 4.1 4.2 4.3 Jones MW, Genova R, O'Rourke MC. Acute cholecystitis.Available:https://www.ncbi.nlm.nih.gov/books/NBK459171/ (accessed 3.9.2021)
- ↑ 5.0 5.1 5.2 5.3 Goodman CC, Snyder TEK. Differential diagnosis for physical therapists screening for referral. St. Louis, MO: Saunders Elsevier; 2013.
- ↑ Goodman CC, Boissonnault W. Pathology Implications for the Physical Therapist. Saunders: Philadelphia; 1998.
- ↑ Goodman CC, Fuller K. Pathology Implications for the Physical Therapist Third Edition. Saunders Elsevier: St. Louis; 2009.
- ↑ Yuzbasioglu Y, Duymaz H, Tanrikulu C, Halhalli H, Koc M, Coskun F, et al. Role of Procalcitonin in Evaluation of the Severity of Acute Cholecystitis. Eurasian Journal Of Medicine [serial on the Internet]. (2016, Oct), [cited March 22, 2017]; 48(3): 162-166. Available from: Academic Search Complete.
- ↑ Terho P, Leppäniemi A, Mentula P. Laparoscopic cholecystectomy for acute calculous cholecystitis: a retrospective study assessing risk factors for conversion and complications. World Journal Of Emergency Surgery [serial on the Internet]. (2016, Nov 16), [cited March 22, 2017]; 111-9. Available from: Academic Search Complete.
- ↑ Goodman CC, Fuller K. Pathology Implications for the Physical Therapist Third Edition. Saunders Elsevier: St. Louis; 2009.
- ↑ ASİLTÜRK LÜLLECİ Z, BAŞYİĞİT S, PİRİNÇÇİ SAPMAZ F, UZMAN M, KEFELİ A, NAZLIGÜL Y, et al. Comparison of ultrasonographic and laboratory findings of acute cholecystitis between elderly and nonelderly patients. Turkish Journal Of Medical Sciences [serial on the Internet]. (2016, Oct), [cited March 21, 2017]; 46(5): 1428-1433. Available from: Academic Search Complete.