Cardiac Implantable Electronic Devices (CIEDs)
Original Editor - Lucinda hampton
Top Contributors - Lucinda hampton, Justin Bryan and Kim Jackson
Introduction[edit | edit source]
Cardiac implantable electronic devices or CIEDs, are a very common medical device[1]. The number of implanted cardiovascular devices has dramatically increased in recent years.
- With the advent of implantable cardioverterdefibrillators and cardiac resynchronization therapy, devices have become more complex.
- There is also an increase of minimally invasive procedures to replace heart valves.[1].
There are two major types of cardiac conduction devices:
- pacemakers
- automatic implantable cardioverter-defibrillators (AICD/ICD) (may be co-implanted as an ICD-pacemaker combination).
Leadless cardiac pacemakers (LLPM) are a recently introduced type of cardiac conduction device. These pacemakers are self-contained right ventricular single-chamber pacemakers[2]. The LLPM use is constantly growing in daily clinical practice and is considered a landmark innovation, through which a new era of cardiac pacing has begun.[3]
Why Pacemakers are Used[edit | edit source]
Heart failure affects about 26 million people all over the world eg about 6 million adults in the US and 900 000 people in the UK suffering from this chronic and often crippling condition.
- The mortality in this illness is about 50% at 5 years from diagnosis.
- Besides immense health costs and the high death rate, life can be extremely burdensome for such patients.
- Many of them are fitted with cardiac pacemakers to keep the struggling heart beating at a regular rate, so as to optimize the work it does at the least possible effort.
- They perform many functions eg bradycardia pacing, cardiac resynchronisation for heart failure, defibrillation and anti-tachycardia pacing for tachyarrhythmias[1]
- Cardiac pacemakers are also often used to treat patients who have survived a heart attack. After a heart attack damage to the heart often occurs eg the heart muscle may have been injured badly, and require an externally generated rhythm as it beats too slowly; the nerve pathways that conduct the electrical impulse from the natural pacemaker region are damaged and fail to carry it all over the heart as usual, leading to irregular and uncoordinated contraction, quickly lead to heart failure and death[4].
Major components[edit | edit source]
2. Major Components (no leads if leadless)
- A pulse generator: a small metal case that contains electronic circuitry with a small computer and a battery that regulate the impulses sent to the heart.
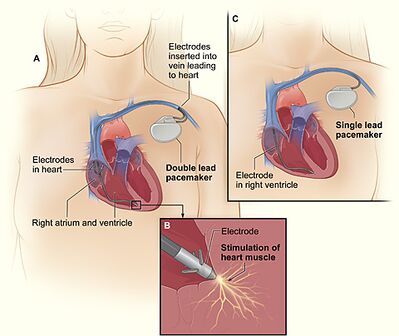
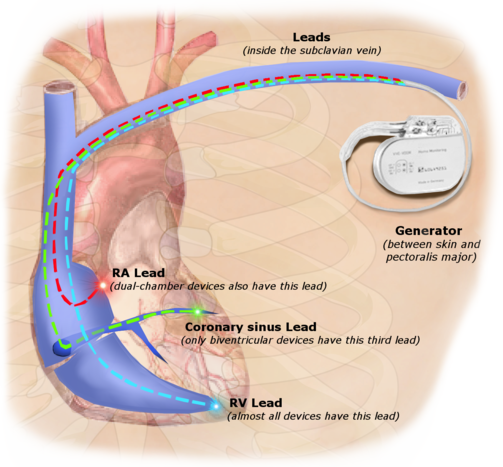
- The lead (or leads) is an insulated wire that is connected to the pulse generator on one end, with the other end placed inside one of the heart's chambers. The lead is almost always placed so that it runs through a large vein in the chest leading directly to the heart. The electrode on the end of a lead touches the heart wall. The lead delivers the electrical impulses to the heart. It also senses the heart's electrical activity and relays this information back to the pulse generator. Pacemaker leads may be positioned in the atrium (upper chamber) or ventricle (lower chamber) or both, depending on the medical condition.[5][2]
Pacemakers[edit | edit source]
Categorisation depends on the number of electrodes and location of pacing:
- Single chamber cardiac pacers: lead terminates in the right ventricle
- Dual-chamber (DDD) pacemakers have two leads (one in the right atrium, one in the right ventricle), each capable of sensing intrinsic electrical activity to determine the need for pacing in each chamber. For “on-demand” dual-chamber pacemakers—the most common types—atrial pacing is determined by the lower rate limit while ventricular pacing is determined by the separately programmed maximum AV delay.[6]
- Biventricular pacers (also known as cardiac resynchronisation therapy): Inserted in the same fashion as a standard pacemaker via the subclavian vein. The major distinguishing feature of a biventricular pacemaker is the insertion of a left ventricular lead to accomplish left ventricular pacing, in addition to the right ventricular lead for right ventricular pacing . Biventricular pacing is an excellent option for certain patients with advanced HF[7].
- Leadless cardiac pacers: implanted into the right ventricle with no leads, introduced in 2015. Not everyone is a candidate for a leadless pacemaker. Currently, the device is available only for patients with certain medical conditions and a slow heart rate (bradycardia) who need single-chamber pacing only. Because there are no wires or generator, there is no need for recipient to limit upper body activity after the implant[8].[2]
Automatic implantable cardioverter defibrillators[edit | edit source]
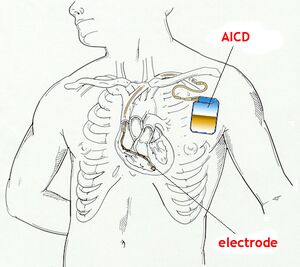
AICDs are common cardiac devices designed for both patient monitoring and therapy in case of ventricular tachycardia or fibrillation. AICDs consist of various combinations of sensing and shocking electrodes. They are frequently combined with a pacemaker, treating both the patient’s established arrhythmia and also acting as a fail-safe system should ventricular fibrillation or ventricular tachycardia occur.
Activation[edit | edit source]
If the heart's rate is slower than the programmed limit, an electrical impulse is sent through the lead to the electrode and causes the heart to beat at a faster rate.
When the heart beats at a rate faster than the programmed limit, the pacemaker generally monitors the heart rate and will not pace. Modern pacemakers are programmed to work on demand only, so they do not compete with natural heartbeats. Generally, no electrical impulses will be sent to the heart unless the heart's natural rate falls below the pacemaker's lower limit.
A biventricular pacemaker (used in the treatment of specific types of heart failure) is used when the two ventricles do not pump in a normal manner (ie ventricular dyssynchrony). When this happens, less blood is pumped by the heart. A biventricular pacemaker paces both ventricles at the same time, increasing the amount of blood pumped by the heart. This type of treatment is called cardiac resynchronization therapy or CRT[5].
Landmark Innovations[edit | edit source]
- Cardiologists at Monash Health have implanted the world’s first totally leadless, physiologic pacemaker system, designed to improve cardiac function in a patient with a severe cardiomyopathy, otherwise known as heart failure. This unique procedure has, for the first time, used two innovative medical devices to resynchronise the pumping of the heart without requiring any wires to be implanted inside the patient’s heart.
- In contrast to transvenous systems, the ‘leadless’ devices used in this patient can be implanted directly inside the heart’s ventricles without any connecting wires.
- The procedure utilises keyhole access through a vein, where an ingenious, ultrasonically activated pacemaker the size of a grain of rice was implanted in the left ventricle. Using the same access, the latest generation, leadless right ventricular pacemaker was also implanted.
Using a new synchronisation method described as ‘physiological pacing’, the right-sided device can sense and track the activity of the atrium above, where the heart’s normal rhythm originates. Working in combination, these devices will provide physiologic, cardiac resynchronisation therapy without the need for wires inside the heart[9].
2.A new study published in the Journal of Physiology on November 14, 2019, reports the development of a radically different type of cardiac pacemaker which could change the prognosis of patients with heart failure.
- This bionic pacemaker follows the natural change in heart rhythm that occurs with breathing, and causes a steep improvement in the efficiency at which the heart supplies blood to the body. The normal heartbeat is a dynamic phenomenon. With every intake of breath, it can be felt to speed up, only to slow down with exhalation – a fascinating change in speed and rhythm called respiratory sinus arrhythmia. There are also several more minor other body processes which modulate the heart rate, causing normal heart rate variability.
- Most automatic pacemakers generate a metronome-like rhythm when the patient is at rest, irrespective of the body’s other operations. This doesn’t take advantage of the natural changes that occur in the body.
- This new bionic pacemaker represent a novel therapy in addition to those already available for the treatment of heart failure.[4]
Physiotherapy[edit | edit source]
There are no specific international policies regarding the administration of physiotherapy modalities in cardiac rhythm device patients and, thus, there are no specific guidelines to be implemented at the local level. Review of the literature and of recommendations from CRD manufacturers suggests that TENS, Diathermy, and Interferential Electrical Current Therapy are best avoided in patients with CRDs[10].
Use of upper limbs For 6 to 8 weeks (with device with leads):
• Avoid upper arm movement on the side of your pacemaker such as reaching high, raking, hanging things and swinging a golf club. • Do shoulder rolls daily on the side of the pacemaker to prevent shoulder stiffness. • You can have sex when you feel comfortable. • Ask your doctor when you can drive. • Do not do any heavy lifting. This means do not lift anything over kilograms or 10 pounds such as a bag of groceries, small suitcase or small child.
A patient's lifestyle is usually not modified to any great degree after the insertion of a pacemaker. There are a few activities that are unwise such as full contact sports and activities that involve intense magnetic fields (should be informed from treating Cardiologist)
- eg large and powerful magnets (MRI) affect pacemakers; do not use beds that vibrate; Large motors: the power from motors such as chain saws, cars, tractors, lawnmowers and recreational vehicles may confuse a pacemaker. If this happens, you will feel dizzy. This is related to how close you are. You need to be 1 foot or 30 centimetres from a working motor.[11]
Final Ending[edit | edit source]
A British charity wants to remove pacemakers from people who have died in the UK and send the devices to developing countries for re-use. Pace4Life says thousands of the life-saving devices, which cost thousands of pounds, are typically thrown away or buried with patients each year in the UK[12].
- Pacemaker reuse is feasible and safe and is a viable option for patients with bradyarrhythmias. Other than the expected lower battery life, reuse of pacemaker generators is noninferior to the use of new devices[13].
References[edit | edit source]
- ↑ 1.0 1.1 1.2 AJGP CIEDs Available from:https://www1.racgp.org.au/ajgp/2018/may/cardiac-rhythm-management-devices (accessed 29.4.2021)
- ↑ 2.0 2.1 2.2 Radiopedia Cardiac conduction devices Available:https://radiopaedia.org/articles/cardiac-conduction-devices (accessed 29.4.2021)
- ↑ Curnis A, Salghetti F, Cerini M, Fabbricatore D, Ghizzoni G, Arrigoni L, Generati G, Arabia G, Maiolo V, Aboelhassan M, Bontempi L. Leadless pacemaker: State of the art and incoming developments to broaden indications. Pacing and Clinical Electrophysiology. 2020 Oct 22.Available from:https://onlinelibrary.wiley.com/doi/10.1111/pace.14097 (accessed 29.4.2021)
- ↑ 4.0 4.1 News Medical New type of bionic pacemaker Available:https://www.news-medical.net/news/20191114/New-type-of-bionic-pacemaker.aspx (accessed 30.4.2021)
- ↑ 5.0 5.1 John Hopkins Pacemaker Available from:https://www.hopkinsmedicine.org/health/treatment-tests-and-therapies/pacemaker-insertion (accessed 30.4.2021)
- ↑ Goldberger AL, Goldberger ZD, Shvilkin A. Clinical electrocardiography: a simplified approach e-book. Elsevier Health Sciences; 2017 Mar 19.Available from: https://www.sciencedirect.com/topics/nursing-and-health-professions/dual-chamber-pacemaker(accessed 30.4.2021)
- ↑ Helio Biventricular pacing Available from:https://www.healio.com/cardiology/learn-the-heart/cardiology-review/topic-reviews/biventricular-pacing (accessed 30.4.2021)
- ↑ Cleveland clinic LLPM Available :https://my.clevelandclinic.org/health/treatments/17166-pacemakers-leadless-pacemaker (accessed 30.4.2021)
- ↑ Monash Health Monash Health implants world-first leadless pacemaker treatment for heart failure. Available: https://monashhealth.org/latest-news/2020/10/15/monash-health-implants-world-first-leadless-pacemaker-treatment-for-heart-failure/ (accessed 30.4.2021)
- ↑ Digby GC, Daubney ME, Baggs J, Campbell D, Simpson CS, Redfearn DP, Brennan FJ, Abdollah H, Baranchuk A. Physiotherapy and cardiac rhythm devices: a review of the current scope of practice. Europace. 2009 Jul 1;11(7):850-9.Available from:https://academic.oup.com/europace/article/11/7/850/498953 (accessed 30.4.2021)
- ↑ St Joes You and your pacemakerAvailable from:https://www.stjoes.ca/patients-visitors/patient-education/p-t/PacemakerSJH-trh%20(2).pdf (accessed 30.4.2021)
- ↑ Mazumdar T. British Charity Calls for Reuse of Pacemakers Abroad. BBB News Health. 2013.Available: https://www.bbc.com/news/health-24828244(accessed 30.4.2021)
- ↑ Nava S, Morales JL, Márquez MF, Barrera F, Gómez J, Colín L, Brugada J, Iturralde P. Reuse of pacemakers: comparison of short and long-term performance. Circulation. 2013 Mar 19;127(11):1177-83.Available:https://www.ahajournals.org/doi/full/10.1161/CIRCULATIONAHA.113.001584 (accessed 30.4.2021)